Abstract
Background
Scarring is a very common complication of severe acne and is difficult to treat by conventional methods. 5-Aminolevulinic acid (ALA) photodynamic therapy (PDT) is a novel treatment for improving acne lesions. Fractional laser resurfacing is a promising treatment for scar treatment because of its unique ability to stimulate the wound healing response and its depth of penetration.
Objective
To evaluate the efficacy of combination therapies of ALA-PDT and ablative fractional Er:YAG laser (2,940 nm) for scarring lesions in severe acne patients.
Methods
A prospective, single-arm, pilot study. Forty subjects with severe acne were treated with 15% ALA-PDT for four times at 10-day intervals. They then received ablative fractional Er:YAG laser treatment five times at 4-week intervals. Three independent investigators evaluated subject outcomes at 1, 3, 6, and 12 months post-treatment (primary outcome); patients also provided self-assessments of improvement (secondary outcome).
Results
Significant reductions in acne score (P<0.01) were obtained at follow-up visits after 1, 3, 6, and 12 months. After 6 month, the lesions showed overall improvement in all of subjects (good to excellent in acne inflammatory lesions), 80% overall improvement in acne scars. After 12 months, most of subjects had improved hypertrophic/atrophic scars (good to excellent in 85%) and no one had recurrent acne inflammatory lesions. Patient self-evaluation also revealed good to excellent improvements (on average) in acne lesions and scarring, with significant improvements in self-esteem after 6 months post-treatment.
Conclusions
PDT can control the inflammation and improve the severity of acne lesions. Fractional resurfacing is a promising new treatment modality for scars by stimulating wound healing and remodeling. The combination therapy is a promising option for severe acne to prevent and improve car formation.
Keywords: acne vulgaris, photodynamic therapy, ablative fractional laser, atrophic scars, 5-aminolevulinic acid, erbium: yttrium-aluminum-garnet laser
INTRODUCTION
Acne is a chronic inflammatory disease of the pilosebaceous units resulting from an androgen-induced increase in sebum production, altered keratinization, leading to follicular colonization by Propionibacterium acnes, and an inflammatory reaction[1]. Acne vulgaris has diverse clinical presentations which include seborrhea (excess production of a greasy secretion), non-inflammatory lesions (open and closed comedones), inflammatory lesions (papules and pustules), and variable degrees of disfiguring scarring [1,2]. About 10% of cases with deep cystic and/or nodular lesions are more resistant to treatment and therefore prone to scarring. Acne, especial moderate to severe, can cause a significant negative impact on psychological well-being and quality of life. Although there are numerous treatment options available for patients with acne including drug and physical therapy, some cases of intractable acne is likely to be resistant to all of the currently available treatments. Some patients show resistance to systemic or local antibiotic therapy targeting P. acnes, which also cannot be aggravated by indiscriminate use of antibiotic therapy. Furthermore, many patients do not tolerate oral treatment with retinoids such as isotretinoin that shrink sebaceous glands, due to severe side-effects [3].
Topical 5-aminolaevulinic acid-photodynamic therapy (ALA-PDT) has been found to be an efficacious treatment for acne vulgaris with the potential to kill bacteria in hair follicles and sebaceous glands, reduce the production of sebum from sebaceous glands, and improve the occlusion of sebaceous follicles [4,5]. Several studies have demonstrated ALA-PDT is a safe and efficient option in clinical practice [2,6]. Our previous clinical study also showed the effect of ALA-PDT in the treatment of moderate to severe facial acne in Chinese patients with Fitzpatrick skin type III and IV [3]. ALA-PDT controlled inflammatory and non-inflammatory acne lesions in a short time accompanied by a low recurrence rate, was well-tolerated and without severe adverse effects. If moderate to severe inflammatory acne lesions can be eliminated at an early stage, it could reduce the possibility of scar formation.
If there are existing scars, effective reconstructive surgery is of paramount importance to the quality of life of acne patients. The long-term care of acne patients encompasses the optimal aesthetic outcome for each patient. The depth and extent of acne scarring varies and can be improved by different procedures including subcision, punch excision, laser resurfacing, dermabrasion, and chemical peels [7,8]. Recently, acne scarring has increasingly been treated with fractional ablative laser treatment, one technique that produces thousands of microthermal areas of dermal ablation separated by areas of untreated skin, with fewer side-effects and a quicker healing period than traditional ablative laser resurfacing [9]. Fractional ablative laser treatment has advantages over other options due to its ability to resurface the epidermis and to produce thermal damage in the dermis to safely promote the formation of new collagen while at the same time allowing rapid healing. It is particularly effective for acne scars which go deep, (often through the entire dermis) and has shown significant decreases of hypertrophic and atrophic scars, decreased hyperpigmentation, decreased erythema, and textural improvements [10]. It is possible that fractional ablative laser can intervene in the process of collagen synthesis in the early stage to prevent the formation of scarring. There may be a role for laser treatment pre-operatively to soften the scar. There is a need for further investigation to determine if treating an early developing scar with fractional laser may help minimize the ultimate scar. In order to verify this point, we evaluated the efficacy of a combination treatment of ALA-PDT with ablative fractional Er:YAG laser (2,940 nm) as a therapeutic option for improving cutaneous lesions in severe acne patients in a prospective single-arm pilot study.
METHODS
Subject Population
This clinical study was performed at the Department of Dermatology, Southwest Hospital, Chongqing, China. It was approved by the local Institutional Review Board, was conducted in compliance with protocol, good clinical practice, and adhered to the Helsinki guidelines. The study enrolled 40 subjects with moderate to severe facial inflammatory acne (graded according to Pillsbury et al. [11]). All subjects were identified as having Fitzpatrick skin type III and IV. There were 32 males and 8 females with an average age of 28 years. No other topical, oral, or light-based therapies were used in the treatment regimen. All subjects confirmed that they were not using other photosensitizing medications. Exclusion criteria included pregnancy, oral/topical antibiotics usage for the acne, herpes simplex outbreak, photosensitivity, history of keloids, and use of retinoids 6 months prior to treatment. Patients were provided with a detailed description of the purpose and possible outcomes of the treatment and signed informed consent forms to participate in the study and provided their permission for clinical photographs to be taken.
Study Design and Treatment Parameters
The study was a prospective, single-arm, pilot study. Patients were treated in the clinic of the Department of Dermatology, Southwest Hospital, Chongqing, China using the existing treatment facilities. Subjects had all makeup and lotions removal immediately prior to treatment. Following cleaning of the skin with 70% isopropyl alcohol, patients received topical 15% ALA in an oil-in-water emulsion on the skin lesions. Following occlusion with plastic film for 2 hours, patients were exposed to 126 J/cm2 red light (Omnilux Revive, Photo Therapeutics, Inc., London, UK) at a wavelength 633±6 nm and output intensity 105mW/cm2 for 20 minutes. Subjects were treated once every 10 days for four sessions [3].
Commencing 1 month following the last ALA-PDT treatment, subjects received ablative fractional 2,940 nm Er:YAG laser treatment given five times at 4-week intervals. A topical anesthetic cream (EMLA [eutectic mixture of lidocaine and prilocaine], AstraZeneca, London, UK) was applied before laser. The laser used was the Pixel Er:YAG system (Harmony® platform, Alma Laser™, Israel) which delivers the laser beam via a hand-piece equipped with a beam splitter which divides the beam into microbeams of 850 mm each in diameter. The window of the laser hand-piece covered an 11 mm × 11 mm treatment area with 49 microbeams (7×7 dots). The system has three treatment pulse length programs: Short (1 milliseconds pulse length), Medium (1.5 milliseconds pulse length), and long (2 milliseconds pulse length). The repetition rate was 2 Hz—2 shots per second, so approximately 500 milliseconds between passes [12]. The single-pass ablation microzone of each pixel measured approximately 150 mm in diameter and 120–140mm in depth [13]. For this study, we used a 7×7 (49-dot) alignment, the output pulse energy being 1,600–1,800 mJ/pulse in a long pulse length program. Four to five stacked laser passes were performed.
Clinical Evaluations
All subjects were asked to return 24 hours after treatment for initial baseline assessment, and 1, 3, 6, and 12 months post last therapy for clinical evaluation. Clinical evaluations consisted of two measures: assessment of inflammatory acne and the improvement of scarring. Evaluation of inflammatory lesions was based on the criteria of Hongcharu et al. [4] and we did minor modification. Briefly, the numbers of skin lesions including comedones, papules, pustules, nodules, and cysts were recorded simultaneously by three dermatologists before each ALA-PDT session. Each type of lesion was allocated a severity index as shown in Table 1. The number of acne lesions was counted manually by the investigators at baseline and at each follow-up visit. The status of skin lesions after therapy was compared with that at baseline. We assessed the clinical efficacy of Er:YAG ablative fractional laser skin resurfacing, including the scars, texture, and hyperpigmentation at the baseline, and 1, 3, 6, 12 months. Overall clinical improvement compared to baseline was assessed by a grading scale that was defined as: less than 25% difference recorded as “slightly better,” 25–50% improvement recorded as “fair,” 51–75% improvement recorded as “good” and 76–100% recorded as “excellent.” Clinical success was also rated by the patients’ self-assessment of their acne score.
TABLE 1.
The Scores for Different Acne Lesions
| Lesions | Score |
|---|---|
| Comedone (<1mm) | 0.5 |
| Inflammatory comedone | 0.75 |
| Papule (1–5 mm) | 1 |
| Pustule | 2 |
| Nodule (>5 mm) | 3 |
| Inflammatory cyst | 4 |
| Scar | 5 |
Patients’ Self-Assessment and Treatment Tolerance
Patients were asked to record information regarding procedure-related pain and other postoperative side effects such as erythema and hyperpigmentation [14]. Patients were instructed on how to score procedure-related pain using an 11-point visual analogue scale (VAS), where 10 was unbearable pain and zero was no pain, and the results were graded as follows: extremely painful (10–9 on the VAS, +++); very painful (7–8, ++); bearable pain (6–4, +); little pain (1–3,±); and no pain (0, −). Answers were tabulated. The patients’ self-evaluation at the follow-up assessment, based on the improvement of the acne lesions, scars, and general skin condition, was graded into one of four categories: slightly better, fair, good, and excellent corresponding to the following numeric responses denoting less than 25%, 25–50%, 51–75%, 76–100% improvement of the aforementioned conditions. After received all treatments and follow-up assessments, subjects gave an evaluation of final satisfaction graded as very satisfied (VS); satisfied (S); somewhat satisfied (FS); and not satisfied (NS). The values scored for VS and S were summed and expressed as a percentage to give the patient satisfaction index (SI).
Adverse Effects
All adverse effects including pruritus, pain, pustules, vesicles, erythema, hyperpigmentation, loss of epidermis, exfoliation, and scarring were recorded in detail at each treatment and follow-up visit. Adverse effects were recorded according to persistence, time to resolve, severity (0, absent; 1, mild; 2, moderate; 3, severe), treatment measure, and outcome.
Statistical Analyses
Statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, NC). Subjects were grouped into categories based on their average objective improvement score. Subjective improvements in scar area and self-esteem ratings were presented as means and SDs. Pre and post-treatment self-esteem scores were compared using a Wilcoxon sign rank test; this non-parametric test was used because the change in self-esteem scores was not normally distributed.
RESULTS
Forty patients with acne vulgaris were treated with ALA-PDT and ablative fractional laser in our department. There were 32 male and 8 females with an average age of 28±0.3 years old. The history of disease ranged from 12 to 60 months (mean 36.5±2.5 months). All of the 40 patients finished the whole therapy course and were successfully followed up through regular clinical consultations. Characteristics of the subjects in each group are shown in Table 2.
TABLE 2.
Baseline of Demographic and Characters of Acne Lesions
| Characteristic | Value |
|---|---|
| Age (years), mean±SD | 28±0.3 |
| Gender (M/F) | 32/8 |
| Skin phototype, n (%) | |
| Type III | 28 |
| Type IV | 12 |
| Global severity, n (%) | |
| Moderate | 18 |
| Severe | 22 |
| Disease history (years), mean±SD | 3.2±1.8 |
| Cutaneous manifestation | |
| Numbers of baseline comedones, median (range) | 10.5 (8–25) |
| Numbers of baseline inflammatory comedones, median (range) | 18.0 (12–42) |
| Numbers of baseline papules, median (range) | 35.0 (20–85) |
| Numbers of baseline pustules, median (range) | 48.0 (36–90) |
| Numbers of baseline nodules, median (range) | 4.5 (2–10) |
| Numbers of baseline cysts, median (range) | 5.0 (3–8) |
| Numbers of baseline scars, median (range) | 155.0 (130–185) |
Clinical Assessment
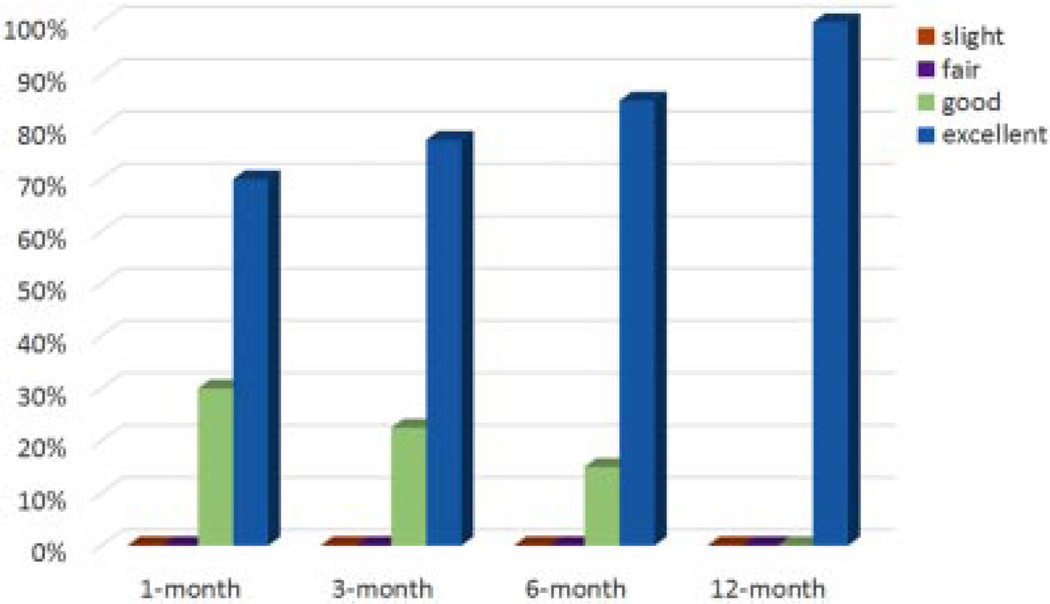
Thirty-eight patients received four treatments with ALA-PDT; while another two patients received an additional treatment because inflammatory lesions still existed after four treatments. Clinical improvement was assessed by three blinded independent dermatologists. The outcome of the combination treatment (ALA-PDT and ablative fractional laser therapy) gave significant improvement, which persisted throughout all four follow-up visits. Significant reductions in acne lesions score were obtained at follow-up visits after 1, 3, 6, and 12 months increasingly. The acne lesions (except scars) began to vanish after the first treatment with ALA-PDT. They continued to gradually improve after the succeeding ALA-PDT sessions. During the period of ablative fractional laser treatment, the acne lesions (except scars) were well-controlled with no recurrence. After all five treatments with ablative fractional laser, the improvement of the subjects’ acne lesions (except scars) at 1-month post-treatment was judged as excellent in 75% (30/40), good in 25% (10/40), fair in 0% (6/ 40), and slight improvement in 0% (2/40). At the 6-month follow-up, the improvement was graded as excellent in 85% (34/40), good in 15% (6/40), fair in 0% (0/40), and slight improvement in 0% (0/40). At the 12-month follow-up, all of the acne lesions (except scars) had disappeared without recurrence and were graded as excellent in 100% (40/40). As shown in Figure 1, there was no significant statistical difference between the four follow-up visits. However, there was a statistically significant clinical improvement in acne lesions (except scar) after treatment compared with the baseline (P<0.01).
Fig. 1.
The improvement of acne inflammatory lesions in 40 patients after treatment. Evaluations were conducted using photographs taken before and 1, 3, 6, and 12 months after serial treatment by three blinded independent dermatologists, using 4-point improvement scale.
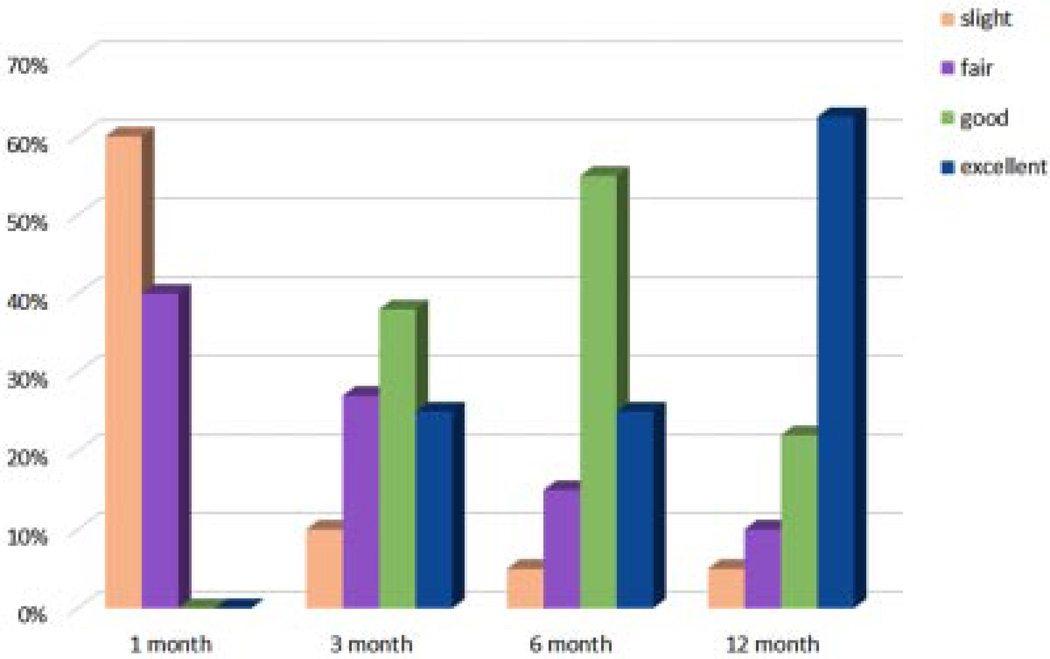
During the whole period of treatment, whether ALA-PDT or ablative fractional laser treatment there was no new formation of scars. At the 1-month follow-up post-treatment, existing acne scars began to improve. As shown in Figure 2, the improvement of subjects’ scars was graded as excellent in 0% (0/40), good in 0% (0/40), fair in 40% (16/40), and slight improvement in 60% (24/40). At the 6-month follow-up, the improvement of the subjects’ scars was recorded as excellent in 25% (10/40), good in 55% (22/40), fair in 15% (6/40), and slight improvement in 5% (2/40). At the 12-month follow-up, the clinical improvement in the appearance of the scars significantly progressed and was graded as excellent in 62.5% (25/40), good in 22.5% (9/40), fair in 10% (4/40), and slight improvement in 5% (2/40). There was significant difference in clinical outcome of acne scars at the 3-month follow-up compared with the 1-month follow-up (P=0.012), at the 6-month follow-up compared with the 3-month follow-up (P=0.005), and at the 12-month follow-up compared with the 6-month follow-up (P=0.0052).
Fig. 2.
The improvement of acne scars in 40 patients after treatment. Evaluations were conducted using photographs taken before and 1, 3, 6, and 12 months after serial treatment by three blinded independent dermatologists, using 4-point improvement scale.
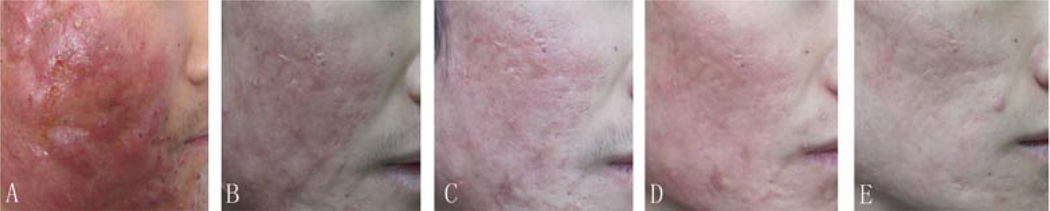
Image analysis evaluated at 1, 3, 6, and 12 months after treatment showed obvious and statistically significant improvements of the skin surface smoothness (P=0.015) and in scar volume (P=0.0029), compared with the baseline measurement. There were further improvements in skin surface smoothness at 3- and 6-month follow-ups, compared with the improvement seen at 1-month followups. However, there was no further improvement of skin surface smoothness at the 12-month follow-up, compared with the improvement in appearance at 6-month follow-up (P=0.165). Clinical photographs from one typical patient before and after treatment are presented in Figure 3.
Fig. 3.
Typical features of one patient received Er:YAG fractional ablative laser therapy. The patient received 15% ALA-PDT (633±6 nm wavelength, 126 J/cm2, 20 minutes) five times at 10-days intervals. After 1 month, he accepted another five times fractional ablative laser therapy (2,900 nm wavelength, 7×7 (49-dot) alignment, 1,600 mJ/P, long pulse, five stacks) at 1-month intervals. (A) Before treatment; (B) 1-month follow-up after treatment; (C) 3-month follow-up after treatment; (D) 6-month follow-up after treatment; (E) 12-month follow-up after treatment.
Patients’ Self-Evaluation and Treatment Tolerance
The self-evaluations of treatment outcome made by the subjects themselves at the 12 month follow-up visit is shown in Table 3. All patients rated themselves as being “very satisfied (VS)” with the improvement in their acne, especially the inflammatory acne lesions. The majority of patients (55%, 22 of 40 subjects) assessed themselves as having an excellent improvement in their acne scars. No subject considered themselves to have a worsened appearance of their acne lesions and scars after the combination treatment. All patients tolerated the PDT and laser therapy. All patients reported that the treatment-related pain was generally well tolerated. Average pain score described by the subjects was 3.5±1.3 (mean±SD) on a scale of 10. The subject tolerance of the treatments tended to improve with successive treatment sessions as evidenced by the consecutive reduction of average pain scores.
TABLE 3.
Patient-Reported Improvement at the Follow-Up After All Treatments
| Improvements, No. of patients (%) after 1 month |
Improvements, No. of patients (%) after 3 months |
Improvements, No. of patients (%) after 6 months |
Improvements, No. of patients (%) after 12 months |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Condition | Slightly better (%) |
Fair (%) |
Good (%) |
Excellent (%) |
Slightly better (%) |
Fair (%) |
Good (%) |
Excellent (%) |
Slightly better (%) |
Fair (%) |
Good (%) |
Excellent (%) |
Slightly better (%) |
Fair (%) |
Good (%) |
Excellent (%) |
| Inflammatory lesions | 0 | 0 | 30 | 70 | 0 | 0 | 15 | 85 | 0 | 0 | 0 | 100 | 0 | 0 | 0 | 100 |
| Acne scars | 52.5 | 40 | 7.5 | 0 | 15 | 20 | 37.5 | 27.5 | 0 | 20 | 40 | 50 | 0 | 12.5 | 22.5 | 65 |
| Skin texture | 70 | 25 | 5 | 0 | 5 | 35 | 30 | 30 | 0 | 25 | 40 | 35 | 0 | 12.5 | 42.5 | 45 |
| Skin smoothness | 2.5 | 7.5 | 37.5 | 52.5 | 0 | 10 | 30 | 60 | 0 | 7.5 | 37.5 | 55 | 2.5 | 17.5 | 45 | 35 |
| Overall satisfaction | 0 | 15 | 40 | 45 | 0 | 2.5 | 30 | 67.5 | 0 | 0 | 35 | 75 | 0 | 0 | 12.5 | 87.5 |
Adverse Effects
When treated with ALA-PDT, a burning sensation occurred in almost all the patients, but seldom led to feeling considerable pain and normally disappeared within 5 minutes. However, the sensation did not worsen with subsequent treatments. Erythema and edema were induced after light exposure, lasted for 1–5 days, and mostly resolved within 2 days. A monomorphic transient acneiform eruption occurred within 5 days. Hyperpigmentation occurred in two patients (5%) at 1 week after the first ALA-PDT treatment and faded completely at 2–3 weeks without any medical treatment except shielding from sunshine. Three patients (7.5%) presented with slight scaling and dryness accompanied by slight exfoliation. Marked dryness, scaling, and desquamation occurred in five patients. All these resolved at the 1-month follow-up visit.
When treated by ablative fractional laser, all patients experienced erythema and edema within the first three days post-treatment, which persisted but decreased in severity within 1 week. The incidence of postinflammatory hyperpigmentation (PIH) was 35% (14 of 40 subjects). All cases with the complication of PIH were graded as mild, except one case which was rated as moderate. The average duration of PIH was 3 weeks (range 2–5 weeks). The rate of PIH at 1 month post-treatment was 15%. By 3 months, the PIH rate decreased to 5%, with most cases being graded as mild. At 6 months, no patient had persistent PIH. No hypopigmentation, pinpoint bleeding blister, erosion, scarring, facial dermatitis, bacterial, or viral infection was observed at the any of the follow-up visits of up to 6–12 months post-treatment. No significant adverse effects or clinical sequelae caused by therapy were observed.
DISCUSSION
Acne scarring is a common sequelae of inflammatory acne vulgaris that may be permanent and socially debilitating to patients. It results from loss of collagen deposition during wound-healing and is considered to be associated with the degree of inflammation of the acne lesions as well as with a late start of adequate treatment [15]. Severe acne remains an important entity to be recognized and treated early to prevent severe scarring and patient suffering [1]. Conventional therapies consist of the following medications: retinoids, oral contraceptives, antiandrogens, and antibiotics. Even with optimal medical therapy, recalcitrant acne is common and severe acne can be intractable. Systemic treatment, including oral isotretinoin and antibiotics, has been proven to be the most effective treatment [2]; however, side effects have been reported with increasing incidence. Therefore, the search for new and more effective acne therapies with lower rates of adverse effect seems imperative.
ALA-PDT was first described to be efficacious in controlling acne vulgaris in adults, with a study in back acne by Hongcharu [4]. Up to now, there have been several literature reports that acne can respond well to PDT using topical ALA or porphyrin derivatives (reviewed in Ref. [16]). The most important biological mechanisms of ALA-PDT are direct sebaceous gland destruction, reduction of follicular obstruction and hyperkeratosis, and immunologic changes [2,4]. Although there remain uncertainties about the precise mechanisms of ALA-PDT for acne treatment, clinical manifestation can be improved in a short period and the long-term acne remission can be maintained with acceptable and tolerable side effects. Now it has been accepted as an alternative acne treatment for those resistant to conventional treatments or who are intolerant of their side effects. It is already clear that higher-ALA dose, longer contact time, and higher light fluence exposure is beneficial for inhibition of sebaceous gland function and to produce prolonged remission of acne vulgaris [16], which is very important for controlling the inflammation of severe acne and reducing the risk of scarring formation. In our previous randomized, placebo-controlled, split-face clinical study, we showed 15% ALA-PDT induced a significant improvement of moderate to severe acne lesions with no recurrent lesions observed during 6 months of follow-up visits [3]. Therefore, considering effectiveness and safety for Chinese patients (mostly with skin type II and III), we used a similar ALA-PDT regimen to control acne lesions in the present clinical trial. The improvement in inflammatory acne lesions was scored as excellent in 75%, 85%, 100%, and 100% at the 1, 3, 6, and 12 months postoperative followup visit respectively, as judged by three different dermatologists. Patients’ self-evaluation showed that 70%, 85%, 100%, and 100% were recorded as excellent at the four different time-point follow-up visits respectively. The results confirmed the efficacy and safety of ALA-PDT to treat severe acne without recurrence for 6 months.
Fractional laser resurfacing is a new concept for laser skin resurfacing using a fractional approach for laser delivery to create microscopic zones of thermal damage with controlled width, densities, and depth of damage in the dermis. Theoretically, the geometry of those microscopic thermal injury zones (MTZs) determines the efficacy of fractional resurfacing laser. In addition, the clinical results also correlate with the depth of the scars or the degree of photodamage being treated. Several ablative fraction resurfacing (AFR) modalities have been already used in clinical practice, providing a promising fractional photothermolysis (FP) treatment option for different cases whether for photoaging (rhytides), or for post-traumatic scars (burn scars, acne atrophic scars, postsurgical scars, etc.). Compared to 10,600 nm CO2 AFR laser, Er:YAG AFR laser can deliver energy more precisely without excessive thermal damage to the surrounding tissue because the absorption of Er:YAG (2,940 nm) is much closer to that maximum of water (3,000 nm), thereby permitting quicker wound healing and recovery of the dermis [17–19]. In addition, Er:YAG AFR laser can deposit much more heat deeply into the dermis and remove the epidermis more precisely when using sub-ablative energies and long pulse program [19]. Meanwhile, the relatively side effects including erythema, edema, PIH, scarring, and skin infection induced by ER:YAG AFR are much less than with CO2 AFR, especially for darker skin phototypes. Therefore, although Er:YAG AFR exerts less dermal tightening than CO2 AFR, it can bring more beneficial morphological changes to both the epidermis and the superficial dermis with less side effects and accelerating wound healing [18].
Several literature reports have demonstrated the efficacy of Er:YAG AFP on acne scars. Lapidoth et al. [13] reported 28 patients treated using the fractional 2,940-nm Er:YAG laser, demonstrated excellent results in 75% of patients after an average of 3.2 treatment sessions. Hu et al. [19] reported that patients suffering from severe atrophic acne scarring, had a 72.7% satisfaction rate, with acceptable downtime in one treatment session using the ablative fractional Er:YAG laser in one clinical study. The results were comparable with the report from Cho [20] and Manuskiatti [21] in their study of fractional CO2 laser in Asian skin. It means that using Er: YAG AFP with long pulse, and multiple passes could produce significant clinical improvements similar to CO2 AFR. The histological examination also showed a correlation between epidermal removal and an increased number of fractional Er:YAG laser passes, thus increasing the levels of residual thermal damage [12].
To achieve the maximum possible therapeutic effect, we chose multiple stacked passes, with the long pulse program, for five consecutive sessions as a treatment regimen to produce better skin remodeling which could be considered as “more aggressive” than has been previously reported in other studies [14]. However, we believe that the treatment as described not only resurfaced the surface of the epidermis but also increased the degree of photothermal dermal damage due to the stacking of passes, thereby depositing sufficient thermal energy into the dermis to stimulate neocollagenesis. This is essential to provide the optimal clinical outcome for both the clinician and the patient, because the architecture of both the epidermis and the dermis is affected. In fact, the external appearance of the skin, including the smoothness and the texture of the epidermis, is what patients first see in the mirror, and constitutes satisfaction with the results. Significant improvement in the appearance of acne scars may result from effective remodeling and tightening of the extracellular matrix. During the follow-up, the improvement of the subjects’ scars at 6-month post-treatment was graded as excellent in 25%, good in 55%. At 12-month follow-up, the improvement of the scar was recorded as excellent in 63%, good in 22%. Patients’ self-evaluations indicated that their satisfaction rates compared well with the clinicians’ evaluations.
The optimal time frame for improvement in scars by fractional ablative laser therapy has not yet been determined. The concept of using laser as a prophylaxis against scaring is relatively new, especially during the early postoperative and post-traumatic period. The current consensus states that laser therapy should occur predominantly after surgery in traumatic scar patients. Consideration may be given to whether there is a role for laser preoperatively to soften the scar [22]. It is important to have a stable, epithelized wound prior to laser therapy. Recently, Ozog et al. [23] published a clinical trial with a small sample size showing improvement of Mohs surgical scars treated with fractional carbon dioxide laser intra-operatively that appeared to improve both appearance and texture. Kim et al. [24] evaluated the efficacy of 2,940 nm Er:YAG AFR for 12 patients with facial laceration scars in the early post-traumatic period (1 month). These clinical results warrant further investigation to determine if treating an early developing scar with fractional lasers may help prophylaxis against scarring or minimize the ultimate scar. Waibel et al. [22] also proposed that the optimal time for treatment for scar resurfacing with laser may vary among individuals but appears to be months—1 year after the injury. Based on these reports, we applied ablative fractional Er: YAG laser to treat acne scars as early as 30 days after controlling the acute inflammation. Although even severe acne can be treated efficiently by ALA-PDT, the loss of collagen deposition caused by the severe inflammatory process may still lead to scarring. Therefore, early employment of ablative fractional Er: YAG laser at 30 days could be useful to minimize the possibility of scar formation and to simultaneously improve the existing acne scars. The results of our pilot study showed the combination treatment controlled the severe acne lesions well and improved the existing scarring while preventing the formation of new scarring.
Although all patients manifested erythema immediately and had mild to moderate edema after PDT and Er:YAG AFR combination, most patients showed good tolerance to the treatment. Immediate application of an ice compress or blowing cool air after therapy is important for decreasing erythema and edema. In our cases hyperpigmentation mostly faded gradually over weeks to months for PDT, the tissue-damage mechanism is cellular apoptosis caused by oxidative damage but not by thermal damage [25], but histopathological studies showed only a slight infiltration of inflammatory cells. The incidence of hyperpigmentation was positively correlated with the ALA concentration in ALA-PDT [3]. However, all of our patients showed a full recovery within 3 months of follow up. With ablative laser therapy, PIH is one of the most important adverse effects, especially for dark-skinned patients. Although the exact pathogenesis of PIH is unknown, it has been postulated as a biologic response of keratinocytes and/or melanocytes to the inflammatory phase of the wound healing cascade and this type of environment can be induced by nonspecific thermal damage caused during laser irradiation. Ruiz- Esparza and Lupton [26] suggested that the duration and intensity of erythema corresponded to the extent of tissue inflammation, with resultant pigmentary disturbances in dark-skinned individuals. In our study, we used a low density (7×7) with the maximum pulse energy output being 1,800 mJ/P and the patient’s erythema resolved in 1– 2 days, postoperatively. The brief duration of erythema may imply that there is a lesser degree of nonspecific thermal damage created around each individual microthermal zone (MTZ) and may also explain the milder degree and faster clearing of PIH.
Transient PIH after conventional ablative fractional CO2 laser resurfacing was observed in 37% of patients with all skin types [27] and in more than 70% of patients with skin type IV or higher [28]. Hu et al. [19] reported a lower PIH rate of 3% using Er:YAGAFR in the treatment of acne scars in type IV skin. Although the incidence of mild to moderate PIH in our clinical trial was high, all of the patients showed a full recovery within 6 months of follow up.
A limitation of this study is the relatively small sample size. Furthermore, the combination treatment regimen in several sessions might increase difficulties in maintaining patient compliance. Nevertheless, significant clinical improvements were found using the combination of ALA-PDT and Er:YAG AFR which may be a potential approach for the treatment of severe acne, preventing the formation of scarring and improving the existing atrophic scars in individuals with dark-skinned phototypes. It will be necessary further investigate the optimum regimen for treating acne in Asian patients in future work.
ACKNOWLEDGMENTS
This study was supported partly by National Natural Science Foundation of China (No. 81172495). Michael R. Hamblin was supported by US NIH grant R01AI050875.
Contract grant sponsor: National Natural Science Foundation of China; Contract grant number: 81172495; Contract grant sponsor: NIH Grant; Contract grant number: R01AI050875; Contract grant sponsor: ASLM.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and have disclosed the following: No authors hold stock, or receive royalties from any companies.
Statement on prior presentation: Part of the Data was presented as an abstract at the American Society of Lasers, Medicine and Surgery Annual Meeting. Boston, MA, April 7, 2013.
REFERENCES
- 1.Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet. 2012;379(9813):361–372. doi: 10.1016/S0140-6736(11)60321-8. [DOI] [PubMed] [Google Scholar]
- 2.Sakamoto FH, Lopes JD, Anderson RR. Photodynamic therapy for acne vulgaris: A critical review from basics to clinical practice: Part I. Acne vulgaris: When and why consider photodynamic therapy? J Am Acad Dermatol. 2010;63(2):183–193. doi: 10.1016/j.jaad.2009.09.056. [DOI] [PubMed] [Google Scholar]
- 3.Yin R, Hao F, Deng J, Yang XC, Yan H. Investigation of optimal aminolaevulinic acid concentration applied in topical aminolaevulinic acid-photodynamic therapy for treatment of moderate to severe acne: A pilot study in Chinese subjects. Br J Dermatol. 2010;163(5):1064–1071. doi: 10.1111/j.1365-2133.2010.09860.x. [DOI] [PubMed] [Google Scholar]
- 4.Hongcharu W, Taylor CR, Chang Y, Aghassi D, Suthamjariya K, Anderson RR. Topical ALA-photodynamic therapy for the treatment of acne vulgaris. J Invest Dermatol. 2000;115(2):183–192. doi: 10.1046/j.1523-1747.2000.00046.x. [DOI] [PubMed] [Google Scholar]
- 5.Zeina B, Greenman J, Purcell WM, Das B. Killing of cutaneous microbial species by photodynamic therapy. Br J Dermatol. 2001;144(2):274–278. doi: 10.1046/j.1365-2133.2001.04013.x. [DOI] [PubMed] [Google Scholar]
- 6.Haedersdal M, Togsverd-Bo K, Wulf HC. Evidence-based review of lasers, light sources and photodynamic therapy in the treatment of acne vulgaris. J Eur Acad Dermatol Venereol. 2008;22(3):267–278. doi: 10.1111/j.1468-3083.2007.02503.x. [DOI] [PubMed] [Google Scholar]
- 7.Thiboutot D, Gollnick H, Bettoli V, Dreno B, Kang S, Leyden JJ, Shalita AR, Lozada VT, Berson D, Finlay A, Goh CL, Herane MI, Kaminsky A, Kubba R, Layton A, Miyachi Y, Perez M, Martin JP, Ramos ESM, See JA, Shear N, Wolf J., Jr Global Alliance to Improve Outcomes in A. New insights into the management of acne: An update from the Global Alliance to Improve Outcomes in acne group. J Am Acad Dermatol. 2009;60(5 Suppl):S1–S50. doi: 10.1016/j.jaad.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 8.Antoniou C, Dessinioti C, Stratigos AJ, Katsambas AD. Clinical and therapeutic approach to childhood acne: An update. Pediatr Dermatol. 2009;26(4):373–380. doi: 10.1111/j.1525-1470.2009.00932.x. [DOI] [PubMed] [Google Scholar]
- 9.Tierney EP, Kouba DJ, Hanke CW. Review of fractional photothermolysis: Treatment indications and efficacy. Dermatol Surg. 2009;35(10):1445–1461. doi: 10.1111/j.1524-4725.2009.01258.x. [DOI] [PubMed] [Google Scholar]
- 10.Waibel J, Beer K. Ablative fractional laser resurfacing for the treatment of a third-degree burn. J Drugs Dermatol. 2009;8(3):294–297. [PubMed] [Google Scholar]
- 11.Pillsbury DMSW, Kligman A, editors. A manual of cutaneous medicine. Philadelphia: W.B Saunders; 1961. [Google Scholar]
- 12.Trelles MA, Velez M, Mordon S. Correlation of histological findings of single session Er:YAG skin fractional resurfacing with various passes and energies and the possible clinical implications. Lasers Surg Med. 2008;40(3):171–177. doi: 10.1002/lsm.20607. [DOI] [PubMed] [Google Scholar]
- 13.Lapidoth M, Yagima Odo ME, Odo LM. Novel use of erbium: YAG(2,940-nm) laser for fractional ablative photothermolysis in the treatment of photodamaged facial skin: A pilot study. Dermatol Surg. 2008;34(8):1048–1053. doi: 10.1111/j.1524-4725.2008.34204.x. [DOI] [PubMed] [Google Scholar]
- 14.Trelles MA, Mordon S, Velez M, Urdiales F, Levy JL. Results of fractional ablative facial skin resurfacing with the erbium: yttrium–aluminium-garnet laser 1 week and 2 months after one single treatment in 30 patients. Lasers Med Sci. 2009;24(2):186–194. doi: 10.1007/s10103-008-0545-3. [DOI] [PubMed] [Google Scholar]
- 15.Goodman G. Postacne scarring: A review. J Cosmet Laser Ther. 2003;5:77–95. doi: 10.1080/14764170310001258. [DOI] [PubMed] [Google Scholar]
- 16.Sakamoto FH, Torezan L, Anderson RR. Photodynamic therapy for acne vulgaris: A critical review from basics to clinical practice: Part II. Understanding parameters for acne treatment with photodynamic therapy. J Am Acad Dermatol. 2010;63(2):195–211. doi: 10.1016/j.jaad.2009.09.057. [DOI] [PubMed] [Google Scholar]
- 17.Karsai S, Czarnecka A, Junger M, Raulin C. Ablative fractional lasers (CO(2) and Er:YAG): A randomized controlled double-blind split-face trial of the treatment of peri-orbital rhytides. Lasers Surg Med. 2010;42(2):160–167. doi: 10.1002/lsm.20879. [DOI] [PubMed] [Google Scholar]
- 18.Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: Nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol. 2008;58(5):719–737. doi: 10.1016/j.jaad.2008.01.003. quiz 738–740. [DOI] [PubMed] [Google Scholar]
- 19.Hu S, Hsiao WC, Chen MC, Huang YL, Chang SL, Shih PY, Gold MH. Ablative fractional erbium-doped yttrium aluminum garnet laser with coagulation mode for the treatment of atrophic acne scars in Asian skin. Dermatol Surg. 2011;37(7):939–944. doi: 10.1111/j.1524-4725.2011.02009.x. [DOI] [PubMed] [Google Scholar]
- 20.Cho SB, Lee SJ, Kang JM, Kim YK, Chung WS, Oh SH. The efficacy and safety of 10,600-nm carbon dioxide fractional laser for acne scars in Asian patients. Dermatol Surg. 2009;35(12):1955–1961. doi: 10.1111/j.1524-4725.2009.01316.x. [DOI] [PubMed] [Google Scholar]
- 21.Manuskiatti W, Triwongwaranat D, Varothai S, Eimpunth S, Wanitphakdeedecha R. Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol. 2010;63(2):274–283. doi: 10.1016/j.jaad.2009.08.051. [DOI] [PubMed] [Google Scholar]
- 22.Waibel J, Wulkan AJ, Lupo M, Beer K, Anderson RR. Treatment of burn scars with the 1,550 nm nonablative fractional erbium laser. Lasers Surg Med. 2012;44(6):441–446. doi: 10.1002/lsm.22038. [DOI] [PubMed] [Google Scholar]
- 23.Ozog DM, Moy RL. A randomized split-scar study of intraoperative treatment of surgical wound edges to minimize scarring. Arch Dermatol. 2011;147(9):1108–1110. doi: 10.1001/archdermatol.2011.248. [DOI] [PubMed] [Google Scholar]
- 24.Kim SG, Kim EY, Kim YJ, Lee SI. The efficacy and safety of ablative fractional resurfacing using a 2,940-Nm Er:YAG laser for traumatic scars in the early posttraumatic period. Arch Plast Surg. 2012;39(3):232–237. doi: 10.5999/aps.2012.39.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Webber J, Luo Y, Crilly R, Fromm D, Kessel D. An apoptotic response to photodynamic therapy with endogenous protoporphyrin in vivo. J Photochem Photobiol B. 1996;35(3):209–211. doi: 10.1016/s1011-1344(96)07291-0. [DOI] [PubMed] [Google Scholar]
- 26.Ruiz-Esparza J, Lupton JR. Laser resurfacing of darkly pigmented patients. Dermatol Clin. 2002;20(1):113–121. doi: 10.1016/s0733-8635(03)00050-0. [DOI] [PubMed] [Google Scholar]
- 27.Nanni CA, Alster TS. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg. 1998;24(3):315–320. doi: 10.1111/j.1524-4725.1998.tb04161.x. [DOI] [PubMed] [Google Scholar]
- 28.Sriprachya-anunt S, Marchell NL, Fitzpatrick RE, Goldman MP, Rostan EF. Facial resurfacing in patients with Fitzpatrick skin type IV. Lasers Surg Med. 2002;30(2):86–92. doi: 10.1002/lsm.10012. [DOI] [PubMed] [Google Scholar]