Key messages
Children who are more unwell are likely to be seen by general practice staff in some of the proposed new models of care.
Training courses and resources are widely available.
Anticipation of and preparation for such events are key.
Why this matters to me
General practitioners, nurse practitioners and other members of primary care teams see a large number of infants and young children in the course of their work. This proportion will increase as new models evolve across the country with GPs (general practitioners) running Urgent Care Centres and with more acute care taking place outside hospital settings. When a health professional is able to identify a sick child and give or refer for early urgent treatment, the outcomes of critically ill children are improved.
Keywords: anaphylaxis, asthma, bronchiolitis, choking, croup, dehydration, emergencies, feverish illness, meningococcal septicaemia, non-blanching rash, pneumonia, urgent care
Abstract
Managing the unwell child can be a frightening experience for everyone involved. As GPs become more involved in delivery of care in Urgent Care Centres and Emergency Units, it is more likely that they will come across a child who is sicker than those attending the surgery. This article will help the GP and the rest of the team to be prepared for this situation – to identify the unwell infant or toddler, to know general management principles and some specific treatment pathways for common emergencies and to take steps to try and prevent children becoming critically ill wherever possible.
Local management pathways may vary so please refer to your local guidelines. Advice from national bodies such as the UK Resuscitation Council, the Advanced Life Support Group and the British National Formulary for Children has been included. Please revisit these resources for updated material.
Prevention and preparation
Prevention
General practitioners (GPs) play a vital role in helping parents cope with their unwell child and, for children with a long-term condition, advising when and how to seek professional help both in and out of hours. Ongoing management should include regular monitoring and continued health education with the aim of preventing episodes of severe illness. This is particularly true of children with, for example, asthma, allergies, diabetes and epilepsy. It is also vital that children who do not attend for their hospital review are monitored and that parents are supported and encouraged to bring their child for review, whether this is within a primary care or hospital setting. There is scope for preventing acute hospital attendance through a greater focus on parent and child education.
Some children with chronic illness are given a ‘passport’ by the paediatric department which gives them rapid access to the paediatric team in the emergency department or direct access to the paediatric assessment unit.
Prevention may include ensuring that school staff are able to respond to a child becoming unwell. Many paediatric departments, children's community nurses and school health advisors are happy to train school staff in the use of injectable adrenaline, on how to respond to diabetic emergencies or seizures, or on how to administer bronchodilators, for example.
Preparation – of own facilities and receiving team in hospital
This encompasses ensuring that both staff in the surgery and the environment and equipment are always ready to receive a sick child.
It includes having rapid access numbers to local paediatric secondary care facilities, as a call to alert a receiving team about a sick child helps with the preparations needed at the hospital.
Recommended equipment and drugs for the surgery and emergencies bag
Oximeters with paediatric sensors are increasingly being used in general practice to enable oxygen saturations to be included as part of the clinical assessment of all sick patients.
A useful summary of recommended equipment and medicines can be found at: www.patient.co.uk/doctor/The-Doctor's-Bag-Contents.htm1
Identification of sick children
As children are difficult to assess and may be more unwell than they appear, a face-to-face assessment which includes an examination is advised.
The identification of an unwell child can be difficult for those not used to examining babies or children. However, using a consistent checklist to make your assessment based on physiology can provide important pointers that a child may be compensating and is more unwell than they seem. Assessment is easier in a child-friendly environment and with the use of age-appropriate distractions to help make the examination go more smoothly.
Unlike adults, about whom the majority of information is obtained from the history, with children observation and examination play a larger role. However a parent's concern that their child is ‘just not right’ should always be taken seriously and a full clinical examination made.
Information on managing unwell children is incorporated as part of NICE guidance provided on the management of Feverish Illness in Children.2 This attempts to categorise children under five years into a red, amber and green system, with appropriate associated action in terms of either referring onto hospital or management within a primary care setting.
A more practical guide for identifying those children that are unwell is available from the the Spotting the Sick Child website,3 which gives advice on under-taking a quick but thorough ‘top to toe’ examination with children.
Three-minute toolkit (reproduced with permission)
Observing
The child's behaviour and colour can be assessed from a distance. Record what the child is actually doing.
Observation can also include counting the respiratory rate and looking for any evidence of rash, recession or nasal flaring before touching the child. Listen for respiratory noises such as audible wheeze, stridor or grunting.
Once the child is more accustomed to you, take their hand and note the temperature, pulse and capillary refill time. Measure oxygen saturations in any child with signs of respiratory distress or shock.
Listen to the breath sounds at the front and back of the chest.
Feel the abdomen, if need be with the child on the parent's lap.
Take the child's temperature.
Examine the ears and throat (see Table 1).
Table 1.
ABCDENTTT checklist
| General |
| Behaviour – normal/lively/irritable/lethargic |
| Colour |
| Airway |
| Stridor |
| Noisy breathing |
| Drooling |
| Breathing |
| Recession/accessory muscles |
| Respiratory rate |
| Auscultation |
| Oxygen saturations |
| Circulation |
| Peripheral temperature and colour |
| Pulse |
| Capillary refill |
| Blood pressure |
| Disability |
| Alert |
| Voice only |
| Pain only |
| Unresponsive |
| ENT |
| Ears and throat |
| Temperature |
| Tympanic or axillary |
| Tummy |
| Abdominal examination |
Some of the pitfalls in assessing children arise because they can deteriorate very quickly. This relates to their young, responsive vasculature which maintains the circulation at the expense of heart rate and respiratory rate up to the point of near collapse.
The clues are often in the raised heart rate and respiratory rate and so being familiar with the normal values for different ages is important (see Table 2).
Table 2.
Table of normal values of vital signs for children
| Age (years) | Respiratory rate (breaths per minute) | Heart rate (beats per minute) | Systolic BP (mmHg) |
|---|---|---|---|
| Neonate | 60 | 160 | 70 |
| <1 | 35–45 | 110–160 | 75 |
| 1–5 | 25–35 | 95–140 | 80–90 |
| 5–12 | 20–25 | 80–120 | 90–110 |
| >12 | 15–20 | 60–100 | 100–120 |
Children can also fluctuate with periods of seemingly near normal activity but then rapid tiring. Some wheezy children appear to tolerate moderate wheeze very well, for example, but they may have reduced oxygen saturations.
The use of pulse oximetry in primary care is increasing and provides an extremely valuable part of the assessment of an ill child.
Courses available and other resources
There are various taught courses to assist non-paediatric trained staff to identify sick babies and children. Paediatric Immediate Life Support is a one-day course to enable participants to: recognise the seriously ill child and initiate appropriate interventions to prevent cardio-respiratory arrest; or to treat the child in respiratory or cardio-respiratory arrest for the short time before the arrival of a resuscitation team or more experienced assistance. See www.resus.org.uk/pages/pilscntr.pdf for centres offering the course and their contact details.
Paediatric Advanced Life Support runs over two days. See www.alsg.org for more information and details of courses.
Another very useful resource is the Spotting the Sick Child DVD or Spotting the Sick Child website mentioned above (www.spottingthesickchild.com). Spotting the Sick Child is a new interactive tool commissioned by the Department of Health to support health professionals in the assessment of the acutely sick child. It concentrates on the seven most common acute presentations (breathing difficulties, fever, rash, fits, dehydration, abdominal pain and head injury).
It covers ‘Basic child assessment’ and ‘Symptoms’ and includes teaching video clips and interactive scenarios for self assessment.
General management
This will always focus on airway–breathing–circulation (ABC) and reassessment of ABC. It is essential that the airway is adequately assessed and high flow oxygen is given before continuing to breathing and circulation. It is also important to check the blood glucose level.
If the child is not improving, keep going back to ABC.
Specific management
Difficulty breathing
Asthma
Please also refer to the British Thoracic Society Guidelines, from which the information in Table 3 is taken.4
Table 3.
Acute asthma in children over two years
| Acute severe |
| SpO2 <92% PEF 33–50% |
| Can't complete sentences in one breath, or too breathless to talk or feed |
| Pulse >125 (>5 years), >140 (2–5 years) |
| Respiration >30/min (>5 years), >40 (2–5 years) |
| Signs of life-threatening asthma |
| SpO2 <92% PEF <33–50% best or predicted |
| Cyanosis |
| Confusion |
| Coma |
| Poor respiratory effort |
| Exhaustion |
| Silent chest |
| Hypotension |
Children with life-threatening asthma or SpO2 <94% should receive high flow oxygen via a tight-fitting face mask or nasal cannulae at sufficient flow rates to achieve normal saturations.
Nebulised beta 2 agonists should be given for acute severe and life-threatening asthma.
Give nebulisers back to back, with Ipratroprium Bromide added to the second and third (250mcg/dose mixed with nebulised beta 2 agonist solution, 125mcg/dose for <5 years).
In mild to moderate asthma, beta 2 agonists should be given increasing by two puffs every two minutes up to 10 puffs, according to response.
Give prednisolone early (20 mg for two- to five-year-olds, 3040 mg for children over five).
Children who have not improved after receiving up to 10 puffs should be referred to hospital. Further doses of bronchodilator should be given as necessary while awaiting transfer.
Children who are transported to hospital by ambulance should be treated with oxygen and nebulised beta 2 agonists during the journey.
The following clinical signs should be recorded:
Pulse rate – increasing tachycardia generally denotes worsening asthma; a fall in heart rate in life-threatening asthma is a pre-terminal event
Respiratory rate and degree of breathlessness
Use of accessory muscles of respiration
Amount of wheezing
Degree of agitation and conscious level.
Bronchiolitis
The following is taken from the SIGN quick reference guide on bronchiolitis.5 (Please see the SIGN website for the full guideline and a useful patient information leaflet).
Refer urgently any infant with acute bronchiolitis or suspected acute bronchiolitis if there are any of the following:
Cyanosis
History of apnoea
Presence of nasal flaring or grunting
Severe chest wall recession
Poor feeding (<50% of usual intake in preceding 24 hours)
Lethargy
Respiratory rate >70/min
Oxygen saturation 94% or less
Uncertainty regarding diagnosis.
Take into account whether the infant is in the early stages of the illness as the illness is likely to worsen over the first few days.
The threshold for hospital referral should be lower in those who are less than three months old, those born at fewer than 35 weeks gestation and those with comorbidities (especially congenital cardiac or lung disease).
Pneumonia
Children with pneumonia are more unwell and tend to have a higher temperature than those with minor respiratory illness. They may not have cough in the early stages and may present with fever and vomiting or abdominal pain. They are often off feeds. It may not be possible to localise the site of the pneumonia as sounds are transmitted all over a small chest.
Children with suspected pneumonia who need referral to hospital are those who are vomiting, not able to take adequate fluids or needing oxygen (oxygen saturations 94% or less). As with other illnesses, families who may not be able to provide adequate observation at home or may not be able to access help quickly should also be referred.
Upper airway obstruction
See also Advanced Paediatric Life Support, Fourth Edition.6
CHOKING
The following is a brief reference only. All staff should have basic life support training according to surgery requirements.
A child who is talking or crying is unlikely to have significant airway obstruction but this can change quickly if the foreign object is dislodged.
Any child with signs of distress, drowsiness, cyanosis or losing consciousness must receive emergency treatment in the form of back blows and either the Heimlich manoeuvre if over four/five years or chest thrusts if under four years (the Heimlich manoeuvre can damage abdominal organs in young children).
Figure 1.
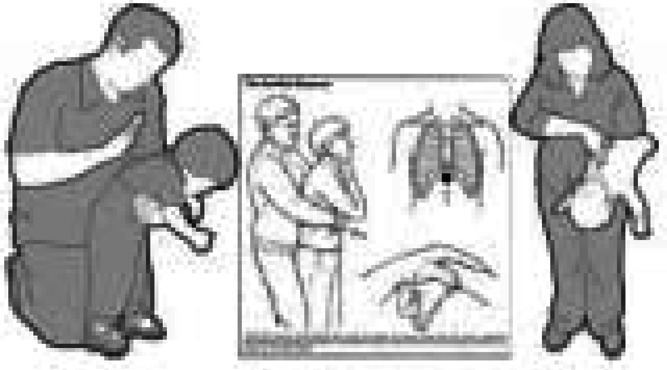
Emergency treatment for choking
CROUP
Try to keep the child and parents as calm as possible. Crying increases the work of breathing.
Keep the child upright or in the most comfortable position for them.
Observe from a distance as much as possible. Look for neck retraction (child is providing their own jaw thrust) or ‘air hunger’.
Give parent oxygen tubing to hold.
Listen for stridor. Obstruction is more severe if the stridor is heard in expiration as well as inspiration (‘biphasic stridor’).
Watch the effort of breathing and the degree of recession.
If there are signs of impeding complete obstruction, drowsiness or reduced oxygen saturations, nebulise:
1–5mls of 1 in 1000 adrenaline with continuous heart rate monitoring. The effect may wear off after 20 minutes but the dose can be given a second time.
2mg Budesonide can also be nebulised as it will have a longer lasting effect.6
Alert the receiving hospital of an incoming 999 call and the need for an anaesthetic assessment and possibly a surgeon to perform an emergency cricothyroidotomy.
Figure 2.
In cases where there is severe obstruction but no immediate threat to life, nebulise 2mg Budesonide and give oral Dexamethasone (1 month – 2 years 150 micrograms/Kg as a single dose. See Table 4 for estimates of weight by age) if able to tolerate by mouth. Stridor at rest is an indication for hospital admission.
Table 4.
Estimates of weight and height by age from BNF for children 20098
| Age | Weight (Kg) | Height (cm) |
|---|---|---|
| Full term neonate | 3.5 | 51 |
| 1 month | 4.3 | 55 |
| 2 months | 5.4 | 58 |
| 3 months | 6.1 | 61 |
| 4 months | 6.7 | 63 |
| 6 months | 7.6 | 67 |
| 1 year | 9 | 75 |
| 3 years | 14 | 96 |
| 5 years | 18 | 109 |
| 7 years | 23 | 122 |
| 10 years | 39 | 149 |
| 14 year old boy | 49 | 163 |
| 14 year old girl | 50 | 159 |
| Adult male | 68 | 176 |
| Adult female | 58 | 164 |
Anaphylaxis
A guideline based on the Resuscitation Council UK Guidelines can be found at:7 www.patient.co.uk/doctor/Anaphylaxis-and-its-Treatment.htm
Box 1. Quick reference anaphylaxis algorithm – child.
- Rapid assessment
- Airway: Look for and relieve airway obstruction, call for help early if signs of obstruction.
- Breathing: Look for and treat bronchospasm and signs of respiratory distress.
- Circulation: Colour, pulse and blood pressure.
- Disability: Assess whether responding or unconscious.
- Exposure: Assess skin with adequate exposure, but avoid excess heat loss.
Consider anaphylaxis when compatible history of rapid onset severe allergic-type reaction with respiratory diffculty and/or hypotension especially if skin changes present.
Give high flow oxygen – using a mask with an oxygen reservoir (greater than 10 litres min-1 to prevent reservoir collapse).
- Lie patient flat:
- Raise the legs (care as may worsen any breathing problems).
- ADRENALINE IM in anterolateral aspect of the middle third of the thigh (safe, easy, effective):
- Child IM dose (The equivalent volume of 1:1000 adrenaline is shown in brackets):
- 12 years: 500 micrograms IM (0.5 mL) i.e. same as adult dose. 300 micrograms (0.3 mL) if child is small or prepubertal
- 6 – 12 years: 300 micrograms IM (0.3 mL)
- <6 years: 150 micrograms IM (0.15 mL)
- Note: Half doses of adrenaline may be safer for patients on amitriptyline, imipramine, MAOI or betablocker.
- When skills and equipment available:
- Establish airway (in anaphylaxis airway obstruction from tissue swelling diffcult to overcome and early expert intubation often needed)
- IV fluid challenge:
- Insert one or more large-bore intravenous cannulae (enable the highest flow).
- Use intraosseous access (if trained to do so) in children when intravenous access is diffcult.
- Give a rapid fluid challenge:
- For children give 20 mL/kg of warmed crystalloid.
- Chlorphenamine (after initial resuscitation). Dose depends on age:
- >12 years and adults: 10 mg IM or IV slowly
- >6 – 12 years: 5 mg IM or IV slowly
- >6 months – 6 years: 2.5 mg IM or IV slowly
- <6 months: 250 micrograms/kg IM or IV slowly
- Hydrocortisone (after initial resuscitation). Dose depends on age:
- >12 years and adults: 200 mg IM or IV slowly
- >6 – 12 years: 100 mg IM or IV slowly
- >6 months – 6 years: 50 mg IM or IV slowly
- <6 months: 25 mg IM or IV slowly
- Monitor:
- Pulse oximetry
- ECG
- Blood pressure
A treatment algorithm poster from the Resuscitation Council.8 Reproduced with permission of ????
Fitting
FIRST AID MEASURES
Make sure the child is in a safe position, lying in the recovery position away from any potentially dangerous objects. Don't try to open the mouth. Make a note of the time. If the seizure continues beyond four to five minutes call for help or dial 999.
ONGOING MANAGEMENT IN A CLINICAL AREA
Give oxygen straight away. Insert oral airway if you know how to do this.
Check the blood glucose.
Try rectal diazepam (see Table 5) if fitting persists longer than 15 minutes.
Consider the possibility of head injury as a cause or as a result of the seizure. If the seizure followed a head injury, a CT scan is indicated.
Hypoglycaemia may be the cause of a seizure, particularly in a young child, but may also arise as a result of the prolonged muscle activity of the seizure itself.
Table 5.
Rectal Diazepam doses if febrile convulsion lasting longer than 15 minutes
| Rectal Diazepam doses (repeated once after ten minutes if necessary): | |
|---|---|
| Neonate | 1.25–2.5mg |
| Child 1 month to 2 years | 5mg |
| Child 2 to 12 years | 5–10mg |
| Child 12 to 18 years | 10mg |
Taken from: Medical Emergencies in the Community, British National Formulary for Children 20099
Dehydration
Babies and young children can become dehydrated very quickly. Worrying features in the history would be no wet nappy for 12 hours (although urine may be missed if it is mixed in with watery diarrhoea). The parents may know a recent weight which can be useful in assessing potential fluid loss. Lethargy and drowsiness are worrying features.
In moderate or severe dehydration, there are often sunken eyes and fontanelle, dry mucous membranes (lips and tongue), increased heart and/or respiratory rate, cool peripheries and possibly increased capillary refill time. The skin may also stay elevated for longer than one second when pinched over an area such as the abdomen.
Children who are not able to tolerate oral fluids or who have moderate or severe dehydration need referral for hospital admission.
DIABETIC KETOACIDOSIS (DKA)
The dehydration associated with DKA can be life threatening. The degree of dehydration is moderate or severe, and there is a raised respiratory rate and glucose and ketones detected in the urine. DKA is an emergency and these children must be referred urgently to hospital. If there are signs of shock, high flow facial oxygen should be given.
When assessing a child with dehydration, don't forget to think about:
Intussusception (history of intermittent crying with pallor, vomiting. The classic ‘redcurrant jelly’ stool is a LATE sign)
Pyloric stenosis (four to six weeks old, forceful vomiting).
Note: It is easy to miss hypernatraemic dehydration in infants as the skin turgor is maintained by the high sodium and the baby may not appear dehydrated. They will however have physiological signs of dehydration such as a raised pulse rate and a raised respiratory rate.
Unwell with non-blanching rash
Children who are unwell with a rash which does not fade with pressure (‘the glass tumbler test’) must be assumed to have meningococcal septicaemia. They may also have meningitis.
Figure 3.
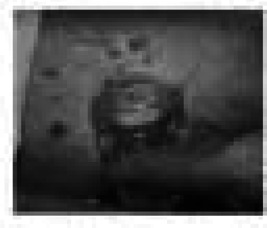
The glass tumbler test
The critical element is to identify signs of early compensated shock:
Tachycardia
Cool peripheries/pallor
Increased capillary refill time
Tachypnoea/pulse oximetry <95%
Confusion, drowsiness, decreased conscious level.
If any of these is present:
A,B,C, high flow oxygen with tight-fitting face mask
Blood glucose stick test
IM Benzyl Penicillin or Cefotaxime (see doses in Table 6) and 999 referral to hospital.
Table 6.
Doses of antibiotics for suspected meningococcal septicaemia
| Benzyl Penicillin doses by intravenous injection (or by intramuscular injection if venous access not available) | |||
| Neonate | 300mg | ||
| Child 1 month to 1 year | 300mg | ||
| Child 1 to 10 years | 600mg | ||
| Child 10 to 18 years | 1.2g | ||
| If history of allergy to penicillin – | |||
| Cefotaxime doses by intravenous injection (or by intramuscular injection if venous access not available): | |||
| Neonate | 50mg/Kg | ||
| Child 1 month to 12 years | 50mg/Kg (max. 1g) | ||
| Child 12 to18 years | 1g | ||
| Or if history of immediate hypersensitivity reaction (including anaphylaxis, angioedema or urticarial reaction to penicillin or to cephalosporins) – | |||
| Chloramphenicol injection: | |||
| By intravenous injection | |||
| Child 1 month – 18 years | 12.5–25 mg/Kg | ||
Taken from: Medical Emergencies in the Community, British National Formulary for Children 20099
Conclusion
With newer models of urgent care delivery, GPs may be faced with sicker children than they would normally see in their surgery. However, by anticipating these events and making use of the wide range of resources available, they will minimise the anxiety associated with managing unwell children.
REFERENCES
- 1.Doctor's Bag – Contents. Patient.co.uk
- 2.Feverish Illness in Children: assessment and initial management in children under five years. National Institute for Health and Clinical Excellence, May 2007. CG 47 [Google Scholar]
- 3.www.spottingthesickchild.com
- 4.www.brit-thoracic.org.uk/Portals/0/Clinical%20Information/Asthma/Guidelines/qrg101%20revised%202009.pdf
- 5.www.sign.ac.uk/pdf/qrg91.pdf
- 6.Advanced Paediatric Life Support (4e) London: British Medical Journal Books; 2005 [Google Scholar]
- 7.www.patient.co.uk/doctor/Anaphylaxis-and-its-Treatment.htm
- 8.www.resus.org.uk/pages/anapost1.pdf
- 9.British National Formulary for Children. 2009
AUTHOR DETAILS
The author is a general paediatrician based at Hammersmith Hospital where there is a Children's Ambulatory Unit providing an extended day service. This is open access for local families and the Unit also receives referrals from local general practitioners. A general practitioner is co-located in the unit seeing children with minor illnesses.
ETHICAL APPROVAL
As this is a review article summarising accepted management pathways, ethical committee approval was not needed.
CONFLICTS OF INTEREST
None.


