Abstract
Determinants of cancer progression and survival are multifactorial and host responses are increasingly appreciated to have a major role. Indeed, the development and maintenance of a systemic inflammatory response has been consistently observed to confer poorer outcome, in both early and advanced stage disease. For patients, cancer-associated symptoms are of particular importance resulting in a marked impact on day-to-day quality of life and are also associated with poorer outcome. These symptoms are now recognised to cluster with one another with anorexia, weight loss and physical function forming a recognised cluster whereas fatigue, pain and depression forming another. Importantly, it has become apparent that these symptom clusters are associated with presence of a systemic inflammatory response in the patient with cancer. Given the understanding of the above, there is now a need to intervene to moderate systemic inflammatory responses, where present. In this context the rationale for therapeutic intervention using nonselective anti-inflammatory agents is clear and compelling and likely to become a part of routine clinical practice in the near future. The published literature on therapeutic intervention using anti-inflammatory agents for cancer-associated symptoms was reviewed. There are important parallels with the development of useful treatments for the systemic inflammatory response in patients with rheumatological disease and cardiovascular disease.
Keywords: systemic inflammation, appetite loss, cachexia, physical function, pain, fatigue, depression, anti-inflammatory agents
Although the mechanisms determining cancer progression continue to be of intense interest to scientists and treatments to oncologists, it is the symptoms associated with cancer progression that are of most interest to patients. In particular, progressive appetite loss, weight (lean tissue) loss, fatigue and pain are extremely debilitating not only impacting on quality of life but also the response to treatment and survival. However, despite their importance, research into symptoms associated with cancer has not been given a high priority by either scientists or clinicians. For example, MacDonald (2007) pointed out that ‘the number of abstracts on all aspects of cancer nutrition totalled 15 out of 4917 papers and posters presented at the 2005 Annual Meeting of the American Society of Clinical Oncology (ASCO); in contrast there were 106 presentations on gemcitabine (Gemzar) alone. No progress on this front was evident at the 2006 ASCO meeting, when the score for nutrition was 10, gemcitabine 86'.
In recent years the importance of the inflammatory responses in determining disease progression in patients with cancer has become recognised (Hanahan and Weinberg, 2011) and has become a hot topic for scientists and clinicians with the terms cancer and inflammation returning 1179 articles in 2002 compared with 3693 articles in 2012 (http://www.ncbi.nlm.nih.gov/pubmed/?term=cancer+and+inflammation). Despite the increasing interest, there remains a paucity of clinical studies showing how such new information might improve the treatment of symptoms in the cancer patient.
For a long time, there have been suspicions that cancer-associated symptoms, in particular the progressive loss of weight and lean tissue, are manifestations of a chronic ongoing systemic inflammatory response. Indeed, some early randomised clinical trial data were consistent with this concept (Lundholm et al, 1994; McMillan et al, 1999) and provoked reviews to call for further work on this hypothesis (MacDonald, 2007; McMillan, 2008).
In addition to clear associations with individuals symptoms and poorer outcome, cancer-associated systemic inflammation is likely to mitigate administration of other effective treatments. For example, the efficacy of many current chemotherapeutics are reliant on metabolic clearance by hepatic cytochrome P450 enzymes, a process which is known to be hindered by ongoing systemic inflammation, potentially resulting in treatment toxicity or failure (Kacevska et al, 2008). Therefore, it is logical that there should be a stratification on the basis of systemic inflammatory response measurement within randomised clinical trials of cancer therapeutics (McMillan, 2013b).
The aim of the present minireview was to examine the evidence in the last decade for the association of the systemic inflammatory response with the range of symptoms including appetite loss, weight loss, fatigue and pain and identify a rational clinical approach to moderate the systemic inflammatory response and reduce symptoms experienced in patients with cancer.
Measurement of the systemic inflammatory response
Although activation of the systemic inflammatory response involves many organ systems, the usual clinical laboratory measures of the magnitude of activation are circulating white cells and acute phase proteins (Gabay and Kushner, 1999). Over the last decade it has become clear that such measurements of an elevated systemic inflammatory response are consistently associated with poor outcome independent of tumour stage. In particular, white cell counts such as neutrophil, lymphocyte and platelet counts and acute phase proteins, such as C-reactive protein and albumin and their combinations, neutrophil lymphocyte ratio (NLR), platelet lymphocyte ratio (PLR) and Glasgow Prognostic Score (GPS) respectively have been reported repeatedly to have prognostic value (Roxburgh and McMillan, 2010; Guthrie et al, 2013; McMillan, 2013a). For example, over the last decade, more than 120 studies (>60 000 patients) have examined the clinical utility of the NLR and/or the GPS to predict patient outcomes in a variety of cancers. Taken together, these systemic inflammation-based scores can be considered to represent an upregulation of the innate immune/inflammatory responses. Irrespective of this, these comprehensive and compelling data have resulted in calls for such systemic inflammation-based prognostic scores to be routinely incorporated into clinical care to improve treatment allocation and the design of randomised clinical trials (McMillan, 2013b; Douglas and McMillan, 2013).
Relationship between systemic inflammatory response, symptom clusters and survival
Symptoms associated with cancer are commonly regarded as natural sequelae to the progression of cancer, that is, due to the tumour burden. However, it has long been recognised that progressive involuntary loss of appetite, weight and physical function are features of advanced disease and aggressive types of tumour such as lung and pancreatic cancer, independent of the tumour stage. Similarly, fatigue, pain and depression are all features of advanced disease. Indeed, in the last decade it has become clear that the common symptoms such as appetite loss, weight loss, physical functioning and fatigue and pain are independently associated with survival in patients with advanced disease (Trajkovic-Vidakovic et al, 2012; Laird et al, 2013a).
Also, there is now a great deal of evidence, at least in animal models, of the role of pro-inflammatory cytokines in producing sickness behaviour that recapitulates many of the symptoms seen in patients with cancer (Illi et al, 2012). Finally, consistent with this concept is that symptoms in patients with cancer rarely exist in isolation but most occur in clusters, three or more symptoms that are related to each other (Kirkova et al, 2010). In particular, there are multiple reports that appetite loss, weight loss and physical function are a symptom cluster (Solheim et al, 2013a) and that fatigue, pain and depression are another (Laird et al, 2011) in patients with cancer. These symptom clusters may be considered to represent in part a neurological response to upregulation of the innate immune response (Dantzer, 2004). Observations that advanced disease and aggressive tumours, such as lung and pancreatic cancer, are associated with a greater activation of the systemic inflammatory response compared with tumours in which symptom clusters are rarely seen, such as breast cancer (Proctor et al, 2010), are consistent with this concept.
Recently in a large international cohort of advanced cancer patients (n=1466), Laird et al (2013b) reported that C-reactive protein was significantly associated with all of the function components of the EORTC QLQ-C30 including cognitive, physical, role, emotional and social. There was also a significant association with appetite loss, pain and fatigue. However, it remains to be clearly established that reduction of markers of the systemic inflammatory response will be accompanied by a clinically relevant improvement in symptoms and survival.
Conclusion
The importance of treating cancer-associated symptoms has recently been highlighted to oncologists with evidence that that the administration of routine chemotherapy protocols are associated with a significant 30-day mortality (NCEPOD, Systemic Anti-Cancer Therapy: For better, for worse?; http://www.ncepod.org.uk/2008sact.htm). Furthermore, that early referral to palliative care for symptom control was associated with not only an improvement in quality of life but also an improvement in survival compared with standard care in patients with advanced non-small cell lung cancer (Temel et al, 2010).
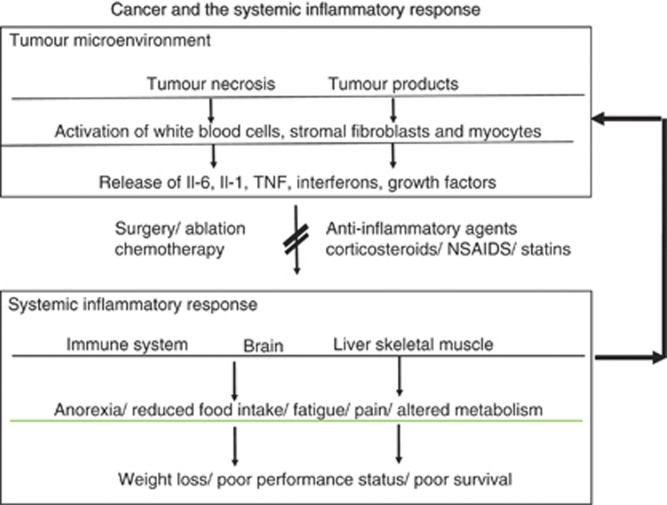
The above literature shows a clear association between the systemic inflammatory response and cancer-associated symptoms (see Figure 1 and also in more detail Saligan and Kim, 2012). Given that activation of the systemic inflammatory response for most patients is chronic and unremitting, this raises the issue of how might it be moderated to ameliorate symptoms in the patient with cancer.
Figure 1.
The relationship between the tumour microenvironment and the host systemic inflammatory response: treat the tumour and treat the host.
Treatment of cancer-associated symptoms in patients with anti-inflammatory agents
Owing to the myriad effects of the systemic inflammatory response in patients with cancer and the established anti-cancer treatments, it is likely that those anti-inflammatory agents most likely to make their way into routine clinical practice in the short term (5–10 years) will be those agents that have a broad brush anti-inflammatory action and have a low or well-documented side-effect profile and readily used alongside standard cancer treatments (some currently used due to comorbid disease). The use of such anti-inflammatory agents will be guided by measures of the systemic inflammatory response as described above.
Corticosteroids
Corticosteroids are known to reduce the systemic inflammatory response, at least in the short term and are frequently prescribed in advanced cancer for symptom control. For example, a survey from the USA reported that 33% oncologists prescribe steroids in the end-of-life care (www.nccn.org, 2013). Moreover, they have been subject to at least six controlled trials accounting for more than 1000 patients and have been shown to improve appetite and quality of life if only for a limited time of a few weeks. A recent placebo-controlled trial demonstrated that dexamethasone 4 mg per day administered to advanced cancer patients for just two weeks resulted in significant improvements in cancer-related symptoms (weight loss, anxiety, fatigue, pain, nausea, anorexia and depression, Yennurajalingam et al, 2013). However, unlike other chronic inflammatory diseases, for example, rheumatoid arthritis, as these drugs have been given empirically in cancer and not specifically tailored to moderate the systemic inflammatory response (e.g., C-reactive protein, GPS, NLR or PLR), it is not clear which corticosteroid should be used nor the amount and timing of the dosage for optimal and continued reduction of the systemic inflammatory response.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Aspirin and other NSAIDs inhibit the enzyme cyclooxygenase and the production of prostaglandins that result in inflammatory responses and pain. These are used extensively in the populations of the western world. There has been a longstanding interest in the use of NSAIDs in the treatment of cancer-associated symptoms (Lundholm et al, 1994; McMillan et al, 1999). More recently, there has been further work that supports the routine use of NSAIDs in treating the most troublesome symptoms associated with cancer (Madeddu et al, 2012). Solheim et al (2013b) in a recent systematic review (including 13 controlled trials of NSAIDS in advanced cancer), reported that 11 studies reported a slowing of weight loss with 4 studies demonstrating a reduction in measures of systemic inflammation. There was also evidence that NSAIDs may improve physical function and patient-reported quality of life and reduce markers of the systemic inflammatory response.
Together with well-defined systemic inflammatory response parameters, the broad-spectrum anti-inflammatory properties of NSAIDs along with their relatively mild side-effect profiles in patients, make them good agents for the manipulation of cancer-associated inflammation with or without gastro-protection. Furthermore, with recent studies demonstrating positive survival outcomes with aspirin use following surgery for colorectal cancer dependent on tumour molecular phenotypes (Liao et al, 2012) and similar work in breast cancer, the role of aspirin/NSAID treatment looks set to expand to early-stage disease. However, it is not clear which NSAID should be used nor the amount and timing of the dosage for optimal and continued reduction of the systemic inflammatory response.
Statins
Statins are HMG-CoA reductase inhibitors that have had a major beneficial impact on the natural history of coronary artery disease in humans. Beyond their cholesterol-lowering properties, statins exhibit important anti-inflammatory activities (Jain and Ridker, 2005). For example, in randomised clinical trials, moderation of the systemic inflammatory response using a statin has been clearly associated with improved outcomes (Ridker et al, 2008). Furthermore, favourable effects on organ rejection following heart and renal transplant confirm an important immunomodulatory effect. Also, similar to NSAIDs, long-term statin use before cancer diagnosis is associated with significantly lower-stage tumours and better long-term survival (e.g., Ng et al, 2011).
Conclusion
From the above, therapeutic intervention using nonselective anti-inflammatory agents has considerable potential to ameliorate the symptoms associated with cancer and therefore the potential to improve the quality and quantity of life in these patients. Indeed, when commenting on the role of NSAIDs in cancer cachexia Christoffersen (2013) recently stated, ‘It is hard to avoid noting the striking contrast between the enormous efforts and resources spent on developing novel and very expensive drugs targeted at signalling pathways, many of which have turned out to have only marginal effects, and the lack of good studies trying out the effects of relatively cheap drugs.'
The current evidence base is such that, in the absence of definitive mechanisms, the clinical use of the nonselective anti-inflammatory agents discussed above should be considered in patients with cancer-associated symptoms and who have a measurement of an elevated systemic inflammatory response. There will remain concerns about the well-documented side effects of routine use of nonselective anti-inflammatory agents, in particular NSAIDs. However, these should be considered against the severity of the symptoms and poor outcome associated with a chronic systemic inflammatory state. Furthermore, the effectiveness of their use is now readily monitored. Therefore, it can be readily envisaged that, with monitoring of their anti-inflammatory effect and potential side effects, such anti-inflammatory agents can be used alongside standard anti-tumour treatment hence the title of the present review. Such work should stimulate a new era of randomised controlled trials of broad-spectrum anti-inflammatory agents to provide definitive clinical protocols to improve the quantity and quality of life of the patient with cancer.
References
- Christoffersen T. Cancer, cachexia, prostanoids, and NSAIDs. Acta Oncol. 2013;52:3–5. doi: 10.3109/0284186X.2012.750429. [DOI] [PubMed] [Google Scholar]
- Dantzer R. Cytokine-induced sickness behaviour: a neuroimmune response to activation of innate immunity. Eur J Pharmacol. 2004;500 (1–3:399–411. doi: 10.1016/j.ejphar.2004.07.040. [DOI] [PubMed] [Google Scholar]
- Douglas E, McMillan DC.2013Towards a simple objective framework for the investigation and treatment of cancer cachexia: The Glasgow Prognostic Score Cancer Treat Reve-pub ahead of print 28 November 2013; doi: 10.1016/j.ctrv.2013.11.007 [DOI] [PubMed]
- Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340 (6:448–454. doi: 10.1056/NEJM199902113400607. [DOI] [PubMed] [Google Scholar]
- Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013;88 (1:218–230. doi: 10.1016/j.critrevonc.2013.03.010. [DOI] [PubMed] [Google Scholar]
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Illi J, Miaskowski C, Cooper B, Levine JD, Dunn L, West C, Dodd M, Dhruva A, Paul SM, Baggott C, Cataldo J, Langford D, Schmidt B, Aouizerat BE. Association between pro- and anti-inflammatory cytokine genes and a symptom cluster of pain, fatigue, sleep disturbance, and depression. Cytokine. 2012;58:437–447. doi: 10.1016/j.cyto.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain MK, Ridker PM. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov. 2005;4 (12:977–987. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- Kacevska M, Robertson GR, Clarke SJ, Liddle C. Inflammation and CYP3A4-mediated drug metabolism in advanced cancer: impact and implications for chemotherapeutic drug dosing. Expert Opin Drug Metab Toxicol. 2008;4:137–149. doi: 10.1517/17425255.4.2.137. [DOI] [PubMed] [Google Scholar]
- Kirkova J, Walsh D, Aktas A, Davis MP. Cancer symptom clusters: old concept but new data. Am J Hosp Palliat Care. 2010;27:282–288. doi: 10.1177/1049909110364048. [DOI] [PubMed] [Google Scholar]
- Laird BJ, Kaasa S, McMillan DC, Fallon MT, Hjermstad MJ, Fayers P, Klepstad P. Prognostic factors in patients with advanced cancer: a comparison of clinicopathological factors and the development of an inflammation-based prognostic system. Clin Cancer Res. 2013;19:5456–5464. doi: 10.1158/1078-0432.CCR-13-1066. [DOI] [PubMed] [Google Scholar]
- Laird BJ, McMillan DC, Fayers P, Fearon K, Kaasa S, Fallon MT, Klepstad P. The systemic inflammatory response and its relationship to pain and other symptoms in advanced cancer. Oncologist. 2013;18 (9:1050–1055. doi: 10.1634/theoncologist.2013-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird BJ, Scott AC, Colvin LA, McKeon AL, Murray GD, Fearon KC, Fallon MT. Pain, depression, and fatigue as a symptom cluster in advanced cancer. J Pain Symptom Manage. 2011;42:1–11. doi: 10.1016/j.jpainsymman.2010.10.261. [DOI] [PubMed] [Google Scholar]
- Liao X, Lochhead P, Nishihara R, Morikawa T, Kuchiba A, Yamauchi M, Imamura Y, Qian ZR, Baba Y, Shima K, Sun R, Nosho K, Meyerhardt JA, Giovannucci E, Fuchs CS, Chan AT, Ogino S. Aspirin use, tumor PIK3CA mutation, and colorectal-cancer survival. N Engl J Med. 2012;367 (17:1596–1606. doi: 10.1056/NEJMoa1207756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundholm K, Gelin J, Hyltander A, Lönnroth C, Sandström R, Svaninger G, Körner U, Gülich M, Kärrefors I, Norli B, et al. Anti-inflammatory treatment may prolong survival in undernourished patients with metastatic solid tumors. Cancer Res. 1994;54:5602–5606. [PubMed] [Google Scholar]
- MacDonald N. Cancer cachexia and targeting chronic inflammation: a unified approach to cancer treatment and palliative/supportive care. J Support Oncol. 2007;5:157–162. [PubMed] [Google Scholar]
- Madeddu C, Dessì M, Panzone F, Serpe R, Antoni G, Cau MC, Montaldo L, Mela Q, Mura M, Astara G, Tanca FM, Macciò A, Mantovani G. Randomized phase III clinical trial of a combined treatment with carnitine+celecoxib±megestrol acetate for patients with cancer-related anorexia/cachexia syndrome. Clin Nutr. 2012;31:176–182. doi: 10.1016/j.clnu.2011.10.005. [DOI] [PubMed] [Google Scholar]
- McMillan DC. An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc. 2008;67:257–262. doi: 10.1017/S0029665108007131. [DOI] [PubMed] [Google Scholar]
- McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39:534–540. doi: 10.1016/j.ctrv.2012.08.003. [DOI] [PubMed] [Google Scholar]
- McMillan DC. Cancer and systemic inflammation: stage the tumour and stage the host. Br J Cancer. 2013;109:529. doi: 10.1038/bjc.2013.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillan DC, Wigmore SJ, Fearon KC, O'Gorman P, Wright CE, McArdle CS. A prospective randomized study of megestrol acetate and ibuprofen in gastrointestinal cancer patients with weight loss. Br J Cancer. 1999;79:495–500. doi: 10.1038/sj.bjc.6690077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng K, Ogino S, Meyerhardt JA, Chan JA, Chan AT, Niedzwiecki D, Hollis D, Saltz LB, Mayer RJ, Benson AB, 3rd, Schaefer PL, Whittom R, Hantel A, Goldberg RM, Bertagnolli MM, Venook AP, Fuchs CS. Relationship between statin use and colon cancer recurrence and survival: results from CALGB 89803. J Natl Cancer Inst. 2011;103:1540–1551. doi: 10.1093/jnci/djr307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor MJ, Talwar D, Balmar SM, O'Reilly DS, Foulis AK, Horgan PG, Morrison DS, McMillan DC. The relationship between the presence and site of cancer, an inflammation-based prognostic score and biochemical parameters. Initial results of the Glasgow Inflammation Outcome Study. Br J Cancer. 2010;103 (6:870–876. doi: 10.1038/sj.bjc.6605855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ, JUPITER Study Group Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6:149–163. doi: 10.2217/fon.09.136. [DOI] [PubMed] [Google Scholar]
- Saligan LN, Kim HS. A systematic review of the association between immunogenomic markers and cancer-related fatigue. Brain Behav Immun. 2012;26:830–848. doi: 10.1016/j.bbi.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solheim TS, Fearon KC, Blum D, Kaasa S. Non-steroidal anti-inflammatory treatment in cancer cachexia: a systematic literature review. Acta Oncol. 2013;52:6–17. doi: 10.3109/0284186X.2012.724536. [DOI] [PubMed] [Google Scholar]
- Solheim TS, Blum D, Fayers PM, Hjermstad MJ, Stene GB, Strasser F, Kaasa S.2013Weight loss, appetite loss and food intake in cancer patients with cancer cachexia: three peas in a pod? - analysis from a multicenter cross sectional study Acta Oncole-pub ahead of print 2 September 2013. [DOI] [PubMed]
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF, Billings JA, Lynch TJ. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- Trajkovic-Vidakovic M, de Graeff A, Voest EE, Teunissen SC. Symptoms tell it all: a systematic review of the value of symptom assessment to predict survival in advanced cancer patients. Crit Rev Oncol Hematol. 2012;84:130–148. doi: 10.1016/j.critrevonc.2012.02.011. [DOI] [PubMed] [Google Scholar]
- Yennurajalingam S, Frisbee-Hume S, Palmer JL, Delgado-Guay MO, Bull J, Phan AT, Tannir NM, Litton JK, Reddy A, Hui D, Dalal S, Massie L, Reddy SK, Bruera E. Reduction of cancer-related fatigue with dexamethasone: a double-blind, randomized, placebo-controlled trial in patients with advanced cancer. J Clin Oncol. 2013;31 (25:3076–3082. doi: 10.1200/JCO.2012.44.4661. [DOI] [PubMed] [Google Scholar]