Abstract
Background:
A significant proportion of squamous cell carcinomas of the oropharynx (OP-SCC) are related to human papillomavirus (HPV) infection and p16 overexpression. This subgroup proves better prognosis and survival but no evidence exists on the correlation between HPV and p16 overexpression based on diagnostic measures and definition of p16 overexpression. We evaluated means of p16 and HPV diagnostics, and quantified overexpression of p16 in HPV-positive and -negative OP-SCCs by mode of immunohistochemical staining of carcinoma cells.
Methods:
PubMed, Embase, and the Cochrane Library were searched from 1980 until October 2012. We applied the following inclusion criteria: a minimum of 20 cases of site-specific OP-SCCs, and HPV and p16 results present. Studies were categorised into three groups based on their definition of p16 overexpression: verbal definition, nuclear and cytoplasmatic staining between 5 and 69%, and ⩾70% staining.
Results:
We identified 39 studies with available outcome data (n=3926): 22 studies (n=1980) used PCR, 6 studies (n=688) used ISH, and 11 studies (n=1258) used both PCR and ISH for HPV diagnostics. The methods showed similar HPV-positive results. Overall, 52.5% of the cases (n=2062) were HPV positive. As to p16 overexpression, 17 studies (n=1684) used a minimum of 5–69% staining, and 7 studies (n=764) used ⩾70% staining. Fifteen studies (n=1478) referred to a verbal definition. Studies showed high heterogeneity in diagnostics of HPV and definition of p16. The correlation between HPV positivity and p16 overexpression proved best numerically in the group applying ⩾70% staining for p16 overexpression. The group with verbal definitions had a significantly lower false-positive rate, but along with the group applying 5–69% staining showed a worse sensitivity compared with ⩾70% staining.
Conclusions:
There are substantial differences in how studies diagnose HPV and define p16 overexpression. Numerically, p16 staining is better to predict the presence of HPV (i.e. larger sensitivity), when the cutoff is set at ⩾70% of cytoplasmatic and nuclear staining.
Keywords: p16, hpv, oropharyngeal tumours, head and neck tumours, human papillomavirus, p16ink4a
Oral and pharyngeal cancers are the sixth most frequent tumour with over 482 000 new cases and 273 000 deaths worldwide in 2008 (Ferlay et al, 2010). The role of high-risk human papillomavirus (HR-HPV) in the carcinogenesis of the uterine cervix is well recognised (Bosch et al, 1995), and owing to numerous studies in the past 10 years, HR-HPV is now also a well-known risk factor in oropharyngeal squamous cell carcinomas (OPSCCs) in addition to established factors such as tobacco and alcohol exposure (Dayyani et al, 2010). Compared with other head and neck squamous cell carcinomas (HNSCCs), HPV-related OPSCCs have different epidemiology, histopathological characteristics, therapeutic response, and clinical outcome (Shah and Patel, 2003; Fakhry and Gillison, 2006; De Vita et al, 2008; Robinson et al, 2010; Westra, 2012).
The small, non-enveloped, DNA virus HPV belongs to the Papillomaviridae family and is known commonly to infect squamous epithelial cells (Doorbar et al, 2012). Cell morphology alone is insufficient to determine the presence of HPV (Lewis et al, 2012), although HPV-positive oropharyngeal cancers are often characterised histologically by a non-keratinising or basaloid morphologic pattern. Two techniques are generally used to diagnose HPV: polymerase chain reaction (PCR) and in situ hybridisation (ISH). Both have strengths and limitations. Human papillomavirus-specific PCR is not routinely available in most diagnostic laboratories; few HPV PCR tests are approved for clinical use, and the method requires a high level of technical skills and special laboratory facilities to prevent contamination. When applied to extracts made from fresh-frozen biopsy samples, the highest sensitivity is obtained, but the PCR analysis does not distinguish the mere presence of HPV from a clinically relevant HPV infection, where the HPV genome is often integrated into the host genome and actively transcribes HPV oncoproteins. Detection of HPV with ISH provides evidence of viral genomes through mRNA or DNA present in the tumour nuclei and is highly specific, although less sensitive than PCR (Robinson et al, 2010). This method does not differentiate between integrated and non-integrated genomes.
The presence of HR-HPV DNA is insufficient to classify accurately tumours as an HPV infection as it may be biologically inactive and not the cause of malignancy. Along with HPV diagnostics, immunohistochemical detection of p16 (p16-IHC) is often used as a surrogate marker for HPV infection and an activity of viral oncoproteins. P16 is a tumour suppressor gene that inhibits cyclin-dependent kinase 4A. In the presence of transcriptionally active HPV, hypophosphorylated retinoblastoma protein (pRb) bind to the HPV oncoprotein E7, allowing the transcriptional activator E2F to be constitutionally active while effectively stopping the negative feedback of free pRb on p16. Overexpression of p16 ensues. Independent of treatment modality, OPSCC patients with p16 overexpression have better prognosis and clinical outcome (Langendijk and Psyrri, 2010). P16-IHC is generally accessible and its technical costs are estimated to be 2–16 times lower than other HPV-specific tests (Lewis, 2012). Several studies have reported difficulties in HPV and p16 diagnostics, as there is no consensus on defining overexpression of p16 by a clear percentage cutoff level, and definitions vary from ⩾5%, ⩾75% to numerous less specific verbal definitions, for example, ‘diffuse and strong nuclear and cytoplasmatic staining' (Smeets et al, 2007; Lewis, 2012). This may be problematic because different staining patterns can correlate differently to HPV-positive and -negative tumours, and staining patterns may ultimately distinguish transcriptionally from non-transcriptionally active HPV infections and thereby help determine prognosis and clinical outcomes.
The aim of this systematic review was to define and categorise overexpression of p16 based on immunohistochemical staining and correlate the categories to HPV-positive and -negative OP-SCCs.
Methods
Search strategy and selection criteria
One author (CGL) undertook electronic literature searches within PubMed (Medline), Embase, and the Cochrane Library. The search strategy was as follows including MESH terms and keywords: ‘HPV' or ‘papillomavirus' or ‘papillomaviridae' and ‘p16' or ‘cdkn2a' or ‘cyclin-dependent kinase inhibitor p16' or ‘p16 genes' and ‘oropharynx' or ‘oropharyngeal' or ‘palatine tonsil' or ‘tonsil' or ‘palatine' or ‘tongue' or ‘mouth' or ‘oral'. Two authors (CGL and MG) independently reviewed the relevance of all resulting study titles and abstracts identified through the above search, and full-text copies of potentially eligible articles were assessed. Finally, one author (CGL) reviewed reference lists of the initially included studies. Studies with identical authors were contacted to avoid including the same study population twice.
We included all studies published in English from January 1980 to October 2012 regardless of funding source. The inclusion criteria were restricted to: age above 18 years, a minimum 20 cases of site-specific OP-SCCs (morphologic variants were included), and HPV and p16 results stated.
Data synthesis
Two authors (CGL and MG) independently extracted relevant data from the included studies and entered them into a piloted data extraction form. The following information were recorded: country, year(s) of biopsy collection, demographics, number of cases, tumour site (base of tongue, palatine tonsils, or other), tumour morphology (keratinising, non-keratinising, or mixed), histopathological grade (carcinoma in situ, poor, moderate, or high differentiation), IHC staining probe, definition of p16 overexpression, biopsy preservation (fresh frozen or paraffin embedded), IHC evaluation by pathologists (yes or no), HPV results (negative or HPV-16, HPV-18, HPV-33, HPV-35, and HPV-58 positive), HPV diagnostics (HPV DNA PCR, HPV DNA ISH, and HPV DNA ISH followed by PCR, HPV RNA RT–PCR, and HPV RNA ISH), and the number of p16-positive and negative cases.
Included studies were categorised into three groups by their definition of p16 overexpression: (a) a verbal definition (e.g. ‘Cases were classified in a binary manner as either positive (any cells with nuclear and cytoplasmatic staining) or negative'), (b) 5–69% nuclear and cytoplasmatic staining, and (c) ⩾70% staining.
Statistical analysis
Statistics were carried out using IBM SPSS Statistics 19.0 (IBM SPSS, Chicago, IL, USA). Descriptive statistics are presented as actual numbers and percentages, or median and range where appropriate. We conducted a meta-analysis using the bivariate model (Reitsma et al, 2005). In the bivariate model, the logit-transformed sensitivities and specificities and the correlation between them across studies are modelled directly. The model accounts for sampling variability within studies and also account for between-study variability through the inclusion of random effects. In the preliminary meta-analyses for each definition of p16 positivity, we fitted the bivariate model separately for each test, and obtained a diagnostic odds ratio, sensitivity, and specificity. Hierarchical summary receiver-operator curve (HSROC) was applied in the meta-analysis and is recommended in the current meta-analytic literature for diagnostic meta-analyses (Leeflang et al, 2013). In addition, HSROCs were plotted with 95% CI. Afterwards, we compared the tests in two separate models, where the definitions used were included as covariates in a meta-regression. Variance components were estimated by restricted maximum likelihood, because of the number of studies and the heterogeneity of the included studies. Statistical analyses on meta-regression were performed in R using the mada package function reitsma.
Results
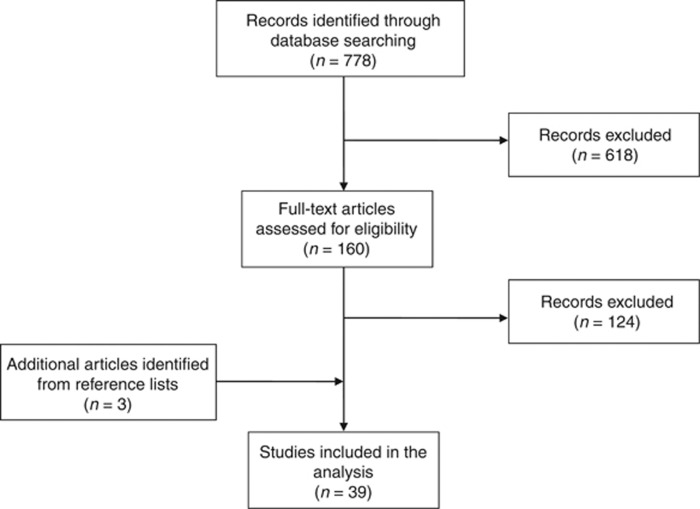
The initial literature search yielded a total of 778 records. From these, we manually selected 160 articles for full-text assessment, of which 112 articles were later excluded. Accordingly, 48 studies were left eligible for inclusion (Figure 1). Additional three studies were later identified through searching reference lists. Studies with identical authors were contacted and resolved in 12 studies excluded; 11 studies were confirmed duplicates by authors; and one study excluded without reply from authors. Thus, a total of 39 studies (n=3926) were included in the review (Table 1).
Figure 1.
PRISMA diagram.
Table 1. Overview of studies.
| Author (year) | Country | Year | Study years | n | Age (years) | M/F | HPV+ | Analysis | P16+ | P16 cutoff (%) | P16 antibody | Sensitivity of p16 (%) | Specificity of p16 (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Al-Swiahb et al (2010) |
Taiwan |
2010 |
1992–2008 |
220 |
51 |
206/14 |
33 |
PCR |
36 |
⩾5% and <70 |
Clone unknown (Neomarkers, Fremont, CA, USA) |
86 |
99 |
|
Ang et al (2010b) |
USA |
2010 |
2002–2005 |
323 |
Unknown |
271/52 |
206 |
PCR |
214 |
⩾70 |
E6H4 (MTM Laboratories AG, Heidelberg, Germany) |
90 |
93 |
|
Charfi et al (2008) |
France |
2007 |
1987–2005 |
52 |
61 |
36/16 |
32 |
PCR |
25 |
⩾5 and <70 |
E6H4 (MTM Laboratories AG, Heidelberg, Germany) |
84 |
59 |
|
Chenevert and Chiosea (2012) |
USA |
2012 |
1956–1969 and 2007–2009 |
97 |
58 |
80/17 |
54 |
ISH |
57 |
⩾70 |
G175-405 (BD Pharmingen, San Diego, CA, USA) |
69 (second period: 86%) |
80 (second period: 90%) |
|
El-Mofty and Patil (2006) |
USA |
2006 |
Unknown |
20 |
Unknown |
Unknown |
12 |
ISH |
11 |
Verbal definition |
Clone unknown (Novacastra Labs Ltd, Newcastle, UK |
100 |
89 |
|
El-Mofty et al (2008) |
USA |
2008 |
Unknown |
32 |
Unknown |
28/4 |
22 |
ISH |
26 |
⩾70 |
Clone unknown (Novacastra Labs Ltd, Newcastle, UK) |
85 |
100 |
|
Evans et al (2011) |
USA |
2011 |
2000–2007 |
30 |
55 |
25/5 |
22 |
PCR and ISH |
22 |
⩾70 |
JC8 (Lab Vision, Fisher Scientific, Pittsburgh, PA, USA) |
NA |
NA |
|
Farshadpour et al (2011) |
The Netherlands |
2011 |
1980–2004 |
32 |
Unknown |
Unknown |
14 |
ISH |
14 |
⩾70 |
Clone unknown (Neomarkers, Fremont, CA, USA) |
93 |
100 |
|
Friedland et al (2012) |
Australia |
2011 |
1996–2008 |
20 |
Unknown |
Unknown |
19 |
PCR |
19 |
Verbal definition |
Clone unknown (Santa Cruz Biotechnology, Santa Cruz, CA, USA) |
100 |
100 |
|
Gao et al (2013) |
USA |
2012 |
1997–2006 |
150 |
56 |
136/14 |
122 |
PCR |
131 |
⩾5 and <70 |
E6H4 (MTM Laboratories AG, Heidelberg, Germany) |
93 |
100 |
|
Hafkamp et al (2008) |
The Netherlands |
2008 |
1992–2001 |
81 |
58 |
59/22 |
33 |
PCR |
37 |
⩾5 and <70 |
E6H4 (Dako, Glostrup, Denmark) |
86 |
98 |
|
Hoffmann et al (2012) |
Germany |
2012 |
2004–2009 |
20 |
Unknown |
16/4 |
12 |
ISH |
14 |
⩾5 and <70 |
CINtecÒ (MTM Laboratories AG, Heidelberg, Germany |
79 |
83 |
|
Holzinger et al (2012) |
Germany |
2012 |
1990–2008 |
196 |
57 |
146/50 |
97 |
PCR |
54 |
Verbal definition |
E6H4 (MTM Laboratories AG, Heidelberg, Germany) |
78 |
59 |
|
Hong et al (2010) |
Australia |
2010 |
1987–2006 |
195 |
59 |
159/36 |
83 |
PCR |
65 |
Verbal definition |
JC2 (Neomarkers, Fremont, CA, USA) |
95 |
84 |
|
Junor et al (2012) |
Scotland |
2012 |
1999–2001 and 2003–2005 |
254 |
60 |
182/72 |
133 |
PCR |
94 |
Verbal definition |
E6H4 (MTM Laboratories, Heidelberg, Germany) |
95 |
46 |
|
Kim et al (2007) |
South Korea |
2007 |
1995–2005 |
52 |
Unknown |
Unknown |
38 |
PCR |
37 |
Verbal definition |
Unknown |
NA |
NA |
|
Klussmann et al (2009) |
Germany |
2009 |
1997–2005 |
60 |
60 |
47/13 |
29 |
PCR |
33/57 |
⩾5 and <70 |
16P04 (Neomarkers, Fremont, CA, USA) |
NA |
NA |
|
Kuo et al (2008) |
Taiwan |
2008 |
1997–2005 |
92 |
51 |
79/13 |
69 |
PCR and ISH |
49 |
⩾5 and <70 |
JC8 (Neomarkers, Fremont, CA, USA ) |
NA |
NA |
|
Laco et al (2011) |
Crech Republic |
2010 |
2000–2009 |
22 |
60 |
13/9 |
18 |
PCR |
22 |
Verbal definition |
CINtec (MTM Laboratories AG, Heidelberg, Germany) |
NA |
NA |
|
Lewis et al (2010) |
USA |
2010 |
1997–2008 |
239 |
55 |
211/28 |
144 |
ISH |
187 |
⩾5 and <70 |
Clone unknown (MTM Laboratories AG, Heidelberg, Germany) |
74 |
90 |
|
Li et al (2007) |
China |
2007 |
1985–2004 |
49 |
58 |
37/12 |
9 |
PCR and ISH |
11 |
Verbal definition |
16p04 (Neomarkers, Fremont, CA, USA ) |
89 |
95 |
|
Licitra et al (2006) |
Italy |
2006 |
1990–1999 |
90 |
58 |
69/21 |
17 |
PCR |
32 |
Verbal definition |
Clone unknown (Neomarkers, Fremont, CA, USA ) |
NA |
NA |
|
Lindquist et al (2012) |
Sweden |
2012 |
1970–2002 |
73 |
59 |
59/14 |
36 |
ISH |
40 |
⩾5 and <70 |
Clone unknown (Pharmingen, San Diego, CA, USA) |
73 |
60 |
|
Mellin Dahlstrand et al (2005) |
Sweden |
2005 |
1983–1999 |
51 |
63 |
39/12 |
25 |
PCR |
27 |
⩾5 and <70 |
E6H4 (DakoCytomation A/S, Carpinteria, CA, USA) |
74 |
79 |
|
Mills et al (2012) |
USA |
2012 |
Unknown |
62 |
Unknown |
Unknown |
33 |
PCR and ISH |
37 |
⩾5 and <70 |
E6H4, predilute, Tris (pH 9.0) (MTM Laboratories Inc., Westborough, MA, USA) |
NA |
NA |
|
Nichols et al (2009) |
USA |
2008 |
Unknown |
44 |
Unknown |
35/9 |
27 |
PCR |
29 |
Verbal definition |
Clone unknown (MTM Laboratories, Heidelberg, Germany) |
100 |
100 |
|
Ukpo et al (2011) |
USA |
2011 |
Unknown |
211 |
56 |
188/23 |
153 |
ISH |
148 |
Verbal definition |
E6H4 (MTM, Laboratories Inc., Westborough, MA, USA) |
98 |
90 |
|
Park et al (2012) |
Korea |
2011 |
2002–2007 |
93 |
62 |
80/13 |
53 |
PCR |
46 |
Verbal definition |
P2D11F11 (Novocastra Labs Ltd, Newcastle, UK) |
100 |
85 |
|
Preuss et al (2008) |
Germany |
2008 |
1998–2005 |
106 |
57 |
77/29 |
30 |
PCR |
61 |
Verbal definition |
16p04 (Neomarkers, Fremont, CA, USA) |
NA |
NA |
|
Quon et al (2013) |
USA |
2011 |
Unknown |
48 |
Unknown |
Unknown |
36 |
PCR and ISH |
35 |
Verbal definition |
E6H4 (MTM Laboratories Inc., Westborough, MA, USA) |
91 |
69 |
|
Reimers et al (2007) |
Germany |
2007 |
1997–2002 |
106 |
59 |
83/23 |
30 |
PCR |
29 |
⩾5 and <70 |
16p04 (Neomarkers, Fremont, CA, USA ) |
86 |
86 |
|
Schache et al (2011b) |
UK |
2011 |
1988–2009 |
108 |
58 |
83/25 |
36 |
PCR and ISH |
42 |
⩾70 |
CINtec (MTM Laboratories AG, Heidelberg, Germany) |
NA |
NA |
|
Semrau et al (2012) |
Germany |
2012 |
2000–2008 |
52 |
56 |
42/10 |
15 |
PCR and ISH |
17 |
⩾5 and <70 |
Clone unknown (Roche MTM Laboratories, Westborough, MA |
NA |
NA |
|
Shi et al (2009) |
Canada |
2009 |
2003–2006 |
111 |
57 |
82/29 |
73 |
PCR and ISH |
72 |
Verbal definition |
CINtec (MTM Laboratories, Westborough, MA, USA) |
NA |
NA |
|
Thavaraj et al (2011) |
UK |
2011 |
Unknown |
142 |
58 |
108/34 |
100 |
PCR and ISH |
90 |
⩾70 |
CINtec (MTM Laboratories Westborough, MA, USA) |
97 |
75 |
|
Ukpo et al (2012) |
USA |
2012 |
1996–2007 |
154 |
56 |
133/21 |
89 |
ISH |
104 |
Verbal definition |
E6H4 (MTM Laboratories Inc., Westborough, MA, USA) |
NA |
NA |
|
Weinberger et al (2010) |
USA |
2010 |
1980–1999 |
140 |
60 |
106/34 |
58 |
ISH |
25 |
Verbal definition |
JC8 (Abcam Corporation, Cambridge MA, USA) |
100 |
57 |
|
Weiss et al (2012) |
Germany |
2012 |
Unknown |
61 |
Unknown |
Unknown |
36 |
PCR |
30 |
⩾5 and <70 |
Unknown |
NA |
NA |
| Zhao et al (2012) | USA | 2012 | 2002–2006 | 38 | Unknown | Unknown | 14 | ISH | 22 | Verbal definition | MAB4133 (Chemicon International Company/Millipore Corporation, Temecula, CA, USA) | NA | NA |
Abbreviations: HPV=human papillomavirus; ISH=in situ hybridisation; NA=not applicable; PCR=polymerase chain reaction.
In the pooled analysis of all studies with demographic information (n=3625), the majority of patients were male subjects (n=2921, 80.6%). Age ranged from 20 to 93 years with a median of 58 years. Thirty-four studies (n=3420 subjects) were European, Australian, or US based, and five studies (n=506 subjects) were Asian. Ethnicity was reported in 22 studies (n=2265), with 69.2% of these patients being Caucasian (n=1568), 11.9% (n=269) were of Asian origin, and 18.9% (n=428) had mixed ethnicity. Tumours were represented throughout the oropharynx, but were primarily located in the palatine tonsils (n=1420, 36.2%). Tumours at the base of the tongue (n=414, 10.5 %) and of unspecified location represent the remaining (n=2092, 53.3%) (Table 2).
Table 2. Patient characteristics.
| Demographics | Total (n=3926) |
|---|---|
| Age, median (range) |
58 (20–93) |
|
Sexa, n=3625 | |
| Male | 2921 |
| Female |
704 |
|
Country, n=3926 | |
| Europe | 1446 |
| Australia | 215 |
| USA | 1759 |
| Asia |
506 |
|
Ethinicity, n=3926 | |
| Caucasian | 1568 |
| Asian | 269 |
| Mixed | 428 |
| Unspecified |
1661 |
|
Tumour origin, n=3926 | |
| Base of tongue | 414 |
| Palatine tonsils | 1420 |
| Unspecified/oropharynx |
2092 |
|
Definition of p16 overexpression, n=3926 | |
| Staining equals or exceeds 70% of nuclei and cytoplasm | 764 |
| Staining between 5 and 69% of nuclei and cytoplasm | 1684 |
| Verbal definition | 1478 |
N=301 subject's sex is unknown.
A total of 52.5% cases (n=2062) were found HPV positive by PCR, ISH, or both. For HPV diagnostics, 22 studies (n=1980) used PCR, 6 studies (n=668) used ISH, and 11 studies (n=1258) used both techniques. In the PCR-based HPV-testing group, 49.6% (n=984) of cases were said to be positive and 59.8% of cases (n=412) were positive in the ISH group, whereas 52.9% (n=666) were positive when both diagnostic approaches were used. The definition of p16 overexpression varied, but all studies dichotomised the results to either negative or positive. In the pooled analysis, p16 overexpression was shown by 37.6% (n=1478) of subjects based on a verbal definition, by 42.9% (n=1684) of subjects based on staining between 5 and 69%, and finally, by 19.5% (n=764) of subjects based on staining equal to or exceeding 70% (Table 2).
Centres placed in the United States defined p16 as positive when staining was between 5 and 69% (6 centres, n=770) or based on staining equal to or exceeding 70% (4 centres, n=482). Six centres (n=507) used a verbal definition. European centres either defined p16 as positive when staining was between 5 and 69% (9 centres, n=602) or based on staining exceeding 70% (3 centres, n=282). Four centres (n=562) used a verbal definition. Three centres (n=194) in Asia used a verbal definition, and two centres (n=312) defined p16 as positive when staining was between 5 and 69%. No Asian centres defined p16 as positive based on staining equal to or exceeding 70%.
Eleven studies (n=861) reported data on histopathologic grade (poorly differentiated, moderate differentiated, highly differentiated, or carcinoma in situ), and six studies (n=634) reported status on tumour morphology (keratinising, non-keratinising, mixed, or unknown). The limited availability of data on tumour morphology did not allow us to examine systematically to what degree the non-keratinising tumours were related to the presence of HPV, as has been observed previously. We found no trends regarding publication year and definition of p16, likely owing to the fact that the included studies were all published in the past 10 years.
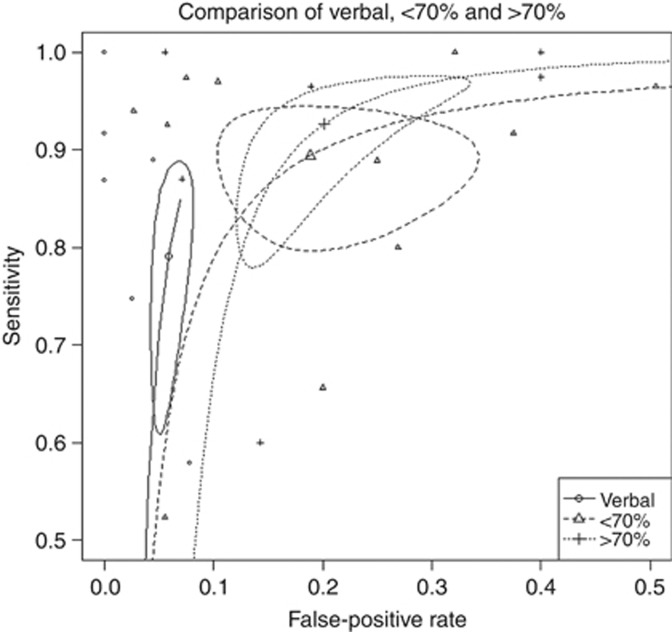
Twenty-five studies (n=2888) provided sufficient information to construct a two-by-two table of both p16-negative/-positive and HPV-negative/-positive biopsies. The correlation between HPV and p16 overexpression was numerically greater, when positivity was defined as staining above ⩾70% with a sensitivity of 0.927 (95% CI: 0.793–0.974). The verbal group and >5–<70% group had a sensitivity of 0.791 (95% CI: 0.608–0.888) and 0.894 (95% CI: 0.805–0.942), respectively. The false-positive rate of 0.059 (95% CI: 0.031–0.112) for the verbal group was superior to the rate of 0.201 (95% Cl: 0.12–0.337) of p16 ⩾70% (see Figure 2).
Figure 2.
Hierarchical summary receiver-operator curve (HSROC) of the studies from Table 1. The studies have been divided into three groups based on their definition of p16 staining: a verbal group, a <70% group, and a >70% group, including 95% CIs for the summary point. The verbal group has a lower false discovery rate, while the >70% group had a greater overall sensitivity and a smaller 95% CI.
Discussion
This is the first systematic review exploring the correlation between HPV infection and p16 overexpression in OPSCCs. This review shows that p16 overexpression correlates numerically better to HPV results if staining of tumour cells exceeds 70% rather than lower percentages or positivity based on a verbal definition. The issue of determining a specific cutoff value for p16 positivity has earlier been addressed in smaller samples supporting staining above 75% or staining above 50% combined with >25% confluent areas to define p16 positivity (Begum and Westra, 2008). We found no statistically significant difference between groups of p16 definition correlated to HPV, which may be because of the great heterogeneity among studies, including different p16 antibodies. In addition, ISH and PCR methods vary from centre to centre, leading to a loss of statistical power to detect differences. The explanation might also be that all p16 groups are equally correlated to HPV status; thus, the level of p16 staining is less important and the status of positivity or negativity is evident for a given staining, that is, most p16-positive tumours are above 70% when positive. Histopathologic grade and morphology was insufficiently reported and an agreement on a grading scheme applicable to OPSCC and consensus on reporting data is important for future research. As to p16 antibodies, an FDA-approved recommendation might be profitable to uniform research methods. It is widely assumed that HPV-related oropharyngeal cancers are poorly differentiated based on the immature appearance of the tumour cells, but in fact they are commonly highly differentiated as they emulate the specialised epithelium of the tonsillar crypts (Westra, 2009). Further data for analysis on this matter might question the challenge of interpreting p16-IHC in mixed and keratinising SSCs. In addition, it should be considered if carcinoma in situ should be included in future similar studies.
In future studies applying p16-IHC and HPV diagnostics, the real value of IHC must be questioned once the site of the tumour is known (oropharynx) and the morphology is recognised (non-keratinising); the chance of a non-keratinising OPSCC being HPV positive is still not known.
Previous data report a prevalence of HPV in OPSCC of 51%, which is similar to our results (O'Rorke et al, 2012). Regardless if studies used PCR, ISH, or both, similar results were achieved.
Oropharyngeal squamous cell carcinomas are characterised by a heterogeneous clinical and molecular profile (Huang et al, 2002; Shah and Patel, 2003; Bosch et al, 2004; De Vita et al, 2008) and have interestingly proven to have a better prognostic outcome in cases with p16 overexpression (Lewis et al, 2010; Ang et al, 2010a). P16-IHC is, however, a diagnostic method causing much debate, and concerns have been raised: p16 overexpression might be associated with functional pRb disturbances irrelevant for the HPV infection (Marur et al, 2010). High-risk human papillomavirus-infected OPSCCs have not necessarily lost the 9p21 allele encoding p16 (Braakhuis et al, 2004), and p16-IHC has been reported 100% sensitive but 79% specific as to carcinomas with HPV infection (Smeets et al, 2007). P16-IHC is performed on just one slide of tumour tissue and staining might vary allowing false-negative results explaining a lower specificity. Lately, cutoff values above 70 or 75% have proven to be of wider use (Ang et al, 2010a; Evans et al, 2011; Schache et al, 2011a) as compared with, e.g., values >10% as a ‘validated' definition of p16 overexpression. In a retrospective study based on material from The Danish Society for Head and Neck Oncology (DAHANCA), the cutoff value was changed in a Letter to the Editor after publication from >10 to >70% (Lassen and Overgaard, 2012).
In conclusion, substantial differences exist in the definition of p16 overexpression and means of HPV diagnostics between studies. To achieve the highest correlation between p16-IHC and HPV results, we advise clinicians and researchers to define p16 overexpression as >70% staining of tumour cells. Future research in this field should report on p16 and HPV results, allowing a better understanding of the association between the two.
Acknowledgments
Authors contribution
CB concepted the idea of the study. CGL and MG searched the scientific literature, extracted data, and led the writing. LK, CGL, and DHJ performed statistics. All authors provided conceptual input, interpreted the findings, and contributed in significant ways to the final article.
The authors declare no conflict of interest.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
References
- Al-Swiahb JN, Huang CC, Fang FM, Chuang HC, Huang HY, Luo SD, Chen CH, Chen CM, Chien CY. Prognostic impact of p16, p53, epidermal growth factor receptor, and human papillomavirus in oropharyngeal cancer in a betel nut-chewing area. Arch Otolaryngol. 2010;136 (5:502–508. doi: 10.1001/archoto.2010.47. [DOI] [PubMed] [Google Scholar]
- Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, Westra WH, Chung CH, Jordan RC, Lu C, Kim H, Axelrod R, Silverman CC, Redmond KP, Gillison ML. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363 (1:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, Westra WH, Chung CH, Jordan RC, Lu C, Kim H, Axelrod R, Silverman CC, Redmond KP, Gillison ML. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363 (1:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begum S, Westra WH. Basaloid squamous cell carcinoma of the head and neck is a mixed variant that can be further resolved by HPV status. Am J Surg Pathol. 2008;32 (7:1044–1050. doi: 10.1097/PAS.0b013e31816380ec. [DOI] [PubMed] [Google Scholar]
- Bosch FX, Manos MM, Munoz N, Sherman M, Jansen AM, Peto J, Schiffman MH, Moreno V, Kurman R, Shah KV. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J Natl Cancer Inst. 1995;87 (11:796–802. doi: 10.1093/jnci/87.11.796. [DOI] [PubMed] [Google Scholar]
- Bosch FX, Ritter D, Enders C, Flechtenmacher C, Abel U, Dietz A, Hergenhahn M, Weidauer H. Head and neck tumor sites differ in prevalence and spectrum of p53 alterations but these have limited prognostic value. Int J Cancer. 2004;111 (4:530–538. doi: 10.1002/ijc.11698. [DOI] [PubMed] [Google Scholar]
- Braakhuis BJ, Snijders PJ, Keune WJ, Meijer CJ, Ruijter-Schippers HJ, Leemans CR, Brakenhoff RH. Genetic patterns in head and neck cancers that contain or lack transcriptionally active human papillomavirus. J Natl Cancer Inst. 2004;96 (13:998–1006. doi: 10.1093/jnci/djh183. [DOI] [PubMed] [Google Scholar]
- Charfi L, Jouffroy T, de Cremoux P, Le Peltier N, Thioux M, Freneaux P, Point D, Girod A, Rodriguez J, Sastre-Garau X. Two types of squamous cell carcinoma of the palatine tonsil characterized by distinct etiology, molecular features and outcome. Cancer Lett. 2008;260 (1–2:72–78. doi: 10.1016/j.canlet.2007.10.028. [DOI] [PubMed] [Google Scholar]
- Chenevert J, Chiosea S. Incidence of human papillomavirus in oropharyngeal squamous cell carcinomas: now and 50 years ago. Hum Pathol. 2012;43 (1:17–22. doi: 10.1016/j.humpath.2011.03.009. [DOI] [PubMed] [Google Scholar]
- Dayyani F, Etzel CJ, Liu M, Ho CH, Lippman SM, Tsao AS. Meta-analysis of the impact of human papillomavirus (HPV) on cancer risk and overall survival in head and neck squamous cell carcinomas (HNSCC) Head Neck Oncol. 2010;2:15–3284-2-15. doi: 10.1186/1758-3284-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vita V, Lawrence T, Rosenberg S, DePinho R, Weinberg R.2008DeVita, Hellman, and Rosenberg's Cancer: Principles & Principles & Practice of Oncology8th ednLippincott Williams & Wilkins: Philadelphia, USA [Google Scholar]
- Doorbar J, Quint W, Banks L, Bravo IG, Stoler M, Broker TR, Stanley MA. The biology and life-cycle of human papillomaviruses. Vaccine. 2012;30 (Suppl 5:F55–F70. doi: 10.1016/j.vaccine.2012.06.083. [DOI] [PubMed] [Google Scholar]
- El-Mofty SK, Patil S. Human papillomavirus (HPV)-related oropharyngeal nonkeratinizing squamous cell carcinoma: characterization of a distinct phenotype. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101 (3:339–345. doi: 10.1016/j.tripleo.2005.08.001. [DOI] [PubMed] [Google Scholar]
- El-Mofty SK, Zhang MQ, Davila RM. Histologic identification of human papillomavirus (HPV)-related squamous cell carcinoma in cervical lymph nodes: a reliable predictor of the site of an occult head and neck primary carcinoma. Head Neck Pathol. 2008;2 (3:163–168. doi: 10.1007/s12105-008-0066-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans MF, Matthews A, Kandil D, Adamson CS, Trotman WE, Cooper K. Discrimination of 'driver' and 'passenger' HPV in tonsillar carcinomas by the polymerase chain reaction, chromogenic in situ hybridization, and p16(INK4a) immunohistochemistry. Head Neck Pathol. 2011;5 (4:344–348. doi: 10.1007/s12105-011-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fakhry C, Gillison ML. Clinical implications of human papillomavirus in head and neck cancers. J Clin Oncol. 2006;24 (17:2606–2611. doi: 10.1200/JCO.2006.06.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farshadpour F, Konings S, Speel EJ, Hordijk GJ, Koole R, van Blokland M, Slootweg PJ, Kummer JA. Human papillomavirus and oropharyngeal squamous cell carcinoma: a case–control study regarding tobacco and alcohol consumption". Pathol Res Int. 2011;2011:806345. doi: 10.4061/2011/806345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127 (12:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- Friedland P, Thomas A, Naran A, Amanuel B, Grieu-Iacopetta F, Carrello A, Harnett G, Meyer C, Phillips M. Human papillomavirus and gene mutations in head and neck squamous carcinomas. ANZ J Surg. 2012;82 (5:362–366. doi: 10.1111/j.1445-2197.2011.05791.x. [DOI] [PubMed] [Google Scholar]
- Gao G, Chernock RD, Gay HA, Thorstad WL, Zhang TR, Wang H, Ma XJ, Luo Y, Lewis JS, Jr, Wang X. A novel RT–PCR method for quantification of human papillomavirus transcripts in archived tissues and its application in oropharyngeal cancer prognosis. Int J Cancer. 2013;132 (4:882–890. doi: 10.1002/ijc.27739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafkamp HC, Manni JJ, Haesevoets A, Voogd AC, Schepers M, Bot FJ, Hopman AH, Ramaekers FC, Speel EJ. Marked differences in survival rate between smokers and nonsmokers with HPV 16-associated tonsillar carcinomas. Int J Cancer. 2008;122 (12:2656–2664. doi: 10.1002/ijc.23458. [DOI] [PubMed] [Google Scholar]
- Hoffmann M, Tribius S, Quabius ES, Henry H, Pfannenschmidt S, Burkhardt C, Gorogh T, Halec G, Hoffmann AS, Kahn T, Rocken C, Haag J, Waterboer T, Schmitt M. HPV DNA, E6*I-mRNA expression and p16INK4A immunohistochemistry in head and neck cancer - how valid is p16INK4A as surrogate marker. Cancer Lett. 2012;323 (1:88–96. doi: 10.1016/j.canlet.2012.03.033. [DOI] [PubMed] [Google Scholar]
- Holzinger D, Schmitt M, Dyckhoff G, Benner A, Pawlita M, Bosch FX. Viral RNA patterns and high viral load reliably define oropharynx carcinomas with active HPV16 involvement. Cancer Res. 2012;72 (19:4993–5003. doi: 10.1158/0008-5472.CAN-11-3934. [DOI] [PubMed] [Google Scholar]
- Hong AM, Dobbins TA, Lee CS, Jones D, Harnett GB, Armstrong BK, Clark JR, Milross CG, Kim J, O'Brien CJ, Rose BR. Human papillomavirus predicts outcome in oropharyngeal cancer in patients treated primarily with surgery or radiation therapy. Br J Cancer. 2010;103 (10:1510–1517. doi: 10.1038/sj.bjc.6605944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Q, Yu GP, McCormick SA, Mo J, Datta B, Mahimkar M, Lazarus P, Schaffer AA, Desper R, Schantz SP. Genetic differences detected by comparative genomic hybridization in head and neck squamous cell carcinomas from different tumor sites: construction of oncogenetic trees for tumor progression. Genes Chromosomes Cancer. 2002;34 (2:224–233. doi: 10.1002/gcc.10062. [DOI] [PubMed] [Google Scholar]
- Junor E, Kerr G, Oniscu A, Campbell S, Kouzeli I, Gourley C, Cuschieri K. Benefit of chemotherapy as part of treatment for HPV DNA-positive but p16-negative squamous cell carcinoma of the oropharynx. Br J Cancer. 2012;106 (2:358–365. doi: 10.1038/bjc.2011.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Koo BS, Kang S, Park K, Kim H, Lee KR, Lee MJ, Kim JM, Choi EC, Cho NH. HPV integration begins in the tonsillar crypt and leads to the alteration of p16, EGFR and c-myc during tumor formation. Int J Cancer. 2007;120 (7:1418–1425. doi: 10.1002/ijc.22464. [DOI] [PubMed] [Google Scholar]
- Klussmann JP, Mooren JJ, Lehnen M, Claessen SM, Stenner M, Huebbers CU, Weissenborn SJ, Wedemeyer I, Preuss SF, Straetmans JM, Manni JJ, Hopman AH, Speel EJ. Genetic signatures of HPV-related and unrelated oropharyngeal carcinoma and their prognostic implications. Clin Cancer Res. 2009;15 (5:1779–1786. doi: 10.1158/1078-0432.CCR-08-1463. [DOI] [PubMed] [Google Scholar]
- Kuo KT, Hsiao CH, Lin CH, Kuo LT, Huang SH, Lin MC. The biomarkers of human papillomavirus infection in tonsillar squamous cell carcinoma-molecular basis and predicting favorable outcome. Mod Pathol. 2008;21 (4:376–386. doi: 10.1038/modpathol.3800979. [DOI] [PubMed] [Google Scholar]
- Laco J, Vosmikova H, Novakova V, Celakovsky P, Dolezalova H, Tucek L, Nekvindova J, Vosmik M, Cermakova E, Ryska A. The role of high-risk human papillomavirus infection in oral and oropharyngeal squamous cell carcinoma in non-smoking and non-drinking patients: a clinicopathological and molecular study of 46 cases". Virchows Archiv. 2011;458 (2:179–187. doi: 10.1007/s00428-010-1037-y. [DOI] [PubMed] [Google Scholar]
- Langendijk JA, Psyrri A. The prognostic significance of p16 overexpression in oropharyngeal squamous cell carcinoma: implications for treatment strategies and future clinical studies. Ann Oncol. 2010;21 (10:1931–1934. doi: 10.1093/annonc/mdq439. [DOI] [PubMed] [Google Scholar]
- Lassen P, Overgaard J. Scoring and classification of oropharyngeal carcinoma based on HPV-related p16-expression. Radiother Oncol. 2012;105 (2:269–270. doi: 10.1016/j.radonc.2012.09.017. [DOI] [PubMed] [Google Scholar]
- Leeflang MM, Deeks JJ, Takwoingi Y, Macaskill P. Cochrane diagnostic test accuracy reviews. System Rev. 2013;2 (1:82–4053-2-82. doi: 10.1186/2046-4053-2-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis JS., Jr P16 Immunohistochemistry as a standalone test for risk stratification in oropharyngeal squamous cell carcinoma. Head Neck Pathol. 2012;6 (Suppl 1:S75–S82. doi: 10.1007/s12105-012-0369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis JS, Jr, Khan RA, Masand RP, Chernock RD, Zhang Q, Al-Naief NS, Muller S, McHugh JB, Prasad ML, Brandwein-Gensler M, Perez-Ordonez B, El-Mofty SK. Recognition of nonkeratinizing morphology in oropharyngeal squamous cell carcinoma – a prospective cohort and interobserver variability study. Histopathology. 2012;60 (3:427–436. doi: 10.1111/j.1365-2559.2011.04092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis JS, Jr, Thorstad WL, Chernock RD, Haughey BH, Yip JH, Zhang Q, El-Mofty SK. P16 positive oropharyngeal squamous cell carcinoma:an entity with a favorable prognosis regardless of tumor HPV status. Am J Surg Pathol. 2010;34 (8:1088–1096. doi: 10.1097/PAS.0b013e3181e84652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Tran N, Lee SC, O'Brien CJ, Tse GM, Scolyer RA, Hong A, Milross C, Yu KH, Rose BR. New evidence for geographic variation in the role of human papillomavirus in tonsillar carcinogenesis. Pathology. 2007;39 (2:217–222. doi: 10.1080/00313020701230823. [DOI] [PubMed] [Google Scholar]
- Licitra L, Perrone F, Bossi P, Suardi S, Mariani L, Artusi R, Oggionni M, Rossini C, Cantu G, Squadrelli M, Quattrone P, Locati LD, Bergamini C, Olmi P, Pierotti MA, Pilotti S. High-risk human papillomavirus affects prognosis in patients with surgically treated oropharyngeal squamous cell carcinoma. J Clin Oncol. 2006;24 (36:5630–5636. doi: 10.1200/JCO.2005.04.6136. [DOI] [PubMed] [Google Scholar]
- Lindquist D, Ahrlund-Richter A, Tarjan M, Tot T, Dalianis T. Intense CD44 expression is a negative prognostic factor in tonsillar and base of tongue cancer. Anticancer Res. 2012;32 (1:153–161. [PubMed] [Google Scholar]
- Marur S, D'Souza G, Westra WH, Forastiere AA. HPV-associated head and neck cancer: a virus-related cancer epidemic. Lancet Oncol. 2010;11 (8:781–789. doi: 10.1016/S1470-2045(10)70017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellin Dahlstrand H, Lindquist D, Bjornestal L, Ohlsson A, Dalianis T, Munck-Wikland E, Elmberger G. P16(INK4a) correlates to human papillomavirus presence, response to radiotherapy and clinical outcome in tonsillar carcinoma. Anticancer Res. 2005;25 (6C:4375–4383. [PubMed] [Google Scholar]
- Mills AM, Beck AH, Pourmand N, Le QT, Kong CS. Evaluation of ProExC as a prognostic marker in oropharyngeal squamous cell carcinomas. Am J Surg Pathol. 2012;36 (8:1158–1164. doi: 10.1097/PAS.0b013e3182600eaa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols AC, Faquin WC, Westra WH, Mroz EA, Begum S, Clark JR, Rocco JW. HPV-16 infection predicts treatment outcome in oropharyngeal squamous cell carcinoma. Otolaryngology. 2009;140 (2:228–234. doi: 10.1016/j.otohns.2008.11.025. [DOI] [PubMed] [Google Scholar]
- O'Rorke MA, Ellison MV, Murray LJ, Moran M, James J, Anderson LA. Human papillomavirus related head and neck cancer survival: a systematic review and meta-analysis. Oral oncology. 2012;48 (12:1191–1201. doi: 10.1016/j.oraloncology.2012.06.019. [DOI] [PubMed] [Google Scholar]
- Park WS, Ryu J, Cho KH, Choi MK, Moon SH, Yun T, Chun BS, Lee GK, Ahn HJ, Lee JH, Vermeer P, Jung YS. Human papillomavirus in oropharyngeal squamous cell carcinomas in Korea: use of G1 cycle markers as new prognosticators. Head Neck. 2012;34 (10:1408–1417. doi: 10.1002/hed.21939. [DOI] [PubMed] [Google Scholar]
- Preuss SF, Weinell A, Molitor M, Stenner M, Semrau R, Drebber U, Weissenborn SJ, Speel EJ, Wittekindt C, Guntinas-Lichius O, Hoffmann TK, Eslick GD, Klussmann JP. Nuclear survivin expression is associated with HPV-independent carcinogenesis and is an indicator of poor prognosis in oropharyngeal cancer. Br J Cancer. 2008;98 (3:627–632. doi: 10.1038/sj.bjc.6604192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quon H, Cohen MA, Montone KT, Ziober AF, Wang LP, Weinstein GS, O'Malley BW. Transoral robotic surgery and adjuvant therapy for oropharyngeal carcinomas and the influence of p16 INK4a on treatment outcomes. Laryngoscope. 2013;123 (3:635–640. doi: 10.1002/lary.22172. [DOI] [PubMed] [Google Scholar]
- Reimers N, Kasper HU, Weissenborn SJ, Stutzer H, Preuss SF, Hoffmann TK, Speel EJ, Dienes HP, Pfister HJ, Guntinas-Lichius O, Klussmann JP. Combined analysis of HPV-DNA, p16 and EGFR expression to predict prognosis in oropharyngeal cancer. Int J Cancer. 2007;120 (8:1731–1738. doi: 10.1002/ijc.22355. [DOI] [PubMed] [Google Scholar]
- Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58 (10:982–990. doi: 10.1016/j.jclinepi.2005.02.022. [DOI] [PubMed] [Google Scholar]
- Robinson M, Sloan P, Shaw R. Refining the diagnosis of oropharyngeal squamous cell carcinoma using human papillomavirus testing. Oral Oncol. 2010;46 (7:492–496. doi: 10.1016/j.oraloncology.2010.02.013. [DOI] [PubMed] [Google Scholar]
- Schache AG, Liloglou T, Risk JM, Filia A, Jones TM, Sheard J, Woolgar JA, Helliwell TR, Triantafyllou A, Robinson M, Sloan P, Harvey-Woodworth C, Sisson D, Shaw RJ. Evaluation of human papilloma virus diagnostic testing in oropharyngeal squamous cell carcinoma: sensitivity, specificity, and prognostic discrimination. Clin Cancer Res. 2011;17 (19:6262–6271. doi: 10.1158/1078-0432.CCR-11-0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schache AG, Liloglou T, Risk JM, Filia A, Jones TM, Sheard J, Woolgar JA, Helliwell TR, Triantafyllou A, Robinson M, Sloan P, Harvey-Woodworth C, Sisson D, Shaw RJ. Evaluation of human papilloma virus diagnostic testing in oropharyngeal squamous cell carcinoma: sensitivity, specificity, and prognostic discrimination. Clin Cancer Res. 2011;17 (19:6262–6271. doi: 10.1158/1078-0432.CCR-11-0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semrau R, Duerbaum H, Temming S, Huebbers C, Stenner M, Drebber U, Klussmann JP, Muller RP, Preuss SF. Prognostic impact of human papillomavirus status, survivin, and epidermal growth-factor receptor expression on survival in patients treated with radiochemotherapy for very advanced nonresectable oropharyngeal cancer. Head Neck. 2012;35 (9:1339–1344. doi: 10.1002/hed.23126. [DOI] [PubMed] [Google Scholar]
- Shah J, Patel K.2003Head and Neck Surgery and Oncology3 ednMoosby Ltd: Edinburgh [Google Scholar]
- Shi W, Kato H, Perez-Ordonez B, Pintilie M, Huang S, Hui A, O'Sullivan B, Waldron J, Cummings B, Kim J, Ringash J, Dawson LA, Gullane P, Siu L, Gillison M, Liu FF. Comparative prognostic value of HPV16 E6 mRNA compared with in situ hybridization for human oropharyngeal squamous carcinoma. J Clin Oncol. 2009;27 (36:6213–6221. doi: 10.1200/JCO.2009.23.1670. [DOI] [PubMed] [Google Scholar]
- Smeets SJ, Hesselink AT, Speel EJ, Haesevoets A, Snijders PJ, Pawlita M, Meijer CJ, Braakhuis BJ, Leemans CR, Brakenhoff RH. A novel algorithm for reliable detection of human papillomavirus in paraffin embedded head and neck cancer specimen. Int J Cancer. 2007;121 (11:2465–2472. doi: 10.1002/ijc.22980. [DOI] [PubMed] [Google Scholar]
- Thavaraj S, Stokes A, Guerra E, Bible J, Halligan E, Long A, Okpokam A, Sloan P, Odell E, Robinson M. Evaluation of human papillomavirus testing for squamous cell carcinoma of the tonsil in clinical practice. J Clin Pathol. 2011;64 (4:308–312. doi: 10.1136/jcp.2010.088450. [DOI] [PubMed] [Google Scholar]
- Ukpo OC, Flanagan JJ, Ma XJ, Luo Y, Thorstad WL, Lewis JS., Jr High-risk human papillomavirus E6/E7 mRNA detection by a novel in situ hybridization assay strongly correlates with p16 expression and patient outcomes in oropharyngeal squamous cell carcinoma. Am J Surg Pathol. 2011;35 (9:1343–1350. doi: 10.1097/PAS.0b013e318220e59d. [DOI] [PubMed] [Google Scholar]
- Ukpo OC, Thorstad WL, Zhang Q, Lewis JS., Jr Lack of association of cadherin expression and histopathologic type, metastasis, or patient outcome in oropharyngeal squamous cell carcinoma: a tissue microarray study. Head Neck Pathol. 2012;6 (1:38–47. doi: 10.1007/s12105-011-0306-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger PM, Merkley MA, Khichi SS, Lee JR, Psyrri A, Jackson LL, Dynan WS. Human papillomavirus-active head and neck cancer and ethnic health disparities. Laryngoscope. 2010;120 (8:1531–1537. doi: 10.1002/lary.20984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D, Koopmann M, Basel T, Rudack C. Cyclin A1 shows age-related expression in benign tonsils, HPV16-dependent overexpression in HNSCC and predicts lower recurrence rate in HNSCC independently of HPV16. BMC Cancer. 2012;12:259–2407-12-259. doi: 10.1186/1471-2407-12-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westra WH. The morphologic profile of HPV-related head and neck squamous carcinoma: implications for diagnosis, prognosis, and clinical management. Head Neck Pathol. 2012;6 (Suppl 1:S48–S54. doi: 10.1007/s12105-012-0371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westra WH. The changing face of head and neck cancer in the 21st century: the impact of HPV on the epidemiology and pathology of oral cancer. Head Neck Pathol. 2009;3 (1:78–81. doi: 10.1007/s12105-009-0100-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao N, Ang MK, Yin XY, Patel MR, Fritchie K, Thorne L, Muldrew KL, Hayward MC, Sun W, Wilkerson MD, Chera BS, Hackman T, Zanation AM, Grilley-Olson JE, Couch ME, Shockley WW, Weissler MC, Shores CG, Funkhouser WK, Olshan AF, Hayes DN. Different cellular p16(INK4a) localisation may signal different survival outcomes in head and neck cancer. Br J Cancer. 2012;107 (3:482–490. doi: 10.1038/bjc.2012.264. [DOI] [PMC free article] [PubMed] [Google Scholar]