Abstract
Objective
This study’s primary aim was to examine whether the positive self-perceptual bias present in many youth with ADHD (Hoza et al., 2004; Hoza, Pelham, Dobbs, Owens, & Pillow, 2002) mediates the relation of childhood ADHD status to later risky behaviors.
Method
Using a subset of children with ADHD and comparison children (n = 645) from the Multimodal Treatment Study of Children with ADHD, we predicted that a positive bias in childhood would partially or fully mediate the relation between having ADHD and risky driving and sexual behaviors eight years later.
Results
Results strongly supported this hypothesis for risky driving behavior, but only provided limited support for risky sexual behavior.
Conclusions
Taken together, findings suggest that future research should explore whether self-perceptual bias may be a useful target of intervention for children with ADHD.
Keywords: ADHD, risky behavior, positive bias, self-perception, risky driving, risky sex
Increasingly, it is recognized that attention-deficit/hyperactivity disorder (ADHD) persists into adulthood for many of those afflicted (Barkley, Murphy, DuPaul, & Bush, 2002). Although the symptom manifestations may change as children age with motor hyperactivity declining and feelings of restlessness increasing (American Psychiatric Association, 1994), some impairment of functioning across life domains generally persists. The types of impairment may shift, however, with the new developmental challenges of adolescence and young adulthood. Although children with ADHD as a group are at increased risk for a variety of negative outcomes relative to typically developing peers (Evans & Hoza, 2011), there is a great deal of heterogeneity in individual outcomes. This heterogeneity requires more research into explanatory mechanisms.
Over the past decade, research has documented the presence of positively biased self-perceptions of competence in many children with ADHD (e.g., Hoza et al., 2004; Hoza et al., 2002), suggesting diminished insight in many children with this disorder. Available data suggest that roughly 30 to 57 percent of children with ADHD display bias scores one standard deviation or more above the sample mean, with estimates varying depending on competence domain assessed (Hoza & Pelham, 1995; Linnea, Hoza, Tomb, & Kaiser, 2012). Importantly, children with ADHD display the greatest levels of positive bias (PB) in areas of greatest impairment (Hoza et al., 2004; Hoza et al., 2002), suggesting that these children either cannot or will not acknowledge their areas of relative incompetence. Recent work addressing this question of incapacity versus self-protection or willful denial has found evidence partially supporting both perspectives (Hoza, Vaughn, Waschbusch, Murray-Close, & McCabe, 2012). In other words, cognitive deficits (McQuade, Tomb, et al., 2011) and self-protection (Diener & Milich, 1997; Hoza et al., 2010; Ohan & Johnston, 2002) may both be contributory factors. These and other potential mechanisms underlying the positive bias are discussed in detail elsewhere (for a review, see Owens, Goldfine, Evangelista, Hoza, & Kaiser, 2007), but like ADHD itself, no single underlying mechanism fully explains the phenomenon.
Even in the absence of a comprehensive understanding of positive bias, recent work demonstrates usefulness of the construct in predicting reduced behavioral treatment responsiveness (Kaiser, Hoza, Pelham, Gnagy, & Greiner, 2008; Mikami, Calhoun, & Abikoff, 2010). Specifically, high levels of positive bias at the beginning of a summer treatment program (STP) predicted worse response to behavioral treatment as manifested in increased conduct problems and decreased peer social preference, even in a predominantly medicated sample (Mikami et al., 2010). Similarly, and also in a STP setting, positive bias statistically mediated the relation between ADHD status and rates of swearing, verbal abuse to staff, intentional aggression to peers and staff, and interrupting others (Kaiser et al., 2008). Taken together, these findings suggest that positive bias is both associated with reduced behavioral treatment responsiveness and a potential mechanism worthy of additional investigation.
It is not entirely clear how children with ADHD who display a positive bias may be disadvantaged. Perhaps they are more likely to use maladaptive strategies beyond the point where such strategies have proven ineffective, and/or are less able or motivated to learn new ones. Indeed, Barkley (1997) argued that certain executive functioning deficits may prevent children with ADHD from being able to carry forward information on past behavior in order to govern future behavior. More recent work emphasizing the heterogeneity of the disorder and hence multiple-deficit models of ADHD (for reviews, see Nigg, 2005; Swanson, Baler & Volkow, 2011), suggests that “disruption of a multicomponent self-regulatory system” (Nigg, 2005, p. 1424) better explains ADHD. Given the heterogeneity of ADHD, it seems probable that children with ADHD who display a positive bias may be substantially different in some way from those without such a bias, and these differences may relate in meaningful ways to important outcome variables.
One area of executive functioning impairment for individuals with ADHD discussed in recent reviews is “flexible strategic response” (Jerome et al., 2006, p. 423). Indeed, the inability of children with ADHD (relative to controls) to respond appropriately to social task demands signaling a need for change in strategy has been documented in several earlier laboratory studies. Regardless of laboratory paradigm, children with ADHD tend to continue with an established response strategy even in the face of evidence (or direct feedback) indicating that a change is needed. For example, children with ADHD, relative to controls, have considerable difficulty utilizing feedback from peers needed to improve performance on a space flight game (Whalen, Henker, Collins, McAuliffe, & Vaux, 1979). Similarly, in a TV talk show task, boys with ADHD displayed “an insensitivity to changing situational demands” (p. 79; Landau & Milich, 1988). If early positive bias in childhood signals an exaggerated form of cognitive inflexibility, it may be considered a risk factor for impairment in areas of later life functioning that require careful forethought, incorporation of feedback from the environment, contemplation of risks and benefits, and well-formulated response strategies.
There are many life circumstances requiring the critical skills of forethought (specifically, contemplation of risks and benefits), and responsiveness to cues from the environment and from others. In the teenage years, however, situations that have high potential for health-endangering outcomes become especially salient. In particular, behaviors that are legal and widely accessible for teens may be particularly problematic if mismanaged with limited skill or insight. Two classes of behaviors that become particularly salient for adolescents with ADHD histories are driving behaviors and sexual practices. A growing body of literature now documents that adolescents with ADHD employ riskier driving practices (for a meta-analytic review see Jerome et al., 2006) as reflected in more license revocations and suspensions, more instances of driving without a license, more repeated driving citations (especially speeding), and involvement in more accidents as a driver compared to youth without ADHD (Barkley, Guevremont, Anastopoulos, DuPaul, & Shelton, 1993; Barkley et al., 2002). In addition, when involved in accidents, youth with ADHD, as compared to controls, are more often at fault, and are involved in more serious accidents as reflected by cost of damages (Barkley et al., 2002). Importantly, these results are found even when considering driving behaviors of adolescents/young adults who were diagnosed with ADHD as children and followed forward into adolescence or young adulthood. For example, one study (Thompson, Molina, Pelham, & Gnagy, 2007) compared adolescent/young adult driving behavior of individuals who were and were not diagnosed with ADHD as children. Considering only those who were active drivers in the past 6 months, and controlling for both age and driving frequency, those with a childhood diagnosis of ADHD self-reported more accidents in the past 6 months, and received more tickets both in the past 6 months and also in their lifetimes, as compared to those without a childhood ADHD diagnosis (Thompson et al., 2007).
Similarly, the limited work investigating sexual practices in those with ADHD suggests that childhood ADHD may be related to later risky sexual behavior. One study of a large sample of boys with ADHD and comparison youth followed prospectively into early adulthood indicated that a childhood ADHD diagnosis predicts earlier onset of sexual activity and intercourse, a greater number of sexual partners, more sex with newly acquainted peers, more casual sex without condom use, and greater frequency of partner pregnancies (Flory, Molina, Pelham, Gnagy, & Smith, 2006). Moreover, a 10-year prospective study of 18 boys with ADHD and 18 comparison boys reported that a higher proportion of participants with ADHD (28% vs. 0%) had fathered children by early adulthood (i.e., average age of 21 years; Hansen, Weiss, & Last, 1999). In addition, findings from a national sample indicated that lower levels of self-regulation (e.g., acting impulsively, struggling to concentrate) in early adolescence predicted engagement in risky sex behaviors during late adolescence (Raffaelli & Crockett, 2003).
Regarding the possible role of conduct problems in this association, findings are mixed. Recent work (Flory et al., 2006) indicates that young men who had ADHD in childhood report certain risky sexual behaviors to a greater extent than controls even in the absence of oppositional defiant or conduct disorder. In contrast, one prospective 5-year follow-up study of girls with and without ADHD reported that conduct disorder, but not ADHD, was associated with being sexually active, having intercourse before age 16, having lifetime history of multiple sexual partners (three or more), or becoming pregnant (Monuteaux, Faraone, Gross, & Biederman, 2007). Given these mixed results, it is difficult to describe the exact relation between risky sexual behavior and ADHD vis-à-vis conduct disorder. Accordingly it seems prudent to consider conduct problems in the context of studying risky sexual behaviors in ADHD; hence, we do so in the present study by controlling for conduct problems in all models.
Any compelling demonstration that early-detected positive bias (i.e., in childhood) predicts or explains later risky behavior, however, must do so beyond the risk of having childhood ADHD. Demonstrating this relation is important for two reasons. First, even in the absence of a positive bias, problems with inattention or hyperactivity/impulsivity might contribute to risky driving or sexual behavior. For example, inattention might cause less focus while driving, whereas hyperactivity or impulsivity may relate to unsafe decision-making both behind the wheel (Thompson et al., 2007) and in regard to sexual activity (Flory et al., 2006). Therefore, any meaningful relation of positive bias to risky outcomes must confer risk beyond that which is already present simply by virtue of having ADHD. Second, if positive bias detected in childhood can be shown not only to predict, but also to mediate, the relation between ADHD status and risky behavior, it may also be a suitable target for intervention with possibilities of altering the trajectory toward risky outcomes.
In light of the literature just reviewed, the goal of the present study was to consider whether the positive self-perceptual bias, present at an early age in many youth with ADHD (Hoza et al., 2004; Hoza et al., 2002), mediates the relation of childhood ADHD status to later risky behaviors–specifically, risky driving and sexual behaviors in adolescence and young adulthood. We predicted that a positive bias, identified in childhood, would partially or fully mediate the relation between having ADHD in childhood, and later risky driving and sexual behaviors eight years later. In the absence of prior literature to guide our research, we took a broad approach, using measures of positive bias from the academic, social, and behavioral domains, to predict a range of indicators of risky behavior. These specific domains were chosen in light of past research showing them to be the ones with the largest effect sizes for positive biases observed in youth with ADHD (Hoza et al., 2004; Hoza et al., 2002).
Method
Participants
Institutional review board evaluation and approval occurred at each site prior to the start of the original Multimodal Treatment Study of Children with ADHD (MTA) study. A subset of 645 participants from the MTA were included in this study. Originally, the MTA was a randomized 14-month clinical trial of ADHD treatments (n = 579). Children with ADHD were recruited through schools, primary medical care facilities, mental health offices, advertisements, parent self-help groups, and word of mouth. At entry into the MTA study, children with ADHD met full diagnostic criteria for ADHD, Combined type, based on a comprehensive evaluation of ADHD that included parent and teacher ratings of symptoms and behavior and a structured diagnostic interview (see Hinshaw et al., 1997, for a comprehensive description of assessment procedures).
Ten months after the completion of the treatment phase of the study and 24 months from baseline, a local normative comparison group (LNCG, n = 289) was recruited to compare outcomes of participants with ADHD to a normative sample of children. In order to make the LNCG sample and the ADHD sample comparable, LNCG participants were recruited from the same grades and schools as the ADHD sample and were of similar age and demographic characteristics. Both the LNCG and ADHD groups had the same screening and inclusion/exclusion criteria (e.g., English-speaking; IQ) except that the LNCG group was not required to meet ADHD categorical or dimensional criteria. As in prior reports (Molina et al., 2009), LNCG children who met diagnostic criteria for ADHD were excluded from the analyses (N=31).
Data for this study were taken from questionnaires completed at the 24-month time point, when participants were 8.2 to 13.9 years-old (M=10.4, SD=.9), and at the 10-year follow-up, when participants were 16.2 to 21.9 years-old (M=18.4, SD=.9). Although participants with ADHD received one of four randomly assigned treatments prior to the 24-month time point, relative differences in treatment groups were no longer discernible by 36-months (Jensen et al., 2007). For the present study, the 24-month and 10-year time points are referred to as Times 1 and 2, respectively. The sample for the current study (N=645), consisted of 412 participants in the ADHD group and 233 participants from the LNCG who provided both Time 1 and Time 2 data. Participants were predominantly male (79%) and racially and ethnically diverse (i.e., 65% Caucasian, 16% African-American, 9% Hispanic or Latino, 7% mixed race, 2% Asian, and 1% other races). At Time 1, participant’s families had a large range of income levels (Range= less than $10,000 to over $75,000, Mean range= $40,000 to $50,000) and 15% received welfare assistance. Five percent of participants had mothers who completed some high school or less, 19% graduated from high school or completed their general education degree, 32% completed some college, 26% were college graduates, and 18% completed an advanced graduate or professional degree. Of the participants who completed the questionnaire regarding risky sexual behavior, 70% reported that they had chosen to be sexually active and of those sexually active, 95% reported sexual intercourse with opposite sex partners only, 0% with same sex partners only, and 5% with both opposite and same sex partners. Compared to the sample for the current study, participants without relevant measures at Time 2 (N=192), were more likely to be from the ADHD group, be male, identify as non-Caucasian, have lower parent income, and have mothers with a lower level of education (all ps < .05).
Predictors of Risky Behavior
Positive bias
Children’s level of positive bias was assessed at Time 1 using the teacher and child versions of the Self-Perception Profile for Children (SPPC; Harter, 1985). The child report version of the SPPC includes six subscales assessing global self-worth and domain-specific self-perceptions of academic competence, social acceptance, athletic competence, physical appearance, and behavioral conduct. Each subscale is assessed with six items, rated on a one to four scale, with higher scores indicating more positive self-perceived competence; items for each subscale were averaged to create subscale scores. The teacher version of the SPPC is a parallel form but only includes the five domain-specific subscales, each assessed with three items. In the present study, positive bias in the academic, social, and behavioral conduct domains was examined given that these are some of the most common areas of impairment for children with ADHD (Hoza, Owens, & Pelham, 1999). Reliability of the SPPC subscales is well-documented with Cronbach’s alphas ranging from 0.71 to 0.86 (Harter, 1985). In the present sample the alphas ranged from .75 to .78 for subscales on the child report version and .89 to .95 for subscales on the teacher report version. As in prior research (Hoza et al., 2002; Hoza et al., 2004), to calculate bias in each of the three domains, a discrepancy score was computed by subtracting the teacher’s rating of the child’s competence from the child’s self-perception score. Given the domain-specific nature of self-perceptions of competence (Harter, 1985), separate discrepancy scores were calculated for each of the three domains. The discrepancy scores reflected the extent to which the children’s perceptions of competence differed from their teachers’ assessments of their competence (Harter, 1985). Scores greater than zero indicated an overestimation of competence (i.e., a positive bias) and scores less than zero indicated an underestimation of competence (i.e., a negative bias).
Estimated IQ
An estimation of children’s general intellectual functioning was included as a covariate in predicting risky behaviors. Estimated IQ was based on a full or partial administration of the WISC-III. For the ADHD group, a full administration of the WISC-III was completed 24 months prior to Time 1 as part of the baseline MTA screening. A Full Scale IQ score based on age norms was derived. For participants in the LNCG group, the Similarities, Block Design, Vocabulary, and Object Assembly subtests of the WISC-III were administered when they were initially recruited at Time 1 and an estimated IQ score was derived based on Sattler’s (2001) scoring.
Conduct Disorder Symptoms
Conduct disorder symptoms at Time 1 were included as a covariate in all analyses and were based on maternal report on the DSM-IV Conduct Disorder Checklist (Hinshaw et al., 1997), which includes 15 items assessing the frequency of DSM-IV Conduct Disorder (CD) behavior on a scale of one (never) to four (often). Items were summed to yield a total conduct problems score, which in the current sample, had a coefficient alpha of .76. This measure has been used as a parent-report measure of conduct disorder symptoms in the MTA study (Hoza et al., 2004; Molina et al., 2009), and when combined with additional aggression items, has been used in MTA reports as a measure of general aggression (e.g., see Hoza et al., 2010; McQuade et al., 2012; Murray-Close et al., 2010).
Risky Driving Behavior
Risky driving at Time 2 (10-year follow-up) was assessed with self- and parent-report from the Driving Behavior Questionnaire (DBQ), developed for the MTA as an adaptation of measures previously used to study driving behavior among non-referred (Donovan, Marlatt, & Salzberg, 1983; Jessor, Donovan, & Costa, 1991) adolescents and young adults and those with ADHD (Barkley et al., 1993; Barkley et al., 2002). The DBQ includes initial questions about whether or not the adolescent currently has, or ever had, a driver’s license or permit. In addition, the DBQ includes initial yes/no questions regarding whether the adolescent has ever engaged in different risky driving behaviors and follow-up questions regarding the frequency of those behaviors. For each variable, adolescent and parent reports were collected. For each participant, the report that indicated the greatest frequency of risky behavior was used in the current analyses.
Frequency of driving illegally
The frequency of driving illegally was assessed in all participants, regardless of whether they had ever had a license or permit. Driving illegally was defined as “driving while below legal age, driving without a learner’s permit or license, driving with a suspended license, driving while in violation of the learner’s permit rules, and driving without legally-required insurance.” Raters were asked to report the number of times the participant had ever driven illegally. Because of the extreme skew of responses, the number of times the participant drove illegally was transformed into an ordinal variable with five levels: never (64.9%), one to three times (14.1%), four to ten times (11.4%), eleven to fifty times (6.0%), or over fifty times (3.6%).
Frequency of traffic violations
The frequency of traffic violations for risky driving was assessed for participants who had ever had a driver’s license or permit or who reported ever driving illegally. Raters were asked to indicate the number of traffic violations received for speeding, failure to stop at a stop sign or signal light, failure to yield right of way, illegal turns, reckless driving, driving while intoxicated, and tailgating. Traffic violations for non-reckless behaviors (e.g., illegal parking or expired registration) were not included. A sum of the number of traffic violations was computed and due to the positive skew of responses, the number of tickets was transformed into an ordinal variable with four levels: none (74.3%), one (12.6%), two (7.1%), or three or more (5.9%).
License/Permit ever revoked/suspended
Participants’ history of license or permit revocation or suspension was assessed (number of times for those who ever had a license or permit). Responses were coded into a dichotomous variable (yes= 1, 8.4%; no = 0, 91.6%).
Risky Sexual Behavior
Participants’ risky sexual behavior at 10-year follow-up was assessed from adolescents’ self-report on the Health and Sexual Behavior Questionnaire (HSBQ). The measure was developed for the MTA, drawing upon previous measures for content (e.g., Health and Sex Behavior Questionnaire, Flory et al., 2006; Tarter, 1997; Jessor, Jessor, & Donovan, 1981; Pittsburgh Adolescent Alcohol Research Center, 1996). Like the DBQ, the HSBQ includes initial questions regarding whether the participant has ever been sexually active as well as questions about sexual history, the frequency of sexual behaviors, and other health problems. In gathering these sensitive data, we used the same protections (certificate of confidentiality) that are widely used in the literature to gather sensitive data. In terms of validity, prior research demonstrates that this measure relates to expected constructs (Flory et al., 2006). In the present study, analyses considered whether PB related to 1) whether or not the participant had ever been sexually active and 2) risky sexual behavior (number of partners, condom use, age at first intercourse) among sexually active participants.
Ever had sex
Participants were asked if they “ever chose to be sexually active.” Responses were coded a 1 if the participant indicated “yes” and coded a 0 if they indicated “no”; 69.7% reported that they had been sexually active and 30.3% reported that they had never been sexually active.
Number of Lifetime Partners
Participants who indicated they were sexually active were asked to indicate the “number of partners that you have chosen to have sexual intercourse with”. Due to the skew of the responses, number of partners reported was transformed into an ordinal variable with six levels: one (22.6%), two partners (18.9%), three to five partners (27.3%), six to nine partners (14.8%), ten to fifteen partners (10.8%), and sixteen or more partners (5.7%).
Failure to use condoms
Participants who reported being sexually active were asked about their frequency of using condoms during sexual intercourse. Given that even occasional failure to use condoms may have serious health risks, participant responses were coded 0 if they reported “always” using condoms (48.8%) and 1 if they reported using condoms “most of the time,” “some of the time,” or “never” (51.2%).
Age at first sexual intercourse
Participants who reported being sexually active were asked to report the age when they first chose to have sexual intercourse; because of the nature of the original question on the survey, responses below 11 years-old were truncated to 11 years-old and responses older than 18 years-old were truncated to 18 years-old. For participants who reported being sexually active, 3.7% were 11 years or younger, 2.3% were 12 years-old, 8.0% were 13 years-old, 8.0% were 14 years-old, 17.0% were 15 years-old, 21.0% were 16 years-old, 22.3% were 17 years-old, and 17.7% were 18 years-old or older when they first chose to have sexual intercourse.
Results
Data Analytic Approach
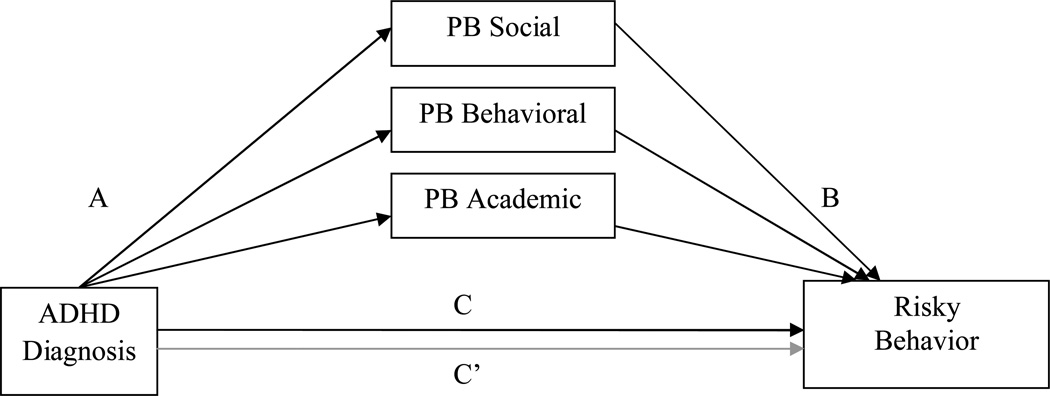
A path analytic approach allowing the simultaneous testing of multiple mediators was used to test our hypotheses in MPlus version 6 (Múthen & Múthen, 2010). Figure 1 illustrates the generic form of the model in which childhood ADHD was presumed to affect PB; PB in turn was presumed to affect risky behavior. Models were tested separately for the driving and sexual behavior outcome variables. Given that the three PB domains (social, behavioral, and academic) were only moderately correlated (see Table 1), they were simultaneously tested in each model to allow examination of their unique associations with the risky behavior variables. Specifically, the three PB scores were regressed on ADHD diagnosis (Path A), risky behavior was regressed on the three PB scores (Path B), risky behavior was regressed on ADHD diagnosis (Path C), and risky behavior was regressed on ADHD diagnosis while controlling for the three PB scores (Path C’). In each model, the effects of childhood estimated IQ and maternal-rated conduct symptoms were considered using MIMIC (MIMIC; Muthén, 1989),1 which estimates the effect of each covariate on all other variables in the model. Inclusion of conduct symptoms as a covariate assisted in controlling for severity of problem behavior, which may not have been fully captured by the dichotomous ADHD status variable. Participants’ age at Time 2 was also included as a covariate using MIMIC because older participants may have had greater opportunity to engage in risky behavior. Bias corrected estimates of the total indirect effect and the specific indirect effects for each of the PB domains were examined and significance levels were interpreted based on confidence intervals (CI). Dependent variables were treated as ordinal in MPlus. Accordingly, R2 values reported are calculated using the McKelvey and Zavoina (1975) technique and can be interpreted as an estimation of variance in the outcome variable that is explained by the model (McKelvey & Zavoina, 1975). Tables 1 through 3 display the correlations among variables.
Figure 1.
Hypothesized Model
Table 1.
Descriptive statistics and Pearson correlation coefficients among independent variables and covariates
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
|---|---|---|---|---|---|---|---|---|
| 1. Social PB |
M = .48 SD = 1.04 |
- | .43*** n = 563 |
.38*** n = 563 |
.32*** n = 563 |
.−.10* n = 557 |
.11* n = 563 |
.11* n = 538 |
| 2. Behavioral PB |
M = .42 SD = 1.05 |
- | .41*** n = 566 |
.29*** n = 566 |
−.15** n = 560 |
.02 n = 566 |
.23*** n = 541 |
|
| 3. Academic PB |
M = .36 SD = 0.92 |
- | .23*** n = 568 |
−.29*** n = 562 |
.02 n = 568 |
.07 n = 543 |
||
| 4. ADHD | ADHD = 1 LNCG = 0 |
- | −.23*** n = 638 |
.03 n = 645 |
.31*** n = 614 |
|||
| 5. Estimated IQ |
M = 104.8 SD = 16.4 |
- | .03 n = 638 |
−.13** n = 607 |
||||
| 6. Age at Time 2 |
M = 18.4 SD = 0.9 |
- | .06 n = 614 |
|||||
| 7. Conduct Symptoms |
M = 16.8 SD = 2.8 |
- | ||||||
Note: ADHD = Attention-Deficit/ Hyperactivity Disorder; M=mean, SD= standard deviation;
p<.05,
p<.01,
p<.001.
Table 3.
Pearson correlation coefficients between risky behavior variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Drive Illegally | - | .21*** | .03 | .13** | .25*** | .00 | −.19** |
| 2. License/Permit Revoked/Suspend | - | .23*** | .18** | .13 | .04 | −.08 | |
| 3. Tickets | - | .13** | .11 | −.07 | .05 | ||
| 4. Ever Had Sex | - | N/A | N/A | N/A | |||
| 5. Lifetime Partners | - | −.08 | −.61*** | ||||
| 6. Condoms Use Failure | - | .03 | |||||
| 7. Age at First intercourse | - |
Note: ADHD = License/Permit Revoked/Suspend (0=never; 1= yes); Ever had sex (0 = no; 1 = yes); Condom Use Failure (0=always uses; 1=fails to always use); N/A = not applicable; Risky behaviors are ordinal variables;
p<.05,
p<.01,
p<.001.
Missing Data
Missing data on independent variables were accounted for using Mplus maximum likelihood estimation techniques. Participants without relevant data at Time 2, compared to those included, had significantly greater PB in the behavioral conduct domain (M= .76, SD = 1.11 versus M=.42, SD = 1.05) and significantly lower estimated IQ (M=99.8, SD = 16.5 versus M=104.8, SD =16.4) but did not differ in regards to social and academic PB, age, or conduct disorder symptoms. Only participants with the opportunity to engage in the risky behavior were included in each model. For example, only sexually active participants were included in analyses of risky sexual behavior (condom use, number of partners, and age at first intercourse). Because we could not assume that participants with missing data at Time 2 had the opportunity to engage in the risky behavior, only subjects with data regarding risky behaviors were included.
Does PB mediate the relation between childhood ADHD and risky driving behavior in young adulthood?
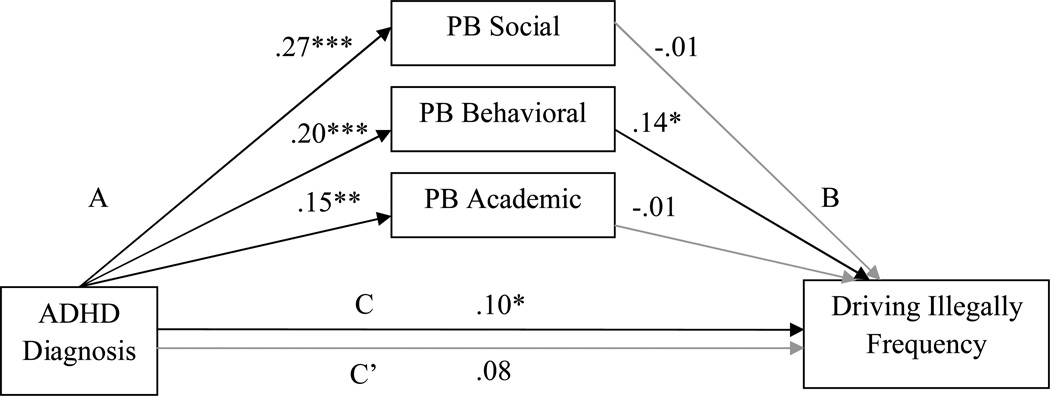
Driving illegally frequency
The first path model examined the direct and indirect (through PB) effects of ADHD diagnosis on the frequency of driving illegally (see Figure 2; R2 for complete model = 3.4%). All participants who completed the DBQ, regardless of whether they had ever had their license, were included (N=604). When the PB variables were not included in the model, ADHD diagnosis was significantly positively related to frequency of driving illegally. When PB was included in the model, ADHD diagnosis was not associated with illegal driving frequency. However, ADHD diagnosis was significantly positively related to PB in each of the three domains and greater PB in the behavioral conduct domain was significantly positively associated with frequency of driving illegally. Childhood estimated IQ, age at Time 2, and maternal-rated conduct symptoms were not significant predictors of illegal driving frequency (all ps > .05). The total indirect effect of the three PB scores was not significant (p >.05), nor were the specific indirect effects of social and academic PB, but the specific indirect effect of PB in the behavioral conduct domain was significant (p < .05; 95% CI .01–.12). Thus, childhood PB in the behavioral conduct domain fully mediated the relation between childhood ADHD diagnosis and a greater frequency of driving illegally in young adulthood.
Figure 2.
Path model predicting driving illegally frequency
Note. PB= positive bias; standardized coefficients are reported. The effect of ADHD on driving illegally frequency without PB included in the model is reported above the line (path C) and with PB included is reported below the line (path C’). Estimated childhood IQ, maternal-rated conduct disorder symptoms, and age at Time 2 were included as covariates; n=604; *p<.05, **p<.01, ***p<.001.
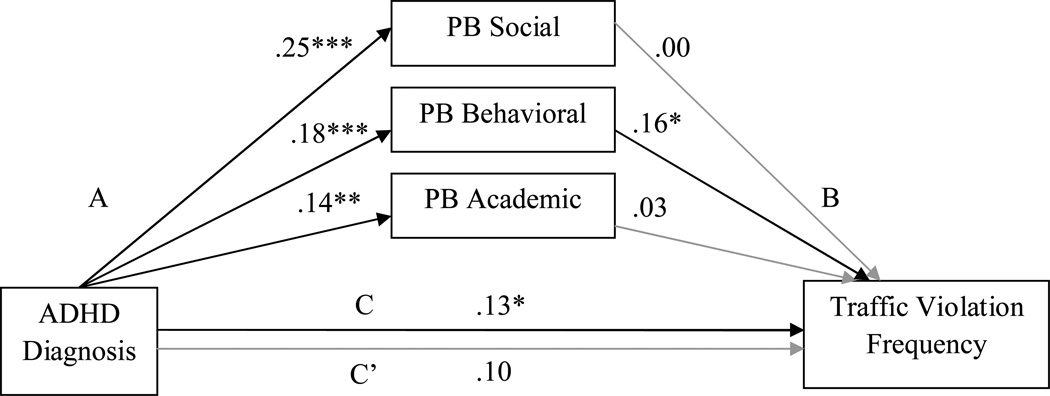
Traffic violation frequency
Figure 3 displays the path model examining the direct and indirect effects (through PB) of ADHD diagnosis on the frequency of traffic violations (R2 for complete model = 15.3%). Participants who had the opportunity to receive a traffic violation (those that had their license or permit or reported driving illegally) were included (N=510). ADHD diagnosis significantly predicted greater frequency of traffic violations when PB was not considered in the model but was not significant when PB was included. Again, ADHD diagnosis was significantly positively related to PB in each of the three domains and PB in the behavioral conduct domain predicted a greater frequency of traffic violations. Older age at Time 2 (p < .001), greater estimated IQ (<.05), and less maternal-rated conduct symptoms (p <.01) were also significantly associated with a greater frequency of traffic violations. The total indirect effect of PB across the three domains was not significant (p > .05). The specific indirect effect of PB in the behavioral conduct domain was significant (p < .01; 99% CI .001–.18); however, the specific indirect effects of PB in the social and academic domains were not significant (ps >.05). Thus, greater PB in the behavioral conduct domain fully mediated the relation between childhood ADHD diagnosis and greater frequency of traffic violations for risky driving in young adulthood.
Figure 3.
Path model predicting traffic violation frequency
Note. PB= positive bias; standardized coefficients are reported. The effect of ADHD on traffic violation frequency without PB included in the model is reported above the line (path C) and with PB included is reported below the line (path C’). Estimated childhood IQ, maternal-rated conduct disorder symptoms, and age at Time 2 were included as covariates; n=510; *p<.05, **p<.01, ***p<.001.
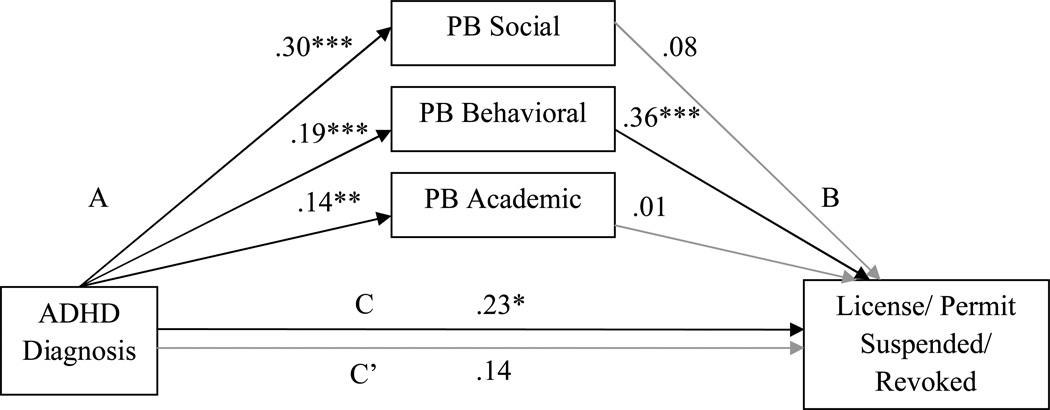
License/Permit ever revoked/suspended
Figure 4 presents the path model examining the direct and indirect effect (through PB) of ADHD diagnosis on having a license or permit revoked or suspended (R2 for complete model = 28.2%). This model included participants who reported ever having their license or permit (N=425). ADHD diagnosis predicted a greater likelihood of having a license/permit revoked/suspended when PB was not included in the model but was no longer a significant predictor when PB was added. ADHD diagnosis was significantly positively associated with PB in each domain and greater behavioral PB predicted a greater likelihood of having ones’ license/permit revoked/suspended. Childhood estimated IQ, age at Time 2, and maternal-rated conduct symptoms were not significant predictors of the likelihood of having ones’ permit/license revoked/suspended (ps > .05). The total indirect effect of PB in the three domains and the specific indirect effect of PB in the behavioral conduct domain were significant (p <.01; 99% CI .02–.39 and p<.01; 99% CI .03–.31, respectively); the specific indirect effects of PB in the social and academic domains were not significant (ps > .05). These results suggest that both the set of childhood PB variables and childhood PB in the behavioral conduct domain fully mediated the relation between childhood ADHD diagnosis and a greater likelihood of having ones’ license or permit revoked or suspended in young adulthood.
Figure 4.
Path model predicating the likelihood of having one’s license/permit suspended/revoked
Note. PB= positive bias; standardized coefficients are reported. The effect of ADHD on license/permit suspended/revoked (1= yes; 0 = no) without PB included in the model is reported above the line (path C) and with PB included is reported below the line (path C’). Estimated childhood IQ, maternal-rated conduct disorder symptoms, and age at Time 2 were included as covariates; n=425; *p<.05, **p<.01, ***p<.001.
Does PB mediate the relation between childhood ADHD and risky sexual behavior in young adulthood?
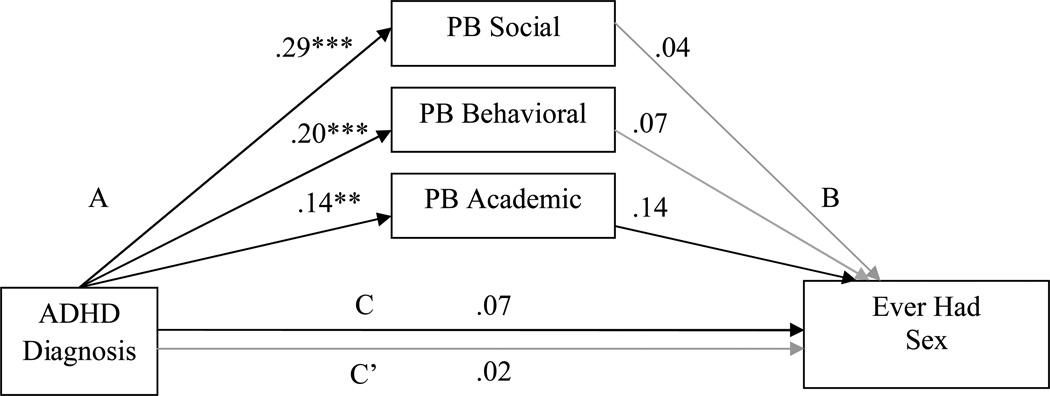
Ever chose to have sex
The path model examining the direct and indirect effect (through PB) of ADHD diagnosis on the choice to be sexually active is displayed in Figure 5 (R2 for complete model = 7.8%). Participants that completed this measure were included in the model (N=406). ADHD diagnosis was not significantly associated with choosing to have sex when considered independent of PB or when the PB scores were included in the model. However, ADHD diagnosis was significantly associated with greater PB in each domain. The PB domains were not significantly related to being sexually active. Older age at Time 2 also predicted a greater likelihood of being sexually active (p < .05,); maternal-rated conduct problems and estimated IQ were not significant predictors (ps > .05). Neither the total indirect effect nor the specific indirect effects were significant (all ps > .05).
Figure 5.
Path model predicting the choice to be sexually active
Note. PB= positive bias; standardized coefficients are reported. The effect of ADHD on ever had sex (1= yes; 0= no) without PB included in the model is reported above the line (path C) and with PB included is reported below the line (path C’). Estimated childhood IQ, maternal-rated conduct disorder symptoms, and age at Time 2 were included as covariates; n=406; *p<.05, **p<.01, ***p<.001.
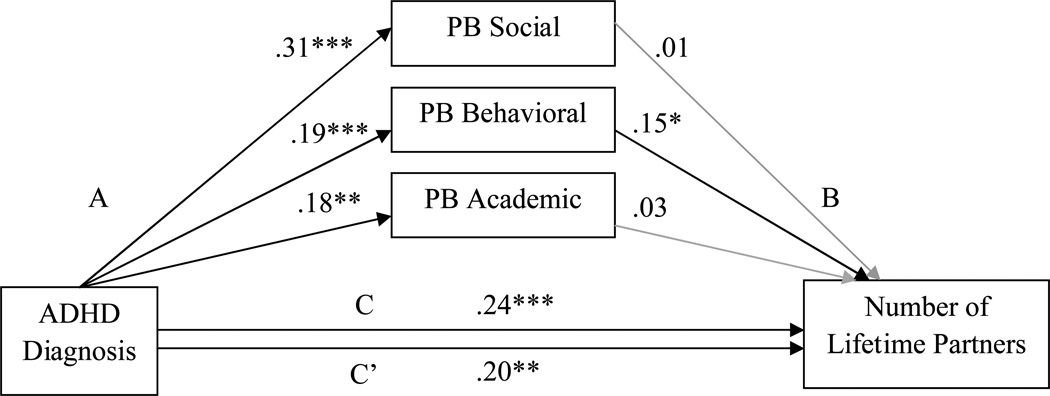
Number of lifetime sexual partners
Figure 6 displays the path model examining the direct and indirect effect (through PB) of ADHD diagnosis on the number of lifetime sexual partners (R2 for complete model = 16.5%). Participants that reported being sexually active were included (N=287). ADHD diagnosis significantly predicted a greater number of lifetime partners when PB was not in the model. When PB was included in the model, ADHD status still predicted more sexual partners and also predicted greater PB in the three domains. PB in the behavioral domain significantly predicted a greater number of sexual partners but PB in the social and academic domains did not predict number of sexual partners. Older age at Time 2 and greater maternal-rated conduct disorder symptoms both predicted a greater number of partners (both ps < .05); childhood estimated IQ was not a significant predictor (p >.05). The specific indirect effect of PB in the behavioral domain was significant (p < .05; 95% CI .01–.16). The total indirect effect and specific indirect effects of PB in the social and academic domains were not significant (p > .05). Thus results indicate that childhood PB in the behavioral conduct domain partially mediated the relation between childhood ADHD diagnosis and greater number of sexual partners in young adulthood.
Figure 6.
Path model predicting the number of lifetime sexual partners
Note. PB= positive bias; standardized coefficients are reported. The effect of ADHD on the number of lifetime partners without PB included in the model is reported above the line (path C) and with PB included is reported below the line (path C’). Estimated childhood IQ, maternal-rated conduct disorder symptoms, and age at Time 2 were included as covariates; n=287; *p<.05, **p<.01, ***p<.001.
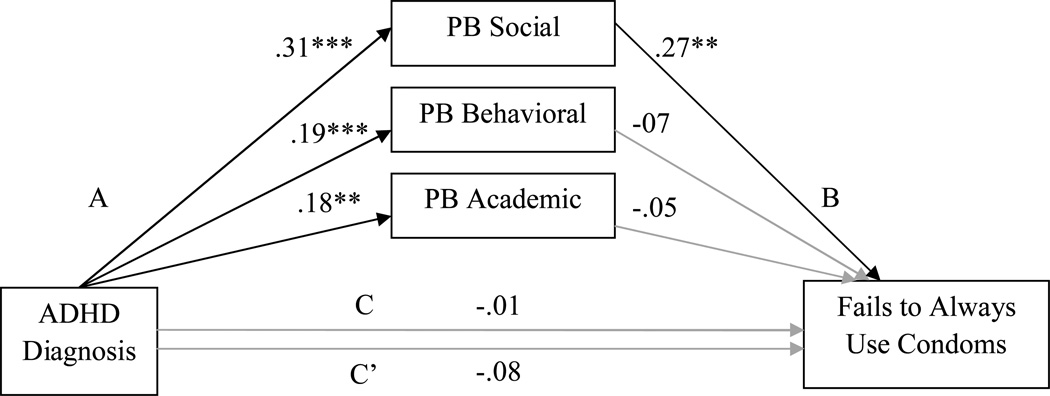
Failure to use condoms
Figure 7 presents the path model examining the direct and indirect effect (through PB) of ADHD diagnosis on use of condoms during sexual intercourse (R2 for complete model = 11.3%). Participants who reported being sexually active were included (N=287). ADHD diagnosis was not a significant predictor of condom use with or without PB included in the model. However, ADHD diagnosis was significantly positively associated with PB in each of the three domains and PB in the social domain was significantly associated with a greater likelihood of failing to always use condoms. Older age at Time 2, conduct symptoms and estimated IQ were not significant predictors (ps > .05). The total indirect effect of all three PB domains and the specific indirect effect of PB in the social domain were significant (p < .05; 95% CI .01–.31 and p < .01; 99% CI .03–.43, respectively); the specific indirect effects of PB in the academic and behavioral conduct domain were not significant (ps > .05). Thus, rather than a direct effect of childhood ADHD diagnosis on condom use, there is only an indirect effect such that childhood ADHD is associated with greater childhood PB in the social domain which, in turn, is associated with greater likelihood of failing to always use condoms during sexual intercourse. In addition, findings suggest that ADHD diagnosis may be indirectly related to a greater likelihood of failing to always use condoms during sexual intercourse through the presence of PB across the set of PB variables.
Figure 7.
Path model predicting condom use
Note. PB= positive bias; standardized coefficients are reported. The effect of ADHD on failure to always use condoms (fails to always use = 1 and always uses condoms = 0) without PB included in the model is reported above the line (path C) and with PB included is reported below the line (path C’). Estimated childhood IQ, maternal-rated conduct disorder symptoms, and age at Time 2 were included as covariates; n=287; *p<.05, **p<.01, ***p<.001.
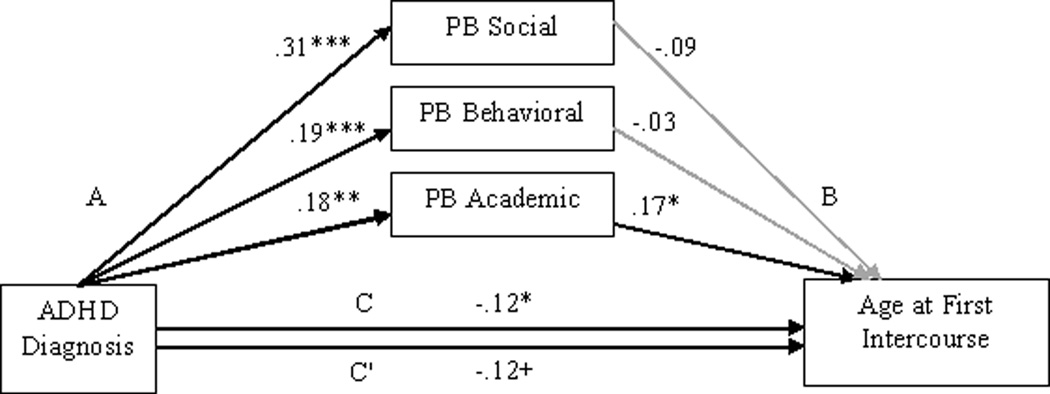
Age at first sexual intercourse
Figure 8 presents the paths examining the direct and indirect effects (through PB) of ADHD diagnosis on age at first intercourse (R2 for complete model = 18.5%). Participants who reported being sexually active were included (N=287). ADHD diagnosis significantly predicted an earlier age at first intercourse without PB included in the model but was only marginally significantly associated with earlier age at first intercourse when PB was included.2 ADHD diagnosis also was significantly related to greater PB in each domain and PB in the academic domain was a significant predictor of an earlier age at first intercourse; PB in the social and behavioral domains were not significant predictors. Greater maternal-rated conduct symptoms, lower IQ, and younger age at Time 2 also predicted a younger age at first intercourse (p < .01, p < .01, and p < .05, respectively). There was a significant specific indirect effect of ADHD diagnosis on age at first intercourse through academic PB (p < .05; 95% CI −.19–−.01); the total indirect effect and specific indirect effect for social and behavioral PB were not significant. Thus greater academic PB partially mediated the association between childhood ADHD status and an earlier age at first intercourse.3
Figure 8.
Path model predicting age at first intercourse
Note. PB= positive bias; standardized coefficients are reported. The effect of ADHD on age at first intercourse without PB included in the model is reported above the line (path C) and with PB included is reported below the line (path C’). Estimated childhood IQ, maternal-rated conduct disorder symptoms, and age at Time 2 were included as covariates; n=287; +p<.1, *p<.05, **p<.01, ***p<.001.
Discussion
This paper is the first to examine whether the positive self-perceptual bias present at an early age in many youth with ADHD (Hoza et al., 2004; Hoza et al., 2002) mediates the relation of childhood ADHD status to later risky behaviors. We predicted that a positive bias, identified in childhood, would partially or fully mediate the relation between having ADHD in childhood, and later risky driving and sexual behaviors eight years later. Results provide strong support for this hypothesis in regard to risky driving behavior, but very limited support relative to risky sexual behavior.
Risky Driving
Results were quite consistent across the three risky driving variables—frequency of driving illegally, frequency of driving tickets, and whether or not one’s license or permit had ever been suspended or revoked. In all three instances, although the direct effect of ADHD diagnosis on risky driving was significant, the relation became nonsignificant once the bias scores were included in the model, indicating full statistical mediation. Importantly, positive bias in the behavioral domain was the only specific indirect effect that accounted for this relation, suggesting that unrealistically positive views of one’s behavioral conduct in childhood mediates the relation between having childhood ADHD and risky driving 8 years later in adolescence or young adulthood.
It is interesting to consider why positive bias in the behavioral domain specifically might be important to later risky driving. This domain “taps the degree to which children like the way they behave, do the right thing, act the way they are supposed to, avoid getting into trouble, and do the things they are supposed to do” (Harter, 1985, p. 6). Inflation in this domain relative to a teacher criterion, therefore, might reflect a failure to acknowledge that one’s behavior is “out of line” and in need of change, a critical step in the feedback-to-behavior-change loop. Thus, positive bias in the behavioral domain may lead individuals to ignore important feedback that would otherwise suggest a need to change driving behavior (e.g., horn honks from other drivers, citations for reckless driving) and/or signal a generally inflexible response strategy on the road.
It is important to note that two prior studies have shown a link between behavioral positive bias in children with ADHD and behaviors indicative of rule-breaking behavior, although these prior studies have considered predictions only over very short time intervals and not in relation to driving violations. Specifically, Mikami and colleagues (2010) reported a positive association between behavioral positive bias and both baseline levels of, as well as worsening behavior over eight weeks, as reflected in a composite variable comprised of counts of noncompliance, verbal abuse to staff, stealing, teasing, lying, and aggression. Similarly, in a summer treatment program setting, Kaiser et al. (2008) reported that behavioral positive bias fully or partially mediated the association between ADHD status and 11 of 14 dependent variables including lying, swearing, verbally abusing staff, teasing, intentional aggression, rule violations, noncompliance, and interrupting others. It is remarkable that behavioral positive bias, assessed in the present study when children were, on average, 10.4 years old, similarly predicted frequencies of driving illegally and committing traffic violations, as well as having one’s permit or license revoked or suspended approximately 8 years later. Importantly, behavioral positive bias fully statistically accounted for (i.e., mediated) the relation between having ADHD and these outcomes, indicating its important role as a mediator variable. That unrealistic views of one’s behavioral competence early in childhood portends later frequency of illegal driving, frequency of driving citations, and having a permit/license suspended or revoked suggests possible continuity over time in the inability to perceive a need for change in one’s behavior or response strategies, although this was not tested directly. We know from prior work that, on average, the PB in the behavioral domain declines as children with ADHD progress into adolescence/young adulthood (Hoza et al., 2010). It may be that those most likely to engage in risky driving are those for whom PB remains stable over time, signaling a persistent pattern of inaccurate risk perception as well as inflexible response strategies similar to those previously associated with risky driving (Jerome et al., 2006). This possibility should be examined in future work.
Given the robust predictive relation of behavioral positive bias to later driving outcomes, even when other important variables (ADHD status, conduct problems, IQ, age) are considered simultaneously, it may be important to include measures of positive bias in standard ADHD assessments. Furthermore, given that symptoms of both ADHD and conduct problems were included in the models, effects for behavioral PB are not simply the result of behavioral incompetence. In fact, prior research by McQuade and colleagues (McQuade, Hoza, Waschbusch, Murray-Close, & Owens, 2011; McQuade, Tomb et al., 2011; McQuade, et al., 2012) has shown that the presence of PB in the academic, social, or behavioral conduct domain in children with ADHD is not merely a reflection of poorer teacher-ratings of competence as some have argued (Swanson, Owens, & Hinshaw, 2012) or greater internalizing or externalizing symptom severity.
Implications for intervention
It remains for future research to demonstrate, however, whether behavioral self-perceptual bias may itself be a useful target of intervention, and whether modifying this self-perceptual style will affect behavioral outcomes either concurrently or at a later time point. Recent work (Hoza et al., 2012) suggests that modifying this bias is indeed possible at least temporarily through laboratory manipulations, although it remains unclear whether this bias can be more permanently altered through intervention or completely eliminated. To our knowledge, few attempts to improve accuracy of self-evaluation in children with ADHD are represented in the published intervention literature. One involving a “match game” (Hinshaw, 2000) is largely descriptive, with data on effectiveness of the intervention not reported. Therefore, its utility is unknown. Another (Sadler, Evans, Schultz & Zoromski, 2011) compared behavior ratings of intervention staff and adolescent participants following social interactions with peers in a group setting. These ratings were used as the basis for discussion of how to utilize social feedback from others to modify future social behavior to meet “ideal self goals.” Although this intervention was extremely promising for the small minority who responded to it (33% met mastery criteria), the majority of participants had not met mastery criteria after ten sessions. Therefore, much remains to be learned regarding how to modify existing interventions, or develop new ones, to improve the ability of individuals with ADHD to utilize accurate self-evaluation towards the goal of improving subsequent behavior. Given the inverse relation between PB and depression (Hoza et al., 2004; Hoza et al., 2002), however, future interventions attempting to modify positive bias should carefully monitor depressive symptoms and appropriately treat this possible side effect.
Another possibility, however, is that positive bias is a significant mediator primarily due to its strong relation with other variables known or suspected to be important in accounting for the association between ADHD and risky driving (e.g., executive functioning deficits). If this is the case, PB may be most useful as a “marker variable” signaling a need to assess for and intervene at the level of these other variables. Addressing the PB may need to be the first step in setting the stage for individuals to accept other needed interventions, for example, those targeted at improving executive functioning deficits. Given that we controlled for IQ, a variable correlated with executive functioning (Mahone et al., 2002), this explanation is less of a concern. Nonetheless, this possibility should be considered in future work.
Risky Sexual Behavior
The findings regarding prediction of risky sexual behavior were less straightforward, but still informative. There was less evidence that positive bias mediated the relation between ADHD status and risky sexual behavior. In fact, there was no evidence of full mediation for any variable, and significant partial mediation was found only for number of sexual partners and age at first intercourse. When predicting number of sexual partners, behavioral positive bias was again the significant specific mediator, highlighting the importance of inflation in the behavioral domain as a possible explanatory variable. Interestingly, for age at first intercourse, it was academic PB that emerged as a significant specific mediator. The importance of the academic domain to the timing of first sexual intercourse may be a result of the fact that adolescents often learn about the reasons to delay sex during sex-education courses at school. In fact, abstinence is the most frequently covered topic in sex-education curricula (Lindberg, Santelli, & Singh, 2006). It is possible that having an academic PB may lead individuals to have greater difficulty judging whether they understand the information provided and subsequently using that information to inform their decisions. This may be one reason that children with ADHD are more likely to engage in sex at an earlier age.
In addition, there was some evidence of persistent direct effects of ADHD diagnosis on risky sexual behaviors (i.e., persisting even after the positive bias variables were added to the model), but only for number of lifetime sexual partners. These findings suggests that characteristics of childhood ADHD, such as impulsivity, even many years later, may directly contribute to having more sexual partners. Whether level of current symptoms in adolescence/adulthood may moderate this association is a useful avenue for future research.
Finally, although there was not a significant direct effect between ADHD status and failure to use condoms, a significant indirect effect of social bias on condom use was found. Specifically, having ADHD was related to having a positive bias in the social domain and having this positive bias was, in turn, related to less regular condom use. Perhaps individuals with a social positive bias worry less about the social ramifications of outcomes associated with lack of condom use (e.g., pregnancy, sexually-transmitted diseases), feeling already (falsely) quite secure in their social status. For individuals without a positive social bias, however, these social ramifications (e.g., that others will judge me, think less of me, reject me) might be a significant motivating factor for choosing to practice safe sex. Such a conclusion is consistent with research showing that undergraduate males with Combined Type ADHD show better social adjustment when they are high on rejection sensitivity (anxiety regarding social rejection), a finding opposite the pattern for comparison peers (Canu & Carlson, 2007).
That PB predicted risky driving more strongly than risky sexual behavior, although unexpected, is not inconsistent with literature examining risk-taking in non-ADHD youth. Specifically, Begg, Langley, and Williams (1999) failed to find common factors that predicted different types of crashes and injuries (including injuries not involving a motor vehicle) in a young adult sample. Although preliminary, our results also suggest that different types of risky behaviors may have unique predictors.
Strengths and Limitations
This study has a number of strengths and limitations. The longitudinal nature of these data better meets the requirements for testing mediation, and therefore may be considered a significant strength. In addition, the large sample size provides adequate power for testing the primary hypotheses, and the inclusion of covariates such as conduct disorder symptoms and IQ effectively rules out several viable alternative explanations of the findings. Finally, by identifying mediating factors between ADHD status and behaviors with potentially dire consequences (e.g., serious injury, sexually transmitted diseases, death), the current study provides an important foundation for essential intervention work that could mitigate risk for children with ADHD.
In terms of limitations, one limitation that may help explain the inconsistent and somewhat perplexing findings for the risky sex variables is that partner views and influences were not considered. Indeed, since risky sexual behavior, by definition, involves another individual, the lack of any data regarding partner views or influences is a significant omission. Additionally, although a strength of our study was the inclusion of both self- and parent-report of risky driving, additional measures such as official police or driving records from state agencies could have enhanced our risky driving measures. Due to limited resources, these measures were not collected. In terms of sample characteristics, although our sample was more than adequate for testing primary hypotheses, it was not sufficient for performing analyses by race/ethnicity. Similarly, although we generally did not find effects of gender (see footnote 1), it is possible that with more females included in the sample, significant differences may have been found. Our sample was exclusively Combined Type ADHD in childhood; therefore our results cannot be generalized to children diagnosed with other subtypes of the disorder, or to individuals meeting diagnostic criteria in adulthood. We also did not have data on medication status at the time of engagement in the driving and sexual behaviors; therefore, we cannot comment on how acute medication status may or may not have influenced these outcomes. Finally, because there was some selective attrition as a function of subject characteristics (e.g., ADHD status, sex, race, parental income and education, level of positive bias, IQ), it is not possible to determine from the present data how this may have biased our results.
Finally, many of the correlations were in a rather low range, and may have been statistically significant primarily due to the large sample size. Even a small effect, however, can be clinically important when stakes are high as they are with risky driving and sexual behavior; even a small reduction in serious injuries, fatalities, and life-threatening STDs can be important and meaningful in terms of saving young adult lives. Thus, although the evidence may not be considered strong at this juncture, we believe it is certainly worthy of future study.
Summary
Whether PB is a cause, correlate, or simply a marker variable for later risky behavior cannot be determined from these analyses. Given the prospective nature of these data, findings suggest that the deficits associated with having a PB in childhood persist throughout adolescence and early adulthood. However, whether a persistent positive bias is necessary to portend these outcomes was not examined directly as PB was only considered at one time point during childhood. Accordingly, an important direction for future work would be to examine if variability in trajectories of self-perception deficits across development influences the extent to which individuals with ADHD engage in risky behavior in young adulthood.
Table 2.
Pearson correlation coefficients of independent variables and covariates with risky behavior variables
| Drive Illegally |
License/Permit Revoked/Suspend |
Tickets | Ever Had Sex |
Lifetime Partners |
Condoms Use Failure |
Age at First intercourse |
|
|---|---|---|---|---|---|---|---|
| Social PB | .06 n = 560 |
.14** n = 397 |
.05 n = 472 |
.08 n = 374 |
.13* n = 253 |
.14* n = 256 |
−.04 n = 256 |
| Behavioral PB | .13** n = 563 |
.25*** n = 398 |
.10* n = 474 |
.09 n = 377 |
.26*** n = 256 |
−.01 n = 259 |
−.15* n = 259 |
| Academic PB | .03 n = 565 |
.10 n = 398 |
.05 n = 474 |
.09 n = 378 |
.15* n = 256 |
−.05 n = 259 |
−.22*** n = 259 |
| ADHD | .10* n = 640 |
.12* n = 443 |
.07 n = 539 |
.04 n = 432 |
.27*** n = 297 |
−.08 n = 299 |
−.24*** n = 300 |
| Estimated IQ | .02 n = 633 |
−.03 n = 439 |
.05 n = 533 |
−.01 n = 428 |
−.17** n = 295 |
.14* n = 297 |
.27*** n = 298 |
| Age at Time 2 | .02 n = 640 |
.08 n = 443 |
.24*** n = 539 |
.10* n = 432 |
.11 n = 297 | .14* n = 299 |
.13* n = 300 |
| Conduct Symptoms | .10* n = 611 |
.07 n = 421 |
−.05 n = 512 |
.11* n = 410 |
.24*** n = 285 |
−.03 n = 287 |
−.26*** n = 288 |
Note: ADHD = Attention-Deficit/ Hyperactivity Disorder (0= LNCG; 1 = ADHD); License/Permit Revoked/Suspend (0=never; 1= yes); Ever had sex (0 = no; 1 = yes); Condom Use Failure (0=always uses; 1=fails to always use); Risky behaviors are ordinal variables;
p<.05,
p<.01,
p<.001.
Acknowledgments
Data analysis and preparation of this article was supported by grant number MH65899 from the National Institute of Mental Health to the first author. The preparation of this manuscript was supported in part by funding from the United States Health and Human Services (USHHS), Administration on Developmental Disabilities (ADD), grant award 90DD0645 awarded to the Center on Disability and Community Inclusion, University of Vermont. The data used in the current paper were drawn from a larger study conducted by the MTA Cooperative Group and supported by the National Institute of Mental Health, the National Institute on Drug Abuse, the Department of Justice, and the Department of Education. (Grant numbers: U01MH50440, U01MH50447, U01MH50453, U01MH50454, U01MH50461, U01MH50467; and contract numbers: N01MH12004, N01MH12007, N01MH12008, N01MH12009, N01MH12010, N01MH12011, N01MH12012). The views expressed in this paper are solely those of the authors, and do not necessarily reflect the views of the National Institute of Mental Health, the National Institute on Drug Abuse, the Department of Justice, the Department of Education, the USHHS, or the ADD and no official endorsement should be inferred. The authors thank Stephen P. Hinshaw and Peter S. Jensen for their helpful comments on an earlier version of this manuscript.
Disclosures: Dr. Arnold has received research funding from CureMark, Forest, Lilly, and Shire, advisory board honoraria from Biomarin, Novartis, Noven, Roche, Seaside Therapeutics, and Shire, consulting fees from Tris Pharma, and travel support from Noven. Dr. Hechtman has been a speaker, served on advisory boards, and received research funds from Janssen Ortho, Purdue Pharma, Shire, and Eli Lilly.
Footnotes
The Multimodal Treatment Study of Children with ADHD (MTA) was a National Institute of Mental Health (NIMH) cooperative agreement randomized clinical trial, continued under an NIMH contract as a follow-up study and finally under a National Institute on Drug Abuse (NIDA) contract. Collaborators from NIMH: Benedetto Vitiello, M.D. (Child & Adolescent Treatment and Preventive Interventions Research Branch), Joanne B. Severe, M.S. (Clinical Trials Operations and Biostatistics Unit, Division of Services and Intervention Research), Peter S. Jensen, M.D. (currently at REACH Institute and Mayo Clinic), L. Eugene Arnold, M.D., M.Ed. (currently at Ohio State University), Kimberly Hoagwood, Ph.D. (currently at Columbia); previous contributors from NIMH to the early phases: John Richters, Ph.D. (currently at National Institute of Nursing Research); Donald Vereen, M.D. (currently at NIDA). Principal investigators and co-investigators from the sites are: University of California, Berkeley/San Francisco: Stephen P. Hinshaw, Ph.D. (Berkeley), Glen R. Elliott, Ph.D., M.D. (San Francisco); Duke University: Karen C. Wells, Ph.D., Jeffery N. Epstein, Ph.D. (currently at Cincinnati Children's Hospital Medical Center), Desiree W. Murray, Ph.D.; previous Duke contributors to early phases: C. Keith Conners, Ph.D. (former PI); John March, M.D., M.P.H.; University of California, Irvine: James Swanson, Ph.D., Timothy Wigal, Ph.D.; previous contributor from UCLA to the early phases: Dennis P. Cantwell, M.D. (deceased); New York University: Howard B. Abikoff, Ph.D.; Montreal Children's Hospital/ McGill University: Lily Hechtman, M.D.; New York State Psychiatric Institute/Columbia University/Mount Sinai Medical Center: Laurence L. Greenhill, M.D. (Columbia), Jeffrey H. Newcorn, M.D. (Mount Sinai School of Medicine). University of Pittsburgh: Brooke Molina, Ph.D., Betsy Hoza, Ph.D. (currently at University of Vermont), William E. Pelham, Ph.D. (PI for early phases, currently at Florida International University). Follow-up phase statistical collaborators: Robert D. Gibbons, Ph.D. (University of Illinois, Chicago); Sue Marcus, Ph.D. (Mt. Sinai College of Medicine); Kwan Hur, Ph.D. (University of Illinois, Chicago). Original study statistical and design consultant: Helena C. Kraemer, Ph.D. (Stanford University). Collaborator from the Office of Special Education Programs/US Department of Education: Thomas Hanley, Ed.D. Collaborator from Office of Juvenile Justice and Delinquency Prevention/Department of Justice: Karen Stern, Ph.D.
Given that the implications of risky behavior may differ by gender, the association between gender and risky behavior also was examined in MPLUS. Analyses showed that females were less likely to have their license or permit revoked or suspended. Follow-up analyses revealed that when gender was accounted for in the model predicting having a license/permit revoked/suspended, findings were consistent to the model in which gender was not a covariate. Gender was not significantly related to any of the other risky behavior variables. Hence, gender was not included as a covariate in analyses.
In general, given the large sample size, marginal effects were not interpreted. In this instance, however, interpreting the marginal effect reflects a more conservative approach (concluding partial mediation rather than full mediation). Therefore, in this instance only, the marginal effect was interpreted.
The effect of ADHD and PB on age at first intercourse also was examined in SPSS version 18.0 using Cox regression, which examines time until an event. Cox regression allows for those participants who had not yet had sex to be included in the analysis. Although Cox regression cannot directly test for mediation, results were consistent with those run in MPLUS and suggested that academic PB predicted early age at first intercourse above and beyond ADHD status.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Barkley RA. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Guevremont DC, Anastopoulos AD, DuPaul GJ, Shelton TL. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: A 3- to 5-year follow-up survey. Pediatrics. 1993;92:212–218. [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, DuPaul GJ, Bush T. Driving in young adults with attention deficit hyperactivity disorder: Knowledge, performance, adverse outcomes, and the role of executive functioning. Journal of the International Neuropsychological Society. 2002;8:655–672. doi: 10.1017/s1355617702801345. [DOI] [PubMed] [Google Scholar]
- Begg DJ, Langley JD, Williams SM. A longitudinal study of lifestyle factors as predictors of injuries and crashes among young adults. Accident Analysis and Prevention. 1999;31:1–11. doi: 10.1016/s0001-4575(98)00039-6. [DOI] [PubMed] [Google Scholar]
- Canu WH, Carlson CL. Rejection sensitivity and social outcomes of young adult men with ADHD. Journal of Attention Disorders. 2007;10:261–275. doi: 10.1177/1087054706288106. [DOI] [PubMed] [Google Scholar]
- Diener MB, Milich R. Effects of positive feedback on the social interactions of boys with attention deficit hyperactivity disorder: A test of the self-protective hypothesis. Journal of Clinical Child Psychology. 1997;26:256–265. doi: 10.1207/s15374424jccp2603_4. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Marlatt GA, Salzberg PM. Drinking behavior, personality factors and high-risk driving: A review and theoretical formulation. Journal of Studies on Alcohol. 1983;44:395–428. doi: 10.15288/jsa.1983.44.395. [DOI] [PubMed] [Google Scholar]
- Evans SW, Hoza B, editors. Treating attention deficit hyperactivity disorder: Assessment and intervention in developmental context. Kingston, NJ: Civic Research Institute; 2011. [Google Scholar]
- Flory K, Molina BSG, Pelham WE, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology. 2006;35:571–577. doi: 10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- Hansen C, Weiss D, Last CG. ADHD boys in young adulthood: Psychosocial adjustment. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:165–171. doi: 10.1097/00004583-199902000-00015. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for the Self-Perception Profile for Children. Unpublished manuscript, University of Denver; 1985. [Google Scholar]
- Hinshaw SP. Attention-deficit/hyperactivity disorder: The search for viable treatments. In: Kendall PC, editor. Child and adolescent therapy: Cognitive-behavioral procedures. 2nd ed. New York: Guilford; 2000. pp. 88–128. [Google Scholar]
- Hinshaw SP, March JS, Abikoff H, Arnold LE, Cantwell DP, Conners CK, Wigal T. Comprehensive assessment of childhood attention-deficit hyperactivity disorder in the context of a multisite, multimodal clinical trial. Journal of Attention Disorders. 1997;1:217–234. [Google Scholar]
- Hoza B, Gerdes AC, Hinshaw SP, Arnold LE, Pelham WE, Molina BSG, Wigal T. Self-perceptions of competence in children with ADHD and comparison children. Journal of Consulting and Clinical Psychology. 2004;72:382–391. doi: 10.1037/0022-006X.72.3.382. [DOI] [PubMed] [Google Scholar]
- Hoza B, Murray-Close D, Arnold LE, Hinshaw SP, Hechtman L the MTA Cooperative Group. Time-dependent changes in positively biased self-perceptions of children with attention-deficit/hyperactivity disorder: A developmental psychopathology perspective. Development and Psychopathology. 2010;22:375–390. doi: 10.1017/S095457941000012X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoza B, Owens JS, Pelham WE. Attention-deficit/hyperactivity disorder. In: Ammerman RT, Hersen M, Last CG, editors. Handbook of prescriptive treatments for children and adolescents. 2nd ed. Boston: Allyn & Bacon; 1999. pp. 63–83. [Google Scholar]
- Hoza B, Pelham WE. Rates of positive bias in children with and without attention-deficit/hyperactivity disorder. 1995 Unpublished raw data. [Google Scholar]
- Hoza B, Pelham WE, Dobbs J, Owens JS, Pillow DR. Do boys with attention-deficit/hyperactivity disorder have positive illusory self-concepts? Journal of Abnormal Psychology. 2002;111:268–278. doi: 10.1037//0021-843x.111.2.268. [DOI] [PubMed] [Google Scholar]
- Hoza B, Vaughn A, Waschbusch DA, Murray-Close D, McCabe G. Can children with ADHD be motivated to reduce bias in self-reports of competence? Journal of Consulting and Clinical Psychology. 2012;80:245–254. doi: 10.1037/a0027299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Arnold LE, Swanson JM, Vitiello B, Abikoff HB, Greenhill LL, Hur K. 3-year follow-up of the NIMH MTA study. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:989–1002. doi: 10.1097/CHI.0b013e3180686d48. [DOI] [PubMed] [Google Scholar]
- Jerome L, Habinski L, Segal A. Attention-deficit/hyperactivity disorder (ADHD) and driving risk: A review of the literature and a methodological critique. Current Psychiatry Reports. 2006;8:416–426. doi: 10.1007/s11920-006-0045-8. [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, Costa FM. Beyond adolescence: Problem behavior and young adult development. NY: Cambridge University Press; 1991. [Google Scholar]
- Jessor R, Jessor L, Donovan JE. Young adult follow-up study, 1981 annual questionnaire. Boulder: University of Colorado, Institute of Behavioral Science; 1981. [Google Scholar]
- Kaiser NM, Hoza B, Pelham WE, Gnagy E, Greiner AR. ADHD status and degree of positive illusions: Moderational and mediational relations with actual behavior. Journal of Attention Disorders. 2008;12:227–238. doi: 10.1177/1087054707311661. [DOI] [PubMed] [Google Scholar]
- Landau S, Milich R. Social communication patterns of attention-deficit-disordered boys. Journal of Abnormal Child Psychology. 1988;16:69–81. doi: 10.1007/BF00910501. [DOI] [PubMed] [Google Scholar]
- Lindberg LD, Santelli JS, Singh S. Changes in formal sex education, 1995–2002. Perspectives on Sexual and Reproductive Health. 2006;38:182–189. doi: 10.1363/psrh.38.182.06. [DOI] [PubMed] [Google Scholar]
- Linnea K, Hoza B, Tomb M, Kaiser N. Does a positive bias relate to social behavior in children with ADHD? Behavior Therapy. 2012;43:862–875. doi: 10.1016/j.beth.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahone EM, Hagelthorn KM, Cutting LE, Schuerholz LJ, Pelletier SF, Rawlins C, Denckla MB. Effects of IQ on executive function measures in children with ADHD. Child Neuropsychology. 2002;8:52–65. doi: 10.1076/chin.8.1.52.8719. [DOI] [PubMed] [Google Scholar]
- McQuade JD, Hoza B, Waschbusch DA, Murray-Close D, Owens JS. Changes in self-perceptions in children with ADHD: A longitudinal study of depressive symptoms and attributional style. Behavior Therapy. 2011;42:170–182. doi: 10.1016/j.beth.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuade JD, Tomb M, Hoza B, Waschbusch DA, Hurt EA, Vaughn AJ. Cognitive deficits and positively biased self-perceptions in children with ADHD. Journal of Abnormal Child Psychology. 2011;39:307–319. doi: 10.1007/s10802-010-9453-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuade JD, Vaughn AJ, Hoza B, Murray-Close D, Molina BSG, Arnold LE, Hechtman L. Perceived social acceptance and peer status differentially predict adjustment in youth with and without ADHD. Journal of Attention Disorders. 2012 doi: 10.1177/1087054712437582. Advance online publication. [DOI] [PubMed] [Google Scholar]
- McKelvey RD, Zavoina W. A statistical model for the analysis of ordinal level dependent variables. Journal of Mathematical Sociology. 1975;4:103–120. [Google Scholar]
- Mikami AY, Calhoun CD, Abikoff HB. Positive illusory bias and response to behavioral treatment among children with attention-deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology. 2010;39:373–385. doi: 10.1080/15374411003691735. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS MTA Cooperative Group. MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(5):484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monuteaux MC, Faraone SV, Gross LM, Biederman J. Predictors, clinical characteristics, and outcome of conduct disorder in girls with attention-deficit/hyperactivity disorder: A longitudinal study. Psychological Medicine. 2007;37:1731–1741. doi: 10.1017/S0033291707000529. [DOI] [PubMed] [Google Scholar]
- Murray-Close D, Hoza B, Hinshaw SP, Arnold LE, Swanson J, Jensen PS, Wells K. Developmental processes in peer problems of children with attention-deficit/hyperactivity disorder in The Multimodal Treatment Study of Children with ADHD: Developmental cascades and vicious cycles. Development and Psychopathology. 2010;22:785–802. doi: 10.1017/S0954579410000465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. Latent variable modeling in heterogeneous populations. Psychometrika. 1989;54:557–585. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6th edition. Los Angeles, CA: Muthen & Muthen; 2010. [Google Scholar]
- Nigg JT. Neuropsychologic theory and findings in attention-deficit/hyperactivity disorder: The state of the field and salient challenges for the coming decade. Biological Psychiatry. 2005;57:1424–1435. doi: 10.1016/j.biopsych.2004.11.011. [DOI] [PubMed] [Google Scholar]
- Ohan JL, Johnston C. Are the performance overestimates given by boys with ADHD self-protective? Journal of Clinical Child Psychology. 2002;31:230–241. doi: 10.1207/S15374424JCCP3102_08. [DOI] [PubMed] [Google Scholar]
- Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM. A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clinical Child and Family Psychology Review. 2007;10:335–351. doi: 10.1007/s10567-007-0027-3. [DOI] [PubMed] [Google Scholar]
- Pittsburgh Adolescent Alcohol Research Center. Sex and Dating Questionnaire. Pittsburgh, PA: University of Pittsburgh; 1996. [Google Scholar]
- Raffaelli M, Crockett LJ. Sexual risk taking in adolescence: The role of self-regulation and attraction to risk. Developmental Psychology. 2003;39:1036–1046. doi: 10.1037/0012-1649.39.6.1036. [DOI] [PubMed] [Google Scholar]
- Sadler JM, Evans SW, Schultz BK, Zoromski AK. Potential mechanisms of action in the treatment of social impairment and disorganization in adolescents with ADHD. School Mental Health. 2011;3:156–168. doi: 10.1007/s12310-011-9058-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattler JM. Assessment of children: Cognitive applications. 4th ed. San Diego: Sattler; 2001. [Google Scholar]
- Swanson EN, Owens EB, Hinshaw SP. Is the positive illusory bias illusory? Examining discrepant self-perceptions of competence in girls with ADHD. Journal of Abnormal Child Psychology. 2012;40:987–998. doi: 10.1007/s10802-012-9615-x. [DOI] [PubMed] [Google Scholar]
- Swanson J, Baler RD, Volkow ND. Understanding the effects of stimulant medications on cognition in individuals with attention-deficit hyperactivity disorder: A decade of progress. Neuropsychopharmacology Reviews. 2011;36:207–226. doi: 10.1038/npp.2010.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarter R. CEDAR follow-up protocol. Pittsburgh: University of Pittsburgh; 1997. [Google Scholar]
- Thompson AL, Molina BSG, Pelham W, Gnagy EM. Risky driving in adolescents and young adults with childhood ADHD. Journal of Pediatric Psychology. 2007;32:745–759. doi: 10.1093/jpepsy/jsm002. [DOI] [PubMed] [Google Scholar]
- Whalen CK, Henker B, Collins BE, McAuliffe S, Vaux A. Peer interaction in a structured communication task: Comparisons of normal and hyperactive boys and of methylphenidate (Ritalin) and placebo effects. Child Development. 1979;50:388–401. doi: 10.1111/j.1467-8624.1979.tb04120.x. [DOI] [PubMed] [Google Scholar]