Abstract
The coexistence of sleep apnea-hypopnea syndrome (SAHS) with chronic obstructive pulmonary disease (COPD) occurs commonly. This so called overlap syndrome leads to more profound hypoxemia, hypercapnic respiratory failure, and pulmonary hypertension than each of these conditions independently. Not infrequently, these patients show profound hypoxemia, despite optimal continuous positive airway pressure (CPAP) therapy for their SAHS. We report a case where CPAP therapy with additional in-line oxygen supplementation failed to accomplish adequate oxygenation. Adding transtracheal oxygen therapy (TTOT) to CPAP therapy provided better results. We review the literature on transtracheal oxygen therapy and how this technique may play a significant role in these complicated patients with overlap syndrome, obviating the need for more invasive procedures, such as tracheostomy.
KEY WORDS: Continuous positive airway pressure, overlap syndrome, respiratory failure, transtracheal oxygen therapy, sleep apnea
INTRODUCTION
Transtracheal oxygen therapy (TTOT) was previously reported as an alternative to continuous positive airway pressure (CPAP) therapy when treating patients with sleep apnea-hypopnea syndrome (SAHS), but this has not been studied extensively. A significant decrease in apnea-hypopnea index (AHI) in some cases has been described. The coexistence of SAHS with chronic obstructive pulmonary disease (COPD), the so called overlap syndrome, carries an increased risk of severe hypoxemia, hypercapnic respiratory failure, and pulmonary hypertension.[1] We present a case of overlap syndrome that proved extremely difficult to treat, despite optimal conventional therapy. The addition of TTOT in combination with CPAP therapy provided better gas exchange while sleeping and awake. This is the first reported case of this combined modality of therapy.
CASE REPORT
A 63-year-old white man with a history of hypercarbic-hypoxemic respiratory failure due to moderate COPD and with mild SAHS, presented with worsening fatigue, dyspnea, and development of peripheral edema. His initial polysomnography 10 years earlier revealed obstructive sleep apnea (OSA) with an AHI of 13.4/hour with oxygen desaturations to 62% on room air, entirely due to obstructive hypopneas. He was completely compliant with CPAP therapy at 11 cm of water pressure in addition to oxygen at 4 liters per minute (LPM), which had been demonstrated to adequately correct his sleep disordered breathing in the sleep laboratory. He was found to have emphysema with an forced expiratory volume in the first second (FEV1) of 67% of predicted. He quit smoking and was compliant with his bronchodilators and medical therapy for diastolic dysfunction.
Despite medical compliance, 8 years later he complained of worsening fatigue. Daytime oxygen requirements while walking rose to 6 LPM and nocturnal oxygen saturations fell to 70% on 5 LPM of oxygen with CPAP. He had to stop working because it was impractical for him to have such high oxygen flows at work. Repeat polysomnography was performed for retitration of CPAP therapy. This demonstrated correction with CPAP at 15 cm of water pressure and 4 LPM of O2, yielding an AHI of 0 with saturations >90%.
Echocardiography and cardiac catheterization showed diastolic dysfunction and no obstructive coronary artery disease or valvular disease. Diuretic therapy was intensified without improving oxygenation or symptoms. Computerized tomography of the chest with contrast showed baseline emphysema and no pulmonary emboli. Repeat pulmonary function was unchanged with FEV1 at 67% of predicted and stable lung volumes. Awake resting arterial blood gas on oxygen at 5 LPM was at baseline (pH: 7.45, PaCO2: 54 torr, PaO: 61 torr). A repeat nocturnal oximetry demonstrated desaturations to 75% on CPAP at 15 cm of water pressure with oxygen at 5 LPM. Interestingly, he never had erythrocytosis with a hemoglobin level of 13.6 g/dl.
He refused suggested tracheostomy in order to initiate nocturnal mechanical ventilation with a positive pressure ventilator, but agreed to have to TTOT in order to improve nocturnal oxygenation. A SCOOP® TTOT catheter was placed using a modified Seldinger technique. Subsequently, CPAP at 15 cm of water pressure was continued with TTOT at 4 LPM. Nocturnal oximetry on these settings showed no desaturations below 87% and <5 min with saturations below 90% [Figure 1]. A repeat blood gas after TTOT was not performed, as this would have required an indwelling arterial catheter to be representative of his true response to therapy while sleeping. Such maneuver was deemed too invasive for clinical therapy, considering his oximetry and overall clinical improvement. A daytime arterial blood gas, in a stable clinical state did demonstrate a decrease in PaCO2 to 48 while awake with TTOT. He had no complications of TTOT except for occasional mucous ball formation early in therapy and occasional tube dislodgment, which over time resolved with further patient education and the addition of guafenesin oral therapy. There were no problems related to air leaks or other pathology around the TTOT catheter site during CPAP therapy, and he markedly improved with decreased fatigue, dyspnea, and edema. He increased his activity level and lost 16 kg with diet and improved exercise tolerance. To determine if CPAP was still required, he was restudied without CPAP and with TTOT at 2 LPM. The overall AHI was 3.5/h, but with a supine AHI of 36/h. Saturations dropped to 87% with 17.2 min <89%. CPAP was reinstituted.
Figure 1.
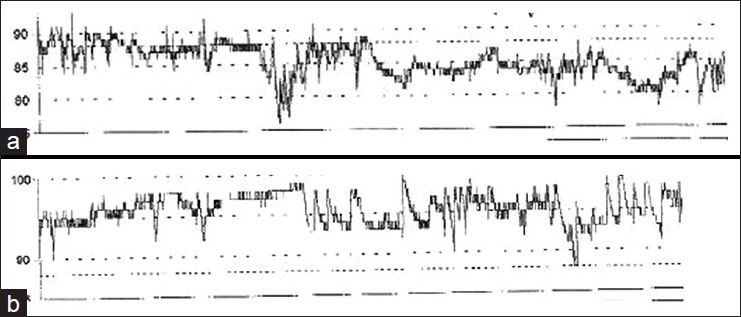
Nocturnal oximetries demonstrating improvement in oxygenation with lower oxygen requirements once TTOT was added to CPAP. Submitted separately: (a) CPAP at 15 cm of water pressure plus oxygen at 5 LPM on 10/6/09. (b) CPAP at 15 cm of water pressure plus TTOT at 4 LPM on 10/14/09
Over the ensuing year he improved further clinically. He intentionally cancelled his disability payments and returned to work as a car salesman with TTOT at 2 LPM with SaO2>90% with ambulation.
DISCUSSION
Management of patients with combined COPD and SAHS is complex. These patients have an increased risk for severe hypoxemia, which is much higher than when these diseases are not coexistent. Additionally, there is also increased risk for hypercapnic respiratory failure and pulmonary hypertension.[2] Our patient had respiratory failure with severe hypoxemia and mild hypercapnia, despite lacking severe COPD or severe SAHS. Correcting his SAHS failed to correct his hypoxemia, with limited therapeutic options. Tracheostomy is usually unwelcomed by patients, as in this case. Bilevel PAP therapy is another consideration, but given the mild degree of SAHS adequately corrected with CPAP and mild hypercapnia, this appeared unlikely to improve sleep apnea and would not improve daytime oxygen requirements.
TTOT was previously investigated in chronic respiratory failure patients, demonstrating decreased oxygen requirements, reduced CO2 levels and diminishing work of breathing. TTOT, through a small percutaneous tracheal catheter, leads to decreased dead space, smaller tidal volumes, and lower minute ventilation.[3,4,5]
TTOT was also utilized in patients with SAHS. Breitenbucher and Keller-Wossidlo in 1989 reported decreased number of severity of desaturations in SAHS treated with TTOT.[6] Chauncey and Aldritch studied four patients with OSA describing lower AHI, shorter desaturations and less sleep fragmentation with TTOT, as compared to nasal cannula oxygen.[7] Later, Farney and Walker compared TTOT to CPAP and nasal cannula oxygen. TTOT improved oxygenation and reduced the AHI from 64.6 to 26.2/h. More recently, Christopher and Schwartz presented a review of TTOT and described their anecdotal success in treating patients with SAHS with TTOT and thoroughly reviewed the subject of TTOT.[8] Additionally, a few patients treated with only insufflated transtracheal room air showed apparent benefit.[9] Subsequently, Schneider et al., evaluated transtracheal gas insufflation in SAHS. They demonstrated that high flow air insufflation (10-15 LPM) helps control SAHS. Nevertheless, higher flows induced laryngospasms, which were prevented using servo systems to intermittently stop flows during the events.[1]
Our case illustrates the successful use of TTOT and CPAP therapy in a patient with concurrent hypoxemic/hypercapnic respiratory failure and sleep apnea. Neither CPAP with supplemental oxygen nor TTOT independently adequately improved the patient's respiratory status. The patient was able to avoid the morbidity of tracheostomy and inconvenience of nocturnal mechanical ventilation and was able to return to work.
Alternatively, high flow air insufflation use has been used in chronic respiratory failure and may help avoid using CPAP therapy. This modality is limited by desiccation of the tracheal mucosa and may cause airway ulcers. In the authors’ experience, these local problems have occurred with high flow TTOT in chronic respiratory failure. Hence, we elected to continue CPAP therapy with low flow TTOT. In our case, another consideration was that creating an ostomy in the trachea for TTOT could decrease CPAP efficacy, by causing a pressure leak. Nevertheless, the TTOT catheter diameter is only 2.7 mm and we had no air leaks with the AHI remaining well controlled without requiring increased CPAP levels. Therefore, TTOT plus CPAP is a feasible therapeutic option in these complex cases.
Though our observations are limited to a single case, we hope to motivate others to further investigate the role of this therapy, while making our colleagues aware of this treatment alternative.
ACKNOWLEDGMENT
The authors gratefully acknowledge support of the Chair of Medicine at Carilion Clinic, Dr. Ralph Whatley.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Schneider H, O’Hearn DJ, Leblanc K, Smith PL, O’Donnell CP, Eisele DW, et al. High-flow transtracheal insufflation treats obstructive sleep apnea. A pilot study. Am J Respir Crit Care Med. 2000;161:1869–76. doi: 10.1164/ajrccm.161.6.9902061. [DOI] [PubMed] [Google Scholar]
- 2.Weitzenblum E, Chaouat A, Kessler R, Canuet M. Overlap syndrome: Obstructive sleep apnea in patients with chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5:237–41. doi: 10.1513/pats.200706-077MG. [DOI] [PubMed] [Google Scholar]
- 3.Heimlich HJ, Carr GC. Transtracheal catheter technique for pulmonary rehabilitation. Ann Otol Rhinol Laryngol. 1985;94:502–4. doi: 10.1177/000348948509400518. [DOI] [PubMed] [Google Scholar]
- 4.Bergozfsky EH, Hurewitz AN. Airway insufflation: Physiologic effects on acute and chronic gas exchange in humans. Am Rev Respir Dis. 1989;140:885–90. doi: 10.1164/ajrccm/140.4.885. [DOI] [PubMed] [Google Scholar]
- 5.Benditt J, Pollock M, Roa J, Celli B. Transtracheal delivery of gas decreases the oxygen cost of breathing. Am Rev Respir Dis. 1993;147:1207–10. doi: 10.1164/ajrccm/147.5.1207. [DOI] [PubMed] [Google Scholar]
- 6.Breitenbucher A, Keller-Wossidlo H, Keller R. Transtracheal oxygen therapy in obstructive sleep apnea syndrome. Schweiz Med Wochenschr. 1989;119:1638–41. [PubMed] [Google Scholar]
- 7.Chauncey JB, Aldrich MS. Preliminary findings in the treatment of obstructive sleep apnea with transtracheal oxygen. Sleep. 1990;13:167–74. [PubMed] [Google Scholar]
- 8.Christopher KL, Schwartz MD. Transtracheal Oxygen Therapy. Chest. 2011;139:435–40. doi: 10.1378/chest.10-1373. [DOI] [PubMed] [Google Scholar]
- 9.Farney RJ, Walker JM, Elmer JC, Viscomi VA, Ord RJ. Transtracheal oxygen, nasal CPAP and nasal oxygen in five patients with obstructive sleep apnea. Chest. 1992;101:1228–35. doi: 10.1378/chest.101.5.1228. [DOI] [PubMed] [Google Scholar]


