Abstract
The purpose of the present research was to develop and characterize mucoadhesive microspheres of curcumin for the potential use of treating gastric adenocarcinoma, gastric and duodenal ulcer associated with Helicobacter pylori. Curcumin mucoadhesive microspheres were prepared using ethyl cellulose as a matrix and carbopol 934P as a mucoadhesive polymer by an emulsion-solvent evaporation technique. Response surface methodology was used for optimization of formulation using central composite design (CCD) for two factors at three levels each was employed to study the effect of independent variables, drug:polymer:polymer ratio (curcumin:ethylcellulose:carbopol 934P)(X1) and surfactant concentration (X2) on dependent variables, namely drug entrapment efficiency (DEE), percentage mucoadhesion (PM), in vitro drug release and particle size (PS). Optimized formulation was obtained using desirability approach of numerical optimization. The experimental values of DEE, PM, % release and PS after 8 h for the optimized formulation were found to be 50.256 ± 1.38%, 66.23%±0.06, 73.564 ± 1.32%, and 139.881 ± 2.56 μm, respectively, which were in close agreement with those predicted by the mathematical models. The drug release was also found to be slow and extended more than 8 h and release rates were fitted to the Power law equation and Higuchi model to compute the diffusional parameters. The prolonged stomach residence time of curcumin mucoadhesive microspheres might make a contribution to H. pylori complete eradication in combination with other antimicrobial agents.
Keywords: Curcumin, Helicobacter pylori, mucoadhesive
INTRODUCTION
Helicobacter pylori (H. pylori) is a gram negative helical rod that colonizes the human gastric mucous layer.[1] H. pylori is reported to be an important etiologic factor in the development of the chronic gastritis, ulcers (gastric and duodenal) and gastric adenocarcinoma.[2] H. pylori carriage rates are about 80-90% in developing countries with high risk of gastric cancer.[3,4] Although the microorganism is susceptible to many antimicrobial agents but clinical trials with a single antimicrobial agent have resulted in a low eradication rate of H. pylori.[5,6,7] The most effective therapies of H. pylori infection require a minimum of two antibiotics in combination with a gastric acid inhibitor. Treatment with this therapy suffers from various side effects, namely nausea, drug resistance, infection recurrence, stomach upset and diarrhea.[8,9] Degradation of antimicrobial (e.g. amoxicillin and clarithromycin by gastric acid) and short residence time of antimicrobial agents in the stomach are two major reasons for the failure of H. pylori eradication.[10,11] Resistance to antibiotics particularly to metronidazole and clarithromycin is also an increasing problem.[12] Because of the undesirable side effects, resistance to antibiotics and high cost of the therapy, makes it very difficult for the effective management of the condition. Therefore, there is an enormous requisite to search for safe, non-toxic, inexpensive and effective non-antibiotic compounds that can inhibit growth of bacteria i.e. H. pylori.
In the Indian traditional medical system, a number of plants and their active constituents are known to possess potent medicinal properties. The plant derived compounds have a long history of clinical use, better patient tolerance and acceptance.[13] There are reports on in vitro and in vivo antimicrobial activity of curcumin on H. pylori. The classical studies of Ronita and coworkers attributed the antimicrobial activity of curcumin against H. pylori.[14,15] Curcumin, 1 7-bis (4-hydroxy-3-methoxyphenyl)-1, 6-heptadiene-3, 5-Dione], a major yellow pigment obtained from the rhizomes of turmeric (Curcuma longa L.), has a wide array of pharmacological and biological activities. Apart from its other activities, namely antioxidant, anti-inflammatory, anti-infectious and anti-carcinogenic, curcumin revealed to target several molecules like growth factors, transcription factors, cytokines and enzymes including metalloproteinase's (MMPs) that are involved in the etiology of diverse diseases. Several studies have demonstrated that H. pylori infection induces the secretion of matrix metalloproteinase's (MMPs) from a variety of gastric cells in vivo as well as in cultured cells, which further contribute to pathogenesis of gastric ulcer and gastric cancer. Gastric epithelial cells appear to be the major source of MMPs in H. pylori-infected gastric tissues. Kundu and coworkers clearly demonstrated that elevated levels of MMP-3 and MMP-9 in gastric tissues of mice or cultured cells due to infection by H. pylori strains (either cag+ve or cag-ve) are inhibited by curcumin treatment. This curcumin mediated down regulation of MMP-3 and MMP-9 levels in H. pylori-infected mice and cultured cells suggest its immense therapeutic potential against H. pylori-associated gastrointestinal diseases. Their study highlights the potential of curcumin-based therapy as a promising anti-H. pylori agent having property to restore and repair the gastric damage caused by H. pylori infection.[16] Increasing complications in the conventional antibiotic combination therapy stimulate an urgent need to develop new non-antibiotic antibacterial agents against H. pylori infection in order to provide safe, effective and specific cellular target moieties. Pre-clinical and clinical trials have revealed that curcumin is safe even up to a dose level of 8.0 g/kg and this makes it all the more important.
Multiparticulate approaches include formulations in the form of pellets, granules, beads, microparticles and nanoparticles. Single unit stomach targeted drug delivery system may suffer from the disadvantage of unintentional disintegration of the formulation that may lead to drastically compromised systemic drug bioavailability or loss of local therapeutic action in the stomach. Mucoadhesive multiparticulate can greatly improve the pharmacotherapy of the stomach through local drug release, leading to high drug concentration at the gastric mucosa, thus eradicating H. pylori from the sub-mucosal tissue of the stomach and making it possible to treat stomach and duodenal ulcer, gastritis and esophagitis. In the present study the bioadhesive system for curcumin was designed, optimized and evaluated.[17]
MATERIALS AND METHODS
Materials
Curcumin was obtained from Himedia, India. Carbopol 934P, Ethylcellulose was a gift from Corona Pharmaceutical, Solan, India. Double distilled water was used in all the preparations. All other solvents and chemicals used were of analytical grade.
Methods
Preparation of mucoadhesive curcumin microspheres
Mucoadhesive microspheres of curcumin were prepared containing carbopol 934P and ethyl cellulose by emulsion-solvent evaporation technique. Briefly, ethyl cellulose was dissolved in a mixture of acetone and ethanol (1:0.5). Curcumin and carbopol 934P were added to the above polymeric solution under stirring. In batches CM-1 to CM-13 the drug-to-polymer (curcumin:ethyl cellulose) ratio was kept constant at 1:3. The resultant mixture was extruded through a syringe (# 20) in a mixture of liquid paraffin (mixture of heavy and light, 1:1) containing 0.5 to 1.5% v/v of Span 60 and stirring was carried out using a propeller stirrer (Remi, Mumbai, India) at 1000 rpm for 3 hours. The amount of Carbopol 934P and the concentration of surfactant were varied in batches CM-1 to CM-13 as shown in Table 1. The microspheres formed were then dried at room temperature. Prepared microspheres were collected by filtration and washed several times with petroleum ether to remove liquid paraffin. The microspheres were then dried at room temperature (at 25°C and 60% relative humidity) for 24 hours.
Table 1.
Translation of coded levels in actual units
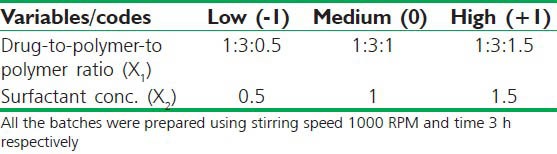
Experimental design
A central composite design was employed for optimization of formulation. The chosen independent factors, i.e., drug:polymer:polymer ratio (Curcumin: Ethylcellulose: Carbopol 934P) (X1) and surfactant concentration (X2) have more significant effects on the property of microspheres. The drug entrapment efficiency (DEE), particle size (PS), percentage mucoadhesion (PM) and drug release after 8 hours were kept as dependent variables.
The actual values for each variable corresponding to the coded levels ±1 are shown in Table 1. A commercially available software package (DOE) for experiment design and analysis was used to plan the experiment. Thirteen batches were planned and the run order within block was randomized to reduce the effect of uncontrolled variables.
Polynomial model (Second-order) was used to generate response surfaces:
y = b0 + b1X1 + b2X2 + b3X12 + b4X22 + b5X1X2
Where y is the measured response associated with each factor level combination; b0 is an intercept; b1 to b5 are regression coefficients; and x1 and x2 are the independent variables. The dependent and independent variables selected are presented in Table 1 along with their low, medium and high levels selected for the study.
Estimation of curcumin
Curcumin was estimated by ultraviolet visible (UV/Vis) spectrophotometric method (Systronic 2202) based on the measurement of absorbance at 424 nanometers. The method was validated for linearity, accuracy and precision. The method obeys Beer's law in the concentration range of 2-20 μg/ml.
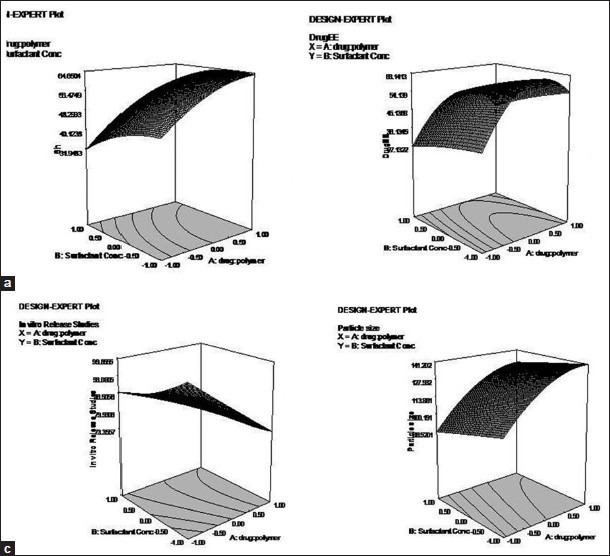
Drug entrapment efficiency (DEE)
Accurately weighed (50 mg) washed microspheres were crushed in a glass mortar pestle and the powdered microspheres were suspended in 10 ml of methanol and kept for 12 h. After filtration appropriate dilution were made with methanol and the absorbance was measured spectrophotometrically at 424 nm against blank. The entrapment efficiency was calculated using the following formula:[18]
Particle size of microspheres
After fabrication and drying the particle size was immediately noted using a microscope. Under the microscope, 150 microspheres particle were counted for particle size using a calibrated optical microscope (Labomed CX RIII, Ambala, India).
Bioadhesion study
The mucoadhesive properties of the microspheres were evaluated by in vitro wash-off test, as reported by Lehr et al. A 1 × 1 cm piece of rat stomach mucosa was tied onto a glass slide (3 inch-by-1 inch) using thread. About 50 microspheres were spread (50) onto the wet, rinsed, tissue specimen and allowed to hydrate. The prepared slide was hung onto one of the groves of a USP tablet disintegrating test apparatus. The tissue specimen was given regular up and down movements in the beaker of the disintegration apparatus, which contained the gastric fluid (pH 1.2). At the end of 30 min, 1 h and at hourly intervals up to 8 h, the number of microspheres still adhering onto the tissue was counted.[19]
Drug release study
The release of curcumin from the microspheres was investigated by using USP XXIV basket apparatus (Electrolab, Mumbai, India) at 37°C ± 0.5°C and at 100 rpm using 900 mL of 0.1N HCl (pH 1.2) as a dissolution medium. Microspheres equivalent to 50 mg of curcumin were used for the test. Sample solution (5 ml) was withdrawn at pre-determined time intervals (every 30 min for 6 h and at hourly intervals up to 8 h), filtered through a 0.45 μm membrane filter, diluted and analyzed spectrophotometrically against the blank treated under similar conditions. An equal amount of fresh medium was replaced immediately after withdrawal of the test sample.
Release kinetics
Data obtained from in vitro release studies were fitted to various kinetic equations to find the mechanism of drug release from the microspheres.[20] The kinetic models used were zero-order, first-order, Higuchi's model, Korsmeyer-Peppas model and Hixson-Crowell cube-root models. The release rate constants (k) and determination coefficients (r) were calculated by means of PCP disso v2.08 software. Curve fitting was performed using PCP disso v2.08 software.
Zero-order release rate kinetics
To study the zero-order release kinetics, the release rate data are fitted to the following equation:
Q = K0t
where “Q” is the fraction of drug released, “K” the release rate constant and “t” is the release time.
First-order kinetics
A first-order release would be predicated by the following equation:

where C = amount of drug remaining at time “t”,
Co = initial amount of the drug and K = first-order rate constant (h–1).
When the data are plotted as cumulative percent drug remaining versus time, it yields a straight line, indicating that the release follows first-order kinetics. The constant “K” can be obtained by multiplying 2.303 with slope.
Higuchi release model
To study the Higuchi release kinetics, the release rate data were fitted to the following equation:
Q = K.t1/2
where “Q” is the amount of drug released, “K” the release rate constant, and “t” is the release time.
When the data are plotted as accumulative drug released versus square root of time, it yields a straight line, indicating that the drug released by diffusion mechanism. The slope is equal to “K”.
The dissolution data were fitted to Peppas equation. Release exponent “n” was calculated.
Mt/M∞ = kp tn
where Mt/M∞ is the fraction of drug released at time t, kp is the kinetic constant of the system, and n is the exponent characteristic of the mode transport.
Fourier transform infrared spectroscopy (FTIR)
FTIR spectra of curcumin and EC/Carbopol 934P microspheres were recorded using FTIR spectrophotometer (Agilent Cary 630 FTIR Spectrometer) to investigate any interaction between curcumin and polymers in formulated microspheres. The scanning range was 4000 to 650 cm−1 and the resolution was 8 cm−1.
Differential scanning calorimetry (DSC)
DSC study was carried out using DSC-60 instrument (Shimadzu corporation, Japan) to check the formation as well as the compatibility of ingredients. Accurately weighed samples were placed on aluminum plates sealed with aluminum seals and the thermogram was obtained at a scanning rate of 10°C/min conducted over a range of 0-200°C under an inert atmosphere flushed with nitrogen at a rate of 20 ml/minute.
Scanning electron microscopy
A scanning electron photomicrograph of optimized drug-loaded mucoadhesive microspheres was taken. A small amount of microspheres was spread on glass stub. Afterwards, the stub containing the sample was placed in the scanning electron microscope (SEM, Quanta-250, FEI, Singapore) chamber. The scanning electron photomicrograph was taken at the acceleration voltage of 15 kV, chamber pressure of 4.58e-6 Torr, and magnification 1200.
Stability studies
Accelerated stability studies were performed at 40°C ± 2°C and 75 ± 5% relative humidity (RH), using Humidity control oven NEC 210R10 (Newtronic Instruments, India) as per ICH guidelines for six months. After 6 months the mucoadhesion and release rate of curcumin from the optimized formulation were determined and statistically analyzed by the unpaired t test (P ≤ 0.05).
RESULT AND DISCUSSION
Preliminary trials
Mucoadhesive microspheres of curcumin were prepared by emulsion-solvent evaporation technique. Microspheres obtained were free flowing in nature. Preliminary trials were carried out to optimize the solvent ratio, namely acetone: ethanol (1:0.5). Surfactants like tween 80, Span 20, span 60 and span 80 was screened and span 60 was found to be suitable surfactant for formulation of mucoadhesive microspheres. To optimize the formulation, central composite design was employed. For a two-factor central composite design, 13 experiments are required and the results of % muchoadhesion, drug entrapment efficiency, drug release after 8 h, and particle size are shown in Table 2.
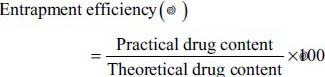
Table 2.
Optimization of mucoadhesive microspheres of curcumin
Data evaluation
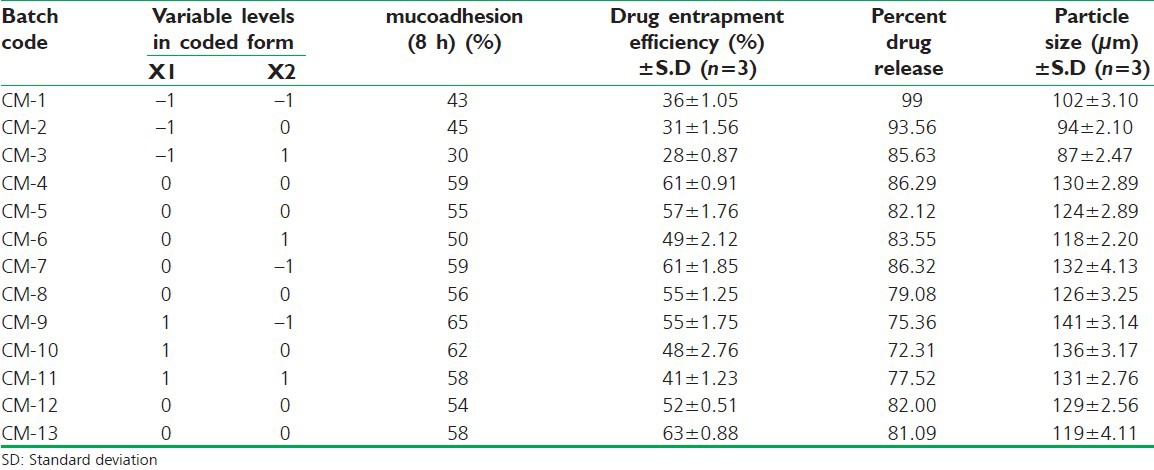
% Muchoadhesion, drug entrapment efficiency, drug release after 8 hours, and particle size were selected as the dependent variables. The equations by a second-order polynomial model are shown as follow, and then the three-dimensional response surface graphs fitted to the equation are shown in Figure 1.
Figure 1.
3D graphs showing the effect of polymer and surfactant concentration on mucoadhesion (a), drug entrapment (b), in vitro release (c) and particle size (d)
The model equation for muchoadhesion after 8 hour
y = 56.76 + 11.17X1 − 4.83X2 − 4.16X12 − 3.16X22 − 1.50X2 (P < 0.01, r = 0.9590)
The concentration of polymer has shown positive effect on mucoadhesive character of the microspheres. Further it was observed that as the concentration of surfactant was increased, there was significant reduction in mucoadhesive properties of the microspheres.
The model equation for DEE
y = 57.17241 + 8.16667X1 −5.66667X2 −16.60345X12 − 1.10345X22− 1.50000X2 (P < 0.01, r = 0.9469)
The equations show that concentration of surfactant significantly affecting the drug loading into the microspheres. An increased surfactant concentration decreases the entrapment efficiency of the microspheres, whereas higher polymer concentration favors entrapment of the drug into the microspheres.
The model equation for in vitro release
y = 82.33−8.83X1− 2.33X2 + 0.14X12 + 2.14X22 + 3.88X2 (P < 0.001, r = 0.9344)
Both the factors viz., concentration of polymer and surfactant has shown negative effect on drug release. As the concentration of polymer has increased the release of drug decreased.
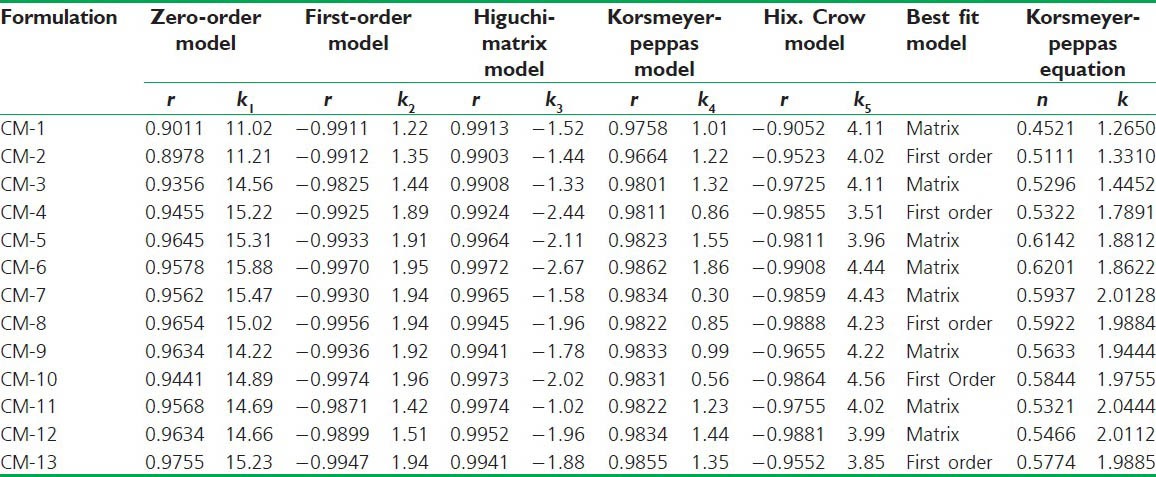
The obtained dissolution data was subjected to mathematical treatment using PCP Disso Ver 2.8 software. The results are shown in Table 3. In the entire formulations Higuchi model was found to be the best fitted model. The release of the drug follows non-fickian release with n value varying from-0.4521-0.6201.
Table 3.
Mathematical modeling of in vitro data
The model equation for particle size
y = 125.48 + 20.83X1 −6.50X2 −10.19X12 −0.19X22 + 1.25X2 (P < 0.01, r = 0.9761)
Polymer concentration has significant effect on particle size. As the concentration is increased, particle size increased.
From contour plots [Figure 2] the best area for formulation to obtain desired responses was found. The best conditions to optimize drug release corresponded to a polymer concentration of 1:2.8:0.9 and a surfactant concentration of 0.39%. A new batch of microspheres were prepared and evaluated. The results are shown in Table 4. Table shows that observed responses were inside the constraints and close to predicted responses.
Figure 2.
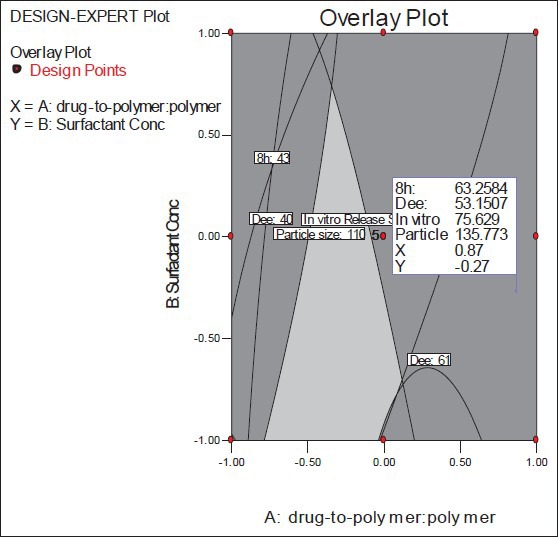
Contour plot for determining optimum formulation of curcumin mucoadhesive microspheres
Table 4.
Observed and predicted values for the optimum formulation of curcumin mucoadhesive microspheres
Particle size analysis
Hundred and fifty microspheres of each batch were sized and the average particle size was calculated. The mean size range of microspheres was found to be between 87 ± 2.47 and 141 ± 3.14 μm for all formulations [Table 2]. Increase in the particle size was observed with increase in polymer concentration that might be due to more viscous nature of polymer solution.
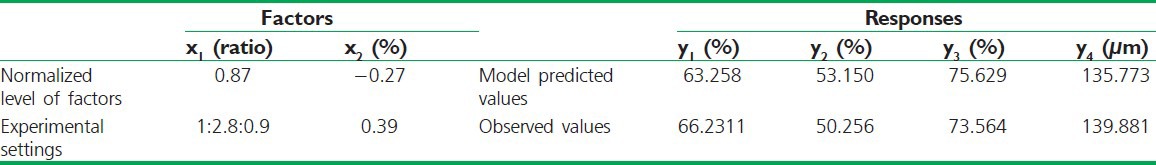
Fourier transform infrared spectroscopy
FTIR analysis revealed that there was no interaction between the drug and the polymers, thus these polymers can be conveniently used in further development of stomach specific mucoadhesive curcumin microspheres. The prominent spectrum of curcumin are as follows: 3510, 1629, 1510, 1428, 1275, 1208, 1153, 1030, 966, 858 and 814 cm−1. Generally, the stretching region of hydroxyl group, O-H was showed at the band range of 3200-3600 cm-1. The band at 3510 cm-1 indicates the presence of hydroxyl group in the curcumin. The strong peak at 1629 cm−1 has a predominantly mixed υ (C = C) and υ (C = O) character. Another strong band at 1603 cm−1 is attributed to the symmetric aromatic ring stretching vibrations υ (C = Cring). The 1510 cm−1 peak is assigned to the υ (C = O), while enol C–O peak was obtained at 1275 cm−1, C–O–C peak at 1030 cm−1, benzoate trans-CH vibration at 960 cm−1 and cis CH vibration of aromatic ring at 713 cm−1. FTIR data in the region of (2300-1500 cm-1) were compared for pure curcumin and curcumin encapsulated in microspheres. Two main characteristics C = O bands [Figure 3a] were observed for crystalline curcumin at 1629 and 1603 cm-1, assigned to the aliphatic and aromatic carbonyl stretching bands, respectively. Microsphere formulation also yielded peaks at the same wavelengths [Figure 3b].
Figure 3.
FTIR spectrum of curcumin (a) and curcumin mucoadhesive microspheres (B)
Differential scanning calorimetry
Stability of curcumin in EC/Carbopol 934P microspheres was investigated by thermal analysis using DSC [Figure 4a and 4b] thermograms. The melting point of curcumin was revealed by endothermic peaks at 176°C. The same thermal behavior was also observed in curcumin-loaded mucoadhesive microspheres but the peak was less sharp and the endothermic peak slightly shifted to higher temperature which suggested that curcumin encapsulated in microspheres. Thermal analysis (DSC) was used to analyze the physical state of drug encapsulated in polymeric microspheres. These results revealed that curcumin encapsulated in microspheres was in crystalline state.
Figure 4.
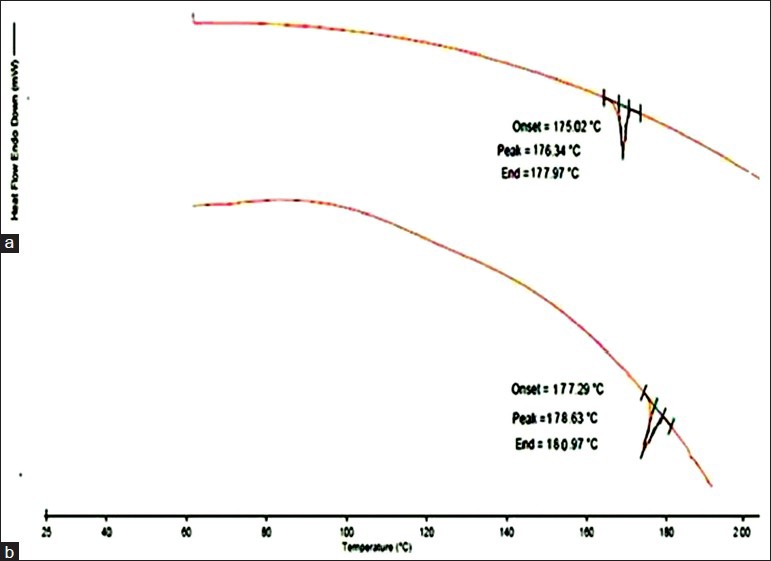
DSC thermogram of pure drug curcumin (a), and optimized microsphere formulation (b)
Scanning electron microscopy
Figure 5 shows scanning electron photomicrographs of optimized drug-loaded mucoadhesive microspheres. The surface morphology of prepared microspheres shows the spherical shape of microspheres with a slightly rough surface which may be because of surface-associated drug crystals.
Figure 5.
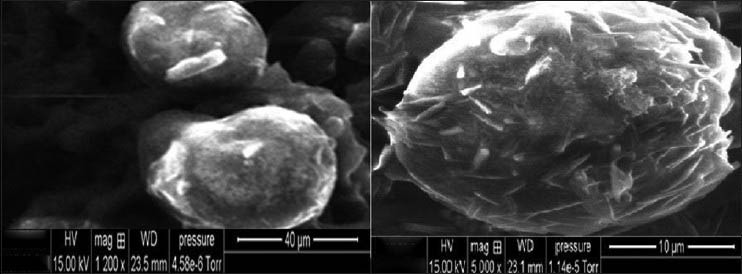
Scanning electron microscopic (SEM) pictures of curcumin microspheres
Drug entrapment efficiency
The entrapment efficiencies of all formulation are showed in Table 2. It was observed that increase in the concentration of the polymer increases the entrapment efficacy. This may be due to increase in the viscosity of the solution, which brought about the decrease in the emulsification leading to the formation of bigger globules in the emulsion.
Bioadhesion study
The study of in vitro bioadhesion revealed that all the batches of prepared microspheres had good bioadhesive property ranging from 30% to 65%. On increasing the polymer (Carbopol 934P) concentration, the bioadhesive property of the microspheres also increased as shown in Table 2. The formulation CM9 showed the highest bioadhesive property (65%). These studies suggest that the spherical matrix of microspheres can interact with mucosubstrate on the surface of the stomach, and adhere to mucosa more strongly and could stay in stomach for prolong period for more effective H. pylori clearance.
Stability studies
Stability studies performed on optimized microspheres as per ICH guidelines for 6 months at 40°C ± 2°C/75% RH ± 5%. Studies indicated no significant changes in mucoadhesion and in vitro drug release pattern (P ≤ 0.05).
CONCLUSION
The optimized formulation for curcumin mucoadhesive microspheres was obtained with ethylcellulose and Carbopol 934P using response surface methodology based on a central composite design. It was found that the optimized formulation was achieved and the observed responses were close to the predicted values for the optimized formulation. The drug release from the optimized formulation showed a controlled-release pattern which could offer both local and systemic action for effective treatment of H. pylori infection. Increasing complications in the conventional triple-therapy (TT) stimulate an urgent need to develop new non-antibiotic antibacterial agents against H. pylori infection that are safe, highly effective and have specific cellular targets. Since curcumin is cheap and easily available in developing countries like India, this study opens scope for an easy therapeutic solution to a potentially complicated H. pylori-related disease.
ACKNOWLEDGMENT
The authors are grateful to Prof. Neeraj Mahindroo for kind guidance in the final outcome of this manuscript and Prof. P.K. Khosla, Vice Chancellor, Shoolini University, Solan for providing facilities and financial assistance during the project. We also acknowledge Corona Pharmaceutical (Solan, India) for generous gift samples of polymers.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Hayama M, Kawakami Y, Kanelo Y, Sona K, Ota H. Helicobacter pylori infection increases cell kinetics in human gastric epithelial cells without adhering to proliferating cells. J Cell Mol Med. 2005;9:746–7. doi: 10.1111/j.1582-4934.2005.tb00508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Umamaheshwari RB, Ramteke S, Jain NK. Anti-Helicobacter Pylori effect of mucoadhesive nanoparticles bearing amoxicillin in experimental gerbils model. AAPS PharmSciTech. 2004;5:60–8. doi: 10.1208/pt050232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bardonnet PL, Faivre V, Boullanger P, Piffaretti JC, Falson F. Pre-formulation of liposomes against Helicobacter pylori: Characterization and interaction with the bacteria. Eur J Pharm Biopharm. 2008;69:908–22. doi: 10.1016/j.ejpb.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 4.Lacy BE, Rosemore J. Helicobacter pylori: Ulcers and more: The beginning of an era. J Nutr. 2001;131:2789S–93S. doi: 10.1093/jn/131.10.2789S. [DOI] [PubMed] [Google Scholar]
- 5.Umamaheshwari RB, Jain NK, Jain S. A new approach in gastro retentive drug delivery system using cholestyramine. Drug Del. 2003;10:151–60. doi: 10.1080/713840399. [DOI] [PubMed] [Google Scholar]
- 6.Labenz J. Current role of acid suppressants in Helicobacter pylori eradication therapy. Pract Res Clin Gastroenterol. 2001;15:413–31. doi: 10.1053/bega.2001.0188. [DOI] [PubMed] [Google Scholar]
- 7.Sepulveda AR, Coelho LG. Helicobacter pylori and gastric malignancies. Helicobact. 2002;7:37–42. doi: 10.1046/j.1523-5378.7.s1.6.x. [DOI] [PubMed] [Google Scholar]
- 8.Lin CK, Hsu PI, Lai KH. One-week quadruple therapy is an effective salvage regimen for Helicobacter pylori infection in patients after failure of standard triple therapy. J Clin Gastroenterol. 2002;5:547–51. doi: 10.1097/00004836-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Kawabami E, Ogata SK, Portorreal AC. Triple therapy with clarithromycin, amoxicillin and omeprazole for Helicobacter pylori eradication in children and adolescents. Arq. Gastroenterol. 2001;3:203–6. doi: 10.1590/s0004-28032001000300011. [DOI] [PubMed] [Google Scholar]
- 10.Cuna M, Alonso MJ, Torres D. Preparation and in vivo evaluation of mucoadhesive microparticles containing amoxicillin-resin complexes for drug delivery to the gastric mucosa. Eur J Pharm Biopharm. 2001;51:199–205. doi: 10.1016/s0939-6411(01)00124-2. [DOI] [PubMed] [Google Scholar]
- 11.Arora S, Budhiraja RD. Chitosan-alginate microcapsules of amoxicillin for gastric stability and mucoadhesion. J Adv Pharm Technol Res. 2012;3:68–74. doi: 10.4103/2231-4040.93555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thong-Ngam D, Chatsuwan T. Antibacterial activity of aloe vera, curcumin, garlic and Plau-noi against Helicobacter pylori. Thai J Gastroenterol. 2007;8:5–11. [Google Scholar]
- 13.Veeresham C. Natural products derived from plants as a source of drugs. J Adv Pharm Technol Res. 2012;3:200–1. doi: 10.4103/2231-4040.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foryst-Ludwiga A, Neumanna M, Schneider-Brachertb W. Curcumin blocks NF-kB and the motogenic response in Helicobacter pylori infected epithelial cells. Biochem Biophys Res Commun. 2004;316:1065–72. doi: 10.1016/j.bbrc.2004.02.158. [DOI] [PubMed] [Google Scholar]
- 15.Ronita De, Kundu P, Swarnakar S, Ramamurthy T, Chowdhury A, Nair GB. Antimicrobial activity of curcumin against Helicobacter pylori isolates from India and during infections in mice. Antimicrob Agents Chem. 2009;53:1592–7. doi: 10.1128/AAC.01242-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kundu P, Ronita De, Pal I, Mukhopadhyay AK, Saha DR, Swarnakar S. Curcumin alleviates matrix metalloproteinase-3 and -9 activities during eradication of Helicobacter Pylori infection in cultured cells and mice. PloS One. 2011;6:e16306. doi: 10.1371/journal.pone.0016306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dey NS, Majumdar S, Rao ME. Multiparticulate drug delivery systems for controlled release: Review article. Trop J Pharm Res. 2008;7:1067–75. [Google Scholar]
- 18.Hari BN, Praneetha T, Prathyusha T, Mounika K, Devi DR. Development of starch-gelatin complex microspheres as sustained release delivery system. J Adv Pharm Technol Res. 2012;3:182–7. doi: 10.4103/2231-4040.101015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lehr CM, Bowstra JA, Tukker JJ, Junginger HE. Intestinal transit of bioadhesive micro- spheres in an in situ loop in the rat. J Control Release. 1990;13:51–62. [Google Scholar]
- 20.Mankala SK, Korla AC, Gade S. Development and evaluation of aceclofenac-loaded mucoadhesive microcapsules. J Adv Pharm Technol Res. 2011;2:245–54. doi: 10.4103/2231-4040.90881. [DOI] [PMC free article] [PubMed] [Google Scholar]


