Abstract
Primary pulmonary lymphoma is a very rare neoplasm that represents only 3-4% of extranodal non-Hodgkin lymphoma (NHL), less than 1% of NHL and only 0.5-1% of primary pulmonary malignancies. Primary pulmonary NHL is most commonly represented by marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue type (MALT lymphoma). The clinical characteristics, methods of treatment, and outcomes are not well-elucidated. We, therefore, reviewed the medical records of five Moroccan patients who were pathologically and clinically diagnosed as primary pulmonary lymphoma and treated in our institute of oncology.
KEY WORDS: Lung, mucosa-associated lymphoid tissue type lymphoma, non-Hodgkin lymphoma
INTRODUCTION
Primary non-Hodgkin lymphoma (NHL) of the lung is very rare, accounting for only 0.4% of all malignant lymphomas.[1] Primary pulmonary lymphoma is defined as a clonal lymphoid proliferation affecting one or both lungs (parenchyma and/or bronchi) in a patient with no detectable extrapulmonary involvement at diagnosis or during the subsequent 3 months.[2] This definition includes: Multifocal mucosa-associated lymphoid tissue (MALT) NHL; pulmonary lymphoma with satellite nodes (hilar or mediastinal); low-grade B-cell PPL; high-grade B-cell PPL.[3] Although there are several treatment options such as tumor resection, radiation and chemotherapy, the therapeutic consensus has not been clearly established. The prognosis is overall good especially in low-grade disease.
Our objective was to analyze the clinical features and to discuss the optimal management and prognostic factors through a literature review.
PATIENTS AND METHODS
Clinical data
We retrospectively reviewed the medical records of five patients with proven malignant primary pulmonary lymphoma treated in Morocco between September 2010 and March 2013. The diagnosis was based on the following criteria: Unilateral or bilateral pulmonary involvement with NHL; no evidence of mediastinal adenopathy; no evidence of extrathoracic disease by clinical staging work-up that includes thorough physical examination, computed tomographic scans of the chest, abdomen and pelvis and the examination of bone marrow biopsy specimens; no history of lymphoma; no evidence of extrathoracic disease up to 3 months after the initial diagnosis.
Consent and statement of ethical approval
The study respected the ethical rules for medical research involving human subjects as stipulated by the World Medical Association Declaration of Helsinki. Informed consent was obtained and documented in writing before study entry. This study was performed after approval by local hospital committees.
RESULTS
Clinical features
The group of five patients included two men and three women, with a median age of 63 years (range: 50-74 years). All patients had respiratory symptoms and three of them had B-symptoms. The radiological findings were various but without lymph node enlargement as listed in Table 1. The pathological diagnosis was obtained with computed tomography-guided biopsy and showed that most patients (80%) had MALT lymphoma and were immunohistochemically CD20+, CD5−, cyclin D1 − and CD10− [Figures 1 and 2.]
Table 1.
The patient's characteristics treatment and outcomes
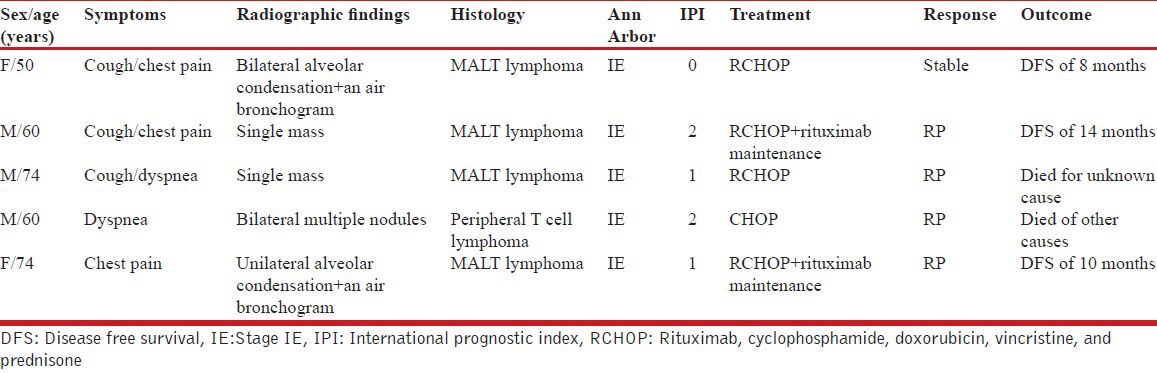
Figure 1.
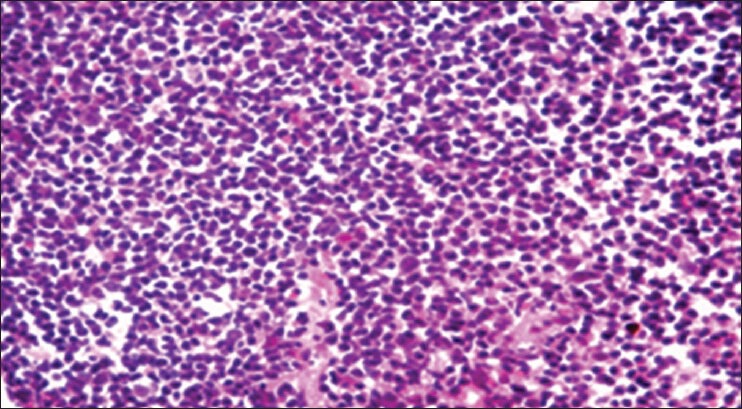
MALT lymphoma: Histologically the tumor is composed of small dark nuclei
Figure 2.
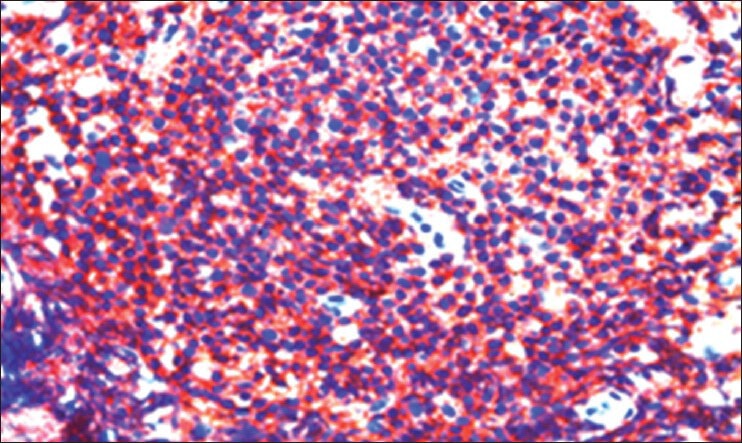
Tumor cells indicate a positive immunohistochemical reaction with CD20
Treatment and outcome
All the patients received chemotherapy only without surgery or radiotherapy. The protocol of chemotherapy was R-CHOP-21 regimen (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) for MALT lymphoma and CHOP-21 alone for T lymphoma. Three cases are still in a disease-free state with a median follow-up of 1 year; and two died at 3 and 6 months (due to congestive heart failure in one and unknown cause in another).
DISCUSSION
PPL is very rare, it represents only 3-4% of extranodal NHL, less than 1% of NHL, and only 0.5-1% of primary pulmonary malignancies.[1] The incidence of primary pulmonary lymphoma peaks in the 6th and 7th decades of life, and the ratio of male to female patients is close to 1:1.[2] Clinical description is nonspecific. When present, symptoms are various, such as cough, mild dyspnea, chest pain, and occasionally hemoptysis. At pulmonary auscultation, crackles are present in less than 20% of cases.[3] The radiographic findings are nonspecific also and include solitary nodule, multiple ill-defined nodules, consolidated mass with air bronchograms, pleura effusions, atelectasis, and cavities.[4] PPL originate frequently from the B cell-lineage which is represented most commonly by marginal zone B-cell lymphoma of MALT of the bronchus that is thought to be acquired as a result of chronic antigenic stimulation such as smoking, autoimmune disease, or infection.[5] In our small series, the majority had MALT lymphoma, three were smokers and one patient was previously treated for tuberculosis 2 years back. Primary pulmonary peripheral T cell lymphoma is, however, extremely rare and has been reported in some few cases.[6]
The treatment options include watch and wait approach, surgery in localized tumors, chemotherapy if the lesions are diffuse or involve both lungs and radiotherapy. But in the absence of comparative series, the efficacy of these treatments cannot be analyzed.[7,8,9]
Nevertheless, the Italian Society of Hematology produced clinical practice-guidelines for the management of these rare tumors. In patients with MALT or non-MALT primary lung NHL, the panel of expert recommended for first-line therapy, combination regimens with anthracycline-based chemotherapy or monotherapy in association or not with rituximab.
In addition, for patients with MALT primary lung NHL surgical resection can be the treatment of choice in localized tumors if complete resection can be achieved.
Radiotherapy is to be reserved for patients with a unique, small lesion and observation only can be an alternative in an asymptomatic patient with localized disease.[10]
Most of the studies confirm the relatively favorable prognosis of patients with PPL irrespective of the treatment modalities. One large series of 70 patients reported a 94% survival at 5 years for low-grade primary pulmonary lymphoma, and a median survival of 3 years for high-grade disease.[2,11,12]
Although our series is small, the clinical and imaging features were consistent with those described in the literature, the prognosis was favorable even the follow-up is still short and the treatment was exclusively based on chemotherapy. We think that ideally, future studies should evaluate prospectively the respective treatment modalities of both low- and high-grade lymphomas to optimize therapeutic outcomes of these rare diseases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ferraro P, Trastek VF, Adlakha H, Deschamps C, Allen MS, Pairolero PC. Primary non-Hodgkin's lymphoma of the lung. Ann Thorac Surg. 2000;69:993–7. doi: 10.1016/s0003-4975(99)01535-0. [DOI] [PubMed] [Google Scholar]
- 2.Martínez Rivera C, Bonnin Vilaplana M, Simón Adiego C, Palacín Forgué A, Puig Zuza J, Sampablo Lauro I. Primary pulmonary lymphoma presenting as a pulmonary mass with cavitation. Arch Bronconeumol. 2004;40:94–6. doi: 10.1016/s1579-2129(06)60201-2. [DOI] [PubMed] [Google Scholar]
- 3.Santos IG, Marchiori E, Zanetti G, Mano CM, Sarcinelli-Luz B, Vianna FG. Primary pulmonary mucosa-associated lymphoid tissue lymphoma computed tomography findings: A case report. Cases J. 2009;2:6329. doi: 10.4076/1757-1626-2-6329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee DK, Im JG, Lee KS, Lee JS, Seo JB, Goo JM, et al. B-cell lymphoma of bronchus-associated lymphoid tissue (BALT): CT features in 10 patients. J Comput Assist Tomogr. 2000;24:30–4. doi: 10.1097/00004728-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Zinzani PL, Tani M, Gabriele A, Poletti V, Stefoni V, Alinari L, et al. Extranodal marginal zone B-cell lymphoma of MALT-type of the lung Single-center experience with 12 patients. Leuk Lymphoma. 2003;44:821–4. doi: 10.1080/1042819031000067972. [DOI] [PubMed] [Google Scholar]
- 6.Lee HJ, IM JG, Goo JM, Kim KW, Choi BI, Chang KH, et al. Peripheral T cell lymphoma: Spectrum of imaging findings with clinical and pathologic features. Radiographics. 2003;23:7–26. doi: 10.1148/rg.231025018. [DOI] [PubMed] [Google Scholar]
- 7.Vanden Eynden F, Fadel E, de Perrot M, de Montpreville V, Mussot S, Dartevelle P. Role of surgery in the treatment of primary pulmonary B-Cell lymphoma. Ann Thorac Surg. 2007;83:236–40. doi: 10.1016/j.athoracsur.2006.08.026. [DOI] [PubMed] [Google Scholar]
- 8.Troch M, Streubel B, Petkov V, Turetschek K, Chott A, Raderer M. Does MALT lymphoma of the lung require immediate treatment? An analysis of 11 untreated cases with long-term follow-up. Anticancer Res. 2007;27:3633–7. [PubMed] [Google Scholar]
- 9.Cadranel J, Wislez M, Antoine M. Primary pulmonary lymphoma. Eur Respir J. 2002;20:750–62. doi: 10.1183/09031936.02.00404102. [DOI] [PubMed] [Google Scholar]
- 10.Zinzani PL, Martelli M, Poletti V, Vitolo U, Gobbi PG, Chisesi T, et al. Practice guidelines for the management of extranodal non-Hodgkin's lymphomas of adult non-immunodeficient patients. Part I: Primary lung and mediastinal lymphomas. A project of the Italian Society of Hematology, the Italian Society of Experimental Hematology and the Italian Group for Bone Marrow Transplantation. Haematologica. 2008;93:1364–71. doi: 10.3324/haematol.12742. [DOI] [PubMed] [Google Scholar]
- 11.Kim JH, Lee SH, Park J, Kim HY, Lee SI, Park JO, et al. Primary pulmonary non-hodgkin's lymphoma. Jpn J Clin Oncol. 2004;34:510–4. doi: 10.1093/jjco/hyh095. [DOI] [PubMed] [Google Scholar]
- 12.Graham BB, Mathisen DJ, Mark EJ, Takvorian RW. Primary Pulmonary Lymphoma. Ann Thorac Surg. 2005;80:1248–53. doi: 10.1016/j.athoracsur.2005.04.014. [DOI] [PubMed] [Google Scholar]


