Abstract
Purpose
The aim of this study is to evaluate the prevalence and severity of low back pain (LBP) and the influence of sciatica and neurological deficits in old men.
Material and method
Mister osteoporosis Sweden includes 3,014 community-dwelling men aged 69–81 years. At study start 3,009 participants answered questions on LBP, low back pain and sciatica (LBP + SCI) or low back pain and sciatica with associated neurological deficits (LBP + SCI + NEU) during the preceding 12 months. Data are presented as proportions or medians with mid-quartile ranges. Differences between groups were tested by χ2 test and Kruskall-Wallis test.
Results
24 % had experienced LBP without SCI, 8 % LBP + SCI and 14 % LBP + SCI + NEU. 10 % of the men with LBP, 22 % of those with LBP + SCI, and 36 % of those with LBP + SCI + NEU rated the pain as severe (p < 0.001). 23 % of the men with LBP, 31 % of those with LBP + SCI and 50 % of those with LBP + SCI + NEU reported limitation in activity of daily living (ADL) (p < 0.001). Men with only LBP had to restrict their activities for 7 days (3–14), those with LBP + SCI 6 days (2–14) and those with LBP + SCI + NEU 10 days (3–30) (p < 0.05).
Conclusions
The 1-year prevalence of LBP in community living men aged 69–81 years was close to 50 % but for individuals with LBP or LBP + SCI the morbidity was low with more than two-thirds having no limitations in ADL. In men with LBP + SCI + NEU more than one-third rated the pain as severe and close to half had limitations in ADL.
Keywords: Elderly men, Epidemiology, Low back pain, Neurological deficits, Sciatica
Introduction
Low back pain (LBP) is one of the most common musculoskeletal disorders [1–3]. A recent review infers the prevalence of LBP to be highest in middle-aged adults and in women [4]. Another report suggests that LBP is more frequent and with longer episodes in old than in young adults [5]. Since both the number and proportion of individuals older than 65 years are increasing in most western populations [6] it seems reasonable to assume that LBP will result in an even greater health care burden in the future [7].
The prevalence and severity of LBP in old men are not thoroughly evaluated [8] and the clinical influence of sciatica and neurological deficits on disability is unclear. Activity of daily living (ADL) is often used to describe functional status but the association between LBP, sciatica, neurological deficits and ADL has in old men yet to be determined. We therefore designed a cross-sectional study in a population-based sample of community living old men with the aim to estimate the one-year prevalence of LBP, sciatica and neurological deficits and to quantify the resulting pain and limitations in ADL. Our research questions were: In old men, (a) what is the one-year prevalence of LBP, sciatica and neurological deficits? (b) do these symptoms result in severe pain and deterioration in ADL?
Materials and methods
Mister osteoporosis (MrOs) Sweden is a multicentre prospective observational study of 3,014 men aged 69–81 years enrolled in Malmö, Gothenburg and Uppsala with the primary aim to evaluate risk factors for osteoporosis and fractures. The men were randomly selected from the national population register and had to be able to walk with or without a cane or a stick but without assistance by another person and could not have bilateral hip replacements to be eligible for participation. The attendance rate was 45 %. The study population has been described in detail in previous publications [9, 10].
At baseline all participants were asked to answer a questionnaire on pain history during the preceding 12 months. As 5 men did not answer these questions, this report includes 3,009 men. There were specific questions regarding LBP and associated symptoms of sciatica and neurological deficits including severity of pain and limitations in ADL (Tables 1, 2). The severity of pain is in the questionnaire graded as mild, moderate and severe and is based on the subjective experience of the participant. We stratified the men in four groups depending on pain history during the preceding 12 months: (a) men without LBP; (b) men with LBP but without sciatica; (c) men with LBP and sciatica but without neurological deficits (LBP + SCI); and (d) men with LBP, sciatica and neurological deficits (LBP + SCI + NEU). LBP was defined as pain in the lower back, SCI as pain emerging from the lower back with radiation to the lower extremity below the buttocks, (without any distinction on pain above or below the knee), and NEU as subjective sensory symptoms in the lower extremity such as tingling and/or sensory deficits and/or motor symptoms such as subjective weakness or paresis in the lower extremity.
Table 1.
Distribution of low back pain (LBP), sciatica (SCI) and neurological deficits (NEU) during 12 months year in 3,009 men aged 69–81 years stratified by age
| Age groups (years) | All men | 69–72 | 73–75 | 76–78 | 79–81 |
|---|---|---|---|---|---|
| LBP without radiating pain to lower extremity | 730 (24.3 %) | 152 (23.7 %) | 214 (23.5 %) | 175 (24.7 %) | 189 (25.3 %) |
| LBP with radiating pain to lower extremity but no neurological symptoms | 226 (7.5 %) | 60 (9.3 %) | 72 (7.9 %) | 50 (7.1 %) | 44 (5.9 %) |
| LBP with radiating pain to lower extremity and only sensory symptoms | 102 (3.4 %) | 20 (3.1 %) | 32 (3.5 %) | 27 (3.8 %) | 23 (3.1 %) |
| LBP with radiating pain to lower extremity and only motor symptoms | 68 (2.3 %) | 16 (2.5 %) | 18 (2.0 %) | 17 (2.4 %) | 17 (2.3 %) |
| LBP with radiating pain to lower extremity and both sensory and motor symptoms | 236 (7.8 %) | 54 (8.4 %) | 68 (7.5 %) | 54 (7.6 %) | 60 (8.0 %) |
| No LBP | 1,647 (54.7 %) | 340 (53.0 %) | 508 (55.7 %) | 385 (54.4 %) | 414 (55.4 %) |
| Total | 3,009 (100 %) | 642 (100 %) | 912 (100 %) | 708 (100 %) | 747 (100 %) |
Data are presented as number and proportion (%). There were no significant differences in distribution between the age strata (p = 0.88)
Table 2.
Severity of low back pain (LBP) and sciatica (SCI) and limitations in activity of daily living (ADL) in men aged 69–81 with LBP, with LBP and sciatica (LBP + SCI) and with LBP + ISC and neurological deficits (LBP + SCI + NEU) in the lower extremity
| Groups | p value for group comparisons | |||
|---|---|---|---|---|
| LBP (n = 730) | LBP + ISC (n = 226) | LBP + ISC + NEU (n = 406) | ||
| Subjectively rated severity of LBP or sciatica | ||||
| Slight | 45.1 % | 30.5 % | 17.7 % | |
| Moderate | 44.9 % | 46.9 % | 45.6 % | <0.001 |
| Severe | 9.7 % | 22.1 % | 36.0 % | |
| Limitations in activity of daily living (ADL) | ||||
| Any limitations due to LBP | 23.3 % | 30.5 % | 50.2 % | <0.001 |
| Difficulty bending down to pick up light objects | 16.4 % | 19.9 % | 33.7 % | <0.05 |
| Difficulty lifting a 5 kg object from the floor | 6.3 % | 8.0 % | 21.7 % | <0.001 |
| Difficulty putting socks on either foot | 10.4 % | 17.7 % | 29.8 % | <0.001 |
| Difficulty getting in or out of front seat of a car | 11.0 % | 13.7 % | 27.8 % | <0.01 |
| Difficulty standing or walking for 2 h | 16.2 % | 18.1 % | 33.3 % | 0.06 |
| Difficulty sitting in a chair for 30 min without standing | 7.8 % | 12.4 % | 19.7 % | 0.35 |
| Forced to lay down at least half of the day due to LBP | 8.7 % | 11.1 % | 17.0 % | <0.97 |
| Partly bedridden due to pain (days) | 0 (0–2) | 0 (0–2) | 0 (0–5) | 0.96 |
| Had to restrict daily activities due to the disability (days) | 7 (3–14) | 6 (2–14) | 10 (3–30) | <0.01 |
Data are presented as proportions (%) or medians with mid-quartile ranges within brackets
The Ethics Committees and Institutional Review Boards at each center approved the study. All participants gave written informed consent before study start and the study was performed in accordance with the declaration of Helsinki. Statistica®, 7.1 (StatWin®) was used for statistical analyses and for group comparisons we utilized the χ2 test and the Kruskall-Wallis test. Data are presented as numbers (n) or proportions (%) for categorical variables and as medians with limits for upper and lower quartiles (25th and 75th percentile) for continuous variables, all non-normally distributed.
Results
Pain scoring
During the 12 months, 45 % of the men had experienced LBP of any type, 24 % LBP without sciatica, 8 % LBP + SCI, and 14 % LBP + SCI + NEU (Table 1). The prevalence of pain was similar in all four age strata (Table 1). 36 % of the men with LBP + SCI + NEU reported the pain as severe, 22 % of those with LBP + SCI and 10 % of those with only LBP (p < 0.001) (Table 2). In virtually all comparisons, there was a grading in severity, some being statistically significant some not, so that individuals with LBP was least affected, individuals with LBP and SCI intermediate and individuals with LBP, SCI + NEU most affected (Table 2).
Activity of daily living (ADL)
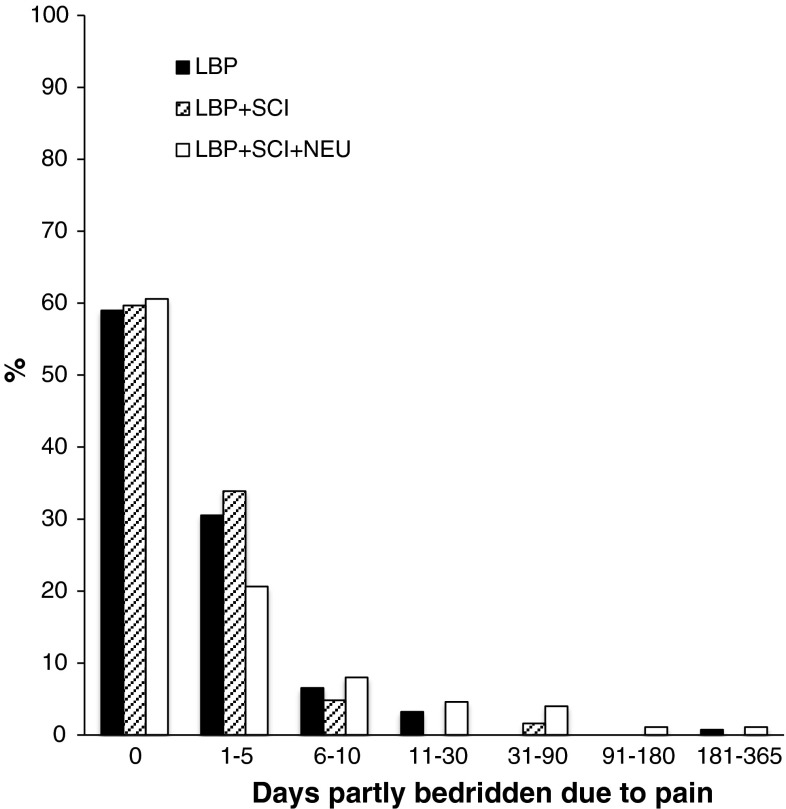
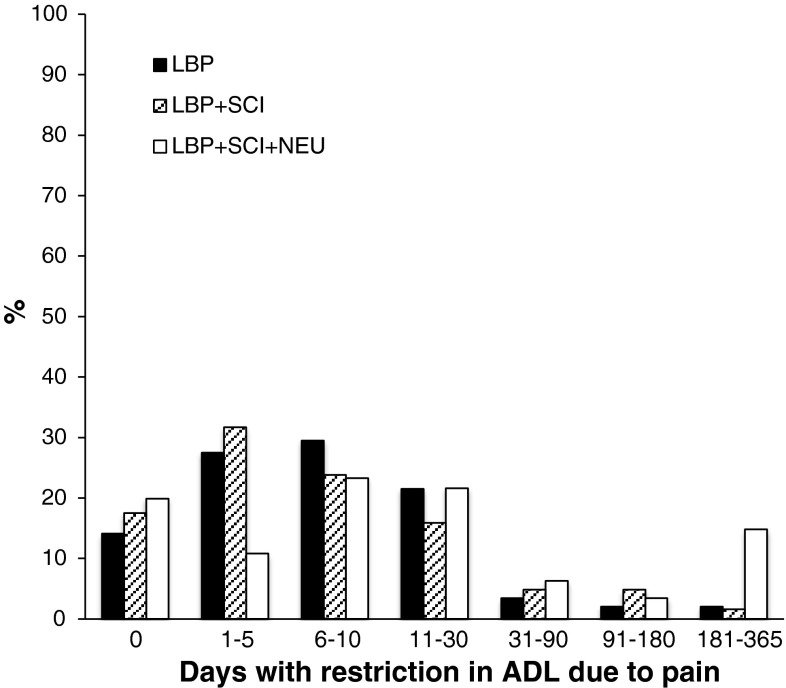
50 % of the men with LBP + SCI + NEU reported impairment in ADL due to the disorder, 31 % of those with LBP + SCI and 23 % of those with only LBP (p < 0.001) (Table 2). The men with LBP + SCI + NEU had to restrict their activities due to the disability for a median of 10 days (mid-quartiles 3–30) during the year, the men with LBP + SCI for a median 6 days (mid-quartiles 2–14) and those with only LBP for a median 7 days (mid-quartiles 3–14) (p < 0.001) (Table 2). As shown in Figs. 1 and 2, there was a skewed distribution and most men had to restrict their activities for only a few days. The four most affected ADL functions were in all subgroups (a) difficulty to bend down and pick up an object, (b) difficulty to put on socks, (c) difficulty to get in and out of a car, and (d) difficulty to stand or walk for 2 h (Table 2). For each of these four activities, we found the highest fraction with impairment in men with LBP + SCI + NEU, intermediate in men with LBP + SCI and the lowest fraction in men with only LBP (Table 2). The prevalence of impairment in ADL was similar in all four age strata, in all three symptom groups LBP (Table 3), LBP + SCI (Table 4) and LBP + SCI + NEU (Table 5).
Fig. 1.
The bars represent the three groups: low back pain only (LBP), low back pain and sciatica (LBP + SCI), and low back pain, sciatica, and neurological symptoms (LBP + SCI + NEU). The figure shows the percentage of individuals with limitations in ADL with different number of LBP driven days in bed
Fig. 2.
Percentage of days with restriction in activity of daily living (ADL) due to pain during 12 months in individuals with low back pain only (LBP), LBP and sciatica (LBP + SCI), and LBP + SCI and neurological symptoms (LBP + SCI + NEU)
Table 3.
Severity of the lower back pain (LBP) and limitations in activity of daily living (ADL) in men aged 69–81 with only LBP (n = 730)
| Age groups | p value for group comparisons | ||||
|---|---|---|---|---|---|
| 69–72 (n = 152) | 73–75 (n = 214) | 76–78 (n = 175) | 79–81 (n = 189) | ||
| Subjectively rated severity of LBP (n = 728) | |||||
| Slight | 49.0 % | 43.0 % | 38.2 % | 50.5 % | |
| Moderate | 41.7 % | 49.5 % | 50.3 % | 37.2 % | 0.18 |
| Severe | 8.6 % | 7.5 % | 11.0 % | 12.2 % | |
| Limitations in activity of daily living (ADL) | |||||
| Any limitations due to LBP (n = 729) | 25.8 % | 20.0 % | 28.3 % | 20.2 % | 0.13 |
| Difficulty bending down to pick up light objects (n = 728) | 14.6 % | 12.1 % | 20.8 % | 18.1 % | 0.82 |
| Difficulty lifting a 5 kg object from the floor (n = 728) | 3.3 % | 3.3 % | 11.0 % | 7.4 % | 0.03 |
| Difficulty putting socks on either foot (n = 730) | 8.6 % | 7.5 % | 14.4 % | 11.7 % | 0.73 |
| Difficulty getting in or out of front seat of a car (n = 730) | 9.9 % | 10.3 % | 13.9 % | 9.6 % | 0.99 |
| Difficulty standing or walking for 2 h (n = 694) | 15.9 % | 14.0 % | 20.8 % | 14.9 % | 0.85 |
| Difficulty sitting in a chair for 30 min without standing (n = 729) | 4.6 % | 8.4 % | 10.4 % | 6.9 % | 0.96 |
| Forced to lay down at least half of the day due to LBP (n = 729) | 10.5 % | 6.1 % | 11.4 % | 7.4 % | 0.60 |
| Partly bedridden due to pain (days) | 0 (0–2) | 0 (0–2) | 0 (0–5) | 0 (0–3) | 0.60 |
| Had to restrict daily activities due to the disability (days) | 7 (3–10) | 10 (4–15) | 5 (2–10) | 7 (3–14) | 0.42 |
Data are presented as proportions (%) or medians with mid-quartile ranges within brackets
Table 4.
Severity of the lower back pain (LBP) and sciatica (SCI) and limitations in activity of daily living (ADL) in men aged 69–81 with LBP and SCI (LBP + SCI) without neurological deficits (n = 226)
| Age groups | p value for group comparisons | ||||
|---|---|---|---|---|---|
| 69–72 (n = 60) | 73–75 (n = 72) | 76–78 (n = 50) | 79–81 (n = 44) | ||
| Subjectively rated severity of LBP or ISC (n = 225) | |||||
| Slight | 36.7 % | 31.9 % | 24.0 % | 27.3 % | |
| Moderate | 43.3 % | 41.7 % | 58.0 % | 47.7 % | 0.75 |
| Severe | 20.0 % | 25.0 % | 18.0 % | 25.0 % | |
| Limitations in activity of daily living (ADL) | |||||
| Any limitations due to LBP (n = 226) | 35.0 % | 33.3 % | 26.0 % | 25.0 % | 0.58 |
| Difficulty bending down to pick up light objects (n = 225) | 25.0 % | 23.6 % | 16.0 % | 11.4 % | 0.40 |
| Difficulty lifting a 5 kg object from the floor (n = 225) | 8.3 % | 6.9 % | 14.0 % | 2.3 % | 0.41 |
| Difficulty putting socks on either foot (n = 226) | 16.7 % | 25.0 % | 10.0 % | 15.9 % | 0.26 |
| Difficulty getting in or out of front seat of a car (n = 226) | 11.7 % | 18.1 % | 12.0 % | 11.4 % | 0.53 |
| Difficulty standing or walking for 2 h (n = 218) | 20.0 % | 19.4 % | 20.0 % | 11.4 % | 0.80 |
| Difficulty sitting in a chair for 30 min without standing? (n = 224) | 13.3 % | 12.5 % | 12.0 % | 11.4 % | 0.69 |
| Forced to lay down at least half of the day due to LBP (n = 226) | 15.0 % | 6.9 % | 6.0 % | 18.2 % | <0.05 |
| Partly bedridden due to pain (days) | 1 (0–3) | 0 (0–0) | 0 (0–1) | 2 (0–5) | <0.05 |
| Had to restrict daily activities due to the disability (days) | 3 (0–7) | 8 (3–14) | 4 (2–14) | 14 (5–30) | 0.08 |
Data are presented as proportion (%) or as medians with mid-quartiles ranges within brackets
Table 5.
Severity of the lower back pain (LBP) and sciatica (SCI) and limitations in activity of daily living (ADL) in men aged 69–81 with LBP and SCI with neurological deficits (NEU) (LBP + SCI + NEU) (n = 406)
| Age groups | p value for group comparisons | ||||
|---|---|---|---|---|---|
| 69–72 (n = 90) | 73–75 (n = 118) | 76–78 (n = 98) | 79–81 (n = 100) | ||
| Subjectively rated severity of LBP (n = 404) | |||||
| Slight | 21.3 % | 18.6 % | 15.3 % | 16.0 % | |
| Moderate | 42.7 % | 48.3 % | 49.0 % | 41.0 % | 0.57 |
| Severe | 36.0 % | 32.2 % | 34.7 % | 42.0 % | |
| Limitations in activity of daily living (ADL) | |||||
| Any limitations due to LBP (n = 403) | 48.3 % | 48.3 % | 48.0 % | 57.0 % | 0.47 |
| Difficulty bending down to pick up light objects (n = 405) | 41.1 % | 28.0 % | 30.6 % | 37.0 % | 0.46 |
| Difficulty lifting a 5 kg object from the floor (n = 405) | 25.6 % | 18.6 % | 16.3 % | 27.0 % | 0.37 |
| Difficulty putting socks on either foot (n = 405) | 32.2 % | 28.8 % | 27.6 % | 31.0 % | 0.86 |
| Difficulty getting in or out of front seat of a car (n = 405) | 30.0 % | 27.1 % | 23.5 % | 31.0 % | 0.60 |
| Difficulty standing or walking for 2 h (n = 383) | 34.4 % | 34.7 % | 29.6 % | 34.0 % | 0.44 |
| Difficulty sitting in a chair for 30 min without standing? (n = 405) | 18.9 % | 16.9 % | 18.4 % | 25.0 % | 0.75 |
| Forced to lay down at least half of the day due to LBP (n = 403) | 21.1 % | 16.1 % | 11.2 % | 20.0 % | 0.55 |
| Partly bedridden due to pain (days) | 0 (0–5) | 0 (0–5) | 0 (0–2) | 0 (0–4) | 0.62 |
| Had to restrict daily activities due to the disability (days) | 10 (7–23) | 14 (0–30) | 10 (2–30) | 12 (5–100) | 0.42 |
Data are presented as proportion (%) or as medians with mid-quartile ranges within brackets
Discussion
During 1 year close to half of all community living men aged 69–81 years experienced LBP in this study. The morbidity was, however, in general low, with gradually increasing morbidity if LBP was associated with sciatica and neurological deficits.
The 46 % one-year prevalence of LBP in our old male population is somewhat high in the perspective of the reported prevalence of 13–49 % in other reports [11–15]. It is, however, difficult to directly compare results since there is no well-established definition of LBP. Efforts have been made to create an international uniform definition, along with a standardized questionnaire with evaluation of topography, temporality and severity of the LBP [16]. The use of this instrument has, however, not become widespread, partly due to the fact that it is only available in English and most studies continue to use their own definition of LBP and their own questionnaires. The use of point prevalence [16], 4-week prevalence [1], and one-year prevalence [2] in different studies further imposes difficulties for comparisons. It is possible that the 12-month recall period we use is associated with recall bias, perhaps avoidable by a shorter period and the use of 4-week prevalence [16]. We, however, focused on grading the severity of pain and limitations in ADL, rather than registering the duration and frequency of symptoms. We believe that the subjective pain level and the pain driven impairment in ADL are the most essential variables for the patient and the association between severity of pain and ADL has not been investigated before.
Since most studies evaluate the one-year prevalence [17], we advocate this time period to facilitate comparison with other settings. A recent systematic review found the one-year prevalence to range from 22 to 65 % in the general population [18]. Prevalence is reported to be higher in adolescents [19] and in young and middle-aged adults than in elderly [20] and those few reports that have included population-based elderly community living individuals have found a prevalence ranging from 13 to 49 % [8], higher in women than in men [4]. Our prevalence is therefore higher than most reported studies, but lower than the 56 % one-year prevalence reported by Hicks et al. Hicks report included 522 participants, all older than 60 years, and inferred that leg pain was common in elderly with LBP and that the likelihood of limitations in ADL was three times higher in those with leg pain. Due to the fact that Hicks recruited participants only from retirement homes and 2/3 of the subjects were women, it is difficult to generalize the results and make a direct comparison to our results.
Other studies have used a different recall period. Vogt et al. [21] included 573 women aged from 50 to 79 years and found a 4-week overall LBP prevalence of 49 %. 8 % in this cohort had only LBP while 41 % had LBP + SCI, a higher proportion than in our study. Yet, in accordance with our results, they found a similar fraction of limitations in ADL due to LBP (11 %) and even more if also lower extremity pain was present (38 %). Since they used 4-week prevalence, included younger individuals, and only women also these results are difficult to compare to ours.
Lavsky-Shulan et al. [22] found a correlation between LBP and impairment in ADL when 3,097 community-dwelling elderly older than 65 years were included. 94 % of the men with LBP rated their pain as mild or moderate and only 6 % as severe. In spite of this, many inferred limitation in ADL due to the LBP, similar in magnitude compared to our results. The report inferred that 15 % had difficulties in walking compared to 16 % in our report, 28 % difficulties in bending compared to 16 % in our cohort and 18 % difficulties to sit compared to 8 % in our cohort. As leg pain and associated neurological deficits were not evaluated in the Lavsky-Shulan study, no comparison could be done regarding these variables.
Although we found a high prevalence of LBP in old men, the morbidity seems in general low. This view is supported by Leveille et al. [13] who reported that LBP in elderly women is associated with mild difficulties in performing, but not inability to execute ADL. They included 1,002 women older than 65 years and found that 42 % had had LBP during the preceding year, 19 % severe LBP, and that women with severe LBP were 3–4 times more likely to have difficulties in ADL. Yet, they found no association between LBP and inability to perform ADL functions. Their inclusion criteria, with self-reported rating of functional tasks at baseline, may result in registration bias and it is therefore difficult to compare the results with our data.
In a report from the Swedish Medical Council in 2000 [24], which is based on the general population statistics (SCB), the reported prevalence of LBP was between 9 and 45 % in an elderly population over the age of 65. However, they also discuss the difficulties of comparing results since the definition of pain differs in different questionnaires. One questionnaire made no distinction between hip and LBP pain and another uses the point prevalence rather than our 1-year prevalence.
To our knowledge there are no published study specifically evaluating the impact of sciatica and neurological symptoms on the clinical manifestation in a population-based cohort of community-dwelling old men. Our data show that the sub-cohort with sciatica and neurological deficits has the most severe disability and that the prevalence of LBP + SCI + NEU was higher than LBP + SCI (Table 1). However, the study design includes weaknesses as we base our inferences on subjective symptoms and we cannot exclude that neurological deficits in some patients may be the result of other diseases.
We found that the prevalence of LBP was not associated with age (in men in the age span 69–81 years) (Table 1). The general belief is that LBP is more common in middle-aged adults than in the elderly [4, 22], while others infer the prevalence of LBP to be highest in the oldest age group [23]. Furthermore, reports infer that severity of LBP increases with age [23]. Our study contradicts all these findings, as the morbidity in the majority of old men with LBP was low. In those with only LBP, 90 % rated their pain as mild or moderate and 75 % had had no limitation in ADL. With these mild symptoms there seems to be little improvement to be gain by intervention, and this group therefore ought to be predominantly symptomatically treated without extensive examination or referral to orthopedic specialists. In contrast, the morbidity is in general high if LBP is associated with sciatica and neurological disability, indicating that this group should be in focus for examination and specialist attention. With limits in health care resources, the medical attention ought therefore to be focused on men with LBP + SCI + NEU, especially the subgroup who had to restrict their daily activities for longer periods, as this group has the greater potential to gain benefits with interventions.
The strengths of this study include the large population-based sample with a high attendance rate of elderly community living men within a small age span. The limitations include the retrospective design that yields a risk of recall bias and the selective subjective evaluation without clinical examinations. Furthermore, it would have been advantageous to specifically evaluate the number and duration of each episode with LBP, the frequency of the associated symptoms, and the recurrence rate.
It must also be emphasized that the limitations of daily living were not of major degree in any of the studied subgroups. Maybe the focus for further treatment and medical interest should therefore be versus those who have greatly reduced or totally lost walking ability due to back pain and sciatica with or without neurological deficits, a specific deficit not evaluated in this study.
We conclude that LBP is a common condition in community living old men, but in general with low morbidity. If LBP is accompanied by sciatica and especially also neurological deficits, the morbidity is generally higher. In the context of a growing older population and limited health care resources, interventions should in our view primarily be targeted at the subgroup with LBP associated with sciatica and neurological deficits, since they have the greatest potential for benefits by interventions.
Acknowledgments
Financial support was received from Skåne University Hospital, Österlund, Pahlsson and Kocks Foundations.
Conflict of interest
None.
References
- 1.Hartvigsen J, Christensen K, Frederiksen H. Back pain remains a common symptom in old age. A population-based study of 4486 Danish twins aged 70-102. Eur Spine J. 2003;12(5):528–534. doi: 10.1007/s00586-003-0542-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartvigsen J, Frederiksen H, Christensen K. Back and neck pain in seniors-prevalence and impact. Eur Spine J. 2006;15(6):802–806. doi: 10.1007/s00586-005-0983-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper JK, Kohlmann T. Factors associated with health status of older Americans. Age Ageing. 2001;30(6):495–501. doi: 10.1093/ageing/30.6.495. [DOI] [PubMed] [Google Scholar]
- 4.Hoy D, et al. A systematic review of the global prevalence of low back pain. Arthr Rheum. 2012;64(6):2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 5.Cassidy JD, et al. Incidence and course of low back pain episodes in the general population. Spine (Phila Pa 1976) 2005;30(24):2817–2823. doi: 10.1097/01.brs.0000190448.69091.53. [DOI] [PubMed] [Google Scholar]
- 6.Statistical Yearbook Sweden 2012, p 538
- 7.Hoy D, et al. Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol. 2010;24(2):155–165. doi: 10.1016/j.berh.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Bressler HB, et al. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine (Phila Pa 1976) 1999;24(17):1813–1819. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 9.Mellstrom D, et al. Free testosterone is an independent predictor of BMD and prevalent fractures in elderly men: MrOS Sweden. J Bone Miner Res. 2006;21(4):529–535. doi: 10.1359/jbmr.060110. [DOI] [PubMed] [Google Scholar]
- 10.Orwoll E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study–a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26(5):569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Cassidy JD, Carroll LJ, Cote P (1998) The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 23(17):1860–1866 (discussion 1867) [DOI] [PubMed]
- 12.Hicks GE, et al. Associations of back and leg pain with health status and functional capacity of older adults: findings from the retirement community back pain study. Arthr Rheum. 2008;59(9):1306–1313. doi: 10.1002/art.24006. [DOI] [PubMed] [Google Scholar]
- 13.Leveille SG, et al. Low back pain and disability in older women: independent association with difficulty but not inability to perform daily activities. J Gerontol A Biol Sci Med Sci. 1999;54(10):M487–M493. doi: 10.1093/gerona/54.10.M487. [DOI] [PubMed] [Google Scholar]
- 14.Reid MC, Williams CS, Gill TM. Back pain and decline in lower extremity physical function among community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 2005;60(6):793–797. doi: 10.1093/gerona/60.6.793. [DOI] [PubMed] [Google Scholar]
- 15.Scudds RJ, Robertson JM. Pain factors associated with physical disability in a sample of community-dwelling senior citizens. J Gerontol A Biol Sci Med Sci. 2000;55(7):M393–M399. doi: 10.1093/gerona/55.7.M393. [DOI] [PubMed] [Google Scholar]
- 16.Dionne CE, et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine (Phila Pa 1976) 2008;33(1):95–103. doi: 10.1097/BRS.0b013e31815e7f94. [DOI] [PubMed] [Google Scholar]
- 17.Hoy D, et al. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–781. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13(3):205–217. doi: 10.1097/00002517-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Jeffries LJ, Milanese SF, Grimmer-Somers KA. Epidemiology of adolescent spinal pain: a systematic overview of the research literature. Spine (Phila Pa 1976) 2007;32(23):2630–2637. doi: 10.1097/BRS.0b013e318158d70b. [DOI] [PubMed] [Google Scholar]
- 20.Edmond SL, Felson DT. Prevalence of back symptoms in elders. J Rheumatol. 2000;27(1):220–225. [PubMed] [Google Scholar]
- 21.Vogt MT, et al. A community-based study of postmenopausal white women with back and leg pain: health status and limitations in physical activity. J Gerontol A Biol Sci Med Sci. 2002;57(8):M544–M550. doi: 10.1093/gerona/57.8.M544. [DOI] [PubMed] [Google Scholar]
- 22.Lavsky-Shulan M, et al. Prevalence and functional correlates of low back pain in the elderly: the Iowa 65+ Rural Health Study. J Am Geriatr Soc. 1985;33(1):23–28. doi: 10.1111/j.1532-5415.1985.tb02855.x. [DOI] [PubMed] [Google Scholar]
- 23.Dionne CE, Dunn KM, Croft PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing. 2006;35(3):229–234. doi: 10.1093/ageing/afj055. [DOI] [PubMed] [Google Scholar]
- 24.SBU (Swedish Medical Council) report from 2000, Frequency of neck and back pain, chap 8, pp 291–302