Abstract
Purpose
The objective of this study was to evaluate the effects of an exercise program focusing on muscle stretching and endurance training on the 12-month incidence of low back pain (LBP) in office workers.
Methods
A 12-month prospective cluster-randomized controlled trial was conducted in healthy office workers with lower-than-normal trunk extension flexibility or trunk muscle endurance. Healthy office workers (n = 563) were randomly assigned at the cluster level into either intervention (n = 282) or control (n = 281) groups. Participants in the intervention group received an exercise program that included daily stretching exercise and twice-a-week muscle endurance training. Those in the control group received no intervention. The 12-month incidence of LBP was the primary outcome. Secondary outcome were pain intensity, disability level, and quality of life and health status. Analyses were performed using the Cox proportional hazard models.
Results
Over the 12-month follow-up, 8.8 % of participants in the intervention group and 19.7 % in the control group developed incidence of LBP. Hazard rate ratios showed a protective effect of the exercise program for LBP (HR = 0.37, 95 % CI 0.22–0.64) after adjusting for biopsychosocial factors. There was no significant difference in pain intensity, disability, and quality of life and health status between those who reported incidence of LBP in the intervention and control groups.
Conclusion
An exercise program consisting of muscle stretching and endurance training is an effective intervention to reduce incident LBP for office workers with lower-than-normal trunk extension flexibility or trunk muscle endurance.
Electronic supplementary material
The online version of this article (doi:10.1007/s00586-014-3212-3) contains supplementary material, which is available to authorized users.
Keywords: Musculoskeletal diseases, Exercise therapy, Disability, Sedentary lifestyle
Introduction
Evidence suggests that exercise therapy can prevent low back pain (LBP) [1]. However, different occupations are exposed to different working conditions and that the nature of the work influences the health of workers [2]. Implementing the same exercise regime for all those employed in differing occupations to prevent musculoskeletal disorders would be irrational. Office work is usually requires prolonged sitting posture. Lack of movement during sitting may induce the shortening of soft tissues, which consequently limits the available joint range of movement [3]. Limited joint movement may distort the normal body biomechanics and contributes to musculoskeletal disorders [4]. One previous study showed that female adolescents with LBP had lower lumbar mobility in all directions than normal subjects [5]. Stretching exercise can increase the range of joint movement and encourage circulation and oxygenation in joints, muscles, and muscle tendon units [3, 6].
Prolonged sitting requires the static contraction of postural muscles, which has been previously identified as a risk factor for musculoskeletal disorders [7]. Continuous low-intensity muscle contraction results in Ca2+ accumulation and homeostatic disturbances in the active muscles due to poor blood circulation and an impaired metabolic waste removal mechanism [8]. These pathological changes lead to microlesions, overuse injury, and pain due to insufficient recovery time [9]. Previous studies demonstrated that low back muscle endurance was an independent predictor of LBP in a working population [10] and muscle endurance training was effective for treating patients with subacute LBP [11]. The objective of this study was to evaluate the effect of an exercise program focusing on muscle stretching and endurance training on the 12-month incidence of LBP among office workers.
Methods
A prospective cluster-randomized controlled trial with 12-month follow-up was conducted. Subjects were included in the study if aged 18–55 years, working full-time, and with at least 1 year of experience in the current position. Subjects were excluded if they had reported spinal symptoms in the previous 6 months, reported pregnancy or had planned to become pregnant in the next 12 months, had a history of trauma or accidents in the spinal region, or had a history of spinal, intra-abdominal and femoral surgery in the previous 12 months. Subjects who had performed regular exercise or had been diagnosed with congenital anomaly of the spine, rheumatoid arthritis, infection of the spine and discs, ankylosing spondylitis, spondylolisthesis, spondylosis, tumor, systemic lupus erythymatosus, or osteoporosis were also excluded.
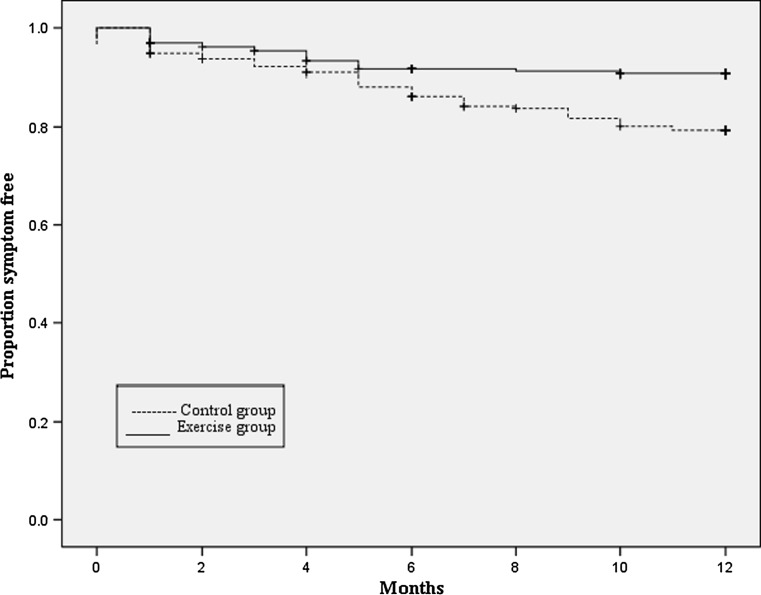
Office workers completed a self-administered questionnaire and receive a physical examination (Fig. 1). Only those who had lower-than-normal trunk extension movement or trunk muscle endurance were included in the study. Lower-than-normal cut-off points were set as previously reported mean scores. Participants were randomly assigned at the cluster level into either intervention or control groups. The designation of intervention was performed using computer-generated randomization and concealed from the data collector. Clusters of participants were located in the same workplaces to avoid contamination of the intervention and to enhance the compliance within the intervention group. A total of 12 clusters (6 clusters for the intervention group and 6 clusters for the control group) were identified and cluster size ranged from 8 to 79 participants. The study was approved by the University Human Ethics Committee and no change was made to methods after trial commencement.
Fig. 1.
CONSORT flowchart of the study
The self-administered questionnaire was used to gather data on individual, work-related physical and psychosocial factors. Individual factors included gender, age, marital status, educational level, frequency of regular exercise or sport, smoking habits, and number of driving hours a day. Work-related physical factors included current job position, number of working hours, and years of working experience. Respondents were asked about the frequency of using a computer, performing various activities during work, and rest breaks. The questionnaire also asked respondents to self-rate the ergonomics of their workstations (desk, chair, and position of monitor) and work environment conditions (ambient temperature, noise level, light intensity, and air circulation). Psychosocial factors were measured by the Job Content Questionnaire [12].
Each participant underwent a physical examination according to standardized protocol and the examiner was blinded to the identity of group assignments.
Waist circumference.
Trunk extension flexibility was assessed by the modified–modified Schöber test. Mean normal range of trunk extension flexibility is 13.2 cm [13]. A low score of the test indicates high flexibility of trunk.
Erector spinae and Multifidus muscle endurance was assessed by the Biering-Sörensen test. An ability to sustain a position for 132 s was considered normal muscle endurance [14].
Transversus abdominis muscle endurance was assessed by the Transversus abdominis isolation test [15]. An ability to repeatedly contract the muscles 10 times was considered normal muscle endurance [15].
Quadratus lumborum muscle endurance was assessed by the Side bridge test. An ability to sustain a position for 51 (for males) or 35 (for females) seconds was considered normal muscle endurance [16].
Intervention
Participants in the intervention group received an exercise program, based on the theoretical effect of prolonged sitting causing pelvic backward rotation and reduced lumbar lordosis [9]. The exercise program consisted of muscle stretching and endurance training (see electronic supplementary material). The stretching exercise was designed to stretch the shortened muscle (i.e. iliopsoas). Participants hold the muscle in the stretched position for 30 s once and perform twice each workday at 10 a.m. and 2 p.m. [3]. The endurance training was designed to increase endurance of the lengthened muscles (i.e. erector spinae, multifidus, quadratus lumborum and transversus abdominis) [4]. Participants repeatedly contracted each muscle 10 times and rested 60 s between muscles. Participants performed the exercise twice a week at home on Wednesday and Sunday. Participants received a short message via mobile phone at 10 a.m. daily on a workday during the first 3 months to remind them to perform the exercise. Participants in the control group did not participate in any exercise program.
The effectiveness of the exercise program on trunk movement and trunk muscle endurance was assessed on 40 subjects, who were randomly selected from both the intervention (n = 20) and control (n = 20) groups. Assessments of trunk extension flexibility and trunk muscle endurance were conducted at baseline, and 3-, 6-, 9- and 12-month follow-ups.
Outcome measures
The incidence of LBP was collected using a diary. The area of the lower back was defined according to the standardized Nordic questionnaire. Participants answered the yes/no question “Have you experienced any low back pain lasting > 24 h during the past month?” If they answered “Yes”, follow-up questions about pain intensity measured by a VAS, and the presence of weakness or numbness in the lower limbs were asked. In this study, participants were identified as cases if they answered “Yes” to the first question, reported pain intensity greater than 30 mm on a 100-mm VAS, and had no weakness or numbness in the lower limbs. The diaries were collected from participants every month over a 12-month period. Those who reported incidence of LBP were asked about their disability level measured by the RMDQ [17] and quality of life and health status measured by the Medical Outcome Study Short-Form Survey version 2.0 (SF36v2) [18].
Statistical analysis
The analysis followed an intention-to-treat approach. The study was designed to have 80 % power to show a 10 % difference in the incidence rate of LBP at the one-sided 5 % level between those who received the exercise program and those who did not. The incidence of LBP was expected to be 23 %.
To determine whether trunk movement and trunk muscle endurance varied over time, one-way analysis of variance (ANOVA) was performed on the intervention and control groups separately. Tukey post hoc comparison was employed to determine whether the two selected means were significantly different from each other. Comparisons of trunk movement and trunk muscle endurance between the intervention and control groups at each time point were conducted using the independent t test.
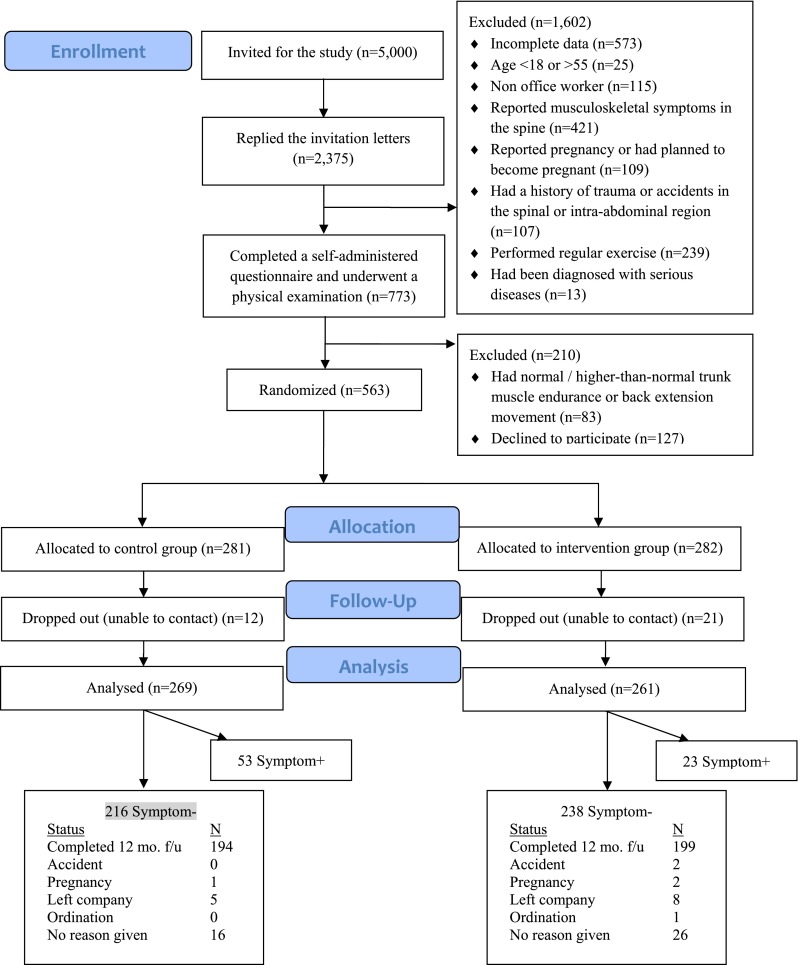
Kaplan–Meier survival curves and relative risks for the intervention and control groups were calculated using survival analysis methodology. Survival time was taken as the time to incident symptoms. Those participants who left the study without manifesting the outcome were censored at the time they left. The two survival curves generated by the Kaplan–Meier method were compared using the log rank test.
The Cox proportional hazards model was used to calculate hazard ratios for the intervention with respect to incident cases for LBP. The covariates of age, gender and psychological scores were forced into all models to reduce confounding due to these factors. The other 45 possible covariates were each examined in multivariate models. If a tested covariate changed the hazard ratio of the intervention variable by 0.05 or more, it was included in the final, adjusted model. The clinical measure of numbers needed to treat was also calculated.
Difference in health outcomes between those reporting incidence of LBP in the intervention and control groups were analyzed using independent t tests. All statistical analyses were performed using SPSS statistical software, version 17.0 (SPSS Inc, Chicago, IL, USA). Statistical significance was set at the 5 % level.
Results
The trial started in February 2011 and concluded in March 2013. Figure 1 shows the flow of participants. After randomization, 33 dropped out of the study and the reason given for dropping out was job change (n = 15) and insufficient time to exercise (n = 18). Table 1 shows the baseline characteristics of the participants in both groups. The mean (SD) of stretching exercise adherence was 149.8 (143.0) sessions, accounting for 31 % of full exercise adherence. The mean (SD) of endurance training adherence was between 53.1 (64.4) and 54.9 (64.9) sessions, accounting for 55–57 % of full exercise adherence (Table 2).
Table 1.
Baseline characteristics of participants
| Characteristic | Mean ± SD | p value | |
|---|---|---|---|
| Intervention group (n = 282) | Control group (n = 281) | ||
| Demographic characteristic | |||
| Gender: female (%) | 65.1 | 72.8 | 0.054 |
| Age (years) | 37.3 ± 10.1 | 36.9 ± 10.7 | 0.711 |
| Weight (kg) | 62.1 ± 14.3 | 60.3 ± 13.1 | 0.117 |
| Height (cm) | 160.9 ± 8.5 | 160.9 ± 7.4 | 0.989 |
| Waist circumference (cm) | 80.6 ± 13.1 | 77.7 ± 12.2 | 0.009* |
| Education (%) | 0.424 | ||
| Lower than Bachelor’s degree | 11.7 | 9.1 | |
| Bachelor’s degree | 69.0 | 72.0 | |
| Higher than Bachelor’s degree | 19.3 | 18.9 | |
| Exercise frequency in the past 12 months (%) | 0.080 | ||
| Never | 25.0 | 18.5 | |
| Occasionally | 61.8 | 68.5 | |
| Regularly | 12.5 | 10.5 | |
| Not sure | 0.7 | 2.5 | |
| Occupational-related characteristic | |||
| Duration of employment (years) | 12.1 ± 9.2 | 12.5 ± 10.5 | 0.636 |
| Working hours per day (hours per day) | 7.8 ± 2.2 | 8.0 ± 3.2 | 0.458 |
| Working days per week (days per week) | 5.0 ± 0.3 | 4.9 ± 0.6 | 0.007* |
| Psychosocial characteristic | |||
| Job control | 35.5 ± 4.5 | 34.9 ± 4.7 | 0.122 |
| Psychological job demand | 31.9 ± 4.3 | 31.8 ± 4.4 | 0.777 |
| Physical job demand | 12.9 ± 2.5 | 13.2 ± 2.4 | 0.306 |
| Job security | 16.7 ± 1.3 | 16.6 ± 2.3 | 0.454 |
| Social support | 30.2 ± 4.6 | 31.2 ± 4.4 | 0.040* |
| Hazard at work | 16.2 ± 3.7 | 16.3 ± 3.5 | 0.724 |
| Physical characteristic | |||
| Trunk extension flexibility (cm) | 13.1 ± 0.8 | 13.3 ± 0.8 | 0.003* |
| Erector spinae and multifidus endurance (s) | 80.8 ± 39.1 | 79.4 ± 39.7 | 0.685 |
| TrA endurance (times) | 4.4 ± 4.1 | 4.6 ± 4.1 | 0.610 |
| Rt. quadratus lumborum endurance (s) | 46.2 ± 27.4 | 46.0 ± 1.9 | 0.932 |
| Lt. quadratus lumborum endurance (s) | 45.9 ± 27.3 | 44.2 ± 31.6 | 0.481 |
* p value < 0.05
Table 2.
Mean number of training sessions and adherence percentage ratios among office workers in the intervention group
| 1–3 month | 4–12 month | 1–12 month | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD | % | n | Mean ± SD | % | n | Mean ± SD | % | |
| Stretching exercise | 120 | 100 | 360 | 100 | 480 | 100 | |||
| Iliopsoas | 195 | 53.6 ± 43.6 | 44.7 | 175 | 129.1 ± 114.0 | 35.9 | 218 | 149.8 ± 143.0 | 31.2 |
| Endurance exercise | 24 | 100 | 72 | 100 | 96 | 100 | |||
| Erector spinae and multifidus | 157 | 18.6 ± 20.8 | 77.5 | 149 | 47.0 ± 52.3 | 65.3 | 187 | 53.1 ± 64.4 | 55.3 |
| Transversus abdominis | 161 | 18.8 ± 21.2 | 78.3 | 152 | 47.9 ± 52.3 | 66.5 | 188 | 54.9 ± 64.9 | 57.2 |
| Quadratus lumborum | 160 | 18.2 ± 20.6 | 75.5 | 150 | 47.5 ± 52.5 | 65.0 | 189 | 53.1 ± 64.6 | 55.3 |
One-way ANOVA indicated a significant effect of time on trunk extension flexibility in both intervention (F4,95 = 2.983, p = 0.023) and control (F4,95 = 4.665, p = 0.002) groups (Table 3). The post hoc Tukey test revealed that trunk extension flexibility at baseline was significantly different from the 6-month and the 9-month follow-ups in the control group and 12-month follow-up in the intervention group (p < 0.05). Comparison of trunk extension flexibility between the intervention and control groups at baseline showed no significant difference (p = 0.565). Trunk extension flexibility in the intervention group was significantly different from the control group at the 3-, 6-, 9-, and 12-month follow-ups (p < 0.05).
Table 3.
Trunk extension flexibility and trunk muscles endurance at baseline, 3-, 6-, 9- and 12-month follow ups for the intervention and control groups
| Mean ± SD | p value | ||
|---|---|---|---|
| Intervention group (n = 20) | Control group (n = 20) | ||
| Trunk extension flexibility (cm) | |||
| Baseline | 12.9 ± 0.7 | 13.0 ± 0.8 | 0.565 |
| 3-month | 12.4 ± 0.7 | 13.5 ± 0.6 | <0.001* |
| 6-month | 12.7 ± 0.7 | 13.7 ± 0.5 | <0.001* |
| 9-month | 12.5 ± 0.5 | 13.7 ± 0.5 | <0.001* |
| 12-month | 12.3 ± 0.5 | 13.1 ± 0.9 | 0.002* |
| Erector spinae and multifidus endurance (s) | |||
| Baseline | 57.6 ± 14.8 | 55.2 ± 20.2 | 0.670 |
| 3-month | 66.9 ± 19.9 | 54.1 ± 24.6 | 0.080 |
| 6-month | 72.6 ± 19.9 | 67.8 ± 30.5 | 0.558 |
| 9-month | 70.7 ± 28.2 | 67.8 ± 30.0 | 0.757 |
| 12-month | 75.0 ± 29.9 | 70.5 ± 23.2 | 0.618 |
| Transversus abdominis endurance (times) | |||
| Baseline | 5.8 ± 4.2 | 5.5 ± 4.5 | 0.800 |
| 3-month | 6.8 ± 3.8 | 6.3 ± 3.8 | 0.651 |
| 6-month | 7.6 ± 2.7 | 7.2 ± 3.1 | 0.627 |
| 9-month | 8.0 ± 2.9 | 7.2 ± 3.2 | 0.372 |
| 12-month | 8.7 ± 2.2 | 7.5 ± 3.2 | 0.180 |
| Right Quadratus lumborum endurance (s) | |||
| Baseline | 33.0 ± 13.3 | 42.5 ± 33.6 | 0.247 |
| 3-month | 35.2 ± 16.5 | 37.6 ± 25.8 | 0.732 |
| 6-month | 33.8 ± 15.9 | 36.6 ± 20.2 | 0.632 |
| 9-month | 36.1 ± 15.3 | 37.1 ± 20.8 | 0.859 |
| 12-month | 41.3 ± 13.8 | 39.4 ± 27.5 | 0.785 |
| Left Quadratus lumborum endurance (s) | |||
| Baseline | 35.1 ± 12.0 | 40.1 ± 28.4 | 0.477 |
| 3-month | 34.5 ± 15.2 | 37.2 ± 24.1 | 0.677 |
| 6-month | 32.9 ± 13.8 | 36.2 ± 18.2 | 0.532 |
| 9-month | 38.1 ± 17.5 | 36.6 ± 19.5 | 0.800 |
| 12-month | 44.3 ± 12.4 | 37.4 ± 26.0 | 0.287 |
* p value < 0.05
One-way ANOVA indicated no significant effect of time on trunk muscle endurance in both intervention (TrA.;F4,95 = 2.343, p = 0.060, Rt. Quadatus lumborum; F4,95 = 0.959, p = 0.434, Lt. Quadatus lumborum; F4,95 = 2.003, p = 0.100, Erector spinae and multifidus; F4,95 = 1.607, p = 0.179) and control (TrA.;F4,95 = 1.108, p = 0.357, Rt. Quadatus lumborum; F4,95 = 0.173, p = 0.952, Lt. Quadatus lumborum; F4,95 = 0.081, p = 0.988, Erector spinae and multifidus; F4,95 = 1.798, p = 0.136) groups. Comparison of trunk muscle endurance between the intervention and control groups at baseline, 3-, 6-, 9-, and 12-month follow ups showed no significant difference (p > 0.05).
Over the 12-month follow up, 8.8 % (23/261) of participants in the intervention group and 19.7 % (53/269) of participants in the control group reported the incidence of LBP. No harm or unintended effect in both groups was reported. The Kaplan–Meier survival curves for the low back cohort showed that there was a significant difference in time to LBP between the intervention and control groups (log rank test probability = 0.001) (Fig. 2). Using the Cox proportional hazard model, a protective effect of the exercise program was found for LBP, in which the exercise program significantly reduced the risk of incidence of LBP by 60 % (HR = 0.37, 95 % CI 0.22–0.64) (Table 4). The number needed to treat was nine (95 % CI 6–20), i.e. for every nine participants who received the exercise program to prevent incident LBP in one participant.
Fig. 2.
The Kaplan–Meier survival curves for low back cohort
Table 4.
Unadjusted and adjusted hazard ratios evaluating the effects of exercise program on incident low back pain (n = 530)
| Hazard ratioa | 95 % CI | p value | |
|---|---|---|---|
| Unadjusted model | 0.44 | 0.27–0.72 | 0.001 |
| Adjusted modelb | 0.37 | 0.22–0.64 | <0.001 |
aCox proportional hazard ratio; the control group is the reference group
bVariable; age, gender, job control, psychological job demand, physical job demand, job security, social support and hazard at work
There was no significant difference in the health outcomes (i.e. pain intensity, disability, physical health and mental health) reported by those having LBP in the intervention and control groups (Table 5).
Table 5.
Pain intensity, disability, and SF-36 physical and mental component summaries
| Variable | Mean ± SD | p value | |
|---|---|---|---|
| Intervention group | Control group | ||
| Pain intensity measured by VAS | 4.7 ± 1.5 | 4.6 ± 1.4 | 0.762 |
| Disability measured by RMDQ | 3.6 ± 4.8 | 3.4 ± 3.1 | 0.849 |
| SF-36 physical component summary | 36.1 ± 8.8 | 33.2 ± 9.6 | 0.262 |
| SF-36 mental component summary | 22.7 ± 6.7 | 22.2 ± 6.7 | 0.788 |
Discussion
Office work usually involves computer use and document work for long hours, which requires prolonged sitting. Deconditioning from prolonged sitting may lead to a reduction in joint mobility and muscle endurance. Evidence suggests that poor lumbar mobility and muscle endurance are risk factors for LBP [5, 10]. A distinct group of healthy participants was selected for the present study, i.e. those with poor trunk extension flexibility or trunk muscle endurance because they were office workers with high risk of LBP and will theoretically benefit from the exercise program. The results revealed that an exercise program reduced incidence of LBP in healthy office workers by 60 %. However, the exercise program provided no benefit for reduction of pain intensity and disability or maintenance of the quality of life and health status in those performing the exercises and who, subsequently, experienced LBP.
Previously, Moore et al. [19] found that an exercise program focusing on balance control and low-back-connected muscle strength training prevented LBP in sedentary healthy workers. Hamberg-van Reenen et al. [20] reported that workers on an 8-week resistance training program performed the lifting tasks for a longer time before reporting considerable discomfort than those in the control group. However, Andersen et al. [21] found that all-round physical exercise did not provide a greater preventive effect on LBP than a reference intervention among office workers.
The effectiveness of exercise for patients with chronic LBP depends on their exercise adherence [22]. The results showed that participants’ adherence to the exercise program was quite low (31 % for stretching exercise and 55–57 % for endurance training). Other studies investigating the effectiveness of exercise programs have had similar issues with exercise adherence [23, 24]. Despite low to moderate participant adherence to exercise program, we found that it was sufficient to significantly increase trunk extension flexibility compared to the control group over the 12-month period. For endurance training, the results also indicated improved muscle endurance in all muscles over the 12-month period in the intervention group. Although TrA, erector spinae, and multifidus muscle endurance in the control group improved over time, the magnitude of improvement seen in the intervention group was greater than in the control group. The lack of statistical significance may be the result of insufficient power to detect the effect because of the large variability of scores. Therefore, a reduction in incidence of LBP among office workers in the intervention group can partly be attributed to the exercise program.
The results showed no significant difference in pain intensity, disability as well as quality of life and health status between the intervention and control groups. The findings imply that effective intervention for prevention of LBP in office workers may differ from those for reduction of disability due to LBP. A recent review of international clinical guidelines for the management of LBP indicated that a supervised exercise program is not recommended for acute LBP. However, exercise therapy is recommended for subacute and chronic LBP but there is no evidence that one form of exercise is superior to another [25]. Further research should evaluate which type of exercise is most appropriate to treat subacute and chronic LBP.
This study proposed an exercise program, which is easy to implement and cost-effective, to prevent LBP in office worker with lower-than-normal trunk extension flexibility or trunk muscle endurance. The exercise program is simple, only requiring a brochure describing the exercises with some advice from a health care professional. It can be carried out within a short space of time: 1–2 min per session twice a day at the workplace for stretching exercise and 6–8 min per session twice a week at home for endurance training. Additionally, the exercise program costs little money as it only requires a brochure, brief training from a health care professional, and a daily short message reminder via mobile phone.
Three main methodological limitations should be taken into consideration when interpreting the results of the present study. First, the present study was conducted in healthy and physically active office workers with lower-than-normal trunk extension flexibility or trunk muscle endurance. Thus, extrapolation of these results to other populations should be made with caution. Further research on the effects of an exercise program focusing on muscle stretching and endurance training on the incidence of LBP in other occupations is suggested. Second, there was no blinding of all participants to treatment allocation. Participant blinding ensures that the apparent effect (or lack of effect) of treatment is not due to the placebo effect or Hawthorne effect. However, it is not possible to blind participants in an exercise-related trial. One strategy that could be conducted to minimize the expectation bias of participants is to set a trial in which at least two exercise interventions are compared and ensure that the interventions are equally credible and acceptable to participants and that participants have limited experience or expectations of either exercise intervention. Third, the nature of several biopsychosocial factors and the diagnosis of LBP were subjective, which may have led to data inaccuracy. The important drawback of self-reported data is a risk of overestimation of exposure. Also, some workers may be more sensitive to any somatic disturbance than others. As a result, there is a risk of under- or over-reporting of the incidence. Future studies should consider inclusion of objective information from a physical examination to increase data accuracy.
Electronic supplementary material
Acknowledgments
This work was funded by the Social Security Office of Thailand (Grant No. 002/2553) and Chulalongkorn University Centenary Academic Development Project (#12).
Conflict of interest
None.
References
- 1.Henchoz Y, Kai-Lik So A. Exercise and nonspecific low back pain: a literature review. Jt Bone Spine. 2008;75:533–539. doi: 10.1016/j.jbspin.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Cote P, van der Velde G, Cassidy JD, Carroll LJ, Hogg-Johnson S, Holm LW, Carragee EJ, Haldeman S, Nordin M, Hurwitz EL, Guzman J, Peloso PM. The burden and determinants of neck pain in workers: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. J Manip Physiol Ther. 2009;32:S70–S86. doi: 10.1016/j.jmpt.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 3.Armiger P, Martyn M. Stretching for function flexibility. Philadelphia: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 4.Oatis CA. Kinesiology: the mechanics & pathomechanics of human movement. 2. Philadelphia: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 5.Peltonen JE, Taimela S, Erkintalo M, Salminen JJ, Oksanen A, Kujala UM. Back extensor and psoas muscle cross-sectional area, prior physical training, and trunk muscle strength—a longitudinal study in adolescent girls. Eur J Appl Physiol Occup Physiol. 1998;77:66–71. doi: 10.1007/s004210050301. [DOI] [PubMed] [Google Scholar]
- 6.Norris C, Matthews M. The role of an integrated back stability program in patients with chronic low back pain. Complement Ther Clin Pract. 2008;14:255–263. doi: 10.1016/j.ctcp.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 7.da Costa BR, Vieira ER. Stretching to reduce work-related musculoskeletal disorders: a systematic review. J Rehabil Med. 2008;40:321–328. doi: 10.2340/16501977-0204. [DOI] [PubMed] [Google Scholar]
- 8.Visser B, van Dieen JH. Pathophysiology of upper extremity muscle disorders. J Electromyogr Kinesiol. 2006;16:1–16. doi: 10.1016/j.jelekin.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Wilson A. Effective management of musculoskeletal injury. A clinical ergonomics approach to prevention, treatment and rehabilitation. Edinburgh: Churchill Livingstone; 2002. [Google Scholar]
- 10.Hamberg-van Reenee H, Ariens G, Blatter B, Twisk J, van Mechelen W, Bongers P. Physical capacity in relation to low back, neck, or shoulder pain in a working population. Occup Environ Med. 2006;63:371–377. doi: 10.1136/oem.2006.026914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chok B, Lee R, Latimer J, Tan SB. Endurance training of the trunk extensor muscles in people with subacute low back pain. Phys Ther. 1999;79:1032–1042. [PubMed] [Google Scholar]
- 12.Phakthongsuk P. Construct validity of the Thai version of the job content questionnaire in a large population of heterogeneous occupations. J Med Assoc Thai. 2009;92:564–572. [PubMed] [Google Scholar]
- 13.Henchoz Y, de Goumoens P, So AK, Paillex R. Functional multidisciplinary rehabilitation versus outpatient physiotherapy for non specific low back pain: randomized controlled trial. Swiss Med Wkly. 2010;140:13133. doi: 10.4414/smw.2010.13133. [DOI] [PubMed] [Google Scholar]
- 14.Latimer J, Maher CG, Refshauge K, Colaco I. The reliability and validity of the Biering-Sorensen test in asymptomatic subjects and subjects reporting current or previous nonspecific low back pain. Spine. 1999;24:2085–2089. doi: 10.1097/00007632-199910150-00004. [DOI] [PubMed] [Google Scholar]
- 15.Richardson CA, Jull G, Hodges P, Hides J. Therapeutic exercise for spine segmental stabilization in low back pain: scientific basis and clinical approach. London: Churchill Livingstone; 1999. [Google Scholar]
- 16.Doymaz F, Cavlak U. Relationship between thigh skinfold measurement, hand grip strength, and trunk muscle endurance: differences between the sexes. Adv Ther. 2007;24:1192–1201. doi: 10.1007/BF02877765. [DOI] [PubMed] [Google Scholar]
- 17.Pensri P, Baxtex G, McDonough S. Reliability and internal consistency of the Thai version of Roland-Morris Disability Questionnaire and Waddell Disability Index for back pain patients. Chula Med J. 2005;49:333–349. [Google Scholar]
- 18.Jirarattanaphochai K, Jung S, Sumananont C, Saengnipanthkul S. Reliability of the medical outcomes study short-form survey version 2.0 (Thai version) for the evaluation of low back pain patients. J Med Assoc Thai. 2005;88:1355–1361. [PubMed] [Google Scholar]
- 19.Moore C, Holland J, Shaib F, Ceridan E, Schonard C, Marasa M. Prevention of low back pain in sedentary healthy workers: a pilot study. Am J Med Sci. 2012;344:90–95. doi: 10.1097/MAJ.0b013e3182364942. [DOI] [PubMed] [Google Scholar]
- 20.Hamberg-van Reenen HH, Visser B, van der Beek AJ, Blatter BM, van Dieen JH, van Mechelen W. The effect of a resistance-training program on muscle strength, physical workload, muscle fatigue and musculoskeletal discomfort: an experiment. Appl Ergon. 2009;40:396–403. doi: 10.1016/j.apergo.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 21.Andersen LL, Christensen KB, Holtermann A, Poulsen OM, Sjogaard G, Pedersen MT, Hensen EA. Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: a 1-year randomized controlled trial. Man Ther. 2010;15:100–104. doi: 10.1016/j.math.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Shirado O, Ito T, Kikumoto T, Takeda N, Minami A, Strax TE. A novel back school using a multidisciplinary team approach featuring quantitative functional evaluation and therapeutic exercises for patients with chronic low back pain: the Japanese experience in the general setting. Spine. 2005;30:1219–1225. doi: 10.1097/01.brs.0000162279.94779.05. [DOI] [PubMed] [Google Scholar]
- 23.Escolar-Reina P, Medina-Mirapeix F, Gascon-Canovas JJ, Montilla-Herrador J, Jimeno-Serrano FJ, de Oliveira Sousa SL, del Bano-Aledo ME, Lomass-Vega R. How do care-provider and home exercise program characteristics affect patient adherence in chronic neck and back pain: a qualitative study. BMC Health Serv Res. 2010;10:60. doi: 10.1186/1472-6963-10-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ryan CG, Gray HG, Newton M, Granat MH. Pain biology education and exercise classes compared to pain biology education alone for individuals with chronic low back pain: a pilot randomised controlled trial. Man Ther. 2010;15:382–387. doi: 10.1016/j.math.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 25.Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19:2075–2094. doi: 10.1007/s00586-010-1502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.