Abstract
Visceral leishmaniasis (VL) is usually characterized by splenomegaly, pallor and fever. Pleural effusion is an uncommon feature of this disease, which is encountered in immunocompromised patients. Here, we report a case of VL with pleural effusion in an immunocompetent patient. Pulmonary symptoms in VL are usually related to bacterial lung infection, vagal nerve compression by splenomegaly, and hypoalbuminaemia with mild pulmonary edema. Our patient presented with cough and chest pain. The clinical features of this case were baffling since they mimicked that of pulmonary tuberculosis. This case report emphasizes the need to recognize the diverse nature of presentation of this curable yet fatal infectious disease.
KEY WORDS: Immunocompetent patient, pleural effusion, visceral leishmaniasis
INTRODUCTION
Leishmaniasis caused by an obligate intracellular protozoan, transmitted by sandfly bites, is endemic in over 80 countries in Africa, Asia, South and Central America, and Europe.[1] Visceral leishmaniasis (VL), caused by Leishmania donovani, is the most severe form of leishmaniasis. VL is characterized by fever, cachexia, hepatosplenomegaly (predominantly splenomegaly), pancytopenia, and hypergammaglobulinemia. Pulmonary involvement is not a common feature of VL.[2] Most of such reported cases are immunocompromised patients.[3,4,5] One uncommon presentation of VL with pleural effusion is being described in a patient, who showed no sign of immune abnormality.
CASE REPORT
A 62-year-old male patient, resident of West Bengal, was suffering from cough and chest pain for the last 6 months. He underwent initial management in a local hospital. He was a non-smoker and non-alcoholic. He had no history of fever, hematemesis, malena, diarrhea, headache, or body ache. He had not suffered from diseases like tuberculosis, asthma, chronic obstructive pulmonary disease (COPD), or gastroesophageal reflux disease (GERD). He was not taking any drugs at that time.
Initial clinical evaluation in the local hospital revealed that the patient had moderate pallor, cachexia but no lymphadenopathy. Auscultation of chest showed bilateral normal breath sounds, Chest radiograph showed a small left-sided pleural effusion. Routine hematological investigations detected pancytopenia with hemoglobin level of 7.7 g/dl. Erythrocyte Sedimentation Rate was 100 mm/h. Mantoux test for tuberculosis was negative. Sputum culture for acid-fast bacilli (AFB) was negative. Ziehl–Neelsen stain of the sputum smears was also negative for AFB.
The patient was prescribed antitussives and analgesics, but no significant improvement occurred. He was then referred to our hospital for further management.
After examining the patient, we obtained another chest radiograph that confirmed the presence of a small left-sided pleural effusion [Figure 1]. Known causes of pleural effusion like heart failure, pneumonia, tuberculosis, or carcinoma of lung were absent in this patient. He did not have any symptoms of arthritis, which is commonly found in autoimmune diseases. Therefore, the cause of pleural effusion remained unexplained.
Figure 1.
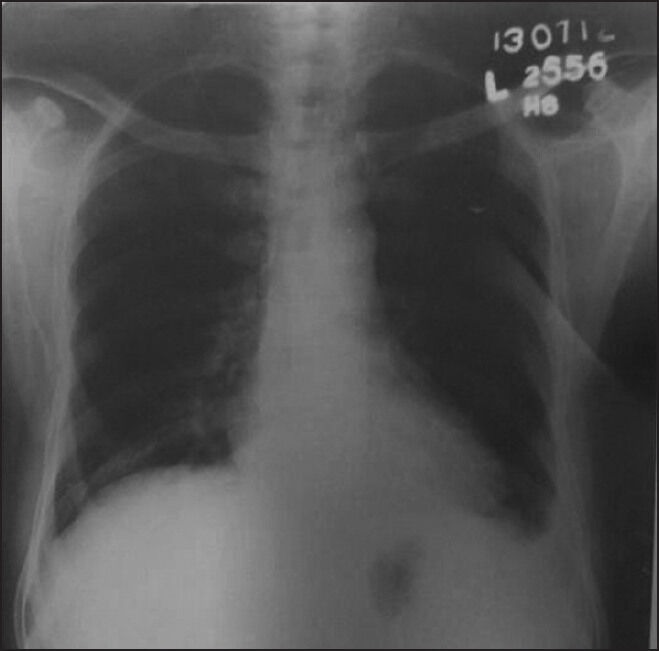
Chest radiograph showing a small left-sided pleural effusion
On thorough examination, a mild splenomegaly was detected. To detect the cause of splenomegaly, serum bilirubin, liver enzymes, and prothrombin time were estimated which were within normal limits. HBsAg, anti-HCV and anti-HIV antibodies were negative by ELISA technique. Widal test for enteric fever and test for malaria antigens were negative.
Total serum protein estimation was done, which was found to be within normal limits. However, the albumin/globulin ratio was reversed, being 0.2. Napier's aldehyde test was then performed which is based on the principle of hypergammaglobulinemia, that occurs in VL. About 1 ml of patient's serum was mixed well with a drop of 40% formalin, shaken and kept at room temperature. Opacification and solidification of serum was seen after 10 min signifying a positive result. Subsequently, bone-marrow aspiration was undertaken, which showed both intracellular and extracellular amastigote forms of L. donovani. Slight excess of plasma cells was also noted [Figure 2].
Figure 2.
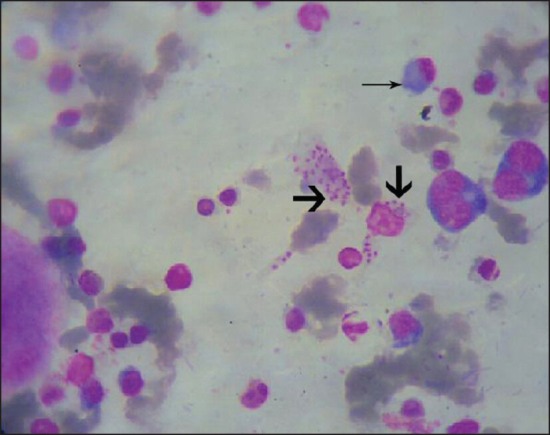
Bone marrow aspiration smear showing amastigote forms of Leishmania donovani (thick arrows) and plasma cells (thin arrow) (Leishman, × 1000)
The patient was treated with IV Sodium Stibogluconate with prompt clinical and laboratory improvement. Chest radiograph was done after 1 month, which showed resolution of preceding pleural effusion [Figure 3]. He was on follow-up for another 6 months, which was uneventful.
Figure 3.
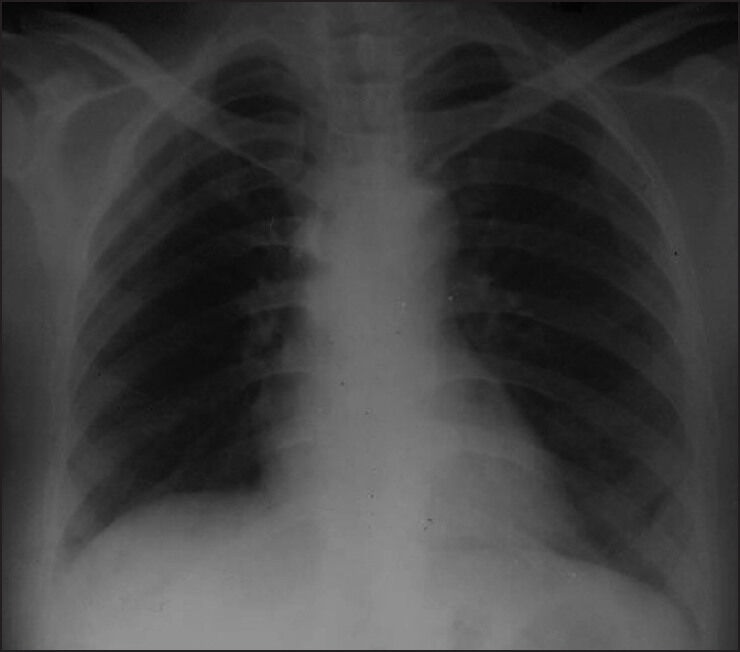
Chest radiograph showing resolution of pleural effusion after one month of treatment with IV sodium stibogluconate
DISCUSSION
The estimated annual global burden of VL is approximately half a million new cases and more than 50,000 deaths, of which 90% occur only in five countries–India, Bangladesh, Nepal, Sudan, and Brazil.[6]
The classical triad of presentation in VL consists of splenomegaly, pallor, and fever. Clinical lung involvement in VL is considered rare. However, a persistent dry cough maybe present in up to 83% of affected patients.[7,8] Common pulmonary symptoms in VL are usually related to bacterial lung infection, vagal nerve compression by splenomegaly, and hypoalbuminemia with mild pulmonary edema.[9] In the present case, the patient presented with chest pain and cough. He had a small left-sided pleural effusion that was detected on chest radiograph. Later, mild splenomegaly was detected on thorough examination.
A few cases of VL with pleural effusion have been reported in immunocompromised patients. Chenoweth et al. reported a case of VL in an AIDS patient who presented with pulmonary symptoms and bilateral pleural effusions.[3] Similar cases have also been reported by Das et al. and Diehl et al.[4,5] Our patient was immunocompetent and yet he presented with pleural effusion.
Raina et al. reported a case of VL with exudative pleural effusion in a 25-year-old immunocompetent patient.[10] The patient had history of cough and chest pain, similar to our case. In contrast to the present case, the patient also presented with other features suggestive of leishmaniasis, like fever and a dragging sensation in the upper abdomen. Surprisingly, our patient had clinical features that mimicked that of tuberculosis.
Kotsifas et al. reported a case of VL in an immunocompetent man with clinical and bronchoscopically confirmed endobronchial and mediastinal involvement. They highlighted that cough should not be overlooked as a presenting symptom of VL and may be a sign of pulmonary involvement.[11]
Pulmonary involvement in VL has been diagnosed by various modalities depending on the lesion present. Chenoweth et al. demonstrated histiocytes containing Leishmania amastigotes in pleural fluid and bone marrow.[3] Bronchial biopsies were performed by Kotsifas et al., in which numerous macrophages containing L. amastigotes were found. They concluded that bronchoscopic examination could detect otherwise undiagnosed pulmonary involvement in VL.[11] Though bronchoscopic examination was not performed in our patient, bone-marrow aspiration was done. Amastigote forms of L. donovani were demonstrated in the aspirate smears, which confirmed the diagnosis of VL.
Newer modalities of diagnosis of VL are now available. Hofman et al. found the anti-Leishmania homologue of receptors for activated C-kinase (LACK) antibody p19-11 to be a highly specific and sensitive paraffin-reactive immunohistochemical marker for the confirmation or identification of Leishmania species in tissue sections.[12] Diehl et al. stated in their study that PCR detection and identification of Leishmania species in body fluids are important diagnostic tools.[5]
VL is treated with sodium stibogluconate (SSG) IM/IV 20 mg/kg/day for 30 days and miltefosine 100 mg daily for 4 weeks in an area where sensitivity of SSG is more than 90%. In areas with SSG sensitivity less than 90% or SSG failures cases it is treated with Amphotericin B 1 mg/kg body weight IV infusion daily or alternate day for 15-20 infusions.[13] Our patient was treated with sodium stibogluconate, with prompt response.
In conclusion, VL is a common disease in West Bengal and prompt diagnosis and treatment are essential to reduce mortality from this infectious disease. The present case is unusual as the patient was immunocompetent and yet presented with cough and pleural effusion clinically mimicking a tubercular lesion.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lamps LW. Intestinal flagellates. In: Lamps LW, editor. Surgical Pathology of Gastrointestinal System: Bacterial, Fungal, Viral and Parasitic Infections. 1st ed. New York: Springer; 2009. pp. 177–82. [Google Scholar]
- 2.Piscopo TV, Mallia AC. Leishmaniasis. Postgrad Med J. 2006;82:649–57. doi: 10.1136/pgmj.2006.047340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chenoweth CE, Singal S, Pearson RD, Betts RF, Markovitz DM. Acquired immunodeficiency syndrome-related visceral leishmaniasis presenting in a pleural effusion. Chest. 1993;103:648–9. doi: 10.1378/chest.103.2.648. [DOI] [PubMed] [Google Scholar]
- 4.Das VN, Pandey K, Kumar N, Hassan SM, Bimal S, Lal CS, et al. Visceral leishmaniasis and tuberculosis in patients with HIV co-infection. Southeast Asian J Trop Med Public Health. 2006;37:18–21. [PubMed] [Google Scholar]
- 5.Diehl RS, Santos RP, Zimmerman R, Luz LP, Weiss T, Jacobson P, et al. Microscopy and polymerase chain reaction detection of Leishmania chagasi in the pleural and ascitic fluid of a patient with AIDS: Case report and review of diagnosis and therapy of visceral leishmaniasis. Can J Infect Dis Med Microbiol. 2004;15:231–4. doi: 10.1155/2004/680153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Leishmaniasis: Burden of disease. [cited 2013 April 8]. Available from: http://www.who.int/leishmaniasis/burden/en .
- 7.Maltezou HC, Siafas C, Mavrikou M. Visceral leishmaniasis during childhood in southern Greece. Clin Infect Dis. 2000;31:1139–43. doi: 10.1086/317455. [DOI] [PubMed] [Google Scholar]
- 8.Sarker CB, Chowdhury KS, Siddiqui NI, Jamal MF, Rahman S, Momen A, et al. Clinical profile of Kala-azar in adults: As seen in Mymensingh Medical College Hospital, Mymensingh, Bangladesh. Mymensingh Med J. 2003;12:41–4. [PubMed] [Google Scholar]
- 9.Tuon FF, Guedes F, Fernandes ER, Pagliari C, Amato VS, Duarte MIS. In situ immune responses to interstitial pneumonitis in human visceral leishmaniasis. Parasite Immunol. 2009;31:98–103. doi: 10.1111/j.1365-3024.2008.01080.x. [DOI] [PubMed] [Google Scholar]
- 10.Raina S, Kaul R, Kashyap R, Gupta D. Atypical presentation of visceral leishmaniasis from non-endemic region. Online J Health Allied Scs. 2010;9:13. [Google Scholar]
- 11.Kotsifas K, Metaxas E, Koutsouvelis I, Skoutelis A, Kara P, Tatsis G. Visceral leishmaniasis with endobronchial involvement in an immunocompetent adult. Case Report Med 2011. 2011. p. 5. 561985. Available from: www.hindawi.com/crim/medicine/2011/561985 . [DOI] [PMC free article] [PubMed]
- 12.Hofman V, Brousset P, Mougneau E, Marty P, Lamant L, Antoine JC, et al. Immunostaining of visceral leishmaniasis caused by Leishmania infantum using monoclonal antibody (19-11) to the leishmania homologue of receptors for activated C-kinase. Am J Clin Pathol. 2003;120:567–74. doi: 10.1309/R3DK-4MR3-W6E5-PH17. [DOI] [PubMed] [Google Scholar]
- 13.MOHFW; [cited 2013 April 10]. Treatment of Kala-azar; National Vector Borne Disease Control Programme (NVBDCP) Available from: http://www.nvbdcp.gov.in/kal8.html . [Google Scholar]


