Abstract
Study Design
Retrospective cohort study of the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database from 2005 to 2010 that included 1,861 patients who had undergone elective posterior lumbar fusion.
Objective
To characterize factors that were independently associated with increased hospital length of stay (LOS) in patients who had undergone elective posterior lumbar fusion.
Summary of Background Data
Posterior lumbar spine fusion is a common surgical procedure used to treat lumbar spine pathology. LOS is an important clinical variable and a major determinant of inpatient hospital costs. There is lack of studies in the literature using multivariate analysis to specifically examine the predictors of LOS after elective posterior lumbar fusion.
Methods
Patients who underwent elective posterior lumbar fusion from 2005 to 2010 were identified in the ACS-NSQIP database. Preoperative and intraoperative variables were extracted for each case and a multivariate linear regression was performed to assess the contribution of each variable to LOS.
Results
A total of 1,861 elective posterior lumbar fusion patients were identified. The average age for patients in this cohort was 60.6 ± 13.9 years (mean ± standard deviation [SD]) with a body mass index (BMI) of 30.3 ± 6.2 kg/m2. 44.7% of patients were male. LOS ranged from 0 days to 51 days. Multivariate linear regression identified age (p < 0.001), morbid obesity (BMI ≥ 40 kg/m2, p < 0.001), American Society of Anesthesiologists (ASA) class (p = 0.001), operative time (p < 0.001), multilevel procedure (p = 0.001), and intraoperative transfusion (p < 0.001) as significant predictors of extended LOS.
Conclusion
The identified preoperative and intraoperative variables associated with extended LOS after elective posterior lumbar fusion may be helpful to clinicians for patient counseling and postoperative planning.
Keywords: length of stay, elective, fusion, lumbar, outcomes, complications, NSQIP, preoperative, intraoperative, postoperative, age, BMI, ASA, operative time, levels, transfusion
Introduction
Posterior lumbar fusion is a common surgical procedure used to treat lumbar spine pathology and is associated with favorable outcomes and low morbidity.1 The average cost of a lumbar fusion ranges from $80,000 to $112,000 per patient, with costs having doubled over the past decade.2,3 Inpatient charges associated with each surgery are closely linked with length of stay (LOS),4,5 and longer hospital stays are associated with increased risk of complications such as postoperative infection,6 venous thromboembolism,6 and delirium.7 In order to reduce costs and provide realistic expectations for patients and providers, it is critical to identify factors that affect length of stay.
Previous studies have described individual factors that contribute to increased length of stay after spine surgery, such as morbid obesity,8 metabolic syndrome,9 black race,10 open surgery versus minimally invasive surgery,11 age,12 chronic obstructive pulmonary disease (COPD),13 antidepressant use,14 unemployment,15 chronic renal disease,15 and intraoperative fluid volume.16 However, these were generally small studies that examined isolated factors, leaving significant room for the effects of confounding variables.
Multivariate analysis has been used previously in the spine literature to identify factors affecting LOS after revision lumbar fusion17 and one-level minimally invasive posterior lumbar interbody fusion and instrumentation.18 These studies identified that age, number of levels fused, fluid balance, narcotic use, and preoperative hemoglobin, among other variables, affect LOS. However, as of this writing, no study has used multivariate analysis to determine which factors affect LOS following primary posterior lumbar fusion. In this study, we use a multivariate linear regression model to determine which preoperative and intraoperative variables affect LOS for patients after elective posterior lumbar fusion. By identifying these factors, modifiable factors could potentially be optimized preoperatively and non-modifiable factors can be used for postoperative planning and patient counseling.
Materials and Methods
Data source
The National Surgical Quality Improvement Program (NSQIP) began as a healthcare quality improvement initiative in the Veteran's Administration (VA) health system in 1994.19 After successful implementation in the VA, the American College of Surgeons (ACS) launched a parallel program for high-volume hospitals outside the VA health system in 1999.20 The ACS-NSQIP database is available to participating hospitals in the United States.
In the NSQIP, more than 135 preoperative, intraoperative, and 30-day postoperative variables are prospectively abstracted from operative reports, medical records, and patient interviews to assess 30-day adjusted surgical outcomes.20 Patients are identified prospectively and randomly sampled at eligible hospitals. Clinical data are collected in the entire 30-day postoperative period, regardless of discharge status within this time.
Study population
The NSQIP database from 2005 to 2010 was used in this study. Posterior lumbar fusion cases were identified using Common Procedural Terminology (CPT) code 22612, which includes minimally invasive and open posterior lumbar fusion cases. Patients who underwent combined anterior-posterior lumbar fusion, concomitant cervical or thoracic spine procedures, other unrelated surgical procedures, or emergent procedures were excluded from analysis.
Data collection
Among the variables available in the NSQIP are independent patient characteristics including sex, age, height, and weight, as well as history of tobacco (current smoker within one year) and alcohol use (greater than two drinks per day within two weeks prior to admission). Body mass index (BMI) was calculated from each patient's height and weight, and morbid obesity was defined as BMI ≥ 40 kg/m2. The NSQIP also includes information on medical comorbidities, including any history of diabetes, hypertension, pulmonary comorbidities, cardiac comorbidities, and American Society of Anesthesiologists (ASA) class. A pulmonary comorbidity was defined as a history of severe chronic obstructive pulmonary disease, requiring ventilator-assisted respiration within 48 hours before surgery, or current pneumonia. Cardiac comorbidity was defined as a history of congestive heart failure (within 30 days before admission), myocardial infarction (within six months before admission), cardiac surgery, percutaneous coronary intervention, or angina (within one month before admission). ASA class ≥ 3 corresponds to severe systemic disease. 21
Intraoperative variables collected include the number of levels operated on, operative time, and any blood transfusions required. Multilevel surgery was defined as any surgery involving more than one spinal level and operative time was dichotomized into operative time ≥ 75th percentile (increased operative time) and operative time < 75th percentile (normal operative time) for this cohort.
Length of stay (LOS)
The primary clinical outcome in this study was length of stay (LOS), defined as the number of calendar days from the operation to hospital discharge. For bivariate analyses, patients were categorized based on LOS as normal LOS (< 75th percentile LOS) or extended LOS (≥ 75th percentile LOS). For multivariate analysis, LOS was treated as a continuous variable so that the magnitude of the effect of each predictor variable on LOS could be determined.
Statistical analysis
SPSS v.19 (IBM, Chicago, IL) was used for all statistical analysis. All tests were two-tailed and the statistical difference was established at a two-sided α level of 0.05 (p < 0.05). Bivariate analyses compared baseline demographic, comorbidity, and operative variables between the normal and extended LOS cohorts. Throughout the study, chi-square and Student t-tests were performed for categorical and continuous variables, respectively.
Multivariate linear regression was performed with LOS as the continuous outcome variable. Preoperative variables included in the model were demographic and comorbidity variables, and intraoperative factors included in the model were operative time, number of operative levels, and any intraoperative transfusions. Co-linearity tests were performed for all independent variables in the model, and standardized and unstandardized beta coefficients from the model were reported.
Results
A total of 1,861 elective posterior lumbar fusion patients were identified that met inclusion criteria. A summary of patient demographics can be found in Table 1, first data column. The average age for patients in this cohort was 60.6 ± 13.9 years (mean ± standard deviation [SD]) with a BMI of 30.3 ± 6.2 kg/m2. This sample was 44.7% male.
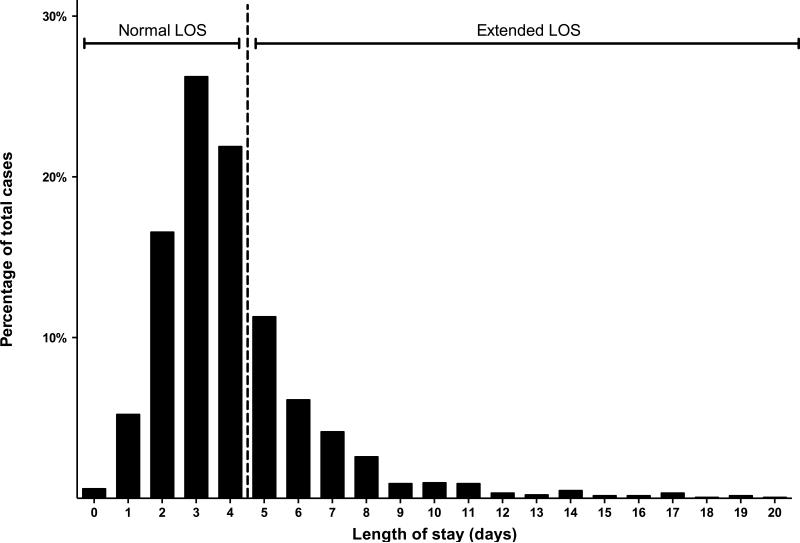
LOS ranged from 0 days (same-day discharge after surgery) to 51 days. Based on the definition of extended LOS as greater than or equal to 75th percentile LOS (≥ 5 days for this cohort), 549 patients (29.5%) were categorized as extended LOS. Figure 1 illustrates the distribution of length of stay, with the vertical dashed line separating normal and extended LOS cohorts.
Figure 1.
Length of stay (LOS) following elective posterior lumbar fusion. Cases with extended length of stay (LOS ≥ 75th percentile or 5 days) are to the right of the vertical dashed line.
Bivariate analyses were then performed to test the effect of each preoperative and operative variable on LOS by comparing normal LOS and extended LOS groups. The results of these analyses can be seen in Table 1. There were significant differences between normal and extended LOS groups for most variables. These included age, BMI, smoking history, ASA class, diabetes, hypertension, pulmonary comorbidity, cardiac comorbidity, operative time, multilevel procedures, and intraoperative transfusion. The normal LOS group had an average LOS of 2.9 ± 1.0 days, while the extended LOS group had an average LOS of 7.4 ± 4.5 days.
Multivariate linear regression was then performed. The results of this analysis can be seen in Table 2. Several factors that had been significant predictors of extended LOS on bivariate analysis were not significant on multivariate analysis. This suggests covariance between variables, with multivariate analysis unmasking the true driving factors for extended LOS. Unstandardized and standardized beta values are reported for each variable in Table 2. Unstandardized beta values represent the change in LOS (in days) for each predictor variable, and standardization of beta values allow the relative effects of predictor variables to be directly compared to one another.
Among preoperative variables, significant predictors of increased hospital LOS were age (Standardized β = 0.142, p < 0.001), morbid obesity (Standardized β = 0.108, p < 0.001), and ASA class (Standardized β = 0.088, p = 0.001). Sex, smoking history, alcohol history, diabetes, hypertension, pulmonary comorbidity, and cardiac comorbidity are all preoperative variables that were not significantly associated with length of stay. Intraoperative variables that were significantly associated with extended LOS were operative time ≥ 75th percentile or 268 minutes (Standardized β = 0.127, p < 0.001), multilevel procedure (Standardized β = 0.094, p = 0.001) and intraoperative transfusion (Standardized β = 0.222, p < 0.001).
Discussion
Hospital length of stay (LOS) after posterior lumbar fusion is important to patients and providers, yet there is no consensus on which factors are associated with extended LOS after posterior lumbar fusion.1,4,5,9-18 This study was thus designed to determine which factors affect LOS after elective posterior lumbar fusion and the relative effects of each factor on LOS. Using the NSQIP database, a total of 1,861 elective posterior lumbar fusion patients were identified and had preoperative and intraoperative variables extracted for each case. Multivariate analysis was performed on preoperative and intraoperative variables to identify factors affecting LOS that a surgeon could use for preoperative patient counseling and postoperative planning.
Preoperative variables that were shown to be significant predictors of extended LOS in the final multivariate linear regression model were age, morbid obesity, and ASA class. Intraoperative variables that were significant in the final model were operative time, multilevel procedure, and intraoperative transfusion. Sex, smoking history, alcohol history, diabetes, hypertension, pulmonary comorbidity, and cardiac comorbidity were not significantly associated with length of stay.
When looking at preoperative variables, it is not surprising that we found age to be associated with extended LOS, as increased age is often associated with greater comorbidities. However, multivariate analysis showed that age was an independent predictor of increased length of stay after adjusting for comorbidities. In fact, age had the largest effect on LOS of the three significant preoperative variables, and had the second-largest effect on LOS out of all variables included in the multivariate model. According to our model, for each additional decade over age 40, LOS increases by approximately one-third of a day.
Age has been found to be a significant predictor of extended LOS in previous studies.12,17 Zheng and colleagues used multivariate analysis to study 112 patients who underwent revision posterior lumbar fusion between 1992 and 1999 and found that increasing age was the only significant predictor of a longer hospital stay.17 A more recent study by Nie et al. reports differences in LOS between age groups after lumbar discectomy.12
It may also not be surprising that morbid obesity (BMI ≥ 40 kg/m2) is associated with extended LOS. Of note, morbid obesity was associated with extended LOS independent of comorbidities typically associated with obesity, such as diabetes and hypertension. These results regarding obesity are in line with previous studies that have detected an association between obesity and extended LOS. Kalanithi et al. looked at 1,455 morbidly obese patients who had undergone any type of spinal fusion from 2003 to 2007 and found that morbid obesity was associated with 97% higher in-hospital complication rates, increased mortality, and significantly longer LOS.8 Memtsoudis et al. used the National Inpatient Sample (NIS) to study patients with metabolic syndrome who had undergone posterior lumbar fusion, and found that metabolic syndrome was an independent risk factor for extended LOS, higher rates of non-routine discharge, and increased rates of major life-threatening complications compared to patients without metabolic syndrome.9 Walid et al. also found that obesity was associated with increased length of stay after spine surgery.13
The American Society of Anesthesiologists (ASA) classification system is a method for anesthesiologists to assess preoperative risk in patients undergoing surgery.21 This study confirms that ASA class can be useful to risk-stratify patients, as our results indicate that ASA class ≥ 3 is associated with extended LOS following elective posterior lumbar fusion. While the ASA classification system takes into account patient comorbidities, it is interesting that ASA class was independently associated with extended LOS. This may be because increased ASA class is associated with an increased number of comorbidities, which may mask the contributions of each individual comorbidity in the multivariate model. It is also possible that the independent association of the ASA class with LOS is because it takes into account additional factors that were not included in this analysis, as the range of comorbidities that fall into the “severe systemic disease” category used to determine ASA classes 3 and above is broad. ASA class has also been found to correlate with other surgical outcomes such as intraoperative blood loss and postoperative surgical site infection in the orthopaedic literature.22,23
Increased operative time (specifically operative time ≥ 75th percentile or 268 minutes) was an intraoperative variable that we found to be significantly associated with extended LOS. One explanation is that increased operative time is generally associated with more complex cases and also may be caused by intraoperative complications. Additionally, increased intraoperative time may be associated with increased intraoperative fluid administration. Increased intraoperative fluid administration has shown to correlate with extended LOS in previous studies.16,18
The second intraoperative variable that was significantly associated with extended LOS was the number of levels fused. Multilevel procedures may also be associated with increased operative time and intraoperative transfusion; however, all of these factors were found to be independent predictors in the final multivariate model while demonstrating low co-linearity. Zheng et al. also found that number of levels fused was a predictor of extended LOS after revision posterior lumbar fusion.17
Intraoperative transfusion was the last intraoperative factor that was significantly associated with extended LOS after elective posterior lumbar fusion and had the greatest overall effect on LOS. While the criteria for intraoperative transfusion may vary between institutions sampled by the NSQIP, the use of intraoperative transfusion signifies the presence of preoperative anemia and/or increased intraoperative blood loss. Decreased preoperative hemoglobin and increased intraoperative blood loss have both been shown to significantly extend LOS after spine surgery.18
Interestingly, several factors did not correlate with extended LOS in our study. Sex, smoking history, alcohol history, diabetes, hypertension, pulmonary comorbidity, and cardiac comorbidity are all preoperative variables that were not significantly associated with extended LOS. While it is intuitive that sex should not affect LOS, it is interesting to note that all comorbidities, except alcohol history, were significant in bivariate analysis, yet none were significant in the final multivariate model. As mentioned before, this is likely because age and ASA class, which were significant in the multivariate model, are associated with increased comorbidities of any type. When unique comorbidities are entered into the model alongside age and ASA, their individual contributions to LOS are diminished. Nonetheless, these factors did not prove to be significant despite the large sample size of this study.
When using a large dataset such as the NSQIP database, there are several limitations. While significant efforts were made by the NSQIP to collect as many patient variables as possible, some information was not captured. Information such as narcotic use, antidepressant use, employment status, open versus closed procedures, and intraoperative fluid volume, all of which were found to affect LOS in previous studies, were not available for this dataset.
Despite its limitations, the NSQIP database is a valuable resource when used to analyze the effects of many patient variables on outcome measures such as LOS for a large number of patients. This study used the powerful tool of multivariate analysis to identify six preoperative and intraoperative factors that are independently associated with extended LOS after elective posterior lumbar fusion. Each factor has support in the spine literature for this effect. The identification of these factors may be useful for preoperative discussion and postoperative planning.
Supplementary Material
Key Points.
Length of stay (LOS) after surgical procedures is important to patients and providers, yet there has been no multivariate study of factors affecting LOS after elective posterior lumbar fusion.
Using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database, elective posterior lumbar fusions were identified and a multivariate linear regression was performed to assess the contribution of preoperative and intraoperative factors to LOS.
Age, morbid obesity (BMI ≥ 40 kg/m2), American Society of Anesthesiologists (ASA) class, operative time, multilevel procedure, and intraoperative transfusion were all independently associated with a significant increase in hospital LOS after elective posterior lumbar fusion.
Among preoperative and intraoperative variables, intraoperative transfusion had the greatest overall effect on LOS, while age was the strongest preoperative predictor of extended LOS following elective posterior lumbar fusion.
Sex, smoking history, alcohol history, diabetes, hypertension, pulmonary comorbidity, and cardiac comorbidity are all preoperative variables that were not significantly associated with extended LOS following elective posterior lumbar fusion.
Acknowledgment
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number TL1TR000141. The content is solely the responsibility of the authors and does not necessarily represent official views of the National Institutes of Health.
The Manuscript submitted does not contain information about medical device(s)/drug(s). National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number TL1TR000141 funds were received to support this work. Relevant financial activities outside the submitted work: grant, consultancy and expert testimony.
Contributor Information
Bryce A. Basques, Yale School of Medicine
Michael C. Fu, Yale School of Medicine
Rafael A. Buerba, Yale School of Medicine
Daniel D. Bohl, Yale School of Medicine
Nicholas S. Golinvaux, Yale School of Medicine
Jonathan N. Grauer, Yale School of Medicine
References
- 1.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. The New England journal of medicine. 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA : the journal of the American Medical Association. 2010;303:1259–65. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goz V, Weinreb JH, McCarthy I, et al. Perioperative Complications and Mortality After Spinal Fusions: Analysis of Trends and Risk Factors. Spine. 2013 doi: 10.1097/BRS.0b013e3182a62527. [DOI] [PubMed] [Google Scholar]
- 4.Epstein NE, Schwall G, Reillly T, et al. Surgeon choices, and the choice of surgeons, affect total hospital charges for single-level anterior cervical surgery. Spine. 2011;36:905–9. doi: 10.1097/BRS.0b013e3181e6c4d8. [DOI] [PubMed] [Google Scholar]
- 5.Browne JA, Cook C, Pietrobon R, et al. Diabetes and early postoperative outcomes following lumbar fusion. Spine. 2007;32:2214–9. doi: 10.1097/BRS.0b013e31814b1bc0. [DOI] [PubMed] [Google Scholar]
- 6.Gephart MG, Zygourakis CC, Arrigo RT, et al. Venous thromboembolism after thoracic/thoracolumbar spinal fusion. World neurosurgery. 2012;78:545–52. doi: 10.1016/j.wneu.2011.12.089. [DOI] [PubMed] [Google Scholar]
- 7.Fineberg SJ, Nandyala SV, Marquez-Lara A, et al. Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine. 2013;38:1790–6. doi: 10.1097/BRS.0b013e3182a0d507. [DOI] [PubMed] [Google Scholar]
- 8.Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine. 2012;37:982–8. doi: 10.1097/BRS.0b013e31823bbeef. [DOI] [PubMed] [Google Scholar]
- 9.Memtsoudis SG, Kirksey M, Ma Y, et al. Metabolic syndrome and lumbar spine fusion surgery: epidemiology and perioperative outcomes. Spine. 2012;37:989–95. doi: 10.1097/BRS.0b013e31823a3a13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lad SP, Bagley JH, Kenney KT, et al. Racial disparities in outcomes of spinal surgery for lumbar stenosis. Spine. 2013;38:927–35. doi: 10.1097/BRS.0b013e31828165f9. [DOI] [PubMed] [Google Scholar]
- 11.Lee KH, Yue WM, Yeo W, et al. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012;21:2265–70. doi: 10.1007/s00586-012-2281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nie H, Hao J, Peng C, et al. Clinical outcomes of discectomy in octogenarian patients with lumbar disc herniation. Journal of spinal disorders & techniques. 2013;26:74–8. doi: 10.1097/BSD.0b013e318236b92d. [DOI] [PubMed] [Google Scholar]
- 13.Sami Walid M, Zaytseva NV. The impact of chronic obstructive pulmonary disease and obesity on length of stay and cost of spine surgery. Indian journal of orthopaedics. 2010;44:424–7. doi: 10.4103/0019-5413.67120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walid MS, Zaytseva NV. Prevalence of mood-altering and opioid medication use among spine surgery candidates and relationship with hospital cost. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2010;17:597–600. doi: 10.1016/j.jocn.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 15.Walid MS, Robinson EC, Robinson JS., Jr. Higher comorbidity rates in unemployed patients may significantly impact the cost of spine surgery. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2011;18:640–4. doi: 10.1016/j.jocn.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 16.Siemionow K, Cywinski J, Kusza K, et al. Intraoperative fluid therapy and pulmonary complications. Orthopedics. 2012;35:e184–91. doi: 10.3928/01477447-20120123-06. [DOI] [PubMed] [Google Scholar]
- 17.Zheng F, Cammisa FP, Jr., Sandhu HS, et al. Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine. 2002;27:818–24. doi: 10.1097/00007632-200204150-00008. [DOI] [PubMed] [Google Scholar]
- 18.Siemionow K, Pelton MA, Hoskins JA, et al. Predictive factors of hospital stay in patients undergoing minimally invasive transforaminal lumbar interbody fusion and instrumentation. Spine. 2012;37:2046–54. doi: 10.1097/BRS.0b013e31825c6688. [DOI] [PubMed] [Google Scholar]
- 19.Fink AS, Campbell DA, Jr., Mentzer RM, Jr., et al. The National Surgical Quality Improvement Program in non-veterans administration hospitals: initial demonstration of feasibility. Annals of surgery. 2002;236:344–53. doi: 10.1097/00000658-200209000-00011. discussion 53-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khuri SF, Henderson WG, Daley J, et al. Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the private sector: the Patient Safety in Surgery study. Annals of surgery. 2008;248:329–36. doi: 10.1097/SLA.0b013e3181823485. [DOI] [PubMed] [Google Scholar]
- 21.Daabiss M. American Society of Anaesthesiologists physical status classification. Indian journal of anaesthesia. 2011;55:111–5. doi: 10.4103/0019-5049.79879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ridgeway S, Wilson J, Charlet A, et al. Infection of the surgical site after arthroplasty of the hip. The Journal of bone and joint surgery. British volume. 2005;87:844–50. doi: 10.1302/0301-620X.87B6.15121. [DOI] [PubMed] [Google Scholar]
- 23.Grosflam JM, Wright EA, Cleary PD, et al. Predictors of blood loss during total hip replacement surgery. Arthritis care and research : the official journal of the Arthritis Health Professions Association. 1995;8:167–73. doi: 10.1002/art.1790080309. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.