Abstract
We have recently shown that there is a heightened stress response after a mild traumatic brain injury (TBI) during the first 2 post-injury weeks. This corresponds to the same post-injury period when exercise does not increase brain-derived neurotrophic factor (BDNF) and autonomic dysfunction becomes evident with exercise. Here we determined stress and autonomic responses to voluntary and forced exercise at a post-injury time window when exercise has been found to elicit beneficial effects. Rats underwent a mild fluid percussion injury and were exercised at post-injury days 28–32 and 35–39. Cardiac and temperature autonomic function were evaluated. Hippocampal tissue was obtained immediately after exercise for analysis of BDNF. In contrast to the sub-acute period, corticosterone and adrenocorticotropic hormone responses to exercise were normalized in the TBI group. Irrespective of injury, forced exercise markedly stimulated the corticotrophic axis and did not increase BDNF. BDNF levels were increased with voluntary exercise in all animals. Rats exposed to forced exercise had lower activity levels during periods of non-exercise. This effect was more pronounced in the TBI rats. Cardiac and temperature autonomic responses to delayed exercise also recuperated. Rats with TBI that underwent forced exercise, however, had higher core body temperatures during experimental manipulations, thus suggesting that exposure to a potent stressor facilitates responsiveness to environmental stimulations.
Key words: : brain derived neurotrophic factor, corticosterone, exercise, temperature
Introduction
Exercise enhances cognitive function and facilitates neuroplasticity.1,2 Given the beneficial effects of exercise, it has been suggested as a rehabilitative intervention for traumatic brain injury (TBI).3 TBI is a concerning public health problem. Approximately 1.4 to 3.8 million concussions occurs each year in the United States alone.4 TBI has a profound effect on quality of life. Even TBI classified under the mild or moderate range is associated with persisting cognitive and affective disturbances.5–8
We have shown, in a rodent model of TBI, that voluntary exercise facilitates recovery by increasing levels of brain-derived neurotrophic factor (BDNF) when it occurs at a delayed time window.9 BDNF facilitates the synapse and enhances neurotransmitter release.10,11 These exercise-induced increases in BDNF have been associated with cognitive enhancement.12 In contrast to delayed post-traumatic exercise, sub-acute exercise (i.e., first 2 post-injury weeks) does not increase BDNF and worsens cognitive function. It is particularly during the first post-injury weeks that the pathophysiological effects of mild TBI are more noticeable. Along these lines, we have recently shown that the regulation of the hypothalamic-pituitary-adrenal (HPA) axis is altered in that the response to stress is heightened during the subacute post-injury period.13,14 It is likely that BDNF is not increased with sub-acute exercise because of corticosterone (CORT) elevations.15,16 Moreover, we have recently reported that cardiac and temperature autonomic dysfunction becomes evident with sub-acute exercise, particularly when it elicits a pronounced response of the corticotrophic axis.17
Here we studied the effects of voluntary and forced exercise on the stress response during the same post-injury period that voluntary exercise has previously been shown to be effective. CORT, adrenocorticotropic hormone (ACTH), and BDNF responses to exercise were determined. We also explored if cardiac and temperature responses to exercise resolved during this delayed post-TBI period.
Methods
Subjects
A total of 57 male Sprague-Dawley rats (mean weight: 267g±2.53 standard error of the mean [SEM]) from Charles River Breeding Labs (Hollister, CA) were used in these experiments. Rats were chosen at random to undergo surgery to induce either sham injury (n=28) or a lateral fluid percussion injury (FPI) (n=29). Animals were handled daily and habituated to a reversed lighting schedule (lights off: 09:30 to 21:30 h). During the experiments, rats were single-housed in opaque plastic bins (50.8×25.4×25.4 cm), which were lined with bedding material. Rats had ad lib access to water and rat chow. All procedures were performed in accordance with the United States National Institutes of Health Guide for the Care and Use of Laboratory Animals and were approved by the UCLA Chancellor's Animal Research Committee.
Lateral FPI
Rats were anesthetized with isofluorane via a nose mask. The level of anesthesia was monitored by level of respiration, muscular relaxation, and pedal reflexes. After loss of pedal reflexes, the scalp and scapular regions were shaved, the animal was secured in a stereotaxic head frame, and the scalp was cleansed with ethanol and povidone-iodine. Rectal temperature was monitored and maintained between 36.5–38.0°C with a thermostatically controlled heating pad (Braintree Scientific Inc., Braintree, MA). The scalp and temporal muscle were reflected and a 3-mm diameter circular craniotomy was made over the left parietal cortex, centered at 3 mm posterior to bregma and 6 mm lateral to the midline. The bone flap was removed and the dura left intact in all animals to receive FPI. The dura was inspected with the aid of a microscope (Wild, Heerburg, Switzerland) to assure that it was intact.
A plastic injury cap was placed over the craniotomy with silicone adhesive, cyanoacrylate, and dental cement. When the dental cement hardened, the cap was filled with 0.9% NaCl solution. Anesthesia was discontinued and the animal was removed from the stereotaxic device. The injury cap was attached to the fluid percussion device. At the first sign of hind-limb withdrawal to a paw pinch, a mild/moderate fluid percussion pulse (1.5 atm) was administered. Apnea times were determined as the time from injury to the return of spontaneous breathing. Time of unconsciousness was determined from the time of injury until the return of the hind-limb withdrawal reflex. Immediately on responding to a paw pinch, anesthesia was restored, the injury cap removed, and the scalp was sutured.
Control sham animals underwent an identical preparation with the exception of the FPI. After suturing, bupivacaine (0.25 mg) was injected into the margins of the scalp incision and triple antibiotic ointment was applied over the incision. The rat was placed in a recovery chamber for approximately 1 h before being returned to its cage. All injuries were performed before 12:00 h.
Transmitter implantation
Three weeks after FPI and 1 week before commencing exercise, rats were implanted with telemetry devices (Respironics Mini Mitter, Bend, OR) to monitor heart rate (HR), core body temperature (CBT), and gross motor activity. As previously described,17 rats were anesthetized with isofluorane (4% for induction and 2.0% for maintenance in 100% O2) via a nose mask. When the animal was fully anesthetized, the ventral surface of the abdomen was shaved and cleansed with ethanol and povidone-iodine. A midline, abdominal skin incision was made followed by an incision along the linea abla. The transmitter was then positioned in the abdominal cavity.
Positive and negative leads from the transmitter were pushed through the abdominal wall, which was then sutured with absorbable material. A small incision of the skin was made near the right clavicle to allow for the end of the negative lead to be pushed subcutanously and sutured to the pectoralis superficialis. A small skin incision was then made to the left of the xiphoid process and cranial to the last rib. The positive lead was then pushed subcutanously and sutured to a chest muscle. Skin was sutured and bupivacaine (0.25 mg) was injected at the wound site and triple antibiotic ointment was applied over the incision.
Forced and voluntary wheel exercise
Animals were randomly assigned to either voluntary exercise (vRW), forced exercise (fRW), or sedentary (Sed) conditions. Exposure to exercise commenced 4 weeks after the FPI and sham injuries. Rats in the vRW condition were placed in cages equipped with a running wheel (RW, diameter=31.8 cm, width=10 cm; Nalge Nunc International, Rochester, NY) that rotated against a resistance of 100 g. These animals were allowed to exercise from post-injury days (PIDs) 28–32 and PIDs 35–39. To make exercise conditions more clinically relevant, a 2-day lapse in exercise was applied. Exercise was quantified by recording the number of wheel revolutions per hour using VitalView Data Acquisition System software (Respironics Mini Mitter Company Inc., Bend, OR). Rats in the fRW condition were exposed to wheels with an attached motor that allowed for speed to be individually controlled (RW, diameter=35.6 cm, width=10.92 cm; Lafayette Instruments, Lafayette, IN). These animals received two daily 20-min exercise sessions (10:00 h and 14:00 h).
CORT and ACTH radioimmunoassays
Blood was collected by tail venepuncture before exercise exposure to obtain baseline values. To determine the response to exercise, blood collections were obtained during the first day of exercise (PID 28) and on PIDs 32, 35, and 39. All blood samples were obtained between 14:00 and 16:00 h during the active dark phase. For those animals under the fRW condition, samples were obtained 5 min after exercise. Rats under the vRW condition were exercising when removed from their cage to obtain blood samples. After the last blood collection on PID 39, rats were sacrificed, and the hippocampus was dissected for further analysis of BDNF. The thymus and adrenal glands were removed and weighed.
Blood samples (250 μL/sample) were collected in ethylenediaminetetraacetic acid-micro collection tubes with added trasyol (Aprotinin, Sigma; 200 kIU/mL). Blood samples were then centrifuged at 2000 rpm for 20 min at 4o C, plasma was separated, aliquoted, and stored at −80o C until assayed for CORT and ACTH. Plasma CORT was assayed with a commercial rat CORT 125I-RIA kit (MP Biomedicals, Inc, Orangeburg, NY) according to the vendor's instructions, as done previously.13 The reported detection limit for the CORT assay is 8 ng/mL and intra- and interassay coefficients of variation are lower than 10.3% and 7.2%, respectively. The results are expressed as ng/mL of plasma. Plasma ACTH levels were assessed with a human ACTH 125I-RIA kit (DiaSorin Corp., Stillwater, MN), according to the vendor's instructions, as done previously.13 The reported detection limit of this assay is 15 g/mL and intra- and interassay coefficients of variation are lower than 10.7% and 5.7%, respectively. The results are expressed as pg/mL of plasma.
Assay for BDNF
BDNF protein was quantified using an enzyme-linked immunosorbent assay kit (Chemikine BDNF; Millipore, Billerica, MA) according to the manufacturer's instructions. Absorbance at 450 nm was measured using an automated microplate reader (BIO-RAD Model 3550, Bio-Rad Laboratories, Hercules, CA). Standards were assayed with the samples on each plate. Duplicate measures were averaged and values were corrected for total amount of protein (as described above) in the sample to derive the pg amount of BDNF protein/mg of total protein.
Data collection and statistical analysis
Telemetry data were collected every minute for the duration of the experiment. This allowed us to determine changes in CBT and HR as a response to exercise. This form of data collection was particularly useful for the animals under the vRW condition because the amount of wheel revolutions is variable. To obtain values for CBT and HR as a response to vRW, only periods with a minimum of 4 consecutive min of exercise were used. Amount of vRW exercise was detected as wheel revolutions. CBT and HR were then normalized to the duration of continuous exercise. In contrast, because the fRW was for a fixed duration, we were able to compare variables regarding fRW recovery by analyzing data collected from the 20 min immediately after the fRW session. Post-vRW values were not obtained because of lack of a prolonged continuous rest period immediately after a bout of vRW. Average values for each daily 12 h light/dark cycle were also calculated for overall analysis of HR, CBT, and activity during periods of non-exercise. This allowed us to detect increases of measured variables at particular hours (i.e., peaks).
Telemetry and the above-described peak data was analyzed by using a Mixed Model Repeated measures analysis where injury (FPI and sham) and exercise (vRW, fRW, Sed) differences were evaluated within time (i.e., PIDs). Differences in individual group means were compared with a significance set at p<0.05 after adjusting for multiple comparisons (Bonferroni corrected) (SPSS Inc., NY). Bonferroni adjusted values are quoted below.
Results
Subjects
Injured rats had a mean (±SEM) unconsciousness duration of 127±9 sec and a mean apnea duration of 23±5 sec. No gross motor impairments of ambulatory ability were observed in any of the injured rats. There were no differences in adrenal or thymus weights of either FPI or sham groups on PID 39, irrespective of exercise condition.
Forced and voluntary exercise
No differences were observed between injury groups when fRW speed was analyzed. A significant time effect was observed across all groups [F(9,85)=4.05, p<0.0005]. Bonferroni corrected comparisons indicated significantly lower running speeds in all animals at the first day of fRW exercise (i.e., PID 28) compared with the other PIDs except PID 29 (p<0.005). PID 29 was significantly different to all days except PID 28.
No injury effects were found in vRW performance during the dark or light phases. Analysis of the number of wheel revolutions during the 12 h dark phase, however, indicated a significant time effect [F(9,129)=3.77, p<0.0005]. Bonferroni corrected comparisons indicated that rats exercised more during the second week of vRW exposure, reaching significance on PID 35, 37, and 38 compared with PID 28–30 (p<0.05). No significant injury or time effects were observed for endurance (6.74 mean±1.6 SEM). Endurance was analyzed as consecutive minutes of exercise when exposed to the vRW.
Activity levels during periods of non-exercise.
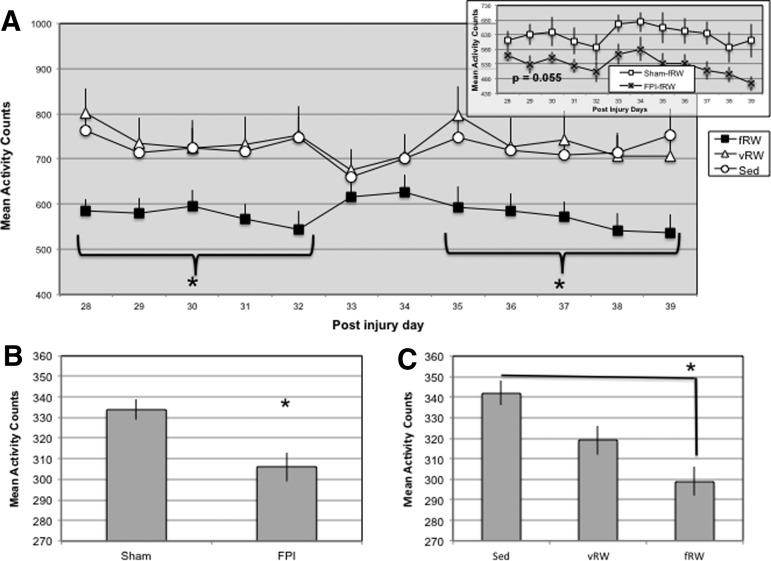
Before the initiation of exercise interventions, no significant differences for overall activity were observed between FPI and sham animals. Significant effects were evident once vRW and fRW exercise were initiated (i.e., PID 28), however. Activity counts, during the non-exercise periods within the dark 12 h period, indicated a significant main effect for exercise F(2,61)=11.26, p<0.0005). Bonferroni corrected comparisons revealed that activity counts were lower in the fRW rats, compared with vRW (p<0.0005) and Sed (p<0.005) groups, a significant Exercise×Time interaction [F(22,464)=3.51, p<0.0005]. Bonferroni corrected comparisons revealed that activity was particularly lower in the fRW group at PIDs 28–32 and 35–39 (p<0.05). It should be noted that activity counts tended to be lower in the FPI-fRW animals compared with sham-fRW (p=0.055); however, significance was not reached (Fig. 1A).
FIG. 1.
Ambulatory activity during the dark 12-h period for rats under sedentary (Sed), forced (fRW), and voluntary (vRW) exercise conditions. Insert indicates fRW speed for sham and fluid percussion injured (FPI) rats (A). FPI rats had less activity counts during the light 12-h period (B). Activity counts were lower in the fRW group during the light period (C). Each value represents the mean number of activity counts in a 1-h sampling interval±standard error of the mean. *p<0.05.
Analysis of activity levels during the 12-h light period showed a main injury effect. FPI rats were more inactive than the sham rats F(1,84)=5.75, p<0.05) (Fig. 1B). A significant main effect for exercise was also found during the 12-h light period F(2,84)=4.93, p<0.05). Bonferroni corrected comparisons indicated significantly lower levels of activity in fRW group compared with the Sed (Fig. 1C).
Overall HR
HR was analyzed 72 h before the initiation of exercise interventions. Although no significant injury effects were observed between FPI and sham, FPI rats tended to have a higher HR during the light phase (p=0.07).
HR was also analyzed after exercise was initiated. A significant main effect for Time was found during the 12-hour dark cycle [F(11,513)=5.79 p<0.0005). Although mean HR values were higher in all the FPI groups, compared with shams, significance was not obtained (Fig. 2A). Analysis of HR during the light cycle indicated that overall HR decreased across time. This was supported by a significant Time effect [F(11,492)=2.49 p<0.005) (Fig 2B).
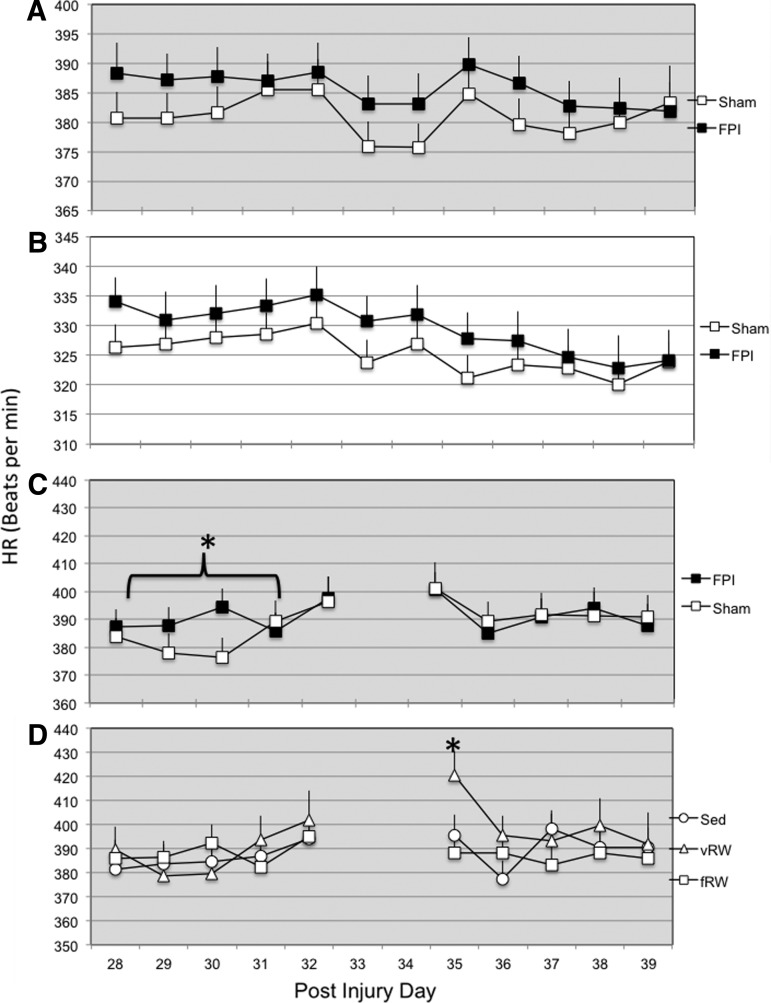
FIG. 2.
Heart rate (HR) of sham and fluid percussion injured (FPI) rats changed across experimental days during the dark (A) and light (B) periods. An increase in HR was evident at 14:00 h. These increases were more pronounced in FPI animals during the first week of exercise (C). Increases in HR were more pronounced in animals exposed to the vRW at 14:00 h during postinjury day 35 (D). Each value represents the mean HR (beats per min)±standard error of the mean. *p<0.05.
HR as a response to exercise
No significant differences in HR, between FPI and sham animals, were observed when analyzing the 20 min after fRW. Likewise, no injury effects for HR were observed during vRW. Two consistent peaks for HR were detected when average telemetry values for each hour were calculated. These occurred at 10:00 and 14:00 h, within the dark 12-hour cycle during days of exercise. Peaks occurred at the same time across the experimental days and coincided with the initiation time of the fRW sessions. Analysis of the 10:00 h HR peak indicated an injury effect during the first week of exercise by a significant Injury×Time interaction [F(9,450)=5.6, p<0.05] (Fig. 2C). A significant Exercise×Time interaction was also observed [F(18,450)=3.03, p<0.0005]. Analysis of the 10:00 h HR peak, through Bonferroni corrected comparisons, indicated that the vRW group had a higher HR on PID 35 compared with animals under the fRW condition (p<0.05) (Fig. 2D). Although the HR at 14:00 h was higher in the FPI-fRW group compared with the Sham-fRW group (mean beats per min: 404±2.98, SEM and 388±3.81, SEM respectively, significance was not obtained.
Overall CBT
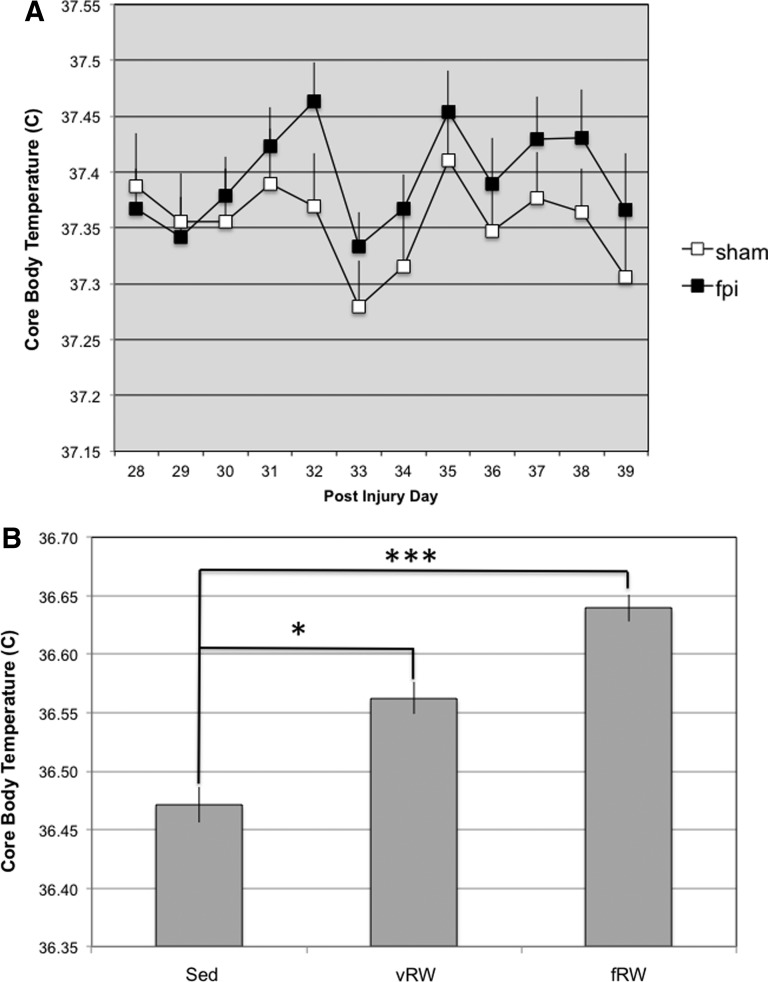
No significant effects were found for CBT during the 72 h before the initiation of exercise interventions. CBT was also analyzed after exercise was initiated. A significant main effect for Time was found during the 12-h dark cycle [F(11,466)=8.92, p<0.005] (Fig. 3A). Analysis of CBT during the light cycle revealed a significant main effects for Time [F(10,380)=5.04, p<0.005] and for Exercise [F(2,90)=12.1, p<0.0005]. Bonferroni corrected comparisons indicated that CBT was higher in fRW compared with Sed (p<0.0005) and in vRW compared with Sed (p<0.05). Comparison between vRW and fRW only did not reach significance (p=0.08) (Fig. 3B).
FIG. 3.
Core body temperature (CBT) of sham and fluid percussion injured (FPI) rats. CBT values varied across time during the dark cycle (A). CBT, during the light cycle, was influenced by exercise condition (Sedentary [Sed], voluntary exercise [vRW], forced exercise [fRW]) (B). Each value represents the mean±standard error of the mean. *p<0.05, ***p<0.0005.
CBT as a response to exercise
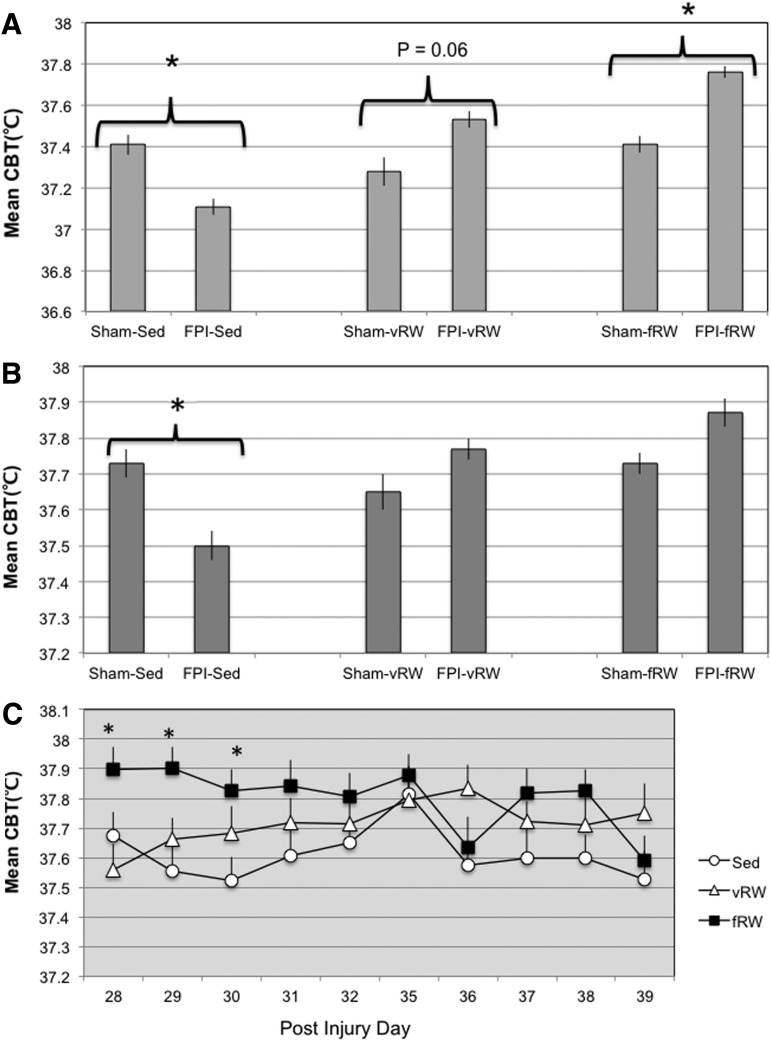
No significant differences in CBT between FPI and sham animals were observed when analyzing the 20 min after fRW. Likewise, no injury effects for CBT were observed during vRW. Two consistent peaks for CBT were detected when average telemetry values for each hour were calculated. These occurred at 10:00 and 14:00 h, within the dark 12-h cycle during days of exercise. Peaks occurred at the same time across the experimental days and coincided with the initiation time of the fRW sessions. Analysis of the 10:00 h CBT peak indicated an Injury×Exercise interaction [F(2,67.65)=7.0, p<0.005]. Further analysis, with Bonferroni corrected comparisons, indicated that CBT was higher in the FPI exercised groups, reaching significance when comparing FPI-fRW and sham-fRW (p<0.05). Although the CBT appeared to be higher in FPI-vRW animals compared with sham-vRW, significance was not obtained (p=0.06). CBT was lower in the FPI animals under Sed conditions (p<0.05) (Fig 4A).
FIG. 4.
An increase in core body temperature (CBT) was evident at 10:00 h post injury. These increases were more pronounced in fluid percussion injured (FPI) animals exposed to the forced (fRW) and voluntary (vRW) exercise groups. CBT was lower in the FPI-sedentary (Sed) group (A). CBT was also lower at 14:00 h in the FPI-Sed group (B). CBT peaks at 14 h were dependent on exercise condition and post-injury day (C). Each value represents the mean±Standard error of the mean. *p<0.05.
A significant effect for Time was also observed [F(9, 366.04)=1,4, p<0.0005]. This was mostly attributed to a raise in CBT at PID 35 compared with other PIDs. Analysis of the 14:00 h peak showed a significant Injury×Exercise interaction [F(2,80)=4.52, p<0.05]. Bonferroni corrected comparisons showed that interaction significance is mostly attributed to significantly lower CBT values in the FPI-Sed compared with sham-Sed (p<0.05) (Fig 4B). A significant Exercise×Time interaction was observed [F(18,347)=1.78, p<0.05]. Bonferroni corrected comparisons revealed that CBT was higher in the fRW groups compared with Sed groups at PID 29 and 30 (p<0.05). CBT in the fRW was also higher compared with vRW at PID 28 (p<0.05) (Fig. 4C). These effects were supported by significant main effects for Exercise [F(2,80)=3.93, p<0.05] and Time [F(9,347)=2.4, p<0.05].
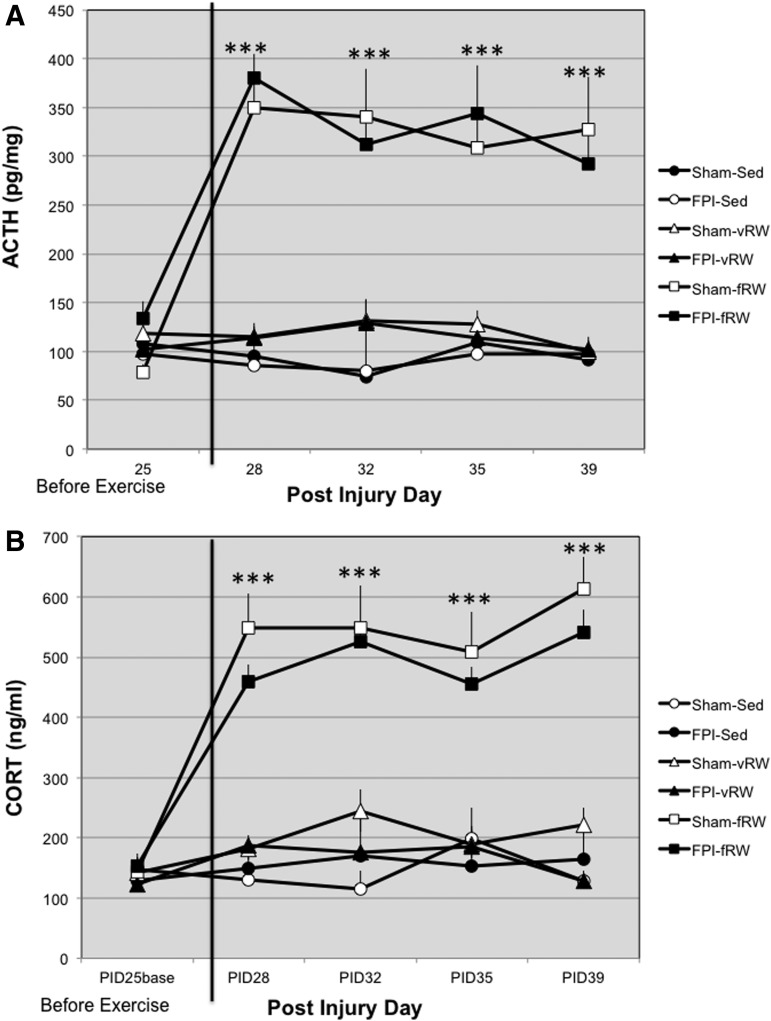
CORT and ACTH
There were no differences in ACTH and CORT, between FPI and sham rats before initiating exercise. Exercise had a strong influence on levels of ACTH [F(2,58)=98.62, p<0.0005]. Bonferroni corrected comparisons indicated that levels of ACTH in the fRW condition were higher compared with both vRW and Sed (p<0.0005) (Fig. 5A). Analysis of CORT revealed similar findings. A significant Exercise×Time interaction was observed [F(6,149)=2.14, p<0.05]. Bonferroni corrected comparisons indicated levels of CORT in the fRW condition were higher compared with both vRW and Sed at all time points (p<0.0005). This was supported by a main effect for Exercise [F(2,68)=132.28, p<0.0005]. (Fig. 5B).
FIG. 5.
Plasma adrenocorticotropic hormone (ACTH) collected pre-exercise and on post-injury days 28, 32, 35, and 39; 5 min after forced exercise (fRW); and randomly during the same 14:00–16:00 h period in voluntary exercising (vRW) and sedentary (Sed) sham and fluid percussion injured (FPI) animals (A). Plasma cortiscosterone (CORT) collected pre-exercise and on post-injury days 28, 32, 35, and 39; 5 min after fRW; and randomly during the same 14:00–16:00-h period in vRW and Sed sham and FPI animals (B). Each value represents the mean±standard error of the mean. ***p<0.0005.
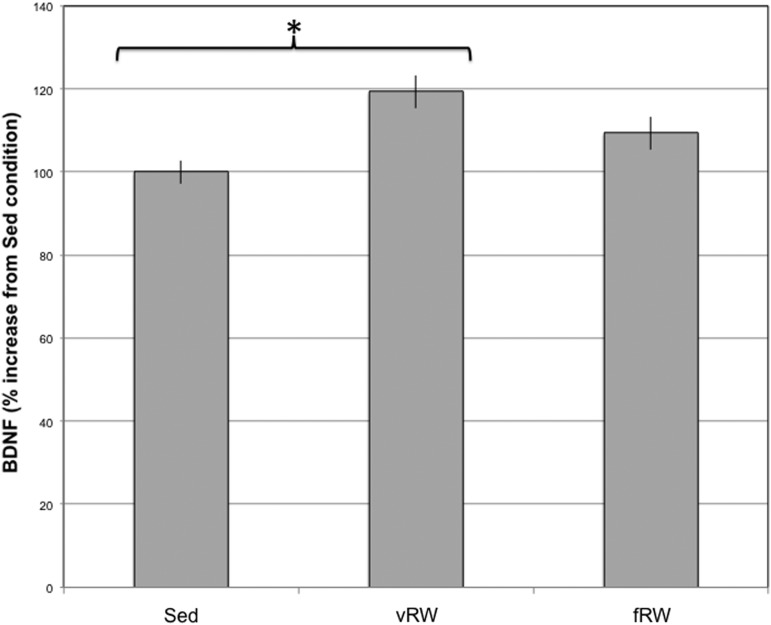
BDNF
Animals under the vRW condition had higher levels of BDNF compared with Sed (p<0.05). This was supported by a significant main effect for Exercise [F(2, 52)=5.4, p<0.05]. (Fig. 6). Increases in BDNF were correlated to the amount of vRW revolutions for the FPI (Adjusted R2=0.69, p<0.005) and sham (Adjusted R2=0.71, p<0.005) groups.
FIG. 6.
Hippocampal brain-derived neurotrophic factor (BDNF) levels at post-injury day 39 after forced (fRW) or voluntary (vRW) exercise compared with sedentary (Sed) condition.
Discussion
Responsiveness to exercise is recovered during the delayed post-injury period
Here we show, in mild/moderate FPI rats, that the stress response to exercise, as determined through ACTH and CORT, has recovered when exercise was delayed by 28 days. Recently, we observed that fRW is a potent stimulus for the HPA axis and that rats with FPI are slower to habituate to this type of exercise when it occurs during the first two post-injury weeks.18 Contrasting with sub-acute exercise, the stress response to delayed fRW exercise in the FPI group did not differ from sham controls.
The response to vRW was also recovered in the FPI group, as determined by increases in BDNF. Exercise-induced BDNF elevations are not observed when vRW occurs during the sub-acute period.9,19 Here we again demonstrated that delayed vRW exercise leads to BDNF increases in FPI rats. BDNF was not increased in animals that underwent fRW. The lack of increase in BDNF in the sham-fRW group was not unexpected and is in accordance with recent studies.18 Given the suppressive effects of glucocorticoids on BDNF,20 it is likely that the negative effects of fRW on BDNF were related to the pronounced elevations in ACTH and CORT found with fRW. It is yet to be determined if prolonged fRW exposure would result in BDNF elevations once animals habituated to the fRW.
Activity levels during the delayed post-injury period
Circadian disruptions are evident in rats with FPI during the sub-acute period.17 This is in accord with sleep disturbances that are commonly observed in patients after TBI21 and are associated with neuroendocrine alterations manifested as HPA circadian rhythm disruptions.22 Here we found no evidence of circadian disruption as indicated by the amount of activity counts and vRW exercise during the light inactive period suggesting that HPA circadian rhythm has recovered by this later period.
Fatigue, which is also a common complaint in patients after a concussion,23 was also evident in FPI rats during the sub-acute period.17 Analysis of endurance during vRW exercise indicated no evidence of fatigue. When activity counts, indicative of ambulatory activity, were analyzed, however, effects suggestive of fatigue were observed in FPI rats. Decreases in activity were more pronounced in animals that had fRW exposure and thus a substantial increase in CORT. Activity counts, during the active dark period, were lower in both FPI and sham animals exposed to the fRW. Interestingly, activity decreases were not observed during the non-exercise days (i.e., PID 33 and 34).
Looking closely at the data, obtained during the dark period, it seems that this effect is mostly attributed to the levels of activity of the FPI-fRW group. Although significance was only approximated, FPI-fRW activity counts, during the active dark period, were consistently lower across all days including PID 33 and 34. We recently reported that activity counts are lower in FPI rats that are exposed to fRW during the sub-acute period.17 This effect becomes evident during the light inactive period, because rats with FPI are less active compared with shams. This decrease in activity, during the light period, might be attributed to exercise after a FPI. All animals under exercise conditions, particularly fRW, had lower activity levels during the light period. Although not statistically significant, activity levels consistently tended to be lower in the FPI-fRW and FPI-vRW compared respectively with sham-fRW and sham-vRW.
Clinically, fatigue is most prevalent during the first post-injury week when neuroendocrine component is evident23 and is in accord with our previous findings in an experimental TBI model. Persistence of fatigue is likely to be influenced by other factors such as depression and anxiety24,25; thus, it is worth mentioning that activity counts were lower in those animals that had marked HPA stimulation through exercise.
CBT and HR as a response to exercise
During the sub-acute period, alterations in temperature regulation become evident with exercise. The CBT of FPI rats remains elevated after sub-acute forced exercise.17 Here we show that impairments in thermoregulation have begun to recover. All animals had elevations in CBT as a result of exercise, predominantly when it was forced. Although FPI rats tended to have higher CBTs compared with shams, these were not significant. Notwithstanding, TBI-related increases in CBT became evident during the morning session of fRW. These increases are likely because of an increased responsiveness to environmental stimulations. CBT was also elevated during the second session of fRW, particularly during the first days of exercise. To a lesser extent, increases in CBT were also observed in those animals that had access to the vRW groups. It should be noted that rats under the vRW groups were exercising during the morning and afternoon fRW sessions. Paradoxically, the CBT was lower in the FPI-Sed animals during both fRW sessions.
HR increases were also found on the days of exercise. Again, these increases only tended to be more pronounced in the FPI groups. There was evidence of increased responsiveness to stimulations because elevations in HR were evident during the FRW sessions, particularly for the FPI animals during the first week of exercise.
Conclusions
Previously, we have shown evidence of hyperresponsiveness to exercise during the sub-acute period. There is an increased sensitivity to stressful events during the first post-injury weeks, as determined by analyzing the HPA axis regulation after restraint-induced stress.13,26 Here we show that recovery of the stress response, as indicated by ACTH and CORT, coincides with the period of responsiveness to exercise. In spite of this, it is likely that neuroendocrine alterations may still influence autonomic function given that FPI rats exposed to a potent stressor (i.e., fRW) were more responsive to experimental manipulations. These findings are reminiscent of human mild TBI, where cognitive impairments and affective disturbances may persist beyond the sub-acute period.
Acknowledgments
We thank Ramin Rajai, Hans Sebastian, and Sam Kazemian for their excellent technical assistance. This research was supported by NIH grant NS06190 to GSG and the UCLA Brain Injury Research Center.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Hillman C.H., Erickson K.I., and Kramer A.F. (2008). Be smart, exercise your heart: exercise effects on brain and cognition. Nat. Rev. Neurosci. 9, 58–65 [DOI] [PubMed] [Google Scholar]
- 2.Farmer J., Zhao X., van Praag H., Wodtke K., Gage F.H., and Christie B.R. (2004). Effects of voluntary exercise on synaptic plasticity and gene expression in the dentate gyrus of adult male Sprague-Dawley rats in vivo. Neuroscience 124, 71–79 [DOI] [PubMed] [Google Scholar]
- 3.Griesbach G.S. (2011). Exercise after traumatic brain injury: is it a double-edged sword? PM R 3, Suppl 1, S64–S72 [DOI] [PubMed] [Google Scholar]
- 4.Laker S.R. (2011). Epidemiology of concussion and mild traumatic brain injury. PM R 3, Suppl 2, S354–S358 [DOI] [PubMed] [Google Scholar]
- 5.Bazarian J.J., Blyth B., and Cimpello L. (2006). Bench to bedside: evidence for brain injury after concussion—looking beyond the computed tomography scan. Acad. Emerg. Med. 13, 199–214 [DOI] [PubMed] [Google Scholar]
- 6.Rapoport M., McCauley S., Levin H., Song J., and Feinstein A. (2002). The role of injury severity in neurobehavioral outcome 3 months after traumatic brain injury. Neuropsychiatry Neuropsychol. Behav. Neurol. 15, 123–132 [PubMed] [Google Scholar]
- 7.Niogi S.N., Mukherjee P., Ghajar J., Johnson C., Kolster R.A., Sarkar R., Lee H., Meeker M., Zimmerman R.D., Manley G.T., and McCandliss B.D. (2008). Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: a 3T diffusion tensor imaging study of mild traumatic brain injury. AJNR Am. J. Neuroradiol. 29, 967–973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McAllister T.W., Flashman L.A., McDonald B.C., and Saykin A.J. (2006). Mechanisms of working memory dysfunction after mild and moderate TBI: evidence from functional MRI and neurogenetics. J. Neurotrauma 23, 1450–1467 [DOI] [PubMed] [Google Scholar]
- 9.Griesbach G.S., Hovda D.A., Molteni R., Wu A., and Gomez-Pinilla F. (2004). Voluntary exercise following traumatic brain injury: brain-derived neurotrophic factor upregulation and recovery of function. Neuroscience 125, 129–139 [DOI] [PubMed] [Google Scholar]
- 10.Tyler W.J., and Pozzo-Miller L.D. (2001). BDNF enhances quantal neurotransmitter release and increases the number of docked vesicles at the active zones of hippocampal excitatory synapses. J. Neurosci 21, 4249–4258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tyler W.J., Zhang X.L., Hartman K., Winterer J., Muller W., Stanton P.K., and Pozzo-Miller L. (2006). BDNF increases release probability and the size of a rapidly recycling vesicle pool within rat hippocampal excitatory synapses. J. Physiol. 574, 787–803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griesbach G.S., Hovda D.A., and Gomez-Pinilla F. (2009). Exercise-induced improvement in cognitive performance after traumatic brain injury in rats is dependent on BDNF activation. Brain. Res. 1288, 105–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Griesbach G.S., Hovda D.A., Tio D.L., and Taylor A.N. (2011). Heightening of the stress response during the first weeks after a mild traumatic brain injury. Neuroscience 178, 147–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reger M.L., Poulos A.M., Buen F., Giza C.C., Hovda D.A., and Fanselow M.S. (2012). Concussive brain injury enhances fear learning and excitatory processes in the amygdala. Biol. Psychiatry 71, 335–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gronli J., Bramham C., Murison R., Kanhema T., Fiske E., Bjorvatn B., Ursin R., and Portas C.M. (2006). Chronic mild stress inhibits BDNF protein expression and CREB activation in the dentate gyrus but not in the hippocampus proper. Pharmacol. Biochem. Behav. 85, 842–849 [DOI] [PubMed] [Google Scholar]
- 16.Schaaf M.J., de Jong J., de Kloet E.R., and Vreugdenhil E. (1998). Downregulation of BDNF mRNA and protein in the rat hippocampus by corticosterone. Brain Res. 813, 112–120 [DOI] [PubMed] [Google Scholar]
- 17.Griesbach G.S., Tio D.L., Nair S., and Hovda D. A. (2013). Temperature and heart rate responses to exercise following mild traumatic brain injury. J. Neurotrauma 30, 281–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Griesbach G.S., Tio D.L., Vincelli J., McArthur D.L., and Taylor A.N. (2012). Differential effects of voluntary and forced exercise on stress responses after traumatic brain injury. J. Neurotrauma 29, 1426–1433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Griesbach G.S., Gomez-Pinilla F., and Hovda D.A. (2007). Time window for voluntary exercise-induced increases in hippocampal neuroplasticity molecules after traumatic brain injury is severity dependent. J. Neurotrauma 24, 1161–1171 [DOI] [PubMed] [Google Scholar]
- 20.Sutton R.L., Hovda D.A., Chen M.J., and Feeney D.M. (2000). Alleviation of brain injury-induced cerebral metabolic depression by amphetamine: a cytochrome oxidase histochemistry study. Neural. Plast. 7, 109–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Castriotta R.J., and Murthy J.N. (2011). Sleep disorders in patients with traumatic brain injury: a review. CNS Drugs 25, 175–185 [DOI] [PubMed] [Google Scholar]
- 22.Llompart-Pou J.A., Perez G., Raurich J.M., Riesco M., Brell M., Ibanez J., Perez-Barcena J., Abadal J.M., Homar J., and Burguera B. (2010). Loss of cortisol circadian rhythm in patients with traumatic brain injury: a microdialysis evaluation. Neurocri. Care 13, 211–216 [DOI] [PubMed] [Google Scholar]
- 23.Norrie J., Heitger M., Leathem J., Anderson T., Jones R., and Flett R. (2010). Mild traumatic brain injury and fatigue: a prospective longitudinal study. Brain Inj. 24, 1528–1538 [DOI] [PubMed] [Google Scholar]
- 24.Bushnik T., Englander J., and Wright J. (2008). Patterns of fatigue and its correlates over the first 2 years after traumatic brain injury. J. Head Trauma Rehabil. 23, 25–32 [DOI] [PubMed] [Google Scholar]
- 25.Englander J., Bushnik T., Oggins J., and Katznelson L. (2010). Fatigue after traumatic brain injury: Association with neuroendocrine, sleep, depression and other factors. Brain Inj. 24, 1379–1388 [DOI] [PubMed] [Google Scholar]
- 26.Griesbach G.S., Vincelli J., Tio D.L., and Hovda D.A. (2012). Effects of acute restraint-induced stress on glucocorticoid receptors and brain-derived neurotrophic factor after mild traumatic brain injury. Neuroscience 210, 393–402 [DOI] [PMC free article] [PubMed] [Google Scholar]