Abstract
Central nervous system (CNS) immune privilege is complex, and it is still not understood how CNS antigens are sampled by the peripheral immune system under steady state conditions. To compare antigen sampling from immune-privileged or nonprivileged tissues, we created transgenic mice with oligodendrocyte or gut epithelial cell expression of an EGFP-tagged fusion protein containing ovalbumin (OVA) antigenic peptides and tested peripheral anti-OVA peptide-specific sentinel OT-I and OT-II T cell activation. We report that oligodendrocyte or gut antigens are sampled similarly, as determined by comparable levels of OT-I T cell activation. However, activated T cells do not access the CNS under steady state conditions. These data show that afferent immunity is normally intact as there is no barrier at the antigen sampling level, but that efferent immunity is restricted. To understand how this one-sided surveillance contributes to CNS immune privilege will help us define mechanisms of CNS autoimmune disease initiation.
The central nervous system (CNS) is considered to be immune-privileged tissue in which adaptive immunity and inflammation are highly controlled. This feature serves to protect post-mitotic neural cells from potential immune response-mediated injury and death. Immune privilege is based on multiple factors, including: 1) presence of the blood-brain barrier (BBB); 2) lack of draining lymphatics; 3) a dearth of professional antigen-presenting cells (APCs), such as dendritic cells (DCs); 4) low expression levels of major histocompatibility complex (MHC) molecules; and 5) many anti-inflammatory soluble modulators1,2. Recently it has become clear that the immune-privileged nature of the CNS is complex and not absolute2,3. Although we understand much about T cell-mediated immunosurveillance of the CNS4,5 and its critical role in protecting these tissues against infections and cancer6,7,8,9, less is known about systemic immunological sampling of CNS antigens and the mechanisms that control CNS autoimmunity.
Drainage of CNS antigens to the periphery might either contribute to tolerance to these antigens or be one of the initial steps in the pathogenesis of CNS autoimmune disease. Cserr and colleagues have shown a suppressed delayed-type hypersensitivity response and ameliorated experimental autoimmune encephalomyelitis (EAE) in rats three weeks after infusing myelin basic protein (MBP) into cerebrospinal fluid (CSF)10,11. However, they also found that removal of the cervical lymph nodes (CLNs) led to a substantial decrease in albumin-specific antibody titers in the serum of rats that had received albumin in the CSF, suggesting that antigen drainage from the CNS can induce an immunogenic response in the periphery12. Consistent with this finding, we have demonstrated that both intracerebrally injected soluble and cell-bound ovalbumin (OVA) antigen can induce peripheral priming, preferential recruitment of OVA-specific CD8+ T cells to the CNS13,14, and hasten the onset of EAE15. Thus, artificially increasing antigen levels in the CNS in the context of injection-induced trauma increases both afferent (antigen drainage) and efferent (leukocyte recruitment) CNS immunity, which might contribute to the initiation and/or exacerbation of CNS autoimmune disease16.
To test whether CNS antigens are sampled under steady state conditions similarly to antigens from nonimmune-privileged tissues, we created three new animal models having either inducible or constitutive Cre recombinase (Cre)-mediated expression of EGFP-tagged OVA257–264-OVA323–339-pigeon cytochrome C (PCC)88–104 neoepitopes in oligodendrocytes (ODCs) of the CNS or constitutive Cre-mediated expression of this fusion protein in gut epithelial cells. We compared the peripheral activation and proliferation of naïve sentinel OT-I and OT-II OVA peptide-specific T cells in all three models. We also tracked responder T cell accumulation in various tissues from mice with and without EAE to test changes in the level of antigen sampling induced under neuroinflammatory conditions.
We found that under steady state conditions there was significant peripheral immunological sampling of constitutively expressed OVA peptides as determined by OT-I T cell proliferation, which was similar in mice expressing ODC or gut epithelial cell neoepitopes. Peripheral T cell activation correlated with the level of CNS neoepitope expression since there was less antigen expression and less T cell proliferation in the inducible ODC OVA peptide mouse model compared to the constitutive one. Responding OT-I T cells shifted from a naïve to effector phenotype upon transfer into mice with constitutive ODC OVA peptide expression but did not infiltrate the CNS. In contrast, neuroinflammation increased the level of antigen sampling and led to the accumulation of OT-I T cells in the inflamed CNS.
Our data provide evidence for the first time that sampling of CNS antigens occurs under normal conditions similarly to that of antigens from nonimmune-privileged tissues such as the gut. CNS inflammation induced during EAE results in increased peripheral antigen sampling. These data suggest that under steady state conditions immune privilege does not result from lack of antigen drainage to the periphery but rather from restricted access of immune cells to the effector site. Elucidating the mechanisms by which CNS-derived antigens reach the peripheral lymphoid tissues and the conditions that permit autoimmune T cell surveillance of the CNS will help us understand the pathogenesis of CNS autoimmune diseases and drive the design of better therapies.
Results
Generation and characterization of the PLP-OP and CNP-OP mice: varying levels of EGFP-tagged neoepitopes in oligodendrocytes
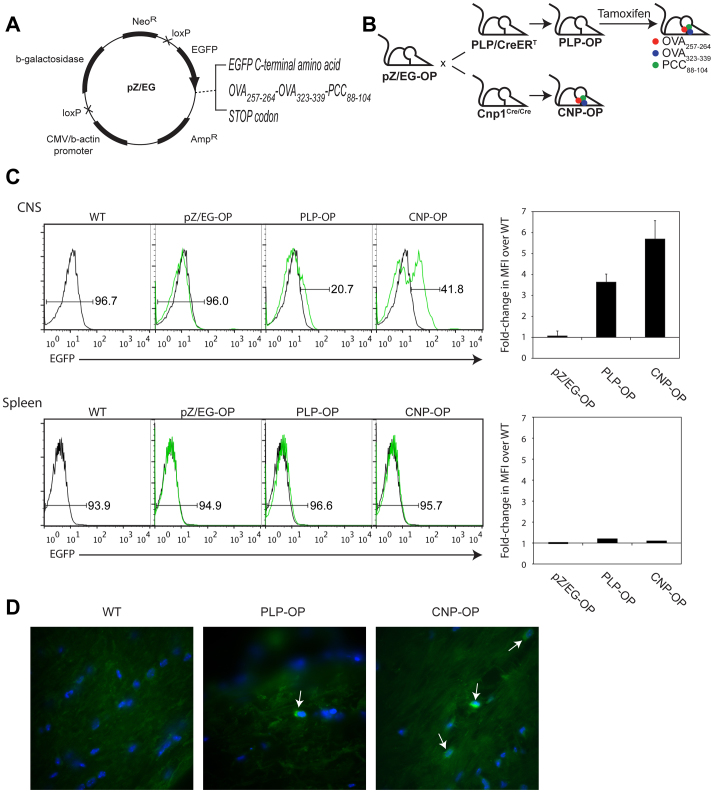
Despite the fact that the CNS is not directly connected to draining lymphatics, two major outflow pathways to the CLNs have been described for CNS interstitial fluid and cerebrospinal fluid via which antigens and APCs may reach the periphery17. Further, although it has been shown that cerebrally injected soluble proteins and DCs reach the CLNs13,14,18,19,20, how endogenous intracellular antigens that are originally sequestered behind the BBB might exit the CNS and induce adaptive autoimmune responses is not fully understood. To address this issue, we used the pZ/EG plasmid (Figure 1A) to create the transgenic loxP-carrying pZ/EG-OP mice having the DNA coding sequence for OVA peptides OVA257–264 (MHC class I-restricted, recognized by OT-I T cells) and OVA323–339 (MHC class II-restricted, recognized by OT-II T cells), and PCC88–104. (These mice are further described in Materials and Methods.) The pZ/EG-OP mice were then crossed with the PLP/CreERT mice or Cnp1Cre/Cre mice to obtain the PLP-OP and CNP-OP mice having tamoxifen (TM)-inducible or constitutive Cre-driven peptide expression in ODCs, respectively (Figure 1B).
Figure 1. EGFP-fused neoepitopes are expressed in CNS of PLP-OP and CNP-OP mice.
(A) Map of pZ/EG plasmid. Neomycin resistance, NeoR; Ampicillin resistance, AmpR. Arrow, 5′ → 3′(drawn by JK). (B) Mouse breeding strategy (drawn by MGH). (C) Histograms show % EGFP+/− cells. WT (black line); transgenic (green line). Column graphs show average fold-change in mean fluorescent intensity (MFI) over WT. Error bars, SEM. (D) Spinal cord; 1000×. DAPI (blue); α-GFP-FITC (green). Arrows, EGFP+ oligodendrocytes.
Flow cytometric analysis following ODC enrichment showed a higher frequency of EGFP-expressing cells in the CNS of CNP-OP mice than in that of TM-treated PLP-OP mice (Figure 1C). Additionally, there was ~6-fold increase in the EGFP MFI over WT in the CNP-OP CNS compared to the PLP-OP CNS (~4-fold EGFP MFI increase over WT) (Figure 1C). In contrast, there was no EGFP expression in CNS tissues from pZ/EG-OP mice or in spleens (Figure 1C) or CLNs (data not shown) from pZ/EG-OP, PLP-OP, and CNP-OP mice. Immunofluorescence staining with anti-GFP antibody confirmed EGFP expression in the spinal cords of CNP-OP and TM-treated PLP-OP mice but not in WT mice (Figure 1D). As CNP and PLP promoters have been shown to drive EGFP transgene expression in Schwann cells of peripheral nervous system (PNS) tissues as well21,22, we performed western blotting to detect EGFP in the sciatic nerve tissue from CNP-OP and PLP-OP mice. EGFP protein expression was below the detectable level in this tissue in both models (data not shown). Since EGFP expression was higher in the CNP-OP compared to the PLP-OP CNS, we examined the ability of EGFP-tagged OVA neoepitopes from CNP-OP mouse brain and sciatic nerve tissue lysates to stimulate OT-I and OT-II splenocytes and found that lysates prepared from the brain, but not the sciatic nerve, induced upregulation of activation marker CD69 on both the OT-I and OT-II T cells (Supplemental Figure 1). Collectively, these data show that the expression of neoepitopes is higher in the CNS of the CNP-OP mice compared to the PLP-OP mice and that neoepitope expression in the PNS is below the threshold for T cell activation. These animal models will allow us to examine peripheral immunosurveillance of CNS neoepitopes under steady state and inflammatory conditions and compare this to surveillance of nonimmune-privileged tissue antigens using a third model.
There is peripheral sampling of CNS neoepitopes by sentinel responder cells under steady state conditions
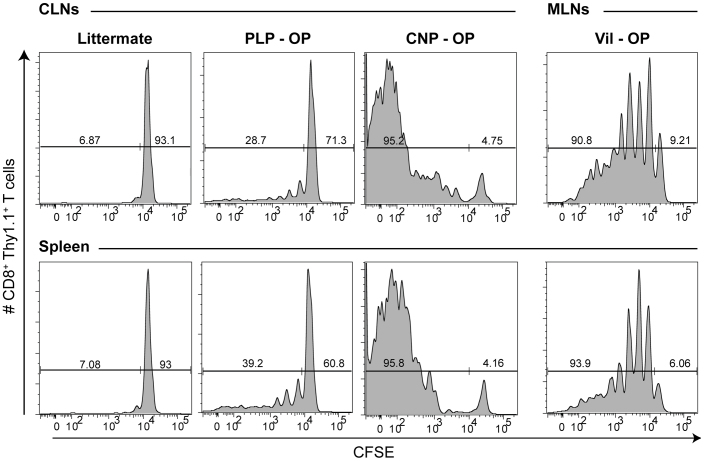
We have previously shown that intracerebral injection of both soluble and DC-bound antigens in naïve C57BL/6 mice induces peripheral activation of antigen-specific T cells and their homing to the CNS13,14,15. However, in these experiments the microtrauma caused by intracerebral injection might elaborate danger signals leading to the activation of APCs and potentially influence immunity to injected antigens. To overcome these limitations and to test peripheral sentinel T cell activation and proliferation in response to varying levels of CNS neoepitopes under steady state conditions, we adoptively transferred naïve CFSE-labeled CD44low CD8+ Thy1.1+ OT-I and CD4+ Thy1.1+ OT-II T cells into TM-treated PLP-OP, CNP-OP, and littermate Thy1.2+/+ hosts. In order to compare the level of peripheral immunosurveillance of antigens from the CNS to that of nonimmune-privileged tissues, we also transferred naïve CD8+ Thy1.1+ OT-I T cells into mice with OVA peptide expression restricted to gut epithelial cells (i.e., the Vil-OP mice). Six days post-adoptive transfer we observed substantial CFSE dilution of the CD8+ Thy1.1+ OT-I T cells in the CLNs and spleen of CNP-OP and, to a lesser extent, PLP-OP mice (Figure 2) but not of the CD4+ Thy1.1+ OT-II T cells (data not shown). Furthermore, we found that the high frequency of CFSE-diluted CD8+ Thy1.1+ OT-I T cells in the CLNs and spleen of the CNP-OP mice was comparable to that of the gut-draining mesenteric lymph nodes (MLNs) and spleen of the Vil-OP mice (Figure 2).
Figure 2. CNS neoepitopes are immunologically surveyed under normal conditions in the periphery.
Mice received 5 × 105 neoepitope-specific T cells. FACS staining was performed on lymphocytes 6 days post-adoptive transfer. Histograms show CFSE dilution of CD8+ Thy1.1+ cells from CLNs (WT, PLP-OP, and CNP-OP mice) and MLNs (Vil-OP mouse) and spleen. Numbers indicate frequency of CFSEhigh vs. CFSElow/int cells. N = 8 littermates, n = 7 PLP-OP, n = 7 CNP-OP, and n = 4 Vil-OP mice (2 independent experiments).
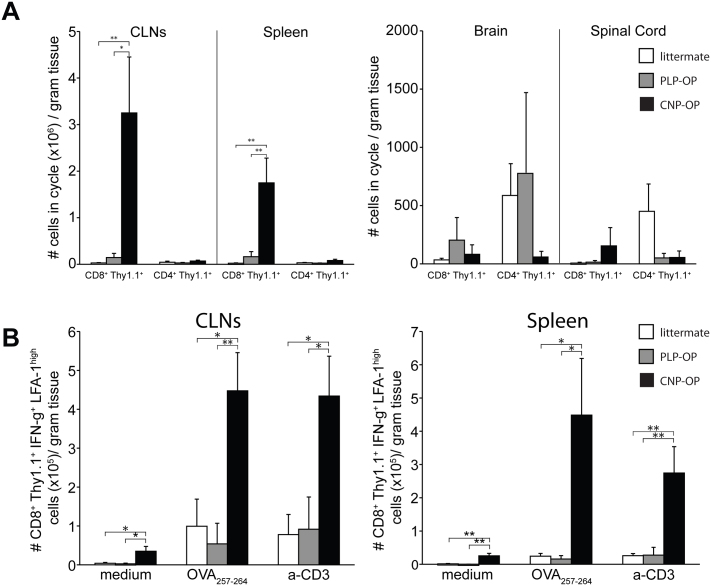
There was a significant accumulation of proliferated CFSElow/int LFA-1high CD8+ Thy1.1+ T cells in both the CLNs and spleen of naïve CNP-OP mice (Figure 3A), which did not reach significance in the PLP-OP mice. By comparison, there was no appreciable accumulation of the transgenic CD4+ Thy1.1+ T cells in these tissues in either model (Figure 3A). In contrast to the high accumulation of OT-I T cells in the secondary lymphoid organs, on average there were fewer than 800 transgenic CD8+ or CD4+ Thy1.1+ T cells per gram of CNS tissue in naïve CNP-OP and PLP-OP mice (Figure 3A). Thus, there is peripheral sampling of the ODC neoepitopes by the CD8+ Thy1.1+ OT-I T cells and not by CD4+ Thy1.1+ OT-II T cells under normal conditions.
Figure 3. Antigen-specific CD8+ T cells accumulate in peripheral tissues of mice with high levels of CNS neoepitope expression.
(A) Column graphs indicate mean # of CFSElow/int LFA-1high CD8+/CD4+ Thy1.1+ cells/gram tissue. (B) Column graphs indicate mean # of CD8+ Thy1.1+ IFN-γ+ LFA-1high cells/gram tissue. Error bars, SEM. *, p < 0.05; **, p < 0.01. Data were generated from n = 8 littermates, n = 7 PLP-OP, and n = 7 CNP-OP mice (2–4 experiments).
The effector T helper (Th) or cytotoxic T lymphocyte (CTL) phenotype of newly activated and expanded T cells is, in part, determined by the cytokines they produce. We therefore tested the ability of the OVA-specific T cells to produce cytokines in a memory recall assay. For this assay, lymphocytes were isolated from the CLNs and spleen six days post-adoptive transfer and stimulated with OVA257–264 and OVA323–339 peptides ex vivo for 4 hours. Transgenic CD4+ Thy1.1+ T cells did not produce IFN-γ or IL-17 (data not shown), which is consistent with a naïve phenotype and their lack of proliferation. However, we observed that CD8+ Thy1.1+ T cells produced IFN-γ+ in the peripheral lymphoid tissues of CNP-OP but not PLP-OP mice (Figure 3B), suggesting that an effector CTL pool was created from the adoptively transferred naïve OT-I cells in the CNP-OP mice. Thus, under conditions in which there is a higher level of neoepitope expression, T cells acquire an effector phenotype but still do not enter the CNS.
Neuroinflammation increases the level of CNS neoepitope sampling, leading to the accumulation of effector CD8+ T cells in the CNS of PLP-OP and CNP-OP mice with EAE
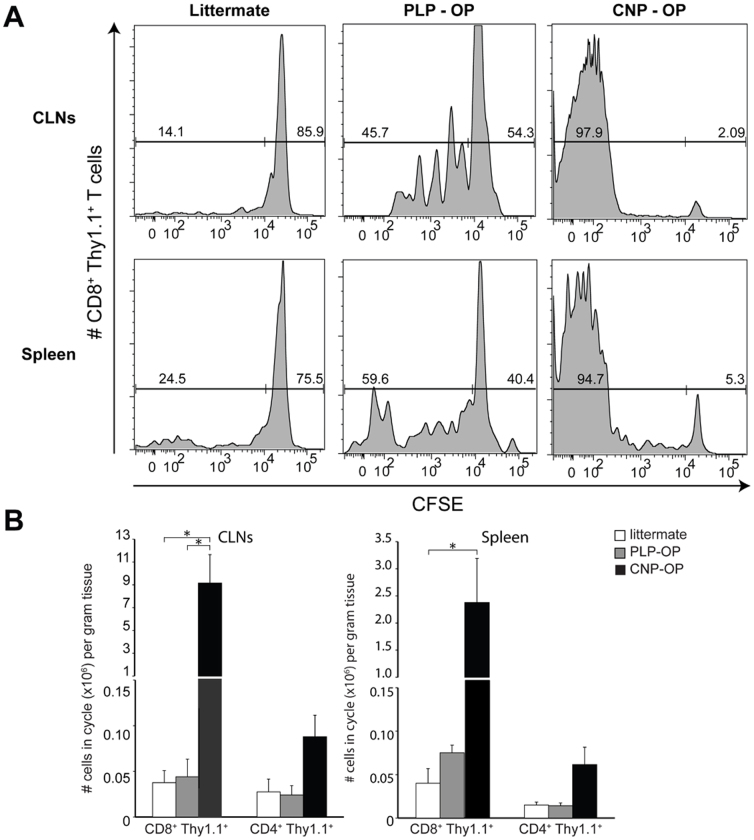
We next tested how neuroinflammation modulates the level of peripheral sampling of CNS neoepitopes. To study this, we induced EAE in TM-treated PLP-OP, CNP-OP, and littermate female mice. Naïve CFSE-labeled CD8+ Thy1.1+ OT-I and CD4+ Thy1.1+ OT-II T cells were adoptively transferred nine days post-EAE induction into the Thy1.2+/+ hosts. Within 1–4 days of disease onset, we observed an increase in the frequency of CFSElow/int CD8+ Thy1.1+ T cells in the peripheral lymphoid tissues of PLP-OP mice, which remained high in the CNP-OP mice (Figure 4A). These data show that active neuroinflammation increases CNS antigen sampling in the CLNs. Although the absolute number of CD8+ Thy1.1+ OT-I T cells in cycle in the periphery increased in the CNP-OP mice, this number actually decreased in the PLP-OP mice compared to non-inflammatory conditions (Figure 4B). This suggested that activated responder OT-I T cells left the peripheral lymphoid tissues and migrated to the inflamed CNS during EAE.
Figure 4. There is increased peripheral immunosurveillance of CNS neoepitopes under neuroinflammatory conditions.
Nine days post-EAE induction, mice received 5 × 105 neoepitope-specific T cells. FACS was performed within 1–4 days of disease onset. (A) Histograms show percentage of CFSElow/int/CFSEhigh cells. (B) Column graphs indicate mean # of CFSElow/int LFA-1high CD8+/CD4+ Thy1.1+ cells/gram tissue. Error bars, SEM. *, p < 0.05; **, p < 0.01. N = 7 littermates, n = 5 PLP-OP and n = 11 CNP-OP mice (3 experiments).
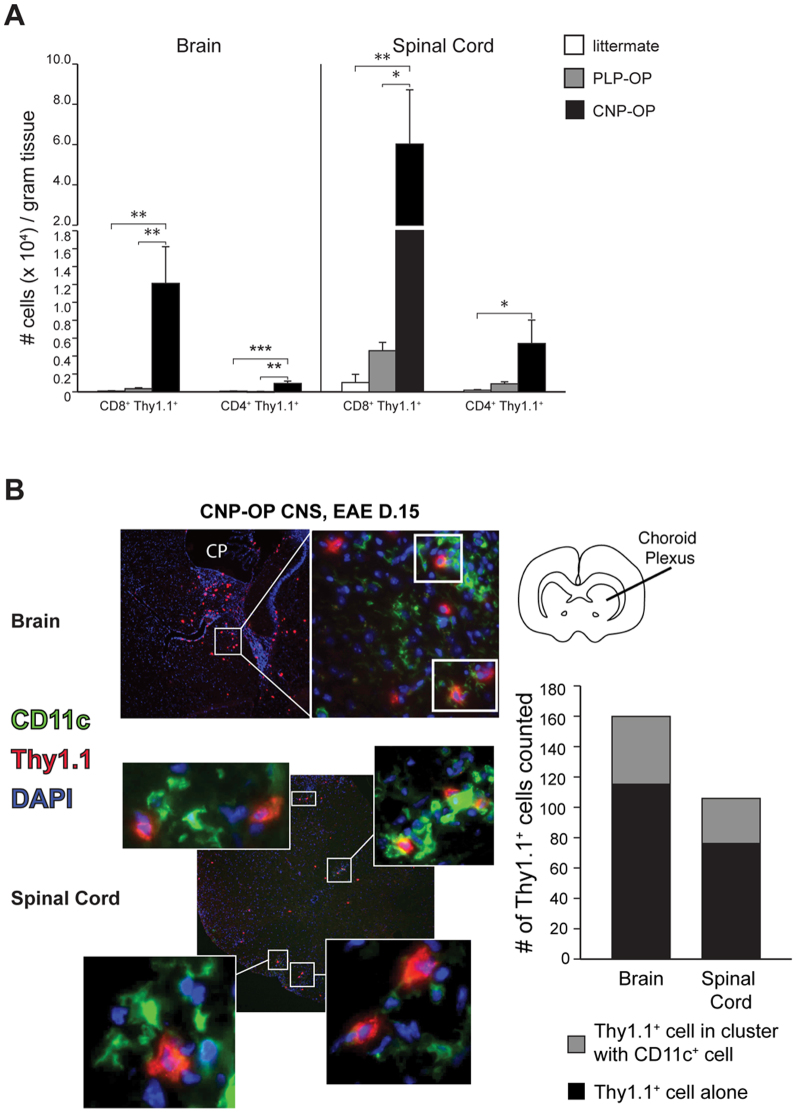
Therefore, we examined whether neuroinflammation induced the homing of OVA-specific T cells to the CNS. Compared to littermate controls, we observed a significant increase in the accumulation of CD8+ Thy1.1+ OT-I T cells in the brain and spinal cord of CNP-OP mice with EAE and a substantial increase in these cells only in the spinal cord of PLP-OP mice with EAE by FACS analysis (Figure 5A). We also confirmed the localization of the OT-I T cells in the CNS tissues of CNP-OP mice at EAE onset (day 15) by immunofluorescent microscopy (Supplemental Figure 2), although they did not exacerbate the initiation phase of clinical EAE compared to mice that did not receive T cells (data not shown). Most importantly, the transgenic OT-I T cells were not detected in the sciatic nerve (Supplemental Figure 2)–further confirming that the level of neoepitopes in the PNS was not sufficient to induce OVA-specific T cell recruitment. Finally, there was a significant accumulation of CD4+ Thy1.1+ OT-II T cells in the CNS of CNP-OP but not PLP-OP mice with EAE (Figure 5A). Collectively, these data indicate that ongoing neuroinflammation strongly enhances efferent immunity by promoting CNS antigen-specific T cell recruitment into the CNS.
Figure 5. Neoepitope-specific CD8+ T cells accumulate in CNS of PLP-OP and CNP-OP mice with EAE.
(A) Column graphs–mean # transgenic cells/gram tissue. N = 7 littermates, n = 5 PLP-OP, n = 11 CNP-OP mice (3 EAE experiments). Error bars, SEM. *, p < 0.05; **, p < 0.01; ***, p < 0.0001 (B) CNP-OP CNS (EAE-D15); 100×. Choroid plexus (CP). White boxes, Thy1.1+(red)/CD11c+(green) cell interactions. Column graphs–11 brain & 20 spinal cord 400× fields (n = 1 CNP-OP EAE mouse).
Next we examined the localization of CNS-infiltrating OT-I T cells. Tertiary lymphoid structures containing T cells and follicular DCs have been shown in the leptomeninges of mice with EAE and humans with multiple sclerosis23,24 and may be critical in maintaining CNS autoimmune disease by providing a local niche for the presentation of CNS autoantigens24,25. Thus, we studied whether the OVA-specific Thy1.1+ T cells associated with DCs in the CNS of CNP-OP mice with EAE (day 15 post-induction) by immunofluorescent microscopy. We noted that transferred Thy1.1+ T cells were distributed predominantly near the choroid plexus and ventricles in the brain (Figure 5B, top left) and uniformly across spinal cord sections (Figure 5B, bottom left). The Thy1.1+ T cells were also frequently found in direct contact with CD11c+ cells (30% of all Thy1.1+ T cells counted in CNS tissues; Figure 5B, boxed and enlarged images). These data support that OVA-specific T cells and DCs preferentially colocalize in the inflamed CNS.
Discussion
Despite the fact that the CNS is relatively immune privileged tissue, autoimmune diseases such as multiple sclerosis (MS) do exist. The purpose of this study was to test peripheral immunological surveillance of CNS neoantigens compared to non-immunologically privileged tissues in an effort to understand how CNS immune privilege is maintained and broken. To address this question, we created mice expressing EGFP-tagged OVA peptides in ODCs or gut epithelial cells and used reporter T cells to indicate neoantigen recognition. In this way, we effectively modeled a scenario in which T cells with high affinity for the neoantigens bypassed central tolerance mechanisms but were kept in check by peripheral tolerance mechanisms, which are thought to be dysregulated in patients with MS26.
In our ODC models, the regulatory sequences of the PLP and Cnp1 genes drive Cre recombinase-mediated EGFP-tagged neoantigen expression in myelinating glial cells at low and high levels, respectively. Although PLP and CNPase proteins are most abundant in central myelin, they are also expressed at significantly lower levels in peripheral myelin22,27,28,29,30,31,32. Our findings that T cells were not stimulated by CNP-OP sciatic nerve tissue lysates in vitro and were not recruited to the sciatic nerves of CNP-OP mice with EAE in vivo suggest that neoantigen expression in peripheral myelin is below the immunological surveillance level. This might be due to either little or no CNP- and PLP-driven transgene expression in the PNS after P3033. Additionally, CNPase is weakly expressed in non-neural cells and tissues, including circulating lymphocytes and the thymus31. However, we did not observe EGFP expression in secondary lymphoid organs of the CNP-OP and PLP-OP mice. While the possibility remains that the level of neoantigen expression could be below the detectable level in these tissues by FACS analysis, peripheral expression of OVA antigen by CD45neg lymph node stromal cells has been shown to result in deletional tolerance of transferred OT-I T cells34. Contrary to this, we observed activation of transferred OT-I T cells, which produced IFN-γ under normal conditions.
Our data showing peripheral expansion of activated OT-I T cells indicates that, similarly to antigens from nonprivileged tissues, there is continuous drainage and immunological sampling of ODC-restricted neoantigens in secondary lymphoid organs of adult mice under normal conditions. This finding is in agreement with that reported by Schildknecht and colleagues who observed expansion of adoptively transferred LCMV antigen-specific CD8+ T cells in all peripheral lymphoid tissues, including both proximal CNS-draining lymph nodes and distal non-draining lymph nodes and spleen, using another inducible PLP driver strain35. However, our result differs from that of Na et al. who did not observe peripheral OVA-specific CD8+ T cell proliferation after P10 in mice with MBP promoter-driven OVA in ODCs36. Their results may indicate OT-I T cell deletion in response to increased levels of OVA, as MBP-specific T cell deletion increases after two weeks of age and correlates with MBP protein expression28.
Our laboratory has previously shown that intracerebrally injected soluble and DC-bound OVA proteins elicit the systemic activation of neoantigen-specific CD8+ T cells and their recruitment to the brain in naïve animals13,14. However, in the PLP-OP and CNP-OP models the peripherally activated OT-I T cells did not accumulate in the CNS. One possibility that could explain this difference is that the microtrauma induced in the cerebral injection model elaborated danger signals that induced T cell homing to the CNS. Yet another possibility is that the physiological levels of the neoantigens are lower in the transgenic mice of the present study, resulting in fewer MHC-peptide complexes and, thus, lower OT-I T cell avidity and incomplete activation in the peripheral lymphoid tissues37. In support of this, a previous study showed weaker OT-I T cell proliferation that remained restricted to gut-associated lymphoid tissues (GALT) in mice fed lower amounts of OVA but showed stronger proliferation that disseminated to LNs beyond GALT in mice fed higher amounts of OVA34. Consistent with this is our finding of weaker peripheral OT-I T cell activation in naive PLP-OP mice with lower neoantigen expression compared to that observed in CNP-OP mice with higher neoantigen expression. Therefore, it is plausible that low T cell avidity may result in incomplete activation of OT-I T cells and their inability to enter the CNS.
We also observed that the transferred OVA-specific T cells did not induce CNS autoimmunity in naïve transgenic PLP-OP or CNP-OP mice. In agreement with this, Na et al. found that OT-I T cells only induced disease in Rag−/− MBP-OVA mice but not in immune-sufficient hosts36. However, another study showed that ODC antigen-specific CD8+ T cells induced CNS disease in immune-sufficient host animals when pre-activated prior to transfer38. Collectively, these results argue that the context of antigen presentation and T cell activation regulate CNS immune privilege and disease initiation.
The question still remains as to how CNS antigens reach the CLNs under normal conditions, but other studies suggest that DC-mediated drainage and cross-presentation are involved. Walter and Albert showed that antigen from intracerebrally injected MHC class I-deficient mOVA/Kb−/− splenocytes is first cross-presented to OT-I T cells in the CLNs prior to their accumulation in the brain39. It has also been shown that cell-associated OVA is more efficiently cross-presented to OT-I T cells than to OT-II T cells, but that soluble OVA stimulates both OT-I and OT-II T cells equally40. Taken together with our data showing a strong OT-I response, these findings support the idea that the ODC-associated OVA is being efficiently cross-presented to the OT-I T cells in the peripheral lymphoid tissues of CNP-OP and PLP-OP mice.
We observed increased peripheral immune surveillance during EAE, which might be due to increased antigen drainage from the CNS as was suggested previously in a study showing that myelin proteins and degradation products from brain lesions of monkeys with EAE and humans with MS can be found in the draining CLNs41. The fact that CNS-infiltrating OT-II T cells were only observed in mice with both high neoantigen expression and active neuroinflammation suggests that the levels of both antigen expression and antigen release/drainage contribute to CNS afferent immunity.
We found that donor T cells colocalized with DCs in the CNS of transgenic mice during the onset of EAE. Surprisingly, however, there was no hastening of disease during this period, which was similar in the PLP-OP and CNP-OP mice that received donor T cells compared to PLP-OP and CNP-OP mice that did not (data not shown). This finding suggests that infiltrating OT-I T cells did not observably contribute to EAE onset and is in agreement with that reported by Schildknecht et al., who observed that non-tolerized myelinating glial cell antigen-specific CD8+ T cells did not induce CNS autoimmunity or inflammation35. As the initiation of EAE is determined by accumulation of DCs42, further studies are needed to determine the role of the neoantigen-specific T cells in the chronic phase of EAE disease in the CNP-OP and PLP-OP mice.
Finally, in this study we observed a higher accumulation of OT-I T cells in the spinal cord than in the brain of PLP-OP and CNP-OP mice during EAE, which may reflect regional differences in the expression pattern of ligands on barrier endothelial cells needed by CD8+ T cells for entry. This is the case for a subset of CD4+ T cells, as CCL20, the ligand for the receptor CCR6 expressed on Th17 cells, is constitutively expressed on epithelial cells of the choroid plexus; this interaction facilitates Th17 cell entry into the brain at this location43 and is a required step for EAE induction. It has been shown that adhesion of CD8+ T cells to inflamed brain microvessels is critically dependent on P-selectin glycoprotein ligand-1 (PSGL-1)44. Interestingly, the receptor for PSGL-1, P-selectin, has been shown to be upregulated more in the spinal cord than in the brain during EAE45. Whether P-selectin is also upregulated more in the spinal cord of the PLP-OP and CNP-OP models under neuroinflammatory conditions remains to be determined.
Here we present two new models that will help facilitate our understanding of the mechanisms governing immune surveillance of the CNS, including the rules governing T cell accumulation in the CNS under various conditions and their contribution to CNS autoimmune disease. At one time it was thought that the CNS was completely isolated from immune surveillance because of lack of draining lymphatics, which prevented escape of CNS antigens, and prevention of immune cell entry due to the BBB3. Our data, instead, suggest that there is continuous surveillance of CNS antigens in peripheral lymphoid tissues, which indicates that immune privilege is not the result of limited antigen sampling. Additionally, neuroinflammation induces CNS accumulation of T cells that have high affinity for CNS antigens. Future work will elucidate how the CNS antigens reach the periphery.
Methods
Mice
The pZ/EG plasmid (generated by Dr. Andras Nagy, Mount Sinai Hospital, Toronto, ON) was designed to express EGFP under the control of the CMV/β-actin promoter. Two loxP sites flank a β-galactosidase expression cassette adjacent to a neomycin resistance gene in the plasmid, which also contains an ampicillin resistance gene between the EGFP expression cassette and the CMV/β-actin promoter complex. The DNA coding sequence for OVA257–264-OVA323–339-PCC88–104 peptides was inserted at the 3′ end of the open reading frame of EGFP before the STOP codon using the QuikChange method (Stratagene, La Jolla, CA). Megaprimers were designed to insert the neoepitopes in a one-step QuikChange reaction. The pZ/EG-OP plasmid was linearized using ScaI restriction enzyme digestion and subsequently purified by electroelution and ethanol precipitation.
Transgenic pZ/EG-OP mice were generated by microinjection of linearized, purified DNA into one-cell C57BL/6 embryos, which were implanted into pseudopregnant C57BL/6 mice. Two founder pZ/EG-OP mouse lines were established. One (#147) was crossed with either PLP/CreERT mice46 or with Cnp1Cre/Cre mice47 to obtain the double transgenic PLP-OP or CNP-OP offspring having either tamoxifen-inducible or constitutive Cre-mediated myelinating glial cell-specific transgene expression, respectively. The pZ/EG-OP mice were also crossed with the Villin-Cre mice (The Jackson Laboratory, Bar Harbor, ME) to generate the Vil-OP mice having constitutive intestinal epithelium-specific transgene expression. Genotyping of the double transgenic mouse strains was done by PCR on genomic DNA using these primer sequences for GFP: GFP sense: 5′-CAC ATG AAG CAG CAC GAC TT-3′; GFP anti-sense: 5′-TGC TCA GGT AGT GGT TGT CG-3′, and the following Cre driver line-specific primer sequences: 1) PLP-OP mice – CreERT sense: 5′-GAT GTA GCC AGC AGC ATG TC-3′; CreERT anti-sense: 5′-ACT ATA TCC GTA ACC TGG AT-3′; 2) CNP-OP mice – CNP-E3 sense: 5′-GCC TTC AAA CTG TCC ATC TC-3′; CNP-E3 anti-sense: 5′-CCC AGC CCT TTT ATT ACC AC-3′; and puro3: 5′-CAT AGC CTG AAG AAC GAG A-3′; and 3) Vil-OP mice – Vil-Cre sense: GTC TGG GAC AGA GAA CAA ACC; Vil-Cre anti-sense: ACA TCT TCA GGT TCT GCG GG. (All primers are from Integrated DNA Technologies, Inc., Coralville, IA.)
The Thy1.1, OVA257-264-specific OT-I, and OVA323–339-specific OT-II mice were also purchased from Jackson, and the OT-I and OT-II mice were bred to the Thy1.1 background. Female mice (6–12 weeks old) were used for the EAE experiments, and male mice were used for the non-EAE experiments. All experiments were conducted in accordance with guidelines from the National Institutes of Health and the University of Wisconsin-Madison Institutional Animal Care and Use Committee.
Tamoxifen treatment
As described by Leone et al.48, tamoxifen (TM) (Sigma, St. Louis, MO) was dissolved in a 9:1 sunflower oil:ethanol mixture at a concentration of 10 mg/mL. Mice were intraperitoneally (i.p.) injected with 1 mg TM twice a day for 5 days.
Oligodendrocyte preparation
Oligodendrocytes (ODCs) were prepared from CNS tissues according to the following protocol adapted from Ji et al.49. Briefly, CNS tissues were minced finely in 5 mL digestion solution containing 1 mg/mL papain (Worthington Biochemical), 20 ng/mL DNase (Sigma), 1.1 mM EDTA, 0.067 mM mercaptoethanol, and 5.5 mM cysteine-HCl in HBSS. Tissues were digested for 30 min at 37°C while gently shaking. Afterwards, the tissues were gently triturated with an 18 G needle, pushed through a 70 μm nylon cell strainer, and washed with five volumes of 5% heat-inactivated FBS in HBSS before centrifugation at 1200 rpm for 7 min. After removing the supernatant, tissues were resuspended in 70% Percoll (GE Healthcare) and overlaid with 30% Percoll and then centrifuged at 1200 rpm for 20 min without brake. CNS cells were collected from the top (i.e., 30%) and interface layers following centrifugation, washed with HBSS followed by FACS buffer, and then run on a FACS Calibur.
EAE induction
EAE was induced by subcutaneous (s.c.) immunization with 100 μg MOG35–55 peptide (Genemed Synthesis, Inc., San Antonio, TX) emulsified in CFA (Difco) supplemented with 5 mg/mL H37Ra Mycobacterium tuberculosis. Pertussis toxin, 200 ng, (List Biological Laboratories, Inc., Campbell, CA) was injected i.p. on the day of EAE induction and again two days later. Clinical scores were assessed daily according to the following scale: 0, no clinical symptoms; 1, limp/flaccid tail; 2, partial hind limb paralysis; 3, complete hind limb paralysis; 4, quadriplegia; 5, moribund or dead. Intermediate scores were assigned for intermediate symptoms.
Adoptive transfer
Lymphocytes from pooled lymph node preparation from OT-I Thy1.1 and OT-II Thy1.1 transgenic mice were CFSE labeled in 1 μM CFSE as previously described50. 5 × 105 CFSE-labeled naïve (i.e., CD44low) OT-I CD8+ Thy1.1+ and OT-II CD4+ Thy1.1+ T cells were adoptively transferred intravenously (i.v.) into the retro-orbital vein of recipient mice.
Lymphocyte isolation, intracellular cytokine staining, and FACS
Mice were deeply anesthetized with ketamine/xylazine and then transcardially perfused with cold PBS. Single cell suspensions were made from cervical lymph nodes (CLNs) and spleens by grinding the tissues between the frosted ends of glass slides. Red blood cells were lysed using ACK lysis buffer, and cells were washed with HBSS. Brain and spinal cord tissues were minced with razor blades and pushed through 70 μm nylon cell strainers. Cells were washed, resuspended in 50% Percoll and overlaid with 30% Percoll. The gradient was centrifuged at 2500 rpm for 30 min at 4°C without brake. The interface was removed and washed before plating. All collected organs were weighed, and live cells were counted using a hemocytometer.
For intracellular cytokine staining, cells were incubated at 37°C with 5% CO2 in complete RPMI 1640 supplemented with GolgiStop (BD Biosciences, San Jose, CA) (1:1000) in the presence of 5 μg/mL OVA257–264/OVA323–339 peptides (Ana Spec, Inc., San Jose, CA) or 5 μg/mL anti-CD3 Ab for 4 hours. After surface staining with antibodies against CD4, CD8, LFA-1, and Thy1.1 in the presence of unlabeled blocking antibody anti-Fcγ-R (2.4G2), cells were fixed and permeabilized with Cytofix/Cytoperm solution (BD Biosciences), and then stained with antibodies against IFN-γ and IL-17. Regulatory CD25+ Foxp3+ cell staining was performed according to protocol from eBioscience, Inc. (San Diego, CA). Data were acquired on a BD LSR II flow cytometer (BD Biosciences) and analyzed using FlowJo software (Tree Star, Inc., Ashland, OR).
Fluorescent microscopy
For frozen sections, mice were first perfused with cold PBS, followed by perfusion with 4% PFA/PBS. Harvested tissues were left in 25% sucrose/PBS overnight at 4°C and then embedded in Tissue-Tek OCT Compound (Sakura Finetek USA, Inc., Torrance, CA) before freezing at −80°C. Five μm-thick tissue cryosections were cut and stored at −80°C until staining. Frozen sections were thawed for 10 min at room temperature and then placed in acetone for 10 min at −20°C. Next, sections were incubated in PBS for 30 min at room temperature (RT) and then blocked with 2.4G2 antibody in 0.1% Triton X-100/PBS (1:50) for 30 minutes before applying anti-GFP-FITC primary antibody in 0.1% Triton X-100/PBS (1:100) for 1 hour at 37°C. Sections were then washed 3 times for 10 min each time with PBS and mounted with ProLong Gold antifade reagent containing DAPI (Invitrogen). All images were acquired with a camera (Optronics Inc., Goleta, CA) mounted on a fluorescence microscope (Olympus BX41, Leeds Precision Instruments). Individual fluorescent channel images were merged using PictureFrame software (Optronics Inc.). The brightness/contrast of the acquired digital images was applied equally across the entire image and equally to control images and analyzed using Adobe Photoshop CS4 software (Adobe Systems Inc., San Jose, CA).
Antibodies
The following fluorophore-conjugated antibodies were purchased from BD Biosciences: anti-CD4 Alx700 (RM4-5), anti-CD4 Alx647 (RM4-5), anti-CD8 PerCP (53–6.7), anti-CD11a (LFA-1) PE-Cy7 (2D7), anti-CD90.1 (Thy1.1) APC-Cy7 (OX-7), anti-CD127 Alx700 (A7R34), anti-CD62L PE (Mel-14), anti-CD44 APC (IM7), anti-IFN-γ APC, and anti-IL-17A PE. Anti-CD25 APC (PC61.5) and anti-Foxp3 PE (FJK-16s) were purchased from eBioscience, Inc. Goat pAb anti-GFP-FITC was purchased from Abcam. Anti-Fcγ-R (2.4G2) was produced from a hybridoma.
Statistics
One-tailed unpaired Student's t-tests were computed using InStat software (GraphPad Software, La Jolla, CA) to make statistical comparisons between groups.
Ethics statement
C57BL/6 WT and Villin-Cre mice were obtained from The Jackson Laboratory (Bar Harbor, ME). Transgenic pZ/EG-OP mice were generated at the University of Wisconsin Biotechnology Center Transgenic Facility by microinjection of linearized, purified DNA into one-cell C57BL/6 embryos. The PLP/CreERT and Cnp1Cre/Cre mice were a generous gift from Dr. Brian Popko (University of Chicago, Chicago, IL). Experimental mice underwent adoptive transfer and/or EAE induction. All animal procedures used in this study were conducted in strict compliance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals and approved by the University of Wisconsin Center for Health Sciences Research Animal Care Committee. All mice (~25 g) were anesthetized with ketamine and xylazine for procedures, and all efforts were made to minimize suffering.
Author Contributions
A.N., C.L., J.K. and J.S.H. generated the construct, transgenic animals and analyzed immune responses of these mice. M.G.H. and B.D.C. performed adoptive transfers, induced EAE, and analyzed cytofluorimetry data. M.Z., A.S. and K.C. contributed to immunohistochemistry and mouse phenotyping. Z.F. and M.S. provided critical conceptual guidance, comments, and reviews. M.G.H. and Z.F. wrote the main manuscript text. M.G.H. and P.H. prepared figures. All authors reviewed the manuscript.
Supplementary Material
Supplemental Material
Acknowledgments
We thank Khen Macvilay, Sinarack Macvilay, Laura Schmitt-Brunold, and Satoshi Kinoshita for excellent technical assistance and Dr. Erika Hèninger and Dr. Dana C. Baiu for technical advice. This research was supported by NIH/NIGMS grant T32-GM007507 (Neuroscience Training Program), and NIH grants R01-NS37570 (Z. Fabry) and R01-AI048087 (M. Sandor).
References
- Fabry Z., Schreiber H. A., Harris M. G. & Sandor M. Sensing the microenvironment of the central nervous system: immune cells in the central nervous system and their pharmacological manipulation. Curr. Opin. Pharmacol. 8, 496–507 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wekerle H. Breaking ignorance: the case of the brain. Curr. Top. Microbiol. Immunol. 305, 25–50 (2006). [DOI] [PubMed] [Google Scholar]
- Galea I., Bechmann I. & Perry V. H. What is immune privilege (not)? Trends Immunol. 28, 12–18 (2007). [DOI] [PubMed] [Google Scholar]
- Kivisakk P. et al. Human cerebrospinal fluid central memory CD4+ T cells: evidence for trafficking through choroid plexus and meninges via P-selectin. Proc. Natl. Acad. Sci. U. S. A. 100, 8389–8394 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransohoff R. M. & Engelhardt B. The anatomical and cellular basis of immune surveillance in the central nervous system. Nat. Rev. Immunol. 12, 623–635 (2012). [DOI] [PubMed] [Google Scholar]
- Caspi R. R. Immunotherapy of autoimmunity and cancer: the penalty for success. Nat. Rev. Immunol. 8, 970–976 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinschmidt-DeMasters B. K. & Tyler K. L. Progressive multifocal leukoencephalopathy complicating treatment with natalizumab and interferon beta-1a for multiple sclerosis. N. Engl. J. Med. 353, 369–374 (2005). [DOI] [PubMed] [Google Scholar]
- Langer-Gould A., Atlas S. W., Green A. J., Bollen A. W. & Pelletier D. Progressive multifocal leukoencephalopathy in a patient treated with natalizumab. N. Engl. J. Med. 353, 375–381 (2005). [DOI] [PubMed] [Google Scholar]
- Van Assche G. et al. Progressive multifocal leukoencephalopathy after natalizumab therapy for Crohn's disease. N. Engl. J. Med. 353, 362–368 (2005). [DOI] [PubMed] [Google Scholar]
- Cserr H. F. & Knopf P. M. Cervical lymphatics, the blood-brain barrier and the immunoreactivity of the brain: a new view. Immunol. Today 13, 507–512 (1992). [DOI] [PubMed] [Google Scholar]
- Harling-Berg C. J., Knopf P. M. & Cserr H. F. Myelin basic protein infused into cerebrospinal fluid suppresses experimental autoimmune encephalomyelitis. J. Neuroimmunol. 35, 45–51 (1991). [DOI] [PubMed] [Google Scholar]
- Harling-Berg C., Knopf P. M., Merriam J. & Cserr H. F. Role of cervical lymph nodes in the systemic humoral immune response to human serum albumin microinfused into rat cerebrospinal fluid. J. Neuroimmunol. 25, 185–193 (1989). [DOI] [PubMed] [Google Scholar]
- Karman J., Ling C., Sandor M. & Fabry Z. Initiation of immune responses in brain is promoted by local dendritic cells. J. Immunol. 173, 2353–2361 (2004). [DOI] [PubMed] [Google Scholar]
- Ling C., Sandor M. & Fabry Z. In situ processing and distribution of intracerebrally injected OVA in the CNS. J. Neuroimmunol. 141, 90–98 (2003). [DOI] [PubMed] [Google Scholar]
- Zozulya A. L. et al. Intracerebral dendritic cells critically modulate encephalitogenic versus regulatory immune responses in the CNS. J. Neurosci. 29, 140–152 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey W. F. Basic principles of immunological surveillance of the normal central nervous system. Glia 36, 118–124 (2001). [DOI] [PubMed] [Google Scholar]
- Laman J. D. & Weller R. O. Drainage of cells and soluble antigen from the CNS to regional lymph nodes. J. Neuroimmune Pharmacol. 8, 840–856 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury M. W., Cserr H. F. & Westrop R. J. Drainage of cerebral interstitial fluid into deep cervical lymph of the rabbit. Am. J. Physiol. 240, F329–336 (1981). [DOI] [PubMed] [Google Scholar]
- Hatterer E. et al. How to drain without lymphatics? Dendritic cells migrate from the cerebrospinal fluid to the B-cell follicles of cervical lymph nodes. Blood 107, 806–812 (2006). [DOI] [PubMed] [Google Scholar]
- Yamada S., DePasquale M., Patlak C. S. & Cserr H. F. Albumin outflow into deep cervical lymph from different regions of rabbit brain. Am. J. Physiol. 261, H1197–1204 (1991). [DOI] [PubMed] [Google Scholar]
- Mallon B. S., Shick H. E., Kidd G. J. & Macklin W. B. Proteolipid promoter activity distinguishes two populations of NG2-positive cells throughout neonatal cortical development. J. Neurosci. 22, 876–885 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan X. et al. Expression of the green fluorescent protein in the oligodendrocyte lineage: a transgenic mouse for developmental and physiological studies. J. Neurosci. Res. 70, 529–545 (2002). [DOI] [PubMed] [Google Scholar]
- Peters A. et al. Th17 cells induce ectopic lymphoid follicles in central nervous system tissue inflammation. Immunity 35, 986–996 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini B., Rosicarelli B., Magliozzi R., Stigliano E. & Aloisi F. Detection of ectopic B-cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain Pathol. 14, 164–174 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aloisi F. & Pujol-Borrell R. Lymphoid neogenesis in chronic inflammatory diseases. Nat. Rev. Immunol. 6, 205–217 (2006). [DOI] [PubMed] [Google Scholar]
- Fritzsching B. et al. Intracerebral human regulatory T cells: analysis of CD4+ CD25+ FOXP3+ T cells in brain lesions and cerebrospinal fluid of multiple sclerosis patients. PLoS One 6, e17988 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal H. C. & Agrawal D. Proteolipid protein and DM-20 are synthesized by Schwann cells, present in myelin membrane, but they are not fatty acylated. Neurochem. Res. 16, 855–858 (1991). [DOI] [PubMed] [Google Scholar]
- Goverman J. M. Immune tolerance in multiple sclerosis. Immunol. Rev. 241, 228–240 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravel M., Di Polo A., Valera P. B. & Braun P. E. Four-kilobase sequence of the mouse CNP gene directs spatial and temporal expression of lacZ in transgenic mice. J. Neurosci. Res. 53, 393–404 (1998). [DOI] [PubMed] [Google Scholar]
- Nave K. A., Lai C., Bloom F. E. & Milner R. J. Splice site selection in the proteolipid protein (PLP) gene transcript and primary structure of the DM-20 protein of central nervous system myelin. Proc. Natl. Acad. Sci. U. S. A. 84, 5665–5669 (1987). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernier L. et al. Molecular cloning of a 2′,3′-cyclic nucleotide 3′-phosphodiesterase: mRNAs with different 5′ ends encode the same set of proteins in nervous and lymphoid tissues. J. Neurosci. 7, 2703–2710 (1987). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu W. P., Collarini E. J., Pringle N. P. & Richardson W. D. Embryonic expression of myelin genes: evidence for a focal source of oligodendrocyte precursors in the ventricular zone of the neural tube. Neuron 12, 1353–1362 (1994). [DOI] [PubMed] [Google Scholar]
- Belachew S., Yuan X. & Gallo V. Unraveling oligodendrocyte origin and function by cell-specific transgenesis. Dev. Neurosci. 23, 287–298 (2001). [DOI] [PubMed] [Google Scholar]
- Lee J. W. et al. Peripheral antigen display by lymph node stroma promotes T cell tolerance to intestinal self. Nat. Immunol. 8, 181–190 (2007). [DOI] [PubMed] [Google Scholar]
- Schildknecht A. et al. Antigens expressed by myelinating glia cells induce peripheral cross-tolerance of endogenous CD8+ T cells. Eur. J. Immunol. 39, 1505–1515 (2009). [DOI] [PubMed] [Google Scholar]
- Na S. Y. et al. Naive CD8 T-cells initiate spontaneous autoimmunity to a sequestered model antigen of the central nervous system. Brain 131, 2353–2365 (2008). [DOI] [PubMed] [Google Scholar]
- Goverman J. Autoimmune T cell responses in the central nervous system. Nat. Rev. Immunol. 9, 393–407 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxena A. et al. Cutting edge: Multiple sclerosis-like lesions induced by effector CD8 T cells recognizing a sequestered antigen on oligodendrocytes. J. Immunol. 181, 1617–1621 (2008). [DOI] [PubMed] [Google Scholar]
- Walter L. & Albert M. L. Cutting edge: cross-presented intracranial antigen primes CD8+ T cells. J. Immunol. 178, 6038–6042 (2007). [DOI] [PubMed] [Google Scholar]
- Li M. et al. Cell-associated ovalbumin is cross-presented much more efficiently than soluble ovalbumin in vivo. J. Immunol. 166, 6099–6103 (2001). [DOI] [PubMed] [Google Scholar]
- de Vos A. F. et al. Transfer of central nervous system autoantigens and presentation in secondary lymphoid organs. J. Immunol. 169, 5415–5423 (2002). [DOI] [PubMed] [Google Scholar]
- Greter M. et al. Dendritic cells permit immune invasion of the CNS in an animal model of multiple sclerosis. Nat. Med. 11, 328–334 (2005). [DOI] [PubMed] [Google Scholar]
- Reboldi A. et al. C-C chemokine receptor 6-regulated entry of TH-17 cells into the CNS through the choroid plexus is required for the initiation of EAE. Nat. Immunol. 10, 514–523 (2009). [DOI] [PubMed] [Google Scholar]
- Battistini L. et al. CD8+ T cells from patients with acute multiple sclerosis display selective increase of adhesiveness in brain venules: a critical role for P-selectin glycoprotein ligand-1. Blood 101, 4775–4782 (2003). [DOI] [PubMed] [Google Scholar]
- Kerfoot S. M. & Kubes P. Overlapping roles of P-selectin and alpha 4 integrin to recruit leukocytes to the central nervous system in experimental autoimmune encephalomyelitis. J. Immunol. 169, 1000–1006 (2002). [DOI] [PubMed] [Google Scholar]
- Doerflinger N. H., Macklin W. B. & Popko B. Inducible site-specific recombination in myelinating cells. Genesis 35, 63–72 (2003). [DOI] [PubMed] [Google Scholar]
- Lappe-Siefke C. et al. Disruption of Cnp1 uncouples oligodendroglial functions in axonal support and myelination. Nat. Genet. 33, 366–374 (2003). [DOI] [PubMed] [Google Scholar]
- Leone D. P. et al. Tamoxifen-inducible glia-specific Cre mice for somatic mutagenesis in oligodendrocytes and Schwann cells. Mol. Cell. Neurosci. 22, 430–440 (2003). [DOI] [PubMed] [Google Scholar]
- Ji Q., Castelli L. & Goverman J. M. MHC class I-restricted myelin epitopes are cross-presented by Tip-DCs that promote determinant spreading to CD8(+) T cells. Nat. Immunol. 14, 254–261 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiber H. A. et al. Dendritic cells in chronic mycobacterial granulomas restrict local anti-bacterial T cell response in a murine model. PLoS One 5, e11453 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material