TO THE EDITOR
Senescence is a state wherein cells are metabolically active but are unable to replicate due to the increased expression of cell cycle check point proteins, such as p16INK4A, that prevent passage of cells through the cycle. p16INK4A expression increases significantly in the basal layer of human epidermis and in dermal fibroblasts, making it a reliable in vivo biomarker of cellular aging in human skin (Krishnamurthy et al., 2004; Ressler et al., 2006; Waaijer et al., 2012). Moreover, p16INK4A has continued to gain strong support as an important component of the aging process (Sharpless, 2004; Campisi and d'Adda di Fagagna, 2007; Baker et al., 2011).
Using in vitro living skin equivalent (LSE) models constructed in-house (Aho et al., 2012) with epidermal keratinocytes (HEKs) from photo-protected sites of different age human donors, and a single neonatal fibroblast donor (Supplementary Information online), we demonstrate that the age of the keratinocyte donor differentially impacts the model's phenotype. Additionally, we have notably demonstrated that it is possible to develop an atrophic, aged model made from young (30–40 years) donor HEKs and to revert aged (53–66 years) donor HEK LSEs to a younger phenotype, by modulating the level of p16INK4A expression.
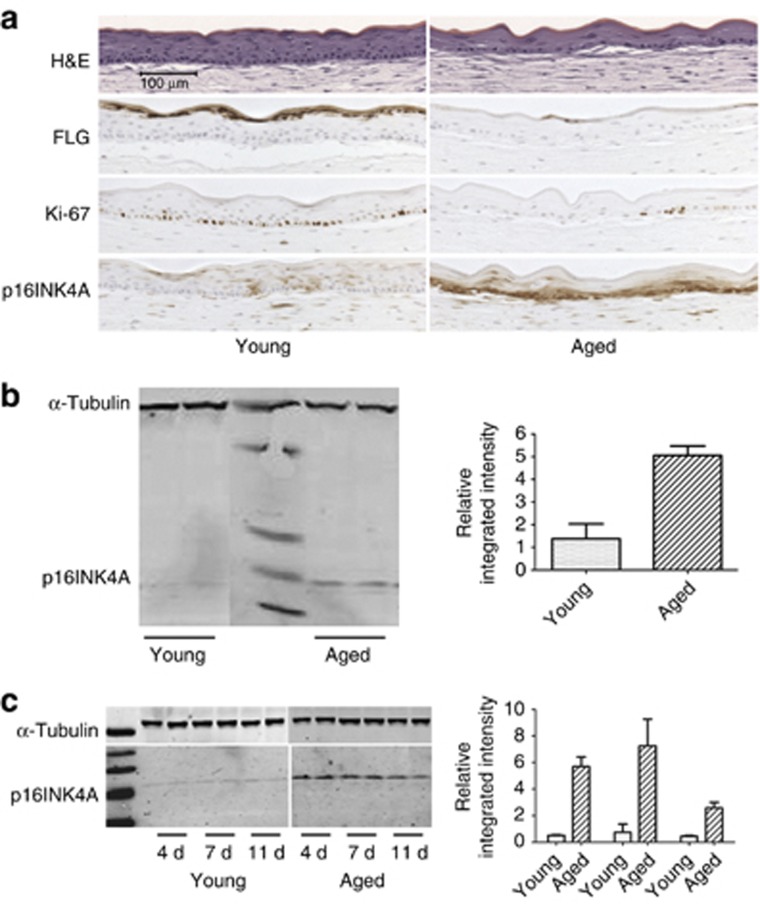
Similar to in vivo, we confirmed that the level of p16INK4A in the aged model increases in the basal cell layer and in the lower epidermis, supporting its usefulness as a biomarker for the aging phenotype. HEKs from two young donors formed normal stratified epidermis with a well-organized basal layer, distinct cell layers, and a normal pattern of differentiation (Figure 1a, left). Models using five different aged donor HEKs displayed an unorganized basal cell layer, fewer spinous and granular layers, and impaired differentiation, as reflected by decreased filaggrin immunostaining (Figure 1a, right). In this model, substantially fewer Ki-67 positive–stained cells were seen in the basal layer. This decrease is in agreement with the observations of Gilhar et al. (2004) in skin biopsies; however, others have seen either an increase (Giangreco et al., 2010) or no change (Ressler et al., 2006) in Ki-67 staining with age in vivo. This may be due to variations between donors or due to in vitro to in vivo differences.
Figure 1.
p16INK4A is associated with the aging epidermis. (a) Formalin-fixed, paraffin-embedded (FFPE) sections from young and aged donor keratinocyte living skin equivalent (LSE) models harvested at 7 days post air exposure. Sections were stained with hematoxylin and eosin or immunostained for detection of filaggrin (FLG), Ki-67, and p16INK4A. (b) Expression of p16INK4A protein from monolayer cell lysates (15 μg) harvested at the time of application to the LSE. (c) Representative immunoblot analysis for p16INK4A from young and aged LSE lysates (15 μg) from duplicate cultures harvested at three different time points post air exposure. Bar=100 μm, applies to all FFPE images.
We compared p16INK4A expression in LSEs made from young and aged donor cells by immunohistochemistry (IHC) and immunoblot, and the micrographs shown are representative of the donor strains tested. In the young donor LSEs, light staining of p16INK4A was observed throughout the epidermis and at a later time point, staining was specifically localized to the basal layer. In these samples, p16INK4A was barely detectable by immunoblot (Figure 1b and c). Conversely, we saw higher p16INK4A expression in the aged LSEs from an early time point and throughout the experiment. Strong staining was identified within the basal cell layer and in the lower stratum spinosum by IHC, substantiated by increased protein detected by immunoblot. This increase in p16INK4A appears to be inversely correlated with the decrease seen in markers of proliferation and differentiation, as first observed by Ressler et al. (2006).
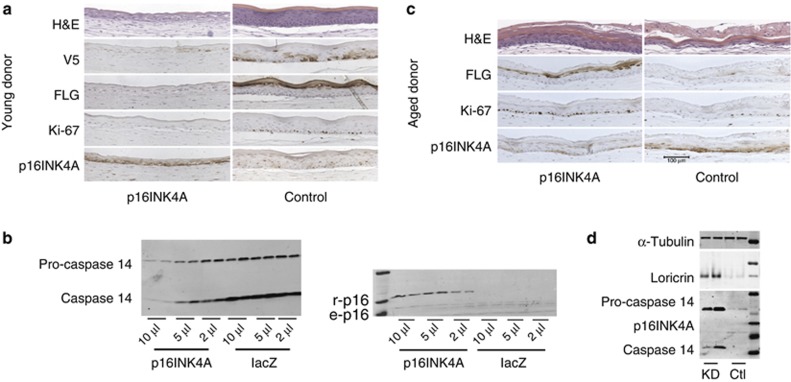
Next, we altered the expression of p16INK4A in LSEs produced from young donor HEKs by lentiviral expression of p16INK4A, driven by a truncated keratin 14 (K14) promoter (Di Nunzio et al., 2008) to target delivery to the physiologically relevant basal layer of epidermis. Here, we observed a dramatic difference in phenotype between LSEs overexpressing p16INK4A and the controls (Figure 2a). Cultures with increased p16INK4A expression showed significant atrophy, with a thinner viable epidermis and no apparent stratum corneum, analogous to the LSEs we had previously prepared from aged donor HEKs. We confirmed these findings with another young donor (not shown), and in both models we observed a phenotypic dose-dependent response, where the severity of atrophy was dependent on the level of p16 gene expression in the model (Figure 2b).
Figure 2.
Reversal of phenotype by targeting p16INK4A in the LSE. (a) Young donor keratinocyte living skin equivalents (LSEs) infected with K14 promoter driven either p16INK4A (left) or lacZ control (right) lentivirus, harvested at 11 days post air exposure. Formalin-fixed, paraffin-embedded (FFPE) sections were stained with hematoxylin and eosin (H&E) or immunostained for V5, filaggrin (FLG), Ki-67, or p16INK4A. (b) Immunoblot analysis for caspase-14 (6 μg, left) and for p16INK4A (25 μg, right, bottom). (c) Aged donor keratinocyte LSEs infected with either p16 miR (left) or non-silencing control miR (right) lentivirus, harvested 7 days post air exposure. FFPE sections were stained with H&E or immunostained for filaggrin (FLG), Ki-67, or p16INK4A. (d) LSE lysates (15 μg) were analyzed for p16INK4A and for the differentiation markers loricrin and caspase-14. r-p16, recombinant p16INK4A; e-p16, endogenous p16. Bar=100 μm.
In the young donor LSEs overexpressing p16INK4A, dose-dependent downregulation of Ki-67, filaggrin, and caspase-14 was observed as compared to the control samples. Moreover, increased levels of p16INK4A protein were detected by IHC in the p16INK4A-infected LSEs, with strong staining in the basal layer reflecting detection of both endogenous and recombinant protein. This was confirmed by the differential banding pattern seen by immunoblot. The lower amounts of Ki-67 staining when p16INK4A expression is high suggests that downregulation of proliferation is occurring. This decrease is likely a consequence of its increased inhibitory effects on CDK4/6 and the retinoblastoma pathway, resulting in cell cycle arrest (Ortega et al., 2002) and increased senescence (Alcorta et al., 1996). Unexpectedly, we observed that the level of endogenous p16INK4A expression appeared higher in the p16INK4A overexpression model. We speculate that the presence of recombinant p16INK4A protein might indirectly upregulate endogenous p16INK4A protein through various detrimental factors excreted from an increased number of senescent cells.
On the basis of these observations, we decided to explore the biological consequences of silencing p16INK4A in the aged donor LSE model. Here, we saw a dramatic improvement in the morphology of the aged donor LSE, which now resembled that of a much younger donor (Figure 2c and d). A striking difference between these LSEs and the atrophic, non–silenced controls was the substantial increase of Ki-67-positive cells in the p16INK4A-silenced cultures with a consequent normalization of terminal differentiation, as detected by the restoration of filaggrin, loricrin, and caspase expression. This was repeated in at least three other aged donor models with similar results. In accordance with the conditional knockout model of Baker et al. (2011), in which senescent p16INK4A-expressing cells were selectively eliminated, and as evidenced by this model's morphology and biomarkers, our results indicate that the atrophic phenotype can be significantly improved in vitro by selectively silencing the expression of p16INK4A.
Collectively, these results further substantiate p16INK4A as a major regulator of aging in the epidermis, thus lending strong support for furthering our knowledge on the function and appearance of aged skin.
For human cells obtained from donors, the Declaration of Helsinki protocols were followed; donors gave written, informed consent; and the Stony Brook University IRB approved of the study.
Acknowledgments
This work was fully supported by Unilever R&D.
Glossary
- HEK
human epidermal keratinocyte
- IHC
immunohistochemistry
- K14
keratin 14
- LSE
living skin equivalent
The authors state no conflict of interest.
Footnotes
SUPPLEMENTARY MATERIAL
Supplementary material is linked to the online version of the paper at http://www.nature.com/jid
Supplementary Material
References
- Aho S, Harding CR, Lee J, et al. Regulatory role for the profilaggrin N-terminal domain in epidermal homeostasis. J Invest Dermatol. 2012;132:2376–2385. doi: 10.1038/jid.2012.174. [DOI] [PubMed] [Google Scholar]
- Alcorta DA, Xiong Y, Phelps D, et al. Involvement of the cyclin-dependent kinase inhibitor p16(INK4a) in replicative senescence of normal human fibroblasts. Proc Natl Acad Sci. 1996;93:13742–13747. doi: 10.1073/pnas.93.24.13742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DJ, Wijshake T, Tchkonia T, et al. Clearance of p16 Ink4a-positive senescent cells delays ageing-associated disorders. Nature. 2011;479:232–236. doi: 10.1038/nature10600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campisi J, d'Adda di Fagagna F. Cellular senescence: When bad things happen to good cells. Nat Rev Mol Cell Biol. 2007;8:729–740. doi: 10.1038/nrm2233. [DOI] [PubMed] [Google Scholar]
- Di Nunzio F, Maruggi G, Ferrari S, et al. Correction of laminin-5 deficiency in human epidermal stem cells by transcriptionally targeted lentiviral vectors. Mol Ther. 2008;16:1977–1985. doi: 10.1038/mt.2008.204. [DOI] [PubMed] [Google Scholar]
- Giangreco A, Goldie SJ, Failla V, et al. Human skin aging is associated with reduced expression of the stem cell markers β1 integrin and MCSP. J Invest Dermatol. 2010;130:604–608. doi: 10.1038/jid.2009.297. [DOI] [PubMed] [Google Scholar]
- Gilhar A, Ullmann Y, Karry R, et al. Ageing of human epidermis: the role of apoptosis, fas and telomerase. Br J Dermatol. 2004;150:56–63. doi: 10.1111/j.1365-2133.2004.05715.x. [DOI] [PubMed] [Google Scholar]
- Krishnamurthy J, Torrice C, Ramsey MR, et al. Ink4a/Arf expression is a biomarker of aging. J Clin Invest. 2004;114:1299–1307. doi: 10.1172/JCI22475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega S, Malumbres M, Barbacid M. Cyclin D-dependent kinases, INK4 inhibitors and cancer. Biochim et Biophys Acta. 2002;1602:73–87. doi: 10.1016/s0304-419x(02)00037-9. [DOI] [PubMed] [Google Scholar]
- Ressler S, Bartkova J, Niederegger H, et al. p16INK4A is a robust in vivo biomarker of cellular aging in human skin. Aging Cell. 2006;5:379–389. doi: 10.1111/j.1474-9726.2006.00231.x. [DOI] [PubMed] [Google Scholar]
- Sharpless NE. Ink4a/Arf links senescence and aging. Exp Gerontol. 2004;39 (11–12 Spec. Iss.:1751–59. doi: 10.1016/j.exger.2004.06.025. [DOI] [PubMed] [Google Scholar]
- Waaijer ME, Parish WE, Strongitharm BH, et al. The number of p16INK4A positive cells in human skin reflects biological age. Aging Cell. 2012;11:722–725. doi: 10.1111/j.1474-9726.2012.00837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.