Abstract
Background. Few data have been published regarding long-term mortality in patients with Parkinson's disease treated with DBS. Methods. This study analyzed long-term mortality rates, causes, and correlates in PD patients treated with DBS. Results. 184 consecutive patients were included; mean follow-up was 50 months. Fifteen deaths occurred (total 8.15%, annual mortality rate 1.94%). Mean age at disease onset and at surgery was 48 ± 2.4 and 63 ± 1.6 years, respectively. Mean disease duration until death was 21 ± 7.8 years. Most deaths related to stroke, myocardial infarction, other vascular/heart disorders, or severe infection; one suicide was recorded. Deceased PD patients were mostly male and had lower motor benefit after DBS, but univariate analysis failed to show significant differences regarding gender and motor benefit. Survival was 99% and 94% at 3 and 5 years. Conclusions. Long-term survival is to be expected in PD patients treated with DBS, possibly higher than previously expected. Death usually supervenes due to vascular events or infection.
1. Introduction
Parkinson's disease is a common, disabling neurodegenerative disorder. Motor symptoms and quality of life improve significantly under adequate treatment, although motor complications commonly arise, typically a few years after the onset of dopaminergic therapy [1]. Several studies have looked into mortality in PD and found a higher risk of death as compared to the general population, even after the introduction of levodopa [2, 3]. Deep brain stimulation (DBS) is an effective procedure in Parkinson's disease (PD) with motor complications [4]. It is safe and surgery-related mortality is low [5]. However, little is known about the long-term mortality in this population, in particular regarding death rates and causes, as few data have been published [6–8]. The recent publication of the EARLYSTIM trial results emphasizes the importance of analyzing this issue in depth, as the number of candidates for DBS will predictably increase in the near future [9]. The aims of this research paper were to evaluate the rates and causes of death in PD patients treated with DBS, up to ten years after surgery.
2. Patients and Methods
Patients enrolled in this study had been consecutively submitted to DBS at the Movement Disorders and Functional Surgery Unit of a large University Hospital between October 2002 and November 2012. All patients were examined before and one month after surgery and then every 6 months. Unified Parkinson's Disease Rating Scale (UPDRS) was assessed before surgery with and without L-dopa medication. After the procedure UPDRS was determined, with stimulation turned on and off. Behavior, mood, activities of daily living, disability, and complications from therapy were assessed using UPDRS (parts I, II, and IV), Schwab and England scale, Beck Depression Inventory, and Geriatric Depression Scale. All patients underwent a comprehensive neuropsychological evaluation prior to surgery and postoperatively at 6 months, 18 months, and 5 years. Neuropsychological test batteries were administered by a trained neuropsychologist. Instruments included the Mini-Mental State Examination, the Frontal Assessment Battery, the Clock Drawing Test, the Dementia Rating Scale, verbal fluency (semantic and phonemic), digit span, associative verbal memory, and visual memory tasks from the Wechsler Memory Scale, the Stroop Test, the Trail Making Test, and the Wisconsin Card Sorting Test. All cognitive assessments before and after surgery were performed while the patients were at a state of pragmatically defined “on.” Postoperative assessments were performed with the stimulators turned on. Adverse events following surgery (including date and cause of death) were recorded during the inpatient period and at each outpatient visit. In addition, general demographic (e.g., age, gender) and clinical data (e.g., disease duration, phenotype, medication type, and dosage) were documented for each patient.
Widely accepted standard inclusion and exclusion criteria for DBS have been observed [10, 11], All subjects met the following criteria: (i) Parkinson's disease diagnosed according to the United Kingdom Parkinson's Disease Society Brain Bank criteria (in our patients the diagnosis had been established for at least 5 years); (ii) at least 50% improvement in motor symptoms after an acute levodopa challenge following complete medication withdrawal for at least 12 hours; (iii) troublesome motor fluctuations and dyskinesias, despite optimal medical therapy adjusted by expert in PD; (iv) clinical examination fully consistent with PD; (v) age up to 70 years, with some degree of flexibility; (vi) absence of dementia or major uncontrolled psychiatric disorders, including suicidal ideation; (vii) absence of neurosurgical, neuroradiological, or general medical contraindications.
Data used in this study concerns follow-up until death or November 2012. No patient was lost to follow-up. Causes of death were determined from confirmed clinical data, except in one patient in whom autopsy was carried out.
Kaplan-Meier survival curves were constructed using death (any cause) as the endpoint. Beyond a descriptive analysis, we performed a comparative analysis using Cox regression to assess differences by gender, disease type, age at motor symptom onset, age at the time of surgery, disease duration until surgery, UPDRS before surgery with and without L-dopa medication, and motor benefit one month after surgery. A descriptive, comparative, and survival analysis was performed, using STATA and SPSS (version 20.0).
3. Results
Between October 2002 and November 2012, 184 PD patients were treated with bilateral deep brain stimulation (181 subthalamic nuclei, 3 globus pallidus internus). Fifteen deaths occurred during the follow-up period (mean 50 months, global mortality 8.15%, and annual mortality rate 1.94%), none of which occurring within the first month after surgery.
3.1. Characteristics of the Whole PD Population Treated with DBS
Sixty-one percent of PD patients treated with DBS were men (n = 113). Mean age at disease onset was 47 ± 9 years (18–64) and mean age at surgery was 60 ± 8 years (33–73). Mean disease duration until surgery was 14 years (5–48). Sixty percent of patients (n = 111) presented akinesia and rigidity as the main disease motor symptoms. Presurgical UPDRS part III average score was 46 ± 11 off medication and 15 ± 7 at the best on state. The average motor benefit in the first month after surgery, based on UPDRS part III before surgery without medication and UPDRS part III after surgery on stimulation and off medication, was 74 ± 14%. There were no significant differences between STN and GPi stimulated patients regarding demographic data, UPDRS scores, or levodopa responsiveness.
3.2. Characteristics of Deceased Patients
Mean age at disease onset and at the time of surgery was 48 ± 2.4 (28–59) and 63 ± 1.6 years (51–71), respectively. Mean disease duration until surgery and until death was 15 ± 1.6 (7–35) and 21 ± 7.8 (11–35) years, respectively. All deceased patients had received subthalamic DBS. Average time elapsed between surgery and death was 65 ± 33.1 months (min 2; max 115), and mean age at the time of death was 67 ± 6.3 (54–76) years. Preoperative UPDRS-III average score was 46 (33–62) off medication and 12 (7–20) at the best on state. The mean motor benefit one month after surgery was 62% (46–85).
Eight of the deceased patients (53%) had clinical criteria for dementia [12], at least at the last observation. Table 1 shows the comparison between deceased and alive patients, regarding baseline features. Deaths were mostly attributed to vascular events (n = 6) and respiratory infections (n = 5); one suicide occurred 39 months after surgery (Table 2). Deceased PD patients were mostly men (n = 13 or 87% of total deaths, P = 0.032) and had gained less motor benefit from surgery (62% versus 76%, P = 0.0004). However, univariate analysis (Cox regression and Kaplan-Meier survival analysis) did not show significant differences regarding gender (HR = 3.740, P = 0.083; IC 95% (0.840–16.654)) or motor benefit (cut-off at 70%: HR = 1.685, P = 0.362; IC 95% (0.549–5.174)) between deceased and nondeceased groups (Figures 1 and 2).
Table 1.
Comparison between deceased patients and survivors.
| Deceased patients | Nondeceased patients | P value | |
|---|---|---|---|
| Male gender: n (%) | 13 (86.67) | 100 (59.17) | 0.032 |
| Age at disease onset (mean, years) | 48.07 ± 2.41 | 46.74 ± 0.69 | 0.707 |
| Akinetic-rigid phenotype: n (%) | 8 (53.33) | 103 (60.95) | 0.564 |
| Age at the time of DBS (mean, years) | 62.8 ± 1.62 | 60.23 ± 0.59 | 0.894 |
| Disease duration until DBS (mean, years) | 14.53 ± 1.59 | 13.42 ± 0.46 | 0.751 |
| UPDRS part III before surgery without L-dopa medication (mean) | 45.6 ± 2.09 | 46.34 ± 0.84 | 0.399 |
| UPDRS part III before surgery with L-dopa medication (mean) | 12.47 ± 1.20 | 14.90 ± 0.51 | 0.083 |
| Motor benefit after surgery (mean, %) | 62.4 ± 5.26 | 75.52 ± 0.96 | 0.0004 |
Table 2.
Deceased PD patients treated with DBS. M: male, F: female.
| Patient | Gender | Time between surgery and death (months) | Cause of death | Comorbidities |
|---|---|---|---|---|
| 1 | M | 48 | Metastasized colon cancer | Hypertension Ischemic stroke |
| 2 | F | 45 | Myocardial infarction | Urinary lithiasis |
| 3 | M | 52 | Pneumonia, sepsis | Hypertension Urinary lithiasis Dementia |
| 4 | M | 69 | Peritonitis, sepsis | Kidney cancer Dementia |
| 5 | M | 39 | Suicide | — |
| 6 | M | 38 | Hemorrhagic stroke | Dyslipidemia Dementia |
| 7 | M | 108 | Hemorrhagic stroke | Prostatic cancer |
| 8 | F | 76 | Traumatic brain injury | Depression Dementia |
| 9 | M | 72 | Ischemic stroke | Diabetes mellitus Hypertension Dementia |
| 10 | M | 115 | Pneumonia | — |
| 11 | M | 26 | Myocardial infarction | Herniated cervical disk |
| 12 | M | 88 | Pneumonia | Diabetes mellitus Prostatic benign hyperplasia Dementia |
| 13 | M | 111 | Pneumonia | Ischemic stroke Dementia |
| 14 | M | 2 | Cardiomyopathy | — |
| 15 | M | 85 | Mesenteric thrombosis | Traumatic subdural hemorrhage Dementia |
Figure 1.
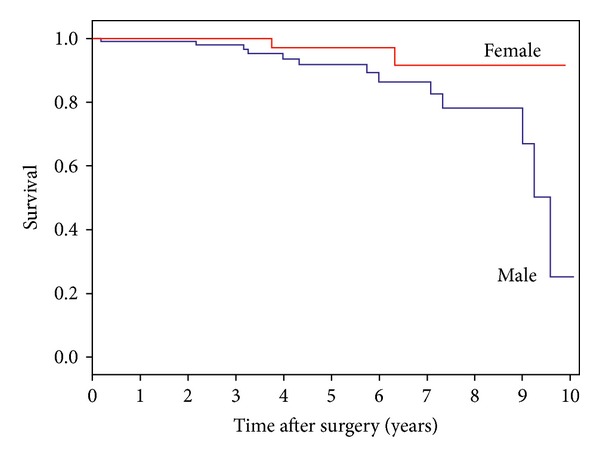
Survival of PD patients by gender. Cox regression indicates no statistical difference between groups.
Figure 2.
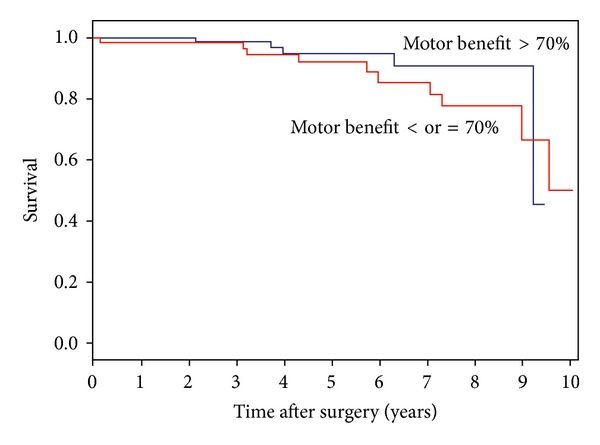
Survival of PD patients by motor benefit following DBS. Cox regression indicates no statistical difference between groups.
Age at surgery higher than 65 years correlated with higher mortality risk (HR = 3.053, P = 0.040; IC a 95% (1.53–8.849)). Survival in this series was 99% at 3 years, 94% at 5 years, and 88% at 7 years after surgery (Figure 3).
Figure 3.
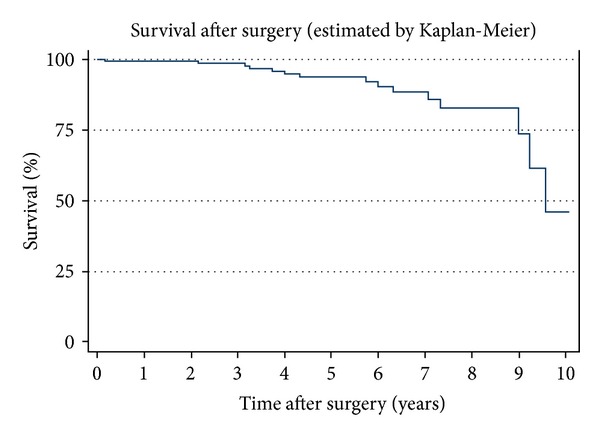
Kaplan-Meier survival curve for the studied population.
4. Discussion
To the best of our knowledge this is the largest series published so far analyzing long-term mortality in DBS-treated PD patients [4, 6–8, 13].
Survival in this series seems somewhat higher than previously reported (Toft et al. found survival rates of 97% at 3 years and 90% at 5 years; Schüpbach et al. reported 97% at 2 years and 89% at 5 years), although it is not possible to calculate whether the difference is significant [6–8]. Anyway, the annual mortality rate reported in this series is clearly lower than that described by Wider et al. (8.5%) [8].
Mean age at death (67 years) was higher than that reported by Schüpbach et al. (63 years), although our patients had a higher mean age at surgery (60 versus 57 years) and a slightly higher mean disease duration until surgery (14 versus 13 years) [7]. The mean follow-up time between surgery and death (65 months) was also higher than previously described (Wider et al. 42 months, Schüpbach et al. 45, and Toft et al. 42) [6–8]. Taken altogether, our results suggest that survival following DBS in PD might be higher than previously estimated.
In this series, age at surgery above 65 years seems to be a predictive mortality factor, as reported by other authors [6, 8]. However, we find ourselves unable to relate this finding to the procedure, and this could be due to natural history only (i.e., older patients are at higher risk of death per se). Preoperative UPDRS-III on and off medication was not different between deceased and nondeceased patients, in contrast to the results reported by Toft et al., who found a relationship between mortality and higher UPDRS score off medication preoperatively [6]. Age at disease onset, disease duration until surgery, and the phenotype of the disease were also not different between groups. Our PD deceased patients were mostly men, which parallels with previously published data reporting greater mortality in male PD patients who did not have DBS [14]. Moreover, deceased patients had lower motor benefit one month after surgery (62% versus 76%, P = 0.0004). One might speculate that axial symptoms in these patients could be more severe thus predisposing to falls, but only one death (out of 15) was related to falling. Otherwise, there were no statistically significant differences between deceased and nondeceased groups with regard to gender or motor benefit. Also, it is not possible to accurately compare STN and GPi groups in this series, due to the very small number of patients in the latter (181 versus 3).
In this series infection was a common cause of death, mainly of respiratory origin, which also stands in agreement with published studies describing pneumonia as an important cause of death in PD [2, 14]. In our series there were no deaths within the first month after surgery, nor any deaths related to the procedure or hardware complications, which stands in agreement with known DBS safety data. There was one suicide (0.54% of all DBS cases), which stands in accordance with the results from the largest multicenter study published so far on this topic in DBS-treated PD patients [15].
Of note, most deceased patients in this study fulfilled criteria for dementia, which has been associated with a higher mortality risk in PD [16].
Our study is limited by the absence of a control group of clinically similar PD patients who did not have DBS (e.g., due to patient refusal to have surgery), in order to compare survival and death causes. Nonetheless, we feel intrigued by the fact that long-term survival seems relatively high for a population of advanced PD patients with long disease duration and wonder whether DBS has any positive effect on survival in PD.
In summary, we found that long-term mortality rates might be lower than previously estimated, and high survival rates are to be expected following DBS in PD, despite the fact that patients already present motor complications and long disease duration at the time of surgery. Mortality is higher among PD male patients or those gaining less motor benefit from surgery, although neither gender nor motor benefit seems to predict death. Older age at surgery correlates with mortality, but this cannot be associated with the procedure itself, and could be simply related to the fact that older people are at higher risk of death. Death in these patients is largely unrelated to PD or surgical complications, as vascular events and pneumonia lead the causes, which stands in line with published epidemiological data in PD. Future research studies should prospectively assess the effect of DBS on patient survival in PD, as compared to best medical therapy.
Acknowledgment
The authors acknowledge Joana Gomes (Faculty of Medicine, University of Porto) for her precious help with statistical methods and analysis.
Disclosure
João Massano has acted as an advisor and received honoraria and financial support to speak or attend meetings from Bial, Grünenthal, Lundbeck, Novartis, and Tecnifar companies; he received educational support from Medtronic and a research grant from the Centro de Investigação Clínica, Centro Hospitalar São João (unrelated to the present work). This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors' Contribution
Sofia Rocha contributed to the conception, organization, and execution of the research project and statistical analysis and also wrote the first draft of the paper. Ana Monteiro contributed to the conception, organization, and execution of the research project. Paulo Linhares contributed to the conception of the research project and also participated in the review and critique of the paper. Clara Chamadoira, Margarida Ayres Basto, Carina Reis, Cláudia Sousa, and Joana Lima participated in the review and critique of the paper. Maria José Rosas contributed to the organization and supervision of the research project and also participated in the review and critique of the paper. João Massano contributed to the conception, organization, and supervision of the research project and also participated in the review and critique of the paper. Rui Vaz supervised the research project and also participated in the review and critique of the paper.
References
- 1.Massano J, Bhatia K. Clinical approach to Parkinson's disease: features, diagnosis, and principles of management. Cold Spring Harbor Perspectives in Medicine. 2012;2(6) doi: 10.1101/cshperspect.a008870.a008870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hely MA, Morris JGL, Traficante R, Reid WGJ, O’Sullivan DJ, Williamson PM. The Sydney multicentre study of Parkinson’s disease: progression and mortality at 10 years. Journal of Neurology Neurosurgery and Psychiatry. 1999;67(3):300–307. doi: 10.1136/jnnp.67.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Posada I, Benito-León J, Louis ED, et al. Mortality from Parkinson’s disease: a population-based prospective study (NEDICES) Movement Disorders. 2011;26(14):2522–2529. doi: 10.1002/mds.23921. [DOI] [PubMed] [Google Scholar]
- 4.Ferreira JJ, Katzenschlager R, Bloem BR, et al. Summary of the recommendations of the EFNS/MDS-ES review on therapeutic management of Parkinson's disease. European Journal of Neurology. 2003;20:5–15. doi: 10.1111/j.1468-1331.2012.03866.x. [DOI] [PubMed] [Google Scholar]
- 5.Benabid AL, Chabardes S, Mitrofanis J, Pollak P. Deep brain stimulation of the subthalamic nucleus for the treatment of Parkinson’s disease. The Lancet Neurology. 2009;8(1):67–81. doi: 10.1016/S1474-4422(08)70291-6. [DOI] [PubMed] [Google Scholar]
- 6.Toft M, Lilleeng B, Ramm-Pettersen J, et al. Long-term efficacy and mortality in Parkinson’s disease patients treated with subthalamic stimulation. Movement Disorders. 2011;26(10):1931–1934. doi: 10.1002/mds.23817. [DOI] [PubMed] [Google Scholar]
- 7.Schüpbach M, Welter M, Bonnet A, et al. Mortality in patients with Parkinson's disease treated by stimulation of the subthalamic nucleus. Movement Disorders. 2007;22(2):257–261. doi: 10.1002/mds.21264. [DOI] [PubMed] [Google Scholar]
- 8.Wider C, Pollo C, Bloch J, Burkhard PR, Vingerhoets FJG. Long-term outcome of 50 consecutive Parkinson’s disease patients treated with subthalamic deep brain stimulation. Parkinsonism and Related Disorders. 2008;14(2):114–119. doi: 10.1016/j.parkreldis.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 9.Schuepbach WM, Rau J, Knudsen K, et al. Neurostimulation for Parkinson's disease with early motor complications. The New England Journal of Medicine. 2013;368:610–622. doi: 10.1056/NEJMoa1205158. [DOI] [PubMed] [Google Scholar]
- 10.Lang A, Houeto J, Krack P, et al. Deep brain stimulation: preoperative issues. Movement Disorders. 2006;21(supplement 14):S171–S196. doi: 10.1002/mds.20955. [DOI] [PubMed] [Google Scholar]
- 11.Bronstein J, Tagliati M, Alterman R, et al. Deep brain stimulation for Parkinson disease an expert consensus and review of key issues. Archives of Neurology. 2011;68(2):165–171. doi: 10.1001/archneurol.2010.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Emre M, Aarsland D, Brown R, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Movement Disorders. 2007;22(12):1689–1707. doi: 10.1002/mds.21507. [DOI] [PubMed] [Google Scholar]
- 13.Vergani F, Landi A, Pirillo D, Cilia R, Antonini A, Sganzerla EP. Surgical, medical, and hardware adverse events in a series of 141 patients undergoing subthalamic deep brain stimulation for Parkinson disease. World Neurosurgery. 2010;73(4):338–344. doi: 10.1016/j.wneu.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 14.Beyer M, Herlofson K, Larsen J. Causes of death in a community-based study of Parkinson's disease. Acta Neurologica Scandinavica. 2001;103:7–11. doi: 10.1034/j.1600-0404.2001.00191.x. [DOI] [PubMed] [Google Scholar]
- 15.Voon V, Krack P, Lang AE, et al. A multicentre study on suicide outcomes following subthalamic stimulation for Parkinson’s disease. Brain. 2008;131(10):2720–2728. doi: 10.1093/brain/awn214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meireles J, Massano J. Cognitive impairment and dementia in Parkinson's disease: clinical features, diagnosis, and management. Front Neurol. 2012;3, article 88 doi: 10.3389/fneur.2012.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]


