Abstract
Study design
Case control series with prospective data collection.
Objective
To establish whether incidental durotomy treated without primary suture repair adversely affects the outcome following lumbar surgery in the longer term.
Method
Outcome scores from a prospective database were used for an audit of dural tears in primary lumbar decompressive surgery. Outcome data collected includes the Short Form 36 General Health Questionnaire (SF36), the Oswestry Disability Index (ODI) and Visual Analogue Scores for leg pain (VAL) and back pain (VAB).
Results
Out of 200 consecutive procedures, a dural tear occurred in 19 (9.5 %) patients. Of 19 patients with a dural tear, data was incomplete in 4 patients, and 1 further patient who had their dural tear sutured was excluded, leaving 14 patients to be studied. There were seven males and seven females, with an average age of 50.8 years (31–69). These 14 patients (group 1) were compared to a matched group (age, sex, surgical diagnosis and duration of follow-up) of 14 patients (group 2) with no tear. Both groups had similar pre-operative scores. At 6-month follow-up, both groups had significant improvements in all outcomes measures except for the general health domain of the SF-36. At final follow-up, patients with dural tears appeared to have better improvements in outcome measures amongst the VAB, VAL and ODI with similar scores in the SF-36 domains.
Conclusion
Our study demonstrates that incidental durotomy in primary lumbar decompressive surgery can be successfully managed without primary suture repair with no adverse effect on surgical outcome in the longer term.
Keywords: Dural tears, Non-suture repair, Outcome
Introduction
Dural tears remain one of the most common complications of surgery related to the lumbar spine. The reported prevalence varies widely from <1 to 17 % [1–4]. A prospective study by Tafazal and Sell [5] of 1,549 cases in the United Kingdom reports rates of 3.5 % for primary discectomy, 8.5 % for spinal stenosis surgery and 13.2 % for revision discectomy.
Numerous consequences of dural tears have been reported including dural cutaneous fistula, pseudo-meningocoele formation, infection, subdural haematoma, meningitis and arachnoiditis [6]. The most common consequences appear to be a posture-related headache, photophobia and dizziness [6]. The purpose of this study was to establish whether managing a dural tear with non-suture repair techniques adversely affects the outcome for the patient in the longer term.
Materials and methods
The senior author (MLN) has maintained a prospective database of surgical procedures performed. Outcome data collected includes the Short Form 36 General Health Questionnaire (SF36) from which the four physical domains were analysed [physical function (PF), role physical (RP), bodily pain (BP), and general health (GH)], the Oswestry Disability Index (ODI) and Visual Analogue Scores for leg pain (VAL) and back pain (VAB). Data have been prospectively recorded pre-operatively and at routine follow-up. Surgical complications have also been recorded prospectively.
From the database, patients were identified who had undergone an elective primary lumbar decompressive procedure, and the incidence of dural tears was established. The medical records of patients with a dural tear (group 1) were examined to determine management at surgery and during the immediate post-operative period as well as to review any post-operative symptoms related to the tear (headache, photophobia, etc.), duration of bed rest and overall duration of hospital stay. A second group (group 2) was established as a control group, matched for age, sex, diagnosis and duration of follow-up from surgery. Patients in group 2 were derived from the same database, and were selected to match the parameters of the patients in group 1. Exclusion criteria included fusion procedures and suture repair of the dural tear. Outcomes for these two groups were compared at 6 months post-operatively and at long-term follow-up to determine whether the outcome of surgery in patients who had a dural tear, and who were treated with non-suture repair methods, differed to outcomes in patients where a dural tear had not occurred. Statistical analysis was performed using the Mann–Whitney U test.
Results
From 1999 to 2007 there were 200 patients recorded as undergoing elective primary lumbar decompressive surgery. All procedures were performed by the senior author, and the underlying diagnosis is shown in Table 1. Most operations involved single level surgery and no procedure involved a supplementary fusion. A dural tear occurred in 19 patients, giving an overall incidence of 9.5 %. The incidence of dural tear varied amongst the diagnostic groups (Table 2). Only one of the dural tears underwent primary suture repair and this patient has been excluded from the analysis. The remainder were merely covered with a variety of materials (Table 2).Tears were regarded as small if they were ≤0.5 cm and large if >0.5 cm. (Table 2). Following surgery, patients were kept on flat bed rest until any related symptoms had settled and then mobilised. Mean duration of bed rest was 2.6 days (range 2–4 days) while the average stay in hospital following surgery was 4.2 days (range 2–7 days). No patient had persistent drainage or required further surgical intervention for their dural tear.
Table 1.
Diagnosis in 200 cases
| Diagnosis | Number |
|---|---|
| Postero-lateral disc | 121 |
| Central disc | 23 |
| Central stenosis | 50 |
| Facet ganglion | 6 |
Table 2.
Dural tear cases
| Patient no. | Diagnosis | Procedure | Dural patch technique | Dural tear size | Bed rest duration | Total in-patient stay | Post-operative symptoms |
|---|---|---|---|---|---|---|---|
| 1 | Central stenosis | Decompressive laminectomy | Surgicel™ | Small | 3 | 7 | Headache/light-headedness |
| 2 | Central stenosis | Decompressive laminotomy | Surgicel™ | Large | 4 | 5 | Light-headedness |
| 3 | Central stenosis | Decompressive laminotomy | Fat | Small | 2 | 4 | Nil |
| 4 | Central stenosis | Decompressive laminectomy | Duragen™ | Punctate | 2 | 3 | Light-headedness |
| 5 | Central stenosis | Decompressive laminotomy | Duragen™ | Punctate | 3 | 6 | Light-headedness |
| 6 | Lateral stenosis | Decompressive laminectomy | Duragen™ | Small | 2 | 6 | Nil |
| 7 | Disc prolapse | Discectomy | Surgicel™ | Small | 2 | 5 | Light-headedness |
| 8 | Disc prolapse | Discectomy | Surgicel™ | Small | 1 | 2 | Nil |
| 9 | Disc prolapse | Discectomy | Nil | Small | 2 | 4 | Headache |
| 10 | Disc prolapse | Discectomy | Duragen™ | Small | 2 | 3 | Headache |
| 11 | Disc prolapse | Discectomy | No repair | Punctate | 1 | 2 | Nil |
| 12 | Central disc | Decompressive laminotomy + discectomy | Duragen™ | Small | 3 | 4 | Headache |
| 13 | Facet cyst | Decompressive laminectomy + excision facet cyst | Fat | Small | 3 | 6 | Headache/light-headedness |
| 14 | Central disc | Decompressive laminotomy + discectomy | Surgicel™ | Small | 2 | 4 | Headache/light-headedness |
Individual patient data
Small tear ≤0.5 cm
Large tear >0.5 cm
Punctate-pinpoint tear
Five patients with a dural tear (group 1) were excluded from the analysis. There were two patients with no pre-operative data, one who had since died of an unrelated cause, one who could not be contacted for long-term follow-up and one patient whose tear was primarily sutured. Group 1 thus consisted of seven males and seven females with a mean age of 50.8 years (range 31–69 years). Mean follow-up from surgery was 5.1 years (range 2–7 years). Outcome scores for the 14 patients in group 1 were compared to the control group of 14 patients in group 2. There were no complications in patients in group 2. Group 2 consisted of seven males and seven females with a mean age of 50.9 years (range 31–70 years). Mean follow-up from surgery was 4.9 years (range 2–7 years). Both groups of patients had similar pre-operative scores for the outcomes measured (Table 3) with no significant differences between them (P > 0.05).
Table 3.
Pre-operative mean scores in patients with dural tears and those without
| VB | VL | ODI | PF | RP | BP | GH | |
|---|---|---|---|---|---|---|---|
| Group 1 (tear) | 59 | 74 | 56 | 29 | 5.8 | 27 | 80 |
| Group 2 (no tear) | 55 | 67 | 46 | 47 | 7.5 | 27 | 95 |
| P value | 0.65 | 0.35 | 0.06 | 0.06 | 0.48 | 0.95 | 0.10 |
VB Visual Analogue Back Pain Score, VL Visual Analogue Leg Pain Score, ODI Oswestry Disability Index, PF physical functioning, RP role physical, BP bodily pain, GH general health
At 6-month follow-up, both groups had significant improvements in all outcomes measures except for the general health domain of the SF-36 (Table 4). All of these outcome measures continued to show significant improvement even at final follow-up (Table 4).
Table 4.
Mean scores pre-operative, 6-month and final follow-up in sampled patients
| Group 1 (dural tear) | Group 2 (no dural tear) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre op | 6/12 FU | P value | Final FU | P value | Pre op | 6/12 FU | P value | Final FU | P value | |
| VB | 59 | 26 | 0.006 | 29 | 0.004 | 55 | 18 | 0.003 | 29 | 0.012 |
| VL | 74 | 23 | 0.03 | 18 | 0.002 | 67 | 11 | 0.001 | 18 | 0.001 |
| ODI | 56 | 31 | 0.03 | 23 | 0.001 | 46 | 19 | 0.006 | 30 | 0.061 |
| PF | 29 | 80 | 0.01 | 82 | 0.001 | 47 | 82 | 0.004 | 86 | 0.001 |
| RP | 6 | 54 | 0.015 | 87 | 0.004 | 8 | 65 | 0.003 | 72 | 0.003 |
| BP | 27 | 63 | 0.009 | 79 | 0.001 | 27 | 85 | 0.001 | 81 | 0.001 |
| GH | 80 | 90 | 0.286 | 87 | 0.701 | 95 | 100 | 0.3 | 84 | 0.164 |
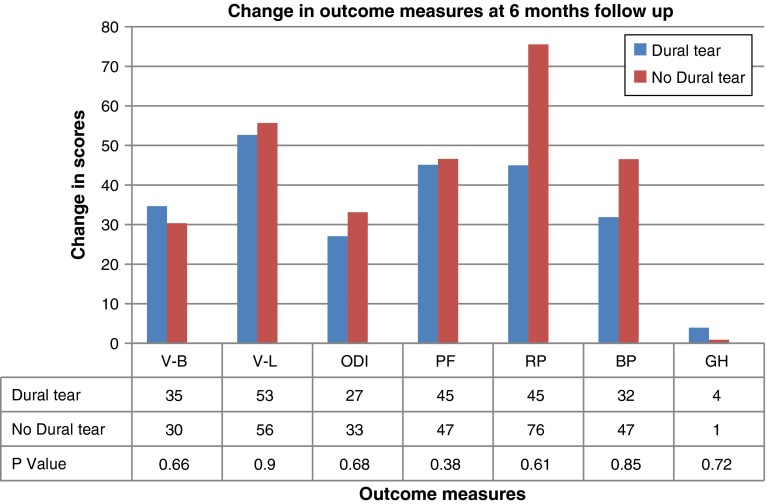
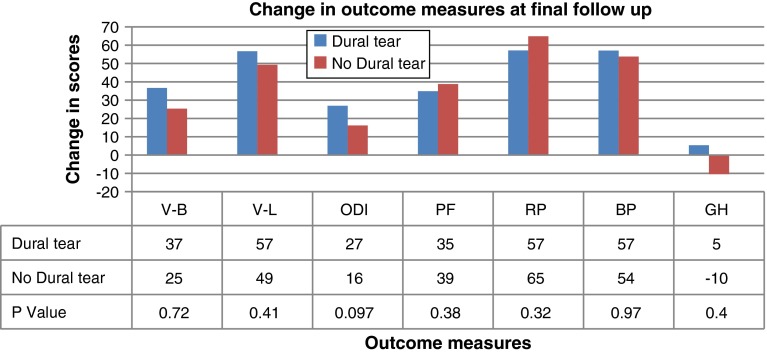
When assessing the change in scores between the two groups, there were some moderate differences at 6-month follow-up in the RP domain of the SF36. However, this was statistically insignificant as was the change in scores amongst the remainder of the outcome measures at 6-month and final follow-up (Figs. 1, 2). At final follow-up, patients with dural tears appeared to have better improvements in outcome measures amongst the VAB, VAL and ODI with similar scores in the SF-36 domains. However, these were not statistically significant (P > 0.05).
Fig. 1.
Change in outcome measures at 6 months
Fig. 2.
Change in outcome measures at final follow-up
Discussion
Generally, the gold standard for the management of a dural tear is accepted as primary suture repair. Other techniques have been employed to deal with the occurrence of a dural tear including the use of fat, muscle or facial grafts [7], use of fibrin glue [8], Surgicel™ as well as DuraGen™ collagen matrix [9]. The use of Surgicel™ in the management of incidental durotomies has previously been reported [10]. We are aware of case reports describing complications occurring in relation to leaving cellulose-based products such as Surgicel™ in wounds for the purposes of haemostasis [11] but we did not encounter any related complications in this study group. To the best of our knowledge, no other published series has evaluated the long-term outcome of patients sustaining a dural tear and being managed with non-suture repair methods. In our series, VB, VL and ODI scores were all improved at 6 months and this improvement was maintained at long-term follow-up regardless of whether a dural tear occurred at the time of surgery.
There is controversy as to whether incidental durotomy sustained during lumbar spine surgery compromises the long-term outcome for the patient. The majority of related studies are retrospective. In a series of 88 tears reported by Wang et al. [12], the authors found that if treated appropriately and successfully, incidental durotomy did not compromise the overall long-term result. A study by Jones et al. [3] of 450 patients with 17 dural tears reported similar results. Recent data from the Swedish spine registry [13] conclude that dural tears are a technical problem, that if dealt with appropriately at the time of surgery, do not compromise the results of discectomy at 1 year post-surgery. This is in contrast to a retrospective case matched study by Saxler et al. [6] of 41 patients with dural tears where the authors found a tendency to more re-operations, longer duration of inability to work and more back pain in those who had sustained a tear.
Traditionally, post-operative management of these patients has consisted of flat bed rest until the symptoms of posture-related headache, etc. have subsided [12]. However, more recently there have been proponents of early mobilisation of these patients following surgery [14, 15]. The small numbers of reports published appears to show that this is safe providing the tear has undergone formal surgical repair. Radcliff et al. [16] have recently reported an increased rate of medical complications in patients with bed rest >24 h as compared to those who were confined to bed for <24 h. Our patient group had a fairly short duration of posture-related symptoms and only a minor increase in duration of in-patient hospital stay. No significant medical complications occurred in any patient in either group.
Dural tears affecting the nerve root sleeve or axilla, or lying anteriorly, present a significant challenge to primary suture repair and anecdotally, therefore, are often managed without suture repair. Suturing the root sleeve may theoretically result in stenosis of the affected root, whilst another potential risk of suture repair is ‘lassoing’ of the underlying cauda equina roots. Reported failure rates for watertight suture repair range from 5 to 9 % [12, 14]. In addition, the pin holes created by passage of the suture needle may convert a low pressure dural defect to a high pressure defect resulting in persistent leakage and possibly accounting for the 5–9 % rate of persistent leakage [9, 17, 18].
Our study, therefore, suggests that a good outcome following lumbar decompressive surgery complicated by a dural tear can be maintained in the long-term without primary suture, and with a post-operative protocol of flat bed rest until posture-related symptoms have resolved.
Conflict of interest
None.
References
- 1.Eismont FJ, Wiesel SW, Rothman R. Treatment of dural tears associated with spinal surgery. JBJS (Am) 1981;63-A:1132–1136. [PubMed] [Google Scholar]
- 2.Finnegan W, Fenlin J, Marvel J, Nardini R, Rothman R. Results of surgical intervention in the symptomatic multiply-operated back patient. Analysis of 67 cases followed for 3 to 7 years. JBJS (Am) 1979;61-A:1077–1082. [PubMed] [Google Scholar]
- 3.Jones A, Stambough J, Balderston R, Rothman R, Booth R. Longterm results of lumbar spine surgery complicated by unintended incidental durotomy. Spine. 1989;14:443–446. doi: 10.1097/00007632-198904000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Kitchel S, Eismont F, Green B. Closed subarachnoid drainage for management of cerebrospinal fluid leakage after an operation on the spine. JBJS (Am) 1989;71-A:984–987. [PubMed] [Google Scholar]
- 5.Tafazal S, Sell P. Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J. 2005;14(3):287–290. doi: 10.1007/s00586-004-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saxler G, Kramer J, Barden B, Kurt A, Pfortner J, Bernsmann K. The longterm clinical sequelae of incidental durotomy in lumbar disc surgery. Spine. 2005;30(20):2298–2302. doi: 10.1097/01.brs.0000182131.44670.f7. [DOI] [PubMed] [Google Scholar]
- 7.Brookfield K, Randolph J, Eismont F, Brown M. Delayed symptoms of cerebrospinal fluid leak following lumbar decompression. Orthopaedics. 2008;31(8):816. doi: 10.3928/01477447-20080801-02. [DOI] [PubMed] [Google Scholar]
- 8.Bosacco SJ, Gardner BA, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery. Clin Orthop Relat Res. 2001;389:238–247. doi: 10.1097/00003086-200108000-00033. [DOI] [PubMed] [Google Scholar]
- 9.Narotam PK, Jose S, Nathoo N, Taylon C, Vora Y. Collagen matrix (DuraGen) in dural repair: analysis of a new modified technique. Spine. 2004;29(24):2861–2867. doi: 10.1097/01.brs.0000148049.69541.ad. [DOI] [PubMed] [Google Scholar]
- 10.Guerin P, et al. Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review. Injury. 2012;43(4):397–401. doi: 10.1016/j.injury.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 11.Szpalski M, Gunzburg R, Sztern B. An overview of blood-sparing techniques used in spine surgery during the perioperative period. Eur Spine J. 2004;13(Suppl 1):S18–S27. doi: 10.1007/s00586-004-0752-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty eight patients. JBJS (Am) 1998;80:1728–1732. doi: 10.2106/00004623-199812000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Stromqvist F, Jonsson B, Stromqvist B. Dural lesions in lumbar disc herniation surgery: incidence, risk factors and outcome. Eur Spine J. 2010;19:439–442. doi: 10.1007/s00586-009-1236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hodges SD, Humphreys SC, Eck JC, Covington LA. Management of incidental durotomy without mandatory bed rest. A retrospective review of 20 cases. Spine. 1999;24(19):2062–2064. doi: 10.1097/00007632-199910010-00017. [DOI] [PubMed] [Google Scholar]
- 15.Than KD, Wang AC, Etame AB, La Marca F, Park P. Postoperative management of incidental durotomy in minimally invasive lumbar spinal surgery. Minim Invasive Neurosurg. 2008;51(5):263–266. doi: 10.1055/s-0028-1082313. [DOI] [PubMed] [Google Scholar]
- 16.Radcliff KE, Sidhu GD, Kepler CK, Gruskay J, Anderson DG, Hilibrand A, Albert TJ, Vaccaro AR (2013) Complications of flat bedrest following incidental dural repair. J Spinal Disord Tech (Epub ahead of print)
- 17.Cammisa FP, Jr, Girardi FP, Sangani PK, et al. Incidental durotomy in spine surgery. Spine. 2000;25:2663–2667. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 18.Jankowitz BT, Atteberry DS, Gerszten PC, Karausky P, Cheng BC, Faught R, Welch WC. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J. 2009;18(8):1169–1174. doi: 10.1007/s00586-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]