Abstract
Women experiencing severe perinatal mental illness during pregnancy or postpartum have unique needs when psychiatric hospitalization is indicated. Although many countries have established mother-baby psychiatric units, similar facilities have not been available in the US. In 2011, the University of North Carolina at Chapel Hill inaugurated the first Perinatal Psychiatry Inpatient Unit (PPIU) in the US. We describe the unique characteristics of the patient population and report clinical outcomes guiding development and refinement of treatment protocols. Ninety-two perinatal patients were admitted between September 2011 and September 2012, and 91 completed self-report measures at admission and discharge. Perinatal unipolar mood disorder was the most frequent primary diagnosis (60.43%), and eleven patients (12%) were admitted with psychosis. The data document clinically and statistically significant improvements in symptoms of depression, anxiety and active suicidal ideation between admission and discharge (p < .0001), as assessed by the Edinburgh Postnatal Depression Scale, Patient Health Questionnaire, and Generalized Anxiety Disorder Scale. Overall functioning was also improved, demonstrated by a significant mean difference of −10.96 in total scores of the Work and Social Adjustment Scale (p < 0.0001). Data suggest that delivering specialized and targeted interventions for severe maternal mental illness in a safe and supportive setting produces positive patient outcomes.
Introduction
Perinatal depression (PND) is a commonly occurring mood disorder during pregnancy and postpartum affecting 10-15% of women and, when untreated, poses significant morbidity to the patient and her family. Although most cases of PND can be effectively managed in outpatient settings, a significant number of women have severe disease requiring psychiatric hospitalization for safety and stabilization. Moreover, although rare, postpartum psychosis (PP) is a severe form of a postpartum mood disorder with rapid onset of symptoms within the first days to weeks postpartum and is characterized by delusions, hallucinations, and bizarre behavior(Doucet, Jones et al. 2011). PP has a prevalence of 0.1% but can have disastrous consequences including maternal suicide and infanticide and usually requires immediate and aggressive inpatient psychiatric treatment(Sit, Rothschild et al. 2006; Blackmore, Rubinow et al. 2013).
Specialized psychiatric mother-baby units (MBU’s) were first developed in the United Kingdom approximately 50 years ago and are now also found in France, Belgium, Germany, The Netherlands, Australia, New Zealand and other parts of Europe(Bardon, Glaser et al. 1968; Isserlis C 1980; Kumar, Marks et al. 1995; Oates 1996; Howard 2000). Inpatient MBU treatment formulation addresses mental illness within the context of maternal functioning and with particular attention to maternal-infant attachment. The European model also has a strong focus on preserving the mother’s role within the family (i.e. meal preparation and/or childcare) as part of inpatient programming. To date, the literature on the efficacy of such MBUs demonstrates good treatment response and mother-infant outcomes in these intensive long-term settings, suggesting the importance of offering this type of specialized care(Stewart 1989; Milgrom, Burrows et al. 1998; Buist, Minto et al. 2004; Cazas and Glangeaud-Freudenthal 2004; Salmon, Abel et al. 2004; Wilson, Bobier et al. 2004; Nair, Bilszta et al. 2010).
Despite the widespread implementation of MBU’s in other countries over the past 50 years, distinct differences between the US health care system and those systems abroad have prevented a similar movement in the US. First, while international mother-baby inpatient units admit infants along with their mothers during treatment, the current US health system does not support the necessary neonatal/pediatric resources that would allow infants to remain on the unit with their mothers 24 hours a day. Second, the overall length of stay (LOS) characterizing US psychiatric hospital admissions is steadily decreasing(Blader 2011). In contrast, in Australia, the average length of stay at an MBU is greater than three weeks(Buist, Minto et al. 2004), a minimum of 14 days longer than most US psychiatric inpatient hospital admissions(Blader 2011). To our knowledge, there have been no published comparisons between the specialized MBUs and hospitalization in a general adult psychiatric unit.
In the US, the clinical need for the development of specialized outpatient perinatal psychiatry programs has produced an increasing demand from both patients and health care providers for specialized inpatient psychiatric care for women with severe mental illness during pregnancy and the postpartum. The first step toward offering such specialized care for perinatal women in the US occurred in 2000, when Brown University began a psychiatric mother-baby day-hospital program(Howard, Battle et al. 2006). In 2008, the University of North Carolina at Chapel Hill (UNC-CH) Neuroscience Hospital piloted a perinatal psychiatry inpatient unit, sharing space with the geriatric psychiatric inpatient unit(Bullard, Meltzer-Brody et al. 2009). However, patient satisfaction comments from 2008-2010 stated discomfort and dislike with the shared space, particularly because of visiting restrictions for babies and small children that impose separation of the mother and baby. Consequently, due to the ever-growing number of referrals to the perinatal psychiatry program and increasing demand from patients and providers, in 2011 this shared space was converted into a new free-standing Perinatal Psychiatry Inpatient Unit (PPIU). Our hope was that, although the service was not identical to the MBUs abroad, we would be able to provide excellent and efficacious patient care in a shorter LOS.
The facilities of the new PPIU include five patient beds (three private and two semi-private), a large day/group treatment room, and a nurse’s station. Although normal hospital hours are extended in the PPIU (8am to 8pm) to encourage infants to remain on the unit as long as possible, no infants (or other family members) are allowed to stay overnight. Unique features of the PPIU include gliders in patient rooms for nursing/feeding, hospital grade breast pumps, refrigeration and freezer storage for breastmilk, group therapies including art, relaxation, behavioral, and Mindfulness-Based Cognitive Therapy, M-wave biofeedback therapy, mother-infant attachment therapy, family and Partner-Assisted Interpersonal Psychotherapy, therapeutic yoga, spiritual support, and full discharge planning for transitioning patients to appropriate community outpatient services. The multidisciplinary staff include nurses cross-trained in obstetrics and psychiatry, lactation consultants, chaplain, recreational and occupational therapists, certified yoga instructor, psychologists, psychiatrists, and a social worker.
Our specific aims for this report are to: (1) Prospectively assess the severity of perinatal psychiatric illness and other comorbid psychiatric symptoms in pregnant or postpartum women admitted to the UNC-CH PPIU at two time points, within 24 hours of admission to the unit and within 24 hours of discharge; (2) Examine additional variables (such as marital status, insurance status, number of children at home, adverse life experiences and functional impairment) that might associate with or predict course or outcome; and (3) report the average LOS, comparing to average LOS reported in the literature for MBUs elsewhere. We hypothesized that a greater number of adverse events and poorer work and social functioning would be associated with increased severity of psychiatric symptoms at admission and decreased response to treatment.
Materials and Methods
We collected self-report survey data at two time points (within 24 hours of inpatient admission and within 24 hours of discharge) from women admitted to the UNC-CH Perinatal Psychiatry Inpatient Unit (PPIU) between September 2011 and September 2012. Eligible subjects were all English-literate women admitted to the PPIU with psychiatric illness during pregnancy or postpartum. One woman refused to complete the surveys both at admission and discharge, and is therefore not included. At admission, approximately 80 women were able to provide self-report data, and all 91 women completed the discharge measures. Between 58 and 65 women completed measures at both time points (not all women completed all scales). While not ideal, these data reflect the challenges to collecting data from individuals with serious mental illness in an active hospital inpatient unit. A few women were too psychotic to complete the measures at admission but able to do so at discharge.
The survey data is part of routine clinical care on the PPIU and as such, it is part of a de-identified clinical database. The UNC Institutional Review Board Committee for the Protection of Human Subjects approved data collection and analysis of the de-identified patient data.
Measures
The Edinburgh Postnatal Depression Scale (EPDS) was developed specifically as a screening tool for postpartum depression(Cox, Holden et al. 1987) but has been validated and highly utilized during the entire perinatal period, including pregnancy(Gaynes, Gavin et al. 2005). It inquires about the common neurovegetative symptoms of depression, excluding somatic symptoms such as fatigue and changes in appetite that occur naturally in pregnancy and would not discriminate depressed women from non-depressed women. The reported split-half reliability of the EPDS was .88 and the standardized Cronbach’s coefficient was 0.87(Cox, Holden et al. 1987). Total scores on this 10-item, multiple-choice scale range from 0-30, with higher scores reflective of greater symptom severity.
The Patient Health Questionnaire-9 (PHQ-9) item form is one of the most commonly utilized screening instruments for depressive symptoms in a wide variety of clinical populations, including obstetric patients(Spitzer, Williams et al. 2000; Kroenke, Spitzer et al. 2001). Nine items are based upon the DSM-IV criteria for Major Depressive Disorder (MDD). In obstetric patients, the instrument was found to have a sensitivity of 73% and specificity of 98% compared to a structured psychiatric interview diagnosis of MDD. Total scores of the nine items range from 0 (no symptoms) to 27 (severe depression), and a tenth item inquires about the difficulty the symptoms may have posed for the patient in functionality(Spitzer, Williams et al. 2000).
The Work and Social Adjustment Scale (WSAS) is a five-item self-report scale that assesses functional impairment associated with a specific problem (e.g., depression)(Mundt, Marks et al. 2002). Responses on the scale range from 0-8 with 0 indicating no impairment and 8 indicating very severe impairment, yielding possible scores between 0 and 40. Questions ask about functioning at work, home, social activities, leisure activities, and close relationships. Reliability and validity data are available for patients with depressive disorders. Internal consistency for the WSAS is reported as Cronbach’s between .79 and .94. The scale has been found to highly correlated with symptom severity(Mundt, Marks et al. 2002).
The Adverse Childhood Experiences (ACE) questionnaire was developed in 1998 by a group of researchers for a large health maintenance organization(Felitti, Anda et al. 1998). Respondents answer “yes” or “no” to ten items on the scale, with “yes” answers carrying a value of one, for a possible range of 0-10 (higher scores indicating more childhood trauma). Items were drawn from existing scales to define psychological and physical abuse, violence against the respondent’s mother, sexual abuse, and alcohol or drug abuse during childhood(Wyatt 1985; Statistics 1991). All questions are prefaced by the phrase, “While you were growing up during your first 18 years of life...”
The Generalized Anxiety Disorder scale (GAD-7) is a brief, seven-item screening tool to assess the presence of Generalized Anxiety Disorder (GAD) in primary care populations(Spitzer, Kroenke et al. 2006; Swinson 2006). Respondents are asked to indicate to what extent over the last two weeks they have felt bothered by their symptoms: not at all (0), several days (1), more than half the days (2), or nearly every day (3). At the cut-off score of 10, reported sensitivity is 89% and specificity is 82% at identifying true cases of GAD. Thresholds for levels of severity are 0-4 “minimal,” 5-9 “mild,” 10-14 “moderate,” and 15-21 “severe.”
We also examined patient satisfaction ratings with the hospital service. All UNC Hospital patients are invited to rate satisfaction on hospital quality utilizing the Press Ganey report and these scores are then tabulated by unit (LLC 2008). Although these hospital-collected data cannot be linked with the data collected by our team, they do provide an overall measure of satisfaction of inpatient service. The Press Ganey report inquires about patient satisfaction with multiple facets of nursing and physician care such as the promptness of responding to patient needs, communication of the team with patient about treatment plan, general helpfulness of all team members, and perceived quality of care.
Statistical Methods
Analyses were conducted using JMP 9.0 statistical software (SAS, Cary, NC). In our sample of women, we performed descriptive statistics that included percent tabulations for categorical variables, means with standard deviations for continuous variables, and medians with ranges where more appropriate. On patients who provided data at both admission and discharge, our primary outcome measures were the symptoms changes (depression and anxiety) and the patient’s perception of functional status from admission until discharge from the inpatient unit, reported by nonparametric correlation coefficients and/or paired t-test analyses. Bivariate analyses were conducted using Chi-square statistics for categorical variables. The statistical significance level was set at p < .05 and there were no corrections for multiple comparisons.
Results
Demographic Characteristics
Table 1 describes the demographic characteristics for our study cohort of ninety-one perinatal patients (38 pregnant and 55 postpartum; two women were both pregnant and postpartum), admitted between September 2011 and September 2012 to the UNC Neurosciences Hospital Perinatal Psychiatric Unit for a mean length of stay (LOS) of 6.93 days (sd = 4.10). Patients averaged 28.81 years of age (sd = 6.12) and were racially diverse (54.95% White, 31.87% African American, 13.64% Hispanic, and 12.09% Other; some endorsed both Hispanic and non-White). More than half were married (53.85%) and almost half were privately insured (49.45%). Patients reported a mean of 3.42 (sd = 2.44) adverse childhood experiences (ACE). Among the adverse experiences reported by our cohort on the ACE, 47% endorsed emotional abuse, 46% reported sexual abuse, 25% reported physical abuse, and 44% reported someone in the childhood home abused alcohol or illicit drugs. With regard to obstetric history, 25% were primiparous; multiparous women reported a median of 2 pregnancies (range = 1 to 14) and one child at home (median, range = 0 to 6).
Table 1. Demographic Variables (n = 91 unless noted).
| Variable | Statistic |
|---|---|
|
| |
| Mean Age (yrs) | 28.81 (sd = 6.12) |
|
| |
| Mean Length Of Stay | 6.93 days (sd = 4.10) |
|
| |
| Race* | % (n) |
| Caucasian | 54.95 (50) |
| African American | 31.87 (29) |
| Hispanic | 13.64 (12) |
| Asian American | 0.01 (1) |
| Other | 10.99 (10) |
|
| |
| Marital Status | |
| Married | 53.85 (49) |
| Co-habiting | 13.19 (12) |
| Single | 25.27 (23) |
| Divorced/Separated | 0.07 (6) |
| Widowed | 0.01 (1) |
|
| |
| Payer Status | |
| Private Insurance | 49.45 (45) |
| No Insurance | 0.09 (9) |
| Medicaid | 39.56 (36) |
|
| |
| Obstetrical Status at time of admission** | |
| Pregnant | 41.76 (38) |
| Postpartum | 60.44 (55) |
|
| |
| Weeks Pregnant (median) | 20 (range 4-40) |
|
| |
| Weeks Postpartum (median) | 16 (range 1-72) |
|
| |
| Parity (n = 76) | |
| Primaparous | 25.00 (19) |
| Multiparous ≤ 4 | 46.05 (35) |
| Multiparous > 4 | 28.95 (22) |
|
| |
| Children at home (n = 90) | |
| None | 11.11 (10) |
| One | 46.66 (42) |
| Two | 23.33 (21) |
| Three or more | 18.89 (17) |
|
| |
| Mean Number of Adverse Life Experiences (n = 80) |
3.42 (sd = 2.44) |
|
| |
| Types of Adverse Experiences | |
| Emotional abuse | 46.25 (37) |
| Sexual abuse | 45.00 (36) |
| Physical abuse | 27.50 (22) |
| Mother/step-mother of patient abused | 23.75 (19) |
| Alcohol or substance abuse in home | 42.50 (34) |
Some women endorsed Hispanic as race and another category as ethnicity.
One woman was both pregnant and postpartum
Primary Psychiatric Diagnosis and Comorbidity
Unipolar mood disorder without psychosis was the most frequent primary discharge diagnosis (60.43%; n = 55), six patients had a diagnosis of bipolar disorder (6.59%), and 11 patients (12.09%) had a psychotic disorder of some kind. Nearly half of the cohort bore diagnoses of comorbid psychiatric illness(es) (40.65%); of the 37 patients receiving a second diagnosis, anxiety disorders were the most represented (40.54%). According to responses on item 10 of the EPDS inquiring about suicidal ideation, 86.49% (64/74) endorsed thoughts of self-harm. Table 2 depicts the diversity of discharge psychiatric diagnoses of our patients.
Table 2. Primary Psychiatric Diagnosis at Discharge and Comorbidity.
| Psychiatric Diagnosis at Discharge | % (n = 91) |
|---|---|
|
| |
| Unipolar Depression without psychosis | 60.43% (55) |
|
| |
| Major Depression with Psychosis | 5.50% (5) |
|
| |
| Mood Disorder NOS | 8.79% (8) |
|
| |
| Bipolar Disorder | 6.59% (6) |
|
| |
| Schizophrenia/Schizoaffective/Psychotic Disorder NOS | 6.59% (6) |
|
| |
| Anxiety Disorder | 7.69% (7) |
|
| |
| Substance Induced Mood Disorder | 4.40% (4) |
|
| |
| Types of Comorbid Psychiatric Illness | |
|
| |
| Anxiety Disorder NOS | 13.19 (12) |
| PTSD | 4.40 (4) |
| OCD | 2.10 (2) |
| GAD | 2.10 (2) |
|
| |
| Primary Comorbid Psychiatric Diagnosis Made | 40.65% (54) |
|
| |
| Report of Suicidal Ideation on Admission Assessment * | 86.49% (64) |
Item 10 of the EPDS Scale
Symptomatic Change
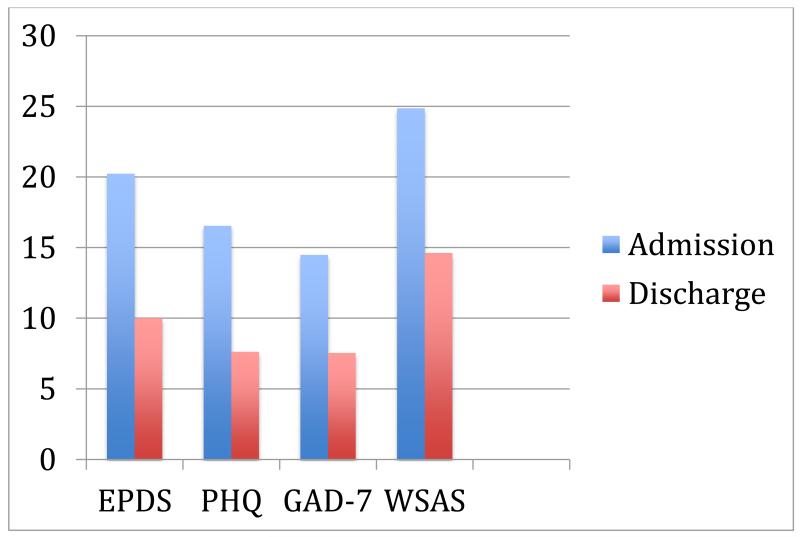
Capturing questionnaires at admission and discharge was challenging due to unexpected discharge and limited time from discharge decision to patient departure. Nevertheless, we captured information at both time points from about two thirds of the cohort, demonstrated in Figure 1. There were significant reductions in symptoms of depression between the time of admission and the day of discharge; the mean score of the EPDS at admission was 20.23 (n= 73, sd = 5.57) and at discharge was 10.00 (n = 76, sd = 5.50). The mean difference of EPDS sum scores (−10.29) calculated by a dependent t-test was significant at p < 0.0001 (n = 65, t-ratio = −12.53, CI = −11.93 to −8.65). Results from the PHQ-9 were similar, with the mean score at admission 16.54 (n = 69, sd = 7.43) and 7.62 (n = 69, sd = 5.79) at discharge, a mean difference of −9.47 (n = 58, mean difference = −9.47, t-ratio = −9.47, CI = −11.48 to −7.47, p < 0.0001). Anxiety reported on the GAD-7 also experienced significant change. On admission, the mean sum score of the GAD-7 was 14.48 (n = 77, sd = 5.52) compared to a mean sum score of 7.54 at discharge (n = 75, sd = 5.15), a significant mean difference of −7.69 (n = 63, t-ratio = −9.58, CI = −9.29 to −6.08, p < 0.0001). Patients also reported that their overall functioning was improved; the mean sum score of the WSAS at admission was 24.86 (n = 76, sd = 10.73) and 14.62 (n = 7, sd = 11.88) at discharge, a significant mean difference of −10.96 (n = 62, t-ratio = −7.28, CI = −13.96 to −7.95, p < 0.0001).
Figure 1. Change Scores by Assessment Instrument.
All significant at p < .0001
Relation between Adverse Childhood Experiences and Symptoms
We examined the relation between symptom status at admission and discharge with the measure of adverse childhood events (ACE), but nonparametric correlation coefficients between the EPDS, PHQ-9, or GAD-7 and the ACE did not reach significance (EPDS r = 0.13, p = 0.28; PHQ-9 r = 0.16, p = 0.20; GAD-7 r = 0.15, p = 0.19).
Relation between Number of Children and Symptoms
The relation between the number of children and maternal symptoms at time of admission was assessed. Women admitted to the unit with more than one child reported significantly greater levels of depression as measured by the EPDS and anxiety symptoms as measured by the GAD-7 compared to the primiparous mothers (p < .0001).
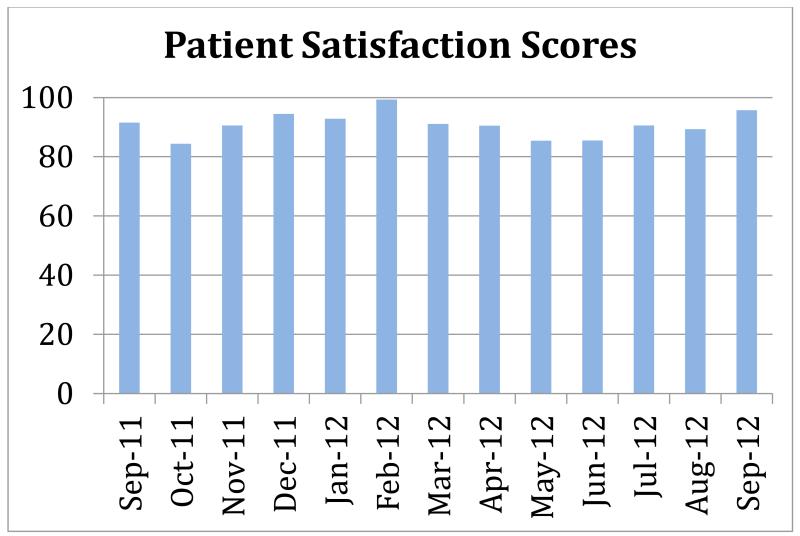
Patient Service Satisfaction on the PPIU
We were also interested in hospital-collected Press Ganey data regarding inpatient experience and perception of care on the PPIU. Patients on the PPIU rated the unit highly with a mean score of 91.9% (depicted in Figure 2) that ranks in the top tier of all units across UNC Hospitals.
Figure 2. Press Ganey Patient Service Satisfaction Scores on the PPIU.
Discussion
The study cohort is comprised of women admitted during the first year of a new specialized inpatient perinatal psychiatry unit (PPIU) for acute stabilization and treatment of severe perinatal mental illness. Most of the women admitted to the PPIU presented with a primary diagnosis of a mood disorder and, consistent with the international literature on the primary psychiatric diagnosis indicating hospitalization(Nair, Bilszta et al. 2010), approximately 12% presented with psychotic symptoms. The EPDS scores at the time of admission indicated severe symptomatology, with the vast majority of the women endorsing active thoughts and intent of self-harm.
This cohort also represents a racially and socioeconomically diverse population of perinatal women. History of childhood trauma was high, with the mean number of adverse childhood experiences greater than three, and emotional, sexual, and physical abuse being the most commonly reported traumatic events. This is consistent with previous literature documenting high rates of abuse and trauma in women with perinatal depression (Ansara, Cohen et al. 2005; Kendall-Tackett 2007; Onoye, Goebert et al. 2009; Silverman and Loudon 2010; Meltzer-Brody, Bledsoe-Mansori et al. 2013) and is likely a risk factor for the degree of symptom severity observed in women requiring inpatient psychiatric hospitalization for perinatal mental illness.
Based upon these findings and those from MBUs abroad, specialized and targeted interventions appear appropriate for mental illness during the perinatal period. In our cohort, the response to treatment was robust as evidenced by statistically and clinically significant reductions in symptom severity and improvement in functioning across all domains including mood, anxiety, and social adjustment and functioning. Ratings of depressive symptoms dropped over 10 points from time of admission to discharge, and ratings of anxiety symptoms dropped almost 8 points, reflecting rapid stabilization and decreased distress over a relatively short period of time, particularly in comparison with the longer LOS reported in international MBUs. This is consistent with the treatment efficacy observed in specialized perinatal psychiatric units across the world and suggests that this is an important and feasible treatment option in the United States (Milgrom, Burrows et al. 1998; Buist, Minto et al. 2004; Salmon, Abel et al. 2004), Moreover, the patient reports of satisfaction with the PPIU were very high (mean=91.9%) as assessed by the Press Ganey surveys over the course of the first year of operation of the PPIU. Patient perception of their care and satisfaction with the PPIU are also meaningful measures of the success of the program.
Due to the relatively short length of stay (LOS) that characterizes inpatient psychiatry units in general in the United States, and consistent with the approximately seven day LOS of this PPIU cohort, programming was developed with a strong focus on teaching skills and tools to manage anxiety and distress post-discharge(Hendrick, Altshuler et al. 2000; Bernstein, Rush et al. 2008; Paul, Downs et al. 2013). Heart-rate variability biofeedback (HRVB) therapy, an effective tool for demonstrating to the patient the physiological effects of anxiety (Karavidas, Lehrer et al. 2007), has been particularly effective as patients see first-hand how relaxation training, diaphragmatic breathing, and mindfulness techniques combat their distress (Beckham, Greene et al. 2013). Individual psychotherapy sessions allow one-to-one targeting of triggers for symptoms and planning for the unique post-discharge challenges each woman will address. A nurse/certified instructor teaches Yoga classes twice a week, and videos are available for patients to extend yoga to other days as well (Battle, Uebelacker et al. 2010; Beddoe, Lee et al. 2010; Babbar, Parks-Savage et al. 2012). Psychotherapy groups two afternoons a week are formatted to include interventions from Mindfulness-Based Cognitive Therapy(Bach and Hayes 2002; Hayes, Luoma et al. 2006; Dimidjian and Davis 2009) and Acceptance and Commitment Therapy(Bach and Hayes 2002; Hayes, Luoma et al. 2006), and art/expressive therapies extend to three other afternoons(Oster, Svensk et al. 2006; Hughes and da Silva 2011) (Hughes and da Silva 2011; Oster et al. 2006). Mothers and infants attend an attachment group, led by a psychologist trained in parent-infant psychotherapy, and a specific group for partners and caregivers is held Wednesday evenings, modeled after Partner-Assisted Interpersonal Psychotherapy(Brandon, Ceccotti et al. 2012).
While the data from the first year of operations are promising, there are limitations to this report. Data were collected from a single PPIU within a university-based hospital system in the US and so may not generalize to a different setting. The sample size of 91 subjects is modest, and we do not have long-term follow-up data on the patients discharged from the unit to assess ongoing treatment response and longitudinal course of illness. Additionally, as is typical in the US healthcare system, infants are not able to room-in on the unit overnight which could potentially impact attachment with the mother.
Summary
The UNC-CH PPIU provides psychiatric care in a safe and supportive setting to pregnant and postpartum women requiring the intensity of a psychiatric hospitalization. The PPIU is the first such inpatient facility in the US and, while modeled after MBU’s located around the world, it was adapted to be compatible with the US health care system. Although infants are not able to stay overnight on the unit, they do spend significant time on the PPIU and care is taken to foster mother-infant attachment and provide treatment of the mother-infant dyad and family. The specialized and targeted interventions appropriate for the perinatal period are aimed at treating anxiety and depression and more severe psychiatric symptoms such as psychosis, in order to help the mother recover. Patient outcomes measured by pre- and post-treatment assessment instruments over the first year of operation of the PPIU demonstrated clinically and statistically significant symptom improvement across all domains, and patient service satisfaction was high.
Future work aims to address the transition from intensive inpatient treatment to the outpatient setting. We will focus on continuing mother-infant attachment therapies and other treatment modalities in a step-wise and evaluative process to ensure the therapies initiated on the PPIU are continued in the outpatient setting. Although patients from our community often move from inpatient treatment to follow-up outpatient care in our Women’s Mood Disorders clinics, a number of patients from outside the region may not have access to the same specialized care. Promising advances in Telehealth and web-based therapies or resources may in the future inform discharge plans.
Acknowledgements
The authors acknowledge support from NIMH (K23MH085165 to SMB and K23MH085007 to AB).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Ansara D, Cohen MM, et al. Predictors of women’s physical health problems after childbirth. J Psychosom Obstet Gynaecol. 2005;26(2):115–125. doi: 10.1080/01443610400023064. [DOI] [PubMed] [Google Scholar]
- Babbar S, Parks-Savage AC, et al. Yoga during pregnancy: a review. American journal of perinatology. 2012;29(6):459–464. doi: 10.1055/s-0032-1304828. [DOI] [PubMed] [Google Scholar]
- Bach P, Hayes SC. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: a randomized controlled trial. Journal of consulting and clinical psychology. 2002;70(5):1129–1139. doi: 10.1037//0022-006x.70.5.1129. [DOI] [PubMed] [Google Scholar]
- Bardon D, Glaser YI, et al. Mother and baby unit: psychiatric survey of 115 cases. British medical journal. 1968;2(5607):755–758. doi: 10.1136/bmj.2.5607.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battle CL, Uebelacker LA, et al. Prenatal yoga and depression during pregnancy. Birth. 2010;37(4):353–354. doi: 10.1111/j.1523-536X.2010.00435_1.x. [DOI] [PubMed] [Google Scholar]
- Beckham AJ, Greene TB, et al. A pilot study of heart rate variability biofeedback therapy in the treatment of perinatal depression on a specialized perinatal psychiatry inpatient unit. Archives of women’s mental health. 2013;16(1):59–65. doi: 10.1007/s00737-012-0318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beddoe AE, Lee KA, et al. Effects of mindful yoga on sleep in pregnant women: a pilot study. Biological research for nursing. 2010;11(4):363–370. doi: 10.1177/1099800409356320. [DOI] [PubMed] [Google Scholar]
- Bernstein IH, Rush AJ, et al. Symptom features of postpartum depression: are they distinct? Depression and anxiety. 2008;25(1):20–26. doi: 10.1002/da.20276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackmore ER, Rubinow DR, et al. Reproductive outcomes and risk of subsequent illness in women diagnosed with postpartum psychosis. Bipolar disorders. 2013 doi: 10.1111/bdi.12071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blader JC. Acute inpatient care for psychiatric disorders in the United States, 1996 through 2007. Archives of general psychiatry. 2011;68(12):1276–1283. doi: 10.1001/archgenpsychiatry.2011.84. [DOI] [PubMed] [Google Scholar]
- Brandon AR, Ceccotti N, et al. Proof of concept: Partner-Assisted Interpersonal Psychotherapy for perinatal depression. Archives of women’s mental health. 2012;15(6):469–480. doi: 10.1007/s00737-012-0311-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buist A, Minto B, et al. Mother-baby psychiatric units in Australia - the Victorian experience. Archives of women’s mental health. 2004;7(1):81–87. doi: 10.1007/s00737-003-0040-6. [DOI] [PubMed] [Google Scholar]
- Bullard ES, Meltzer-Brody S, et al. The need for comprehensive psychiatric perinatal care-the University of North Carolina at Chapel Hill, Department of Psychiatry, Center for Women’s Mood Disorders launches the first dedicated Inpatient Program in the United States. Am J Obstet Gynecol. 2009;201(5):e10–11. doi: 10.1016/j.ajog.2009.05.004. author reply e11. [DOI] [PubMed] [Google Scholar]
- Cazas O, Glangeaud-Freudenthal NM. The history of Mother-Baby Units (MBUs) in France and Belgium and of the French version of the Marce checklist. Archives of women’s mental health. 2004;7(1):53–58. doi: 10.1007/s00737-003-0046-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM, et al. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British journal of psychiatry: the journal of mental science. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Davis KJ. Newer variations of cognitive-behavioral therapy: behavioral activation and mindfulness-based cognitive therapy. Current psychiatry reports. 2009;11(6):453–458. doi: 10.1007/s11920-009-0069-y. [DOI] [PubMed] [Google Scholar]
- Doucet S, Jones I, et al. Interventions for the prevention and treatment of postpartum psychosis: a systematic review. Archives of women’s mental health. 2011;14(2):89–98. doi: 10.1007/s00737-010-0199-6. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evidence report/technology assessment (Summary) 2005;119:1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, et al. Acceptance and commitment therapy: model, processes and outcomes. Behaviour research and therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hendrick V, Altshuler L, et al. Postpartum and nonpostpartum depression: differences in presentation and response to pharmacologic treatment. Depression and anxiety. 2000;11(2):66–72. doi: 10.1002/(sici)1520-6394(2000)11:2<66::aid-da3>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Howard LM. The separation of mothers and babies in the treatment of postpartum psychotic disorders in Britain 1900-1960. Archives of Womens Mental Health. 2000;3:1–5. [Google Scholar]
- Howard M, Battle CL, et al. A psychiatric mother-baby day hospital for pregnant and postpartum women. Archives of women’s mental health. 2006;9(4):213–218. doi: 10.1007/s00737-006-0135-y. [DOI] [PubMed] [Google Scholar]
- Hughes EG, da Silva AM. A pilot study assessing art therapy as a mental health intervention for subfertile women. Human reproduction. 2011;26(3):611–615. doi: 10.1093/humrep/deq385. [DOI] [PubMed] [Google Scholar]
- Isserlis C VM, Dingli D. Hospitalization Mere-Enfant. Ann Med Psychology. 1980;138:935–992. [PubMed] [Google Scholar]
- Karavidas MK, Lehrer PM, et al. Preliminary results of an open label study of heart rate variability biofeedback for the treatment of major depression. Applied psychophysiology and biofeedback. 2007;32(1):19–30. doi: 10.1007/s10484-006-9029-z. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett KA. Violence against women and the perinatal period: the impact of lifetime violence and abuse on pregnancy, postpartum, and breastfeeding. Trauma Violence Abuse. 2007;8(3):344–353. doi: 10.1177/1524838007304406. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, et al. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R, Marks M, et al. Clinical survey of a psychiatric mother and baby unit: characteristics of 100 consecutive admissions. Journal of affective disorders. 1995;33(1):11–22. doi: 10.1016/0165-0327(94)00067-j. [DOI] [PubMed] [Google Scholar]
- LLC AM. Press Ganey: public reporting gives huge boost to patient satisfactoin. Healthcare benchmarks and quality improvement. 2008;15:121–123. [PubMed] [Google Scholar]
- Meltzer-Brody S, Bledsoe-Mansori SE, et al. A prospective study of perinatal depression and trauma history in pregnant minority adolescents. American journal of obstetrics and gynecology. 2013;208(3):211 e211–217. doi: 10.1016/j.ajog.2012.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milgrom J, Burrows GD, et al. Psychiatric illness in women: a review of the function of a specialist mother-baby unit. The Australian and New Zealand journal of psychiatry. 1998;32(5):680–686. doi: 10.3109/00048679809113123. [DOI] [PubMed] [Google Scholar]
- Mundt JC, Marks IM, et al. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. The British journal of psychiatry: the journal of mental science. 2002;180:461–464. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- Nair R, Bilszta J, et al. Review of patients admitted to a specialist inpatient parent-infant psychiatric service. Australasian psychiatry: bulletin of Royal Australian and New Zealand College of Psychiatrists. 2010;18(6):567–572. doi: 10.3109/10398562.2010.525641. [DOI] [PubMed] [Google Scholar]
- Oates M. Psychiatric services for women following child-birth. International Review of Psychiatry. 1996;8(1):87–98. [Google Scholar]
- Onoye JM, Goebert D, et al. PTSD and postpartum mental health in a sample of Caucasian, Asian, and Pacific Islander women. Arch Womens Ment Health. 2009;12(6):393–400. doi: 10.1007/s00737-009-0087-0. [DOI] [PubMed] [Google Scholar]
- Oster I, Svensk AC, et al. Art therapy improves coping resources: a randomized, controlled study among women with breast cancer. Palliative & supportive care. 2006;4(1):57–64. doi: 10.1017/s147895150606007x. [DOI] [PubMed] [Google Scholar]
- Paul IM, Downs DS, et al. Postpartum Anxiety and Maternal-Infant Health Outcomes. Pediatrics. 2013 doi: 10.1542/peds.2012-2147. [DOI] [PubMed] [Google Scholar]
- Salmon MP, Abel K, et al. A national audit of joint mother and baby admissions to UK psychiatric hospitals: an overview of findings. Archives of women’s mental health. 2004;7(1):65–70. doi: 10.1007/s00737-003-0042-4. [DOI] [PubMed] [Google Scholar]
- Silverman ME, Loudon H. Antenatal reports of pre-pregnancy abuse is associated with symptoms of depression in the postpartum period. Arch Womens Ment Health. 2010;13(5):411–415. doi: 10.1007/s00737-010-0161-7. [DOI] [PubMed] [Google Scholar]
- Sit D, Rothschild AJ, et al. A review of postpartum psychosis. Journal of women’s health. 2006;15(4):352–368. doi: 10.1089/jwh.2006.15.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of internal medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, et al. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. American journal of obstetrics and gynecology. 2000;183(3):759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- Statistics, N. C. f. H. Exposure to alcholism in the family: United States, 1988. Department of Health and Human Services; Washington DC: 1991. Advance Data, No. 205. [Google Scholar]
- Stewart DE. Psychiatric admission of mentally ill mothers with their infants. Canadian journal of psychiatry. Revue canadienne de psychiatrie. 1989;34(1):34–38. doi: 10.1177/070674378903400109. [DOI] [PubMed] [Google Scholar]
- Swinson RP. The GAD-7 scale was accurate for diagnosing generalised anxiety disorder. Evidence-based medicine. 2006;11(6):184. doi: 10.1136/ebm.11.6.184. [DOI] [PubMed] [Google Scholar]
- Wilson DA, Bobier C, et al. A perinatal psychiatric service audit in New Zealand: patient characteristics and outcomes. Archives of women’s mental health. 2004;7(1):71–79. doi: 10.1007/s00737-003-0043-3. [DOI] [PubMed] [Google Scholar]
- Wyatt GE. The sexual abuse of Afro-American and white-American women in childhood. Child abuse & neglect. 1985;9(4):507–519. doi: 10.1016/0145-2134(85)90060-2. [DOI] [PubMed] [Google Scholar]