Abstract
Objective
While multiple social and behavioral risk factors associated with obesity co-occur among young children, most studies have examined them separately. The purpose of this study is to examine the relationship between social risk factors, behavioral problems, health behaviors and obesity among preschool children in the Fragile Families and Child Wellbeing Study (N=1589).
Methods
A cumulative social risk score was created by summing maternal reports of intimate partner violence, food insecurity, housing insecurity, maternal depressive symptoms, maternal substance use, and father's incarceration, obtained when the child was 3 years old. Mothers reported on the child's internalizing and externalizing behaviors with the Child Behavior Checklist (CBCL) at age 5. Mothers also reported on hours the child spent watching TV and sleeping as well as servings of soda or juice drinks the child consumed per day. Child height and weight were measured at age 5. Obesity was defined as Body Mass Index (BMI) >=95th percentile.
Results
In regression analyses adjusted for health behaviors, behavioral problems and socio-demographic factors, cumulative social risk was associated with obesity among girls. Externalizing behavioral problems, were associated with obesity among girls (PR 1.5 95%CI 1.2, 1.7) and boys (PR 1.3 95%CI 1.1, 1.6). Short sleep duration was also associated with obesity among girls (PR 1.2 95% CI 1.0, 1.4) and boys (PR 1.3 95%CI 1.1, 1.5) even after adjusting for behavioral problems and social risk factors. Watching more than 2 hours of television per day was associated with obesity among boys (PR 1.5, 95%CI 1.2, 1.9) but not girls.
Conclusions
Co-occurring social and behavioral risk factors are associated with obesity among five-year old children.
Childhood obesity is a major public health problem in the United States (US) that disproportionately affects African American and Hispanic children as well as children of low socioeconomic status (SES) (1, 2). These racial/ethnic groups tend to live in environments characterized by high social stress (family and neighborhood), which recent evidence has linked to increased risk of obesity (3-5). For example, children living in a home where there are reports of maternal intimate partner violence (IPV)(3), child maltreatment and neglect, maternal depression and maternal drug use have a higher likelihood of becoming obese. Furthermore, as the number of social stressors experienced increases, so does the magnitude of obesity risk (6). Social stressors are frequently associated with other dysfunctional behaviors, (7) and most likely these respective risks are positively reinforcing each other. Prior studies have focused on the influence of one specific type of risk factor at a time, such as social (3, 8, 9) or behavioral risks (10, 11); with few studies exploring how multiple risks factors are simultaneously implicated in obesity (12). Identifying specific types of risks more likely to influence obesity early in life can directly inform interventions that could specifically target such risks. This study extends previous research by investigating profiles of social and behavioral risk associated with obesity among preschoolers.
Among younger children, those who experience social stressors are also more likely to experience behavioral problems (13). Longitudinal studies have documented a relationship between child behavior and obesity (14-17). Anderson and colleagues noted a modest association between externalizing behaviors among 24-month old children and higher Body Mass Index (BMI) at 24 months and through age 12 (14). A relationship between depressive symptoms and obesity has been documented among male and female adolescents and adults, (18) however among younger children the relationship has been noted only among girls (15, 19).
Less is known about the relationship between social stressors and obesogenic health behaviors, particularly among young children. While using food as a way to cope with stressful situations has been shown among adult populations, (20) in very young children, health behaviors may reflect their parent behaviors and/or the home environment (21). Furthermore, little is known about the relationship between sedentary lifestyle and stressful home environments. In a stressful home environment certain sedentary behaviors, such as television viewing, may be used as a tool to manage the child's time and keep him or her occupied. It may also be harder for a parent to maintain health-promoting routines in the household, such as regular bedtime and restricted television viewing, both factors associated with obesity.
Previous work showed that the association between cumulative social risk and childhood obesity among preschool children (4-6 years of age) was only apparent among girls enrolled in the Fragile Families and Child Wellbeing Study (6). However, little is known about the relationship between social risk factors and specific health behaviors among children, which may elucidate potential mechanisms explaining this relationship. Furthermore, in very young children the relationship between behavioral problems, health behaviors and obesity has not been examined. In this study, the relationship between social risk factors and obesogenic behavioral factors is examined, as well as the relationship between social factors, behavioral problems, health behaviors and obesity among five-year old boys and girls.
METHODS
Study Population
Analyses were conducted using public-use data available from the Fragile Families and Child Wellbeing Study, a prospective birth cohort study that follows a sample of mother-child pairs from 20 large cities in the US. Non-marital births were over-sampled relative to marital births in a ratio of 3 to 1. The study is a joint effort by Princeton University's Center for Research on Child Wellbeing (CRCW) and Center for Health and Wellbeing, Columbia University's Social Indicators Survey Center, and The National Center for Children and Families (NCCF) (http://www.fragilefamilies.princeton.edu). Details on the study design can be found in Reichman and colleagues 2001 (22). In brief, 4898 women were recruited from 75 hospitals during the birth of the child between 1998-2000 in 20 US cities with populations over 200,000. Random samples of both married and unmarried births were selected until preset quotas were reached. Upon completion of screening and determination of eligibility, consent was obtained. Mothers completed a baseline interview at delivery and participated in follow-up interviews when the children were approximately 12, 36 and 60 months of age. All children who remained in follow-up were asked to participate in an in-home assessment at the 60-month follow-up; 2489 completed the assessment. The 1589 children used in final analyses had complete information on the social risk factors of interest and height and weight information at the 60-month follow-up. Those who did not participate in the 60-month in-home assessment differed significantly by race/ethnicity from those who participated (Blacks, 46% non-participants vs. 50% participants p < .0001; Hispanics 28% non-participants vs. 24% participants p < .0001).
Social Risk Factors
Each of the six social risk factors was assessed at both the 12- and 36-month assessment.
Maternal Mental Health
Mothers answered the Composite International Diagnostic Interview – Short Form (CIDI-SF), (23) a screening for depression that is based on one of the most widely used structured diagnostic interviews to assess adult psychiatric disorders in epidemiological studies (24). The CIDI-SF was scored according to the developer's guidelines (http://www.fragilefamilies.princeton.edu/documentation/core/scales/ff_3yr_scales.pdf accessed June 03, 2010), which generates probable diagnosis of psychiatric disorders consistent with the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV; APA, 1994). To ascertain probable depression, mothers were initially asked if they experienced dysphoria (depression) or anhedonia (lack of enjoyment of what is often experienced as pleasurable) in the past year for a specific duration (two weeks or more, and if so, whether such symptoms lasted most of the day and occurred every day). If presence and persistence of symptoms were positive, mothers were asked about seven other symptoms, such as losing interest in typically enjoyable activities, trouble sleeping and thinking about death. A probable depression score resulted from adding up the answers to these seven symptoms plus the first dysphoric symptom, if present, ranging therefore from 0 to 8. A score of three or more is considered as a probable case. Also, if a mother reported taking antidepressants, she was considered as a probable case.
Maternal Substance Use
Mothers were asked whether in the past month they drank more than 5 alcoholic beverages in one day, had smoked pot or marijuana or if they had used cocaine, crack, LSD, speed, heroin or other hard drugs. In addition, mothers were asked whether alcohol/drugs had interfered with their daily life, personal relations or whether they had sought help or treatment for a drug or alcohol problem since the child's birth. Mothers affirming any of these questions were classified as using drugs/alcohol.
Intimate Partner Violence
Maternal IPV was assessed at the 12- and 36- month follow-up assessments, using previously validated questions (25, 26). Mothers were asked to think about their relationship with the baby's father or current partner and were then asked: 1) “How often does he slap or kick you?”; 2) “How often does he hit you with a fist or object that could hurt you?”; 3) “How often does he try to make you have sex or do sexual things you don't want to?”; and 4) “Were you ever cut or bruised or seriously hurt in a fight with the baby's father or current partner?” Mothers who responded ‘often’ or ‘sometimes’ as opposed to ‘never’ to either of the first three questions or who responded ‘yes’ to the last question were categorized as experiencing IPV for the relevant time period.
Housing Insecurity
Mothers were asked whether they had been evicted from their home in the past 12 months, stayed in shelter/car or abandoned vehicle, not paid full rent or mortgage or if they moved in with other people because of financial problems. These questions were derived from the Survey on Income and Program Participation (27) and the New York City Social Indicators Survey (28). Mothers affirming one or more of the above questions were categorized as experiencing housing insecurity.
Food Insecurity
Mothers were asked whether in the past 12 months they were ever hungry but could not afford to buy more food or whether their children were hungry but they could not afford to buy more food (27). Mothers endorsing either question were characterized as experiencing food insecurity.
Paternal Incarceration
Mothers were asked whether the father of the child was currently incarcerated.
Cumulative Social Index
The cumulative social index has been previously described (6). Briefly, dichotomous variables were created for each of the 6 social factors (probable maternal depression, IPV, maternal drug/alcohol use, housing insecurity, food insecurity, paternal incarceration) obtained at 12- and 36-month assessments. A score of 1 was assigned for each item endorsed for each of the 6 measures for each year. The cumulative score was created by summing over the dichotomous variables for both assessments and ranged from 0 to 12, with higher scores indicating a higher level of cumulative social risk, resulting in the total cumulative social risk score (Mean 1.3 SD 1.5).
Child Obesity
Trained interviewers measured height and weight with participants wearing light clothing and no shoes during the 60-month assessment (child age 5). A portable stadiometer (SECA 214 Road Rod Stadiometer) for height and an electronic scale (SECA 840 Bella Digital Scale, Hanover, MD) was used to measure weight. BMI was calculated from measured height and weight (kg/m2) measured at the 36-month follow-up. The Center for Disease Control and Prevention (CDC) BMI growth reference (29) was used to determine age- and gender-specific BMI percentiles (BMIp). Obesity at age 5 was defined as BMI >=95th percentile at the 5-year assessment.
Child Behavioral Problems
To assess child behavior, mothers where asked to complete the Child Behavior Checklist (CBCL) based on their child's behavior in the past two months during the 60-month follow-up (30, 31). The CBCL measures a series of symptoms, that include both internalizing (i.e., depressive, anxious, withdrawn) and externalizing (i.e., aggressive, destructive) behaviors. Items assessing specific behaviors were read to the mother who was asked to indicate whether the statement was (0) not true, (1) sometimes or somewhat true, or (2) very true or often true. Scores for the subscales can be calculated by adding the scores for each item allowing comparison to T scores and percentiles for the normalization sample of each subscale. As done in previous studies, behavioral problems were characterized as a T score greater than 65 considered a clinical score. These analyses focus on the CBCL externalizing and internalizing scales. Because of the high correlation between these two dimensions (Pearson= 0.49, p <0.001), they are considered separately in regression analysis
Health Behaviors
During the 60-month follow-up mothers were asked questions regarding their child's physical activity, sleep habits, TV, and dietary habits. Mothers were asked on average how many hours of TV the child watched on a typical weekday as well as the average hours of TV watched on a typical weekday. TV watching was categorized as watching 2 or more hours per day. Mothers were also asked on average how many hours a night the child sleeps. Lack of sleep was categorized as less than or equal to 9 hours based on established recommendations (32). To assess soda consumption, mothers were asked on a typical day how many servings of soda the child drank. Similarly, to assess fruit juice, mothers were asked to indicate how many servings of fruit juice the child drank in a typical day. Soda and fruit juice consumption was categorized as drinking 3 or more servings of soda or juice in a day.
Socio-demographic Factors
Data on child sex and child race/ethnicity (based on the mother's self-identified race/ethnicity as child's race/ethnicity was not collected) were collected on the baseline survey. Marital status of the parents (married/cohabitating or not married at child's birth), maternal education (some college, high school graduate, less than high school) and receipt of public assistance, were also considered.
Data Analysis
Inverse probability weighting (IPW) was used to adjust for potential selection bias (33, 34). The weights are the inverse of the probability of follow-up vs. loss to follow-up given baseline covariates, obtained with the use of binary logistic regression. Weights were assigned to each child (N=1589) to represent the full study sample.
Bivariate analyses were conducted to estimate the association between behavioral problems, health behaviors and cumulative social risk as well as the relationships between these risk factors and obesity stratified by gender. Due to the high prevalence of obesity, the odds ratio may not be a good approximation of the risk ratio, hence log binomial regression models were used to estimate prevalence ratios (PR) and estimate the associations between all the risk factors (social, behavioral and health behaviors) and obesity adjusting for socio-demographic factors. All analyses were weighted using IPW and conducted in SAS version 9.0 (SAS Institute, Cary, NC).
RESULTS
Table 1 shows the distribution of demographics, childhood obesity and study covariates. In the sample of 1589 children, 51% are boys, 51% African-American and 27% Hispanic (Table 1). Seventeen percent of children were obese at age 5. Seventeen percent and 4% of children had externalizing and internalizing scores at or above the clinical range. A greater number of girls were reported as sleeping 9 hours or less compared to boys. Boys were more likely to have internalizing behavioral problems than girls. No other gender differences were noted in the distribution of social risk factors, obesity, health behaviors or study covariates.
Table 1.
Demographics, Social risk Factors, Obesity and Health Behaviors, Fragile Families and Child Wellbeing Study (N=1589)
| Girls (N=782) | Boys (N=807) | p-value | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Race/Ethnicitya | |||||
| White | 172 | 22.0 | 183 | 22.7 | 0.60 |
| African American | 390 | 49.9 | 413 | 51.2 | |
| Hispanic/Other | 220 | 28.1 | 211 | 26.2 | |
| Mothers Highest Education Attained | |||||
| Some College/College Grad | 288 | 36.8 | 284 | 35.2 | 0.48 |
| High School Graduate | 200 | 25.6 | 228 | 28.3 | |
| Less than High School | 294 | 37.6 | 295 | 36.6 | |
| Mothers Marital Status: Married or Cohabitating | 503 | 64.3 | 500 | 62.0 | 0.33 |
| Income from Public Assistance | 190 | 24.3 | 221 | 27.4 | 0.16 |
| Obesity at age 5 | 141 | 18.0 | 129 | 16.0 | 0.28 |
| Cumulative Social Risk | |||||
| None | 340 | 43.5 | 332 | 41.1 | 0.60 |
| One | 181 | 23.2 | 189 | 23.4 | |
| Two | 261 | 33.4 | 286 | 35.4 | |
| Externalizing problems | 137 | 17.5 | 126 | 15.6 | 0.31 |
| Internalizing problems | 23 | 2.9 | 45 | 5.6 | 0.01 |
| Sleep < =9hrs | 425 | 54.4 | 382 | 47.3 | 0.005 |
| TV > 2hrs | 485 | 62.2 | 508 | 63.0 | 0.70 |
| Soda/Juice >=3 day | 495 | 63.4 | 491 | 60.8 | 0.31 |
Based on mother's race/ethnicity
In bivariate analyses of the associations between social risk factors and obesity, experiencing more than one social risk factor was associated with obesity among girls but not boys (40.4% vs 31.8%, girls, p < 0.05) (Table 2). Externalizing behavioral problems were associated with obesity among girls (26.2% vs 15.6%, p < 0.05). Watching more than 2 hours of television per day was associated with obesity among boys (72.9% vs 61.1%, p < 0.05) (Table 2). No associations between health behaviors and obesity were noted among girls.
Table 2.
Unadjusted association between obesity, social risk and health behaviors, stratified by gender, Fragile Families and Child Wellbeing Study (N=1589).
| Girls N=782 | Boys N=807 | |||||
|---|---|---|---|---|---|---|
| Non-Obese % | Obese % | p-value | Non-Obese % | Obese % | p-value | |
| Cumulative Social Risk | ||||||
| None | 45.6 | 34.0 | 40.9 | 42.6 | ||
| One | 22.6 | 25.5 | 0.09a | 24.0 | 20.2 | 0.40a |
| Two | 31.8 | 40.4 | 0.01a | 35.1 | 37.2 | 0.94a |
| Externalizing problems | 15.6 | 26.2 | 0.004 | 14.6 | 20.9 | 0.07 |
| Internalizing problems | 2.8 | 3.6 | 0.64 | 5.6 | 4.7 | 0.62 |
| Sleep < =9hrs | 53.0 | 60.3 | 0.12 | 46.6 | 51.2 | 0.34 |
| TV > 2hrs | 61.0 | 66.7 | 0.21 | 61.1 | 72.9 | 0.01 |
| Soda/Juice >=3 day | 63.3 | 63.1 | 0.96 | 60.6 | 62.0 | 0.76 |
Compared to no risk factors
Figures 1 and 2 show the prevalence of behavioral problems and health behaviors by cumulative social risk group. Boys and girls who experienced two or more social risk factors had higher prevalence of externalizing behavioral problems compared to those experiencing no risk factors (26% vs. 8% boys; 24% vs. 12% girls, p < 0.05). Furthermore, experiencing two or more social risk factors compared to none, was significantly associated with lack of sleep (51% vs. 39%), television watching for more than 2 hours a day (72% vs. 55%), and high soda and juice consumption (67% vs. 54%) among boys (all p < 0.05) (Figure 1). Among girls, cumulative social risk was associated with soda and juice consumption (69% vs. 59%, p< 0.05) (Figure 2).
Figure 1.
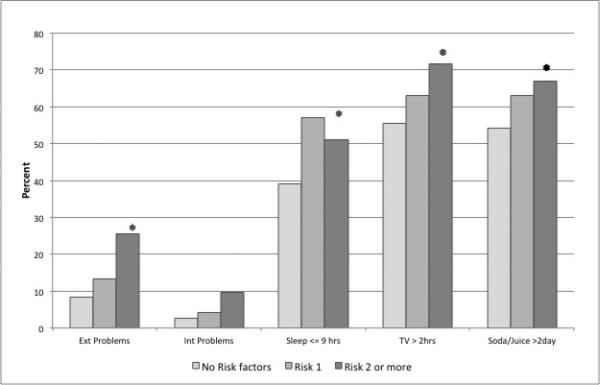
Prevalence of health behaviors and behavioral problems by cumulative social risk group for boys, Fragile Families and Child Wellbeing Study
*p < 0.05 , compared to no risk factors
Figure 2.
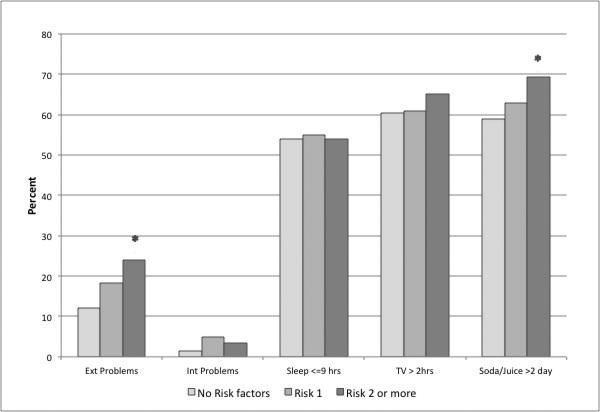
Prevalence of health behaviors and behavioral problems by cumulative social risk group for girls, Fragile Families and Child Wellbeing Study
*p < 0.05, compared to no risk factors
In fully adjusted models, cumulative social risk remained associated with obesity among girls, but not boys (Table 3). Externalizing behavioral problems (girls PR 1.5 95%CI 1.2, 1.7 and boys PR 1.3 95%CI 1.1, 1.6) and lack of sleep (girls PR 1.2 95%CI 1.0, 1.4 and boys PR 1.3 95%CI 1.1, 1.5) were associated with obesity among both boys and girls. Television viewing for more than 2 hours a day was associated with obesity among boys (PR 1.5 95%CI 1.2, 1.9) but not girls.
Table 3.
Cumulative social risk, behavioral problems, health and obesity at age 5, Fragile Families and Child Wellbeing Study (N=1589)
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Girls PR 95%CI | Boys PR 95%CI | Girls PR 95%CI | Boys PR 95%CI | |
| Cumulative Social Risk | ||||
| None | Reference | Reference | Reference | Reference |
| One | 1.32 (1.1,1.6)* | 0.82 (0.6,1.0) | 1.34 (1.1,1.7)* | 0.81 (0.6, 1.0) |
| Two or more | 1.54 (1.3,1.9)* | 0.92 (0.8,1.1) | 1.61 (1.3,2.0)* | 0.96 (0.8, 1.2) |
| Externalizing problems | 1.46 (1.2,1.7)* | 1.34 (1.1,1.6)* | ------- | ------ |
| Internalizing problems | ----- | ------ | 0.99 (0.6,1.65 | 0.68 (0.4,1.0) |
| Sleep < =9hrs | 1.20 (1.0,1.4)* | 1.27 (1.1,1.5)* | 1.25 (1.1,1.5)* | 1.30 (1.1,2.3)* |
| TV > 2hrs | 1.05 (0.9,1.3) | 1.52 (1.2,1.9)* | 1.05 (0.9,1.3) | 1.56 (1.3,1.9)* |
| Soda/Juice >=3 day | 0.83 (0.7,1.0) | 0.98 (0.8,1.2) | 0.89 (0.7, 1.1) | 0.99 (0.8,1.2) |
p < 0.05
Model 1 includes externalizing behaviors and excludes internalizing behaviors and is further adjusted for race/ethnicity, maternal education, maternal marital status, and receipt of public assistance.
Model 2 includes internalizing behaviors and excludes externalizing behaviors and is further adjusted for race/ethnicity, maternal education, maternal marital status, and receipt of public assistance.
DISCUSSION
This study examined the relationship between multiple social risk factors, behaviors and childhood obesity in a longitudinal study of urban five-year-old children. In adjusted analyses, externalizing behaviors, short sleep duration and TV watching were all associated with obesity among boys. Among girls, cumulative social risk factors, externalizing problems and short sleep duration were associated with obesity even after accounting for a number of socio-demographic factors. Cumulative risk factors were associated with externalizing behaviors and soda/juice consumption among boys and girls and with sleep duration and TV watching among boys.
The relationship between social risk factor and health behaviors is consistent with other studies, which have noted associations between stressful environments and sleep habits (35) and internalizing and externalizing behaviors (36) among children. Associations were also noted between soda/juice consumption, TV watching and social risk factors. In a stressful environment parents may not be emotionally available to care for the needs of the child and thus be more inclined to use a TV to occupy the child or give in to a child's request for soda/juice. However with the exception of soda/juice consumption, these associations were only evident among boys. It is plausible that observed gender differences are associated with socially acceptable strategies to manage stress-related behavioural problems in children that are linked to the child's sex.
Associations between behavioral problems and obesity were also noted. Similar associations have been previously documented between externalizing behaviors and obesity as was noted in this study among five-year-old boys and girls (14). Anderson and colleagues recently documented a relationship between externalizing behaviors and BMI among children. Externalizing behaviors are indicative of more impulsivity, poor inhibitory control and lack of self-regulation. In a recent study, Graziano and colleagues demonstrated that low self regulation among toddlers, as well as low inhibitory control skills/higher reward sensitivity, is associated with obesity at age 5 (37). Children with higher reward sensitivity may engage in impulsive eating and may request foods that are sweet and high in fat which are reportedly tastier than healthier/bland foods. In a Dutch study of 6-13 year old children, impulsivity and reward responsiveness were associated with childhood BMI, indirectly through overeating (38). We furthermore note that externalizing behaviors but not internalizing behaviors were associated with obesity. This is contrary to other studies, which have noted associations between internalizing behaviors (depression) and obesity particularly among girls. Possible differences could be attributed to the age of the sample and the low prevalence of internalizing problems in this sample. While most internalizing behaviors have been associated with obesity among adolescents this sample is considerably younger. Only one study, to our knowledge, has documented a relationship between internalizing behaviors among children entering kindergarten and obesity (39) noting a significant cross-sectional association between parent rated and teacher rated internalizing behaviors and obesity among girls (39).
Among girls, the relationship between social risk factors and obesity appears to be independent of health behaviors and behavioral problems. Suggesting other factors associated with social stress are responsible for the associations noted. Alternatively, it is plausible that the measures used are too imprecise. For example while the CBCL is a well validated measure to assess child behavioral problems it was not designed to specifically measure impulsivity or reward sensitivity specific behaviors that have been associated with obesity among children.
Furthermore, the health behavior measures used are limited in that diet and overall physical activity was not specifically assessed, and furthermore these factors were only assessed at the five-year follow-up which may be attributing to the lack of association. It is also plausible other factors, not assessed, such as emotional eating or emotional regulation are responsible for these associations. While a test for mediation was not conducted in these analyses due to the timing of data collection for these behaviors and obesity, the co-occurrence of health behaviors, behavioral problems and obesity was examined in this cohort of pre-school children. Despite these limitations the current study has a number of strengths. The analyses are based on a national sample of mainly children of low socioeconomic status, with objectively measured height and weight. Furthermore, the study jointly explores the association between social risk factors, obesity and behavior, which had not been done previously.
In these analyses associations were noted between the cumulative exposure to social risk factors, behavioral problems, health behaviors and obesity among five-year-old children. Disentangling the mechanisms linking social risk factors in early life, child behavior, and obesity among young children can better inform intervention and prevention efforts to curb childhood obesity. If social risk factors and behavioral problems are the upstream contributors of obesogenic health behaviors (i.e., excess TV watching, lack of sleep), more effective prevention and intervention efforts can be developed to target these health behaviors and thus prevent childhood obesity and its consequences. If replicated, these findings lend support to efforts to further explicate profiles of social risk, behavioral problems, and health behaviors that are associated with obesity risk among preschool children.
Acknowledgements
Dr. Suglia was supported by Grant Number 7K01HL103199-03. Dr. Duarte was supported by Grant Number R21HD056170 from National Institute of Child Health and Human Development (NICHD). Dr. Earle Chambers was supported by the John D. and Catherine T. MacArthur Foundation. Dr. Boynton-Jarrett was supported by the William T Grant Foundation and Grant Number K12HD43444. The Fragile Families and Child Wellbeing Study was supported by Grant Number R01HD36916 from NICHD. The contents of the paper are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Health.
Footnotes
Conflict of Interest: None to Declare
All authors state no conflict of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bethell C, Simpson L, Stumbo S, Carle AC, Gombojav N. National, state, and local disparities in childhood obesity. Health Aff (Millwood) 2010 Mar-Apr;29(3):347–56. doi: 10.1377/hlthaff.2009.0762. [DOI] [PubMed] [Google Scholar]
- 2.Obesity prevalence among low-income, preschool-aged children - United States, 1998-2008. MMWR Morb Mortal Wkly Rep. 2009 Jul 24;58(28):769–73. [PubMed] [Google Scholar]
- 3.Boynton-Jarrett R, Fargnoli J, Suglia SF, Zuckerman B, Wright RJ. Association between maternal intimate partner violence and incident obesity in preschool-aged children: results from the fragile families and child well-being study. Arch Pediatr Adolesc Med. 2010 Jun;164(6):540–6. doi: 10.1001/archpediatrics.2010.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garasky S, Stewart SD, Gundersen C, Lohman BJ, Eisenmann JC. Family stressors and child obesity. Soc Sci Res. 2009 Dec;38(4):755–66. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obes Rev. 2010 Nov 3; doi: 10.1111/j.1467-789X.2010.00813.x. [DOI] [PubMed] [Google Scholar]
- 6.Suglia SF, Duarte CS, Chambers EC, Boynton-Jarrett R. Cumulative Social Risk and Obesity in Early Childhood. Pediatrics. 2012 Apr 16; doi: 10.1542/peds.2011-2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012 Jan;129(1):e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 8.Whitaker RC, Phillips SM, Orzol SM, Burdette HL. The association between maltreatment and obesity among preschool children. Child Abuse Negl. 2007 Nov-Dec;31(11-12):1187–99. doi: 10.1016/j.chiabu.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gibson LY, Byrne SM, Davis EA, Blair E, Jacoby P, Zubrick SR. The role of family and maternal factors in childhood obesity. Med J Aust. 2007 Jun 4;186(11):591–5. doi: 10.5694/j.1326-5377.2007.tb01061.x. [DOI] [PubMed] [Google Scholar]
- 10.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity. 2008 Feb;16(2):265–74. doi: 10.1038/oby.2007.63. [Meta-Analysis Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Review] [DOI] [PubMed] [Google Scholar]
- 11.Gillis LJ, Bar-Or O. Food away from home, sugar-sweetened drink consumption and juvenile obesity. J Am Coll Nutr. 2003 Dec;22(6):539–45. doi: 10.1080/07315724.2003.10719333. [DOI] [PubMed] [Google Scholar]
- 12.Wells NM, Evans GW, Beavis A, Ong AD. Early childhood poverty, cumulative risk exposure, and body mass index trajectories through young adulthood. Am J Public Health. 2010 Dec;100(12):2507–12. doi: 10.2105/AJPH.2009.184291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Soc Sci Med. 2006 Jan;62(1):13–27. doi: 10.1016/j.socscimed.2005.05.030. [DOI] [PubMed] [Google Scholar]
- 14.Anderson SE, He X, Schoppe-Sullivan S, Must A. Externalizing behavior in early childhood and body mass index from age 2 to 12 years: longitudinal analyses of a prospective cohort study. BMC Pediatr. 2010;10:49. doi: 10.1186/1471-2431-10-49. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003 Apr;111(4 Pt 1):851–9. doi: 10.1542/peds.111.4.851. [Comparative Study Multicenter Study Research Support, U.S. Gov't, P.H.S.] [DOI] [PubMed] [Google Scholar]
- 16.Lumeng JC, Gannon K, Cabral HJ, Frank DA, Zuckerman B. Association between clinically meaningful behavior problems and overweight in children. Pediatrics. 2003 Nov;112(5):1138–45. doi: 10.1542/peds.112.5.1138. [Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 17.Duarte CS, Sourander A, Nikolakaros G, Pihlajamaki H, Helenius H, Piha J, et al. Child mental health problems and obesity in early adulthood. The Journal of Pediatrics. 2010 Jan;156(1):93–7. doi: 10.1016/j.jpeds.2009.06.066. [Research Support, Non-U.S. Gov't] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002 Sep;110(3):497–504. doi: 10.1542/peds.110.3.497. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.] [DOI] [PubMed] [Google Scholar]
- 19.Anderson SE, Cohen P, Naumova EN, Must A. Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Arch Pediatr Adolesc Med. 2006 Mar;160(3):285–91. doi: 10.1001/archpedi.160.3.285. [DOI] [PubMed] [Google Scholar]
- 20.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007 Nov-Dec;23(11-12):887–94. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 21.Parks EP, Kumanyika S, Moore RH, Stettler N, Wrotniak BH, Kazak A. Influence of stress in parents on child obesity and related behaviors. Pediatrics. 2012 Nov;130(5):e1096–104. doi: 10.1542/peds.2012-0895. [Research Support, N.I.H., Extramural Research Support, U.S. Gov't, P.H.S.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reichman N, Teitler J, Garfinkel I, McLanahan S. Fragile Families: Sample and Design. Children and Youth Services Review. 2001;23(4/5):303–26. [Google Scholar]
- 23.Kessler R, Andrews G, Mroczek D, Ustun T, Wittchen H. The World Health Organization Composite International Diagnostic Interview Short-From (CIDI-SF). International Journal of Methods in Psychiatric Research. 1998;7:171–85. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kessler RC, Wittchen H-U, Abelson JM, McGonagle KA, Schwarz N, Kendler KS, et al. Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US National Comorbidity Survey. International Journal of Methods in Psychiatric Research. 1998;7:33–55. [Google Scholar]
- 25.Lloyd S. The effects of domestic violence on women's employment. Law and Policy. 1997;19:139–67. [Google Scholar]
- 26.Sweet J, Bumpass L, Call V. NSFH Working Paper #1: Center for Demography and Ecology. University of Wisconsin-Madison; 1988. The Design and Content of The National Survey of Families and Households. [Google Scholar]
- 27.Survey on Income and Program Participation [database on the Internet] United States Census Bureau; 1996. [Google Scholar]
- 28.Garfinkel I, Meyers M. New York City Social Indicators 1997 A Tale of Many Cities. Columbia University School of Social Work, Center NYCSIS; New York: 1997. [Google Scholar]
- 29.Statistics NCfH . 2000 CDC Growth Charts: United States. Hyattsville, MD: 2004. [Google Scholar]
- 30.Achenbach TM. Manual for the Child Behavior Checklist / 2-1 and 1992 Profile. Univeristy of Vermont Department of Psychiatry; Burlington, VT: 1992. [Google Scholar]
- 31.Achenbach TM, Rescorla L. Manual for the ASEBA Preschool Forms and Profiles. University of Vermont, Research Center for Children, Youth & Families; Burlington, VT: 2000. [Google Scholar]
- 32.Matricciani LA, Olds TS, Blunden S, Rigney G, Williams MT. Never enough sleep: a brief history of sleep recommendations for children. Pediatrics. 2012 Mar;129(3):548–56. doi: 10.1542/peds.2011-2039. [Review] [DOI] [PubMed] [Google Scholar]
- 33.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000 Sep;11(5):550–60. doi: 10.1097/00001648-200009000-00011. [Research Support, U.S. Gov't, P.H.S.] [DOI] [PubMed] [Google Scholar]
- 34.Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004 Sep;15(5):615–25. doi: 10.1097/01.ede.0000135174.63482.43. [Research Support, U.S. Gov't, P.H.S.] [DOI] [PubMed] [Google Scholar]
- 35.Spilsbury JC. Sleep as a mediator in the pathway from violence-induced traumatic stress to poorer health and functioning: a review of the literature and proposed conceptual model. Behav Sleep Med. 2009;7(4):223–44. doi: 10.1080/15402000903190207. [Research Support, N.I.H., Extramural Review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Augustyn M, Frank DA, Posner M, Zuckerman B. Children who witness violence, and parent report of children's behavior. Arch Pediatr Adolesc Med. 2002 Aug;156(8):800–3. doi: 10.1001/archpedi.156.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Graziano PA, Calkins SD, Keane SP. Toddler self-regulation skills predict risk for pediatric obesity. Int J Obes (Lond) 2010 Apr;34(4):633–41. doi: 10.1038/ijo.2009.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van den Berg L, Pieterse K, Malik JA, Luman M, Willems van Dijk K, Oosterlaan J, et al. Association between impulsivity, reward responsiveness and body mass index in children. Int J Obes. 2011 Oct;35(10):1301–7. doi: 10.1038/ijo.2011.116. [Multicenter Study Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 39.Datar A, Sturm R. Childhood overweight and parent- and teacher-reported behavior problems: evidence from a prospective study of kindergartners. Arch Pediatr Adolesc Med. 2004 Aug;158(8):804–10. doi: 10.1001/archpedi.158.8.804. [Research Support, U.S. Gov't, P.H.S.] [DOI] [PubMed] [Google Scholar]


