Abstract
Background and Purpose:
Recently, megavoltage (MV) photon volumetric modulated arc therapy (VMAT) has gained widespread acceptance as the technique of choice for prostate cancer patients undergoing external beam radiation therapy. However, radiation treatment planning for patients with metallic hip prostheses composed of high-Z materials can be challenging due to (1) presence of streak artifacts from prosthetic hips in computed tomography dataset, and (2) inhomogeneous dose distribution within the target volume. The purpose of this study was to compare the dosimetric quality of VMAT techniques in the form of Rapid Arc (RA) for treating low-risk prostate cancer patient with bilateral prostheses.
Materials and Methods:
Three treatment plans were created using RA techniques utilizing 2 arcs (2-RA), 3 arcs (3-RA), and 4 arcs (4-RA) for 6 MV photon beam in Eclipse treatment planning system. Each plan was optimized for total dose of 79.2 Gy prescribed to the planning target volume (PTV) over 44 fractions. All three RA plans were calculated with anisotropic analytical algorithm.
Results:
The mean and maximum doses to the PTV as well as the homogeneity index among all three RA plans were comparable. The plan conformity index was highest in the 2-Arc plan (1.19) and lowest in the 4-Arc plan (1.10). In comparison to the 2-RA technique, the 4-RA technique reduced the doses to rectum by up to 18.8% and to bladder by up to 7.8%. In comparison to the 3-RA technique, the 4-RA technique reduced the doses to rectum by up to 14.6% and to bladder by up to 3.5%.
Conclusion:
Based on the RA techniques investigated for a low-risk prostate cancer patient with bilateral prostheses, the 4-RA plan produced lower rectal and bladder dose and better dose conformity across the PTV in comparison with the 2-RA and 3-RA plans.
Keywords: Avoidance sector, bilateral, prostate cancer, prosthesis, RapidArc, volumetric modulated arc therapy
Introduction
According to the most recent statistics released by the American Cancer Society, prostate cancer will be the most commonly diagnosed cancer in American men in 2013 with an estimation of 238,590 new cases and 29,790 deaths.[1] Prostate cancer is generally diagnosed among older men[2] who may also have osteoarthritis, for which a common treatment is metallic hip replacement. Among treatment options available for prostate cancer, external beam radiation therapy (EBRT) is one of them. Recently, the number of elderly prostate cancer patients with one or two metallic hips requiring EBRT is increasing. However, radiation treatment planning for patients with metallic hips composed of high-Z materials such as Titanium can be challenging due to (1) presence of streak artifacts from prosthetic hips in computed tomography (CT) dataset of the patient [Figure 1], and (2) inhomogeneous dose distribution within the target volume due to attenuation and dose perturbation by the prosthetic hips. Dose reduction between 10% and 64% has been reported in a megavoltage (MV) X-ray beam in the presence of high-Z materials.[3,4,5,6] Furthermore, commercially available treatment planning systems (TPSs) may not accurately predict dose near and beyond the metallic hips, and the limitation of TPS in beam modeling can cause significant errors in the dose calculations.[5,6,7,8,9]
Figure 1.
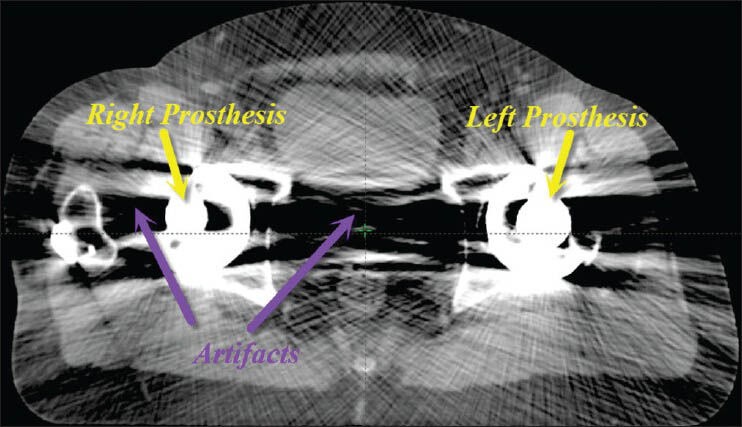
A transversal view of computed tomography slice of prostate cancer patient showing bilateral metallic hip prostheses and artifacts
The American Association of Physicists in Medicine Task Group 63 recommends a treatment plan set up that avoids the beam entrance through the metallic prosthetic devices.[8] Several researchers have investigated the radiation treatment techniques avoiding metallic hips, especially, using intensity modulation radiation therapy (IMRT).[6,10,11,12,13] The IMRT is an advanced form of 3-dimensional conformal radiation therapy that combines intensity modulated beams leading to the construction of highly conformal dose distributions. Recently, a novel radiation technique called volumetric modulated arc therapy (VMAT) was introduced.[14] The VMAT system can deliver a highly conformal radiation dose to the target using one or more arcs, and the delivery technique allows the simultaneous variation of gantry rotation speed, dose rate and multi-leaf collimator field aperture.[14] Since VMAT technique such as RapidArc (RA) (Varian Medical Systems, Palo Alto, CA) can achieve IMRT quality dose distributions with reduction in the treatment delivery time and decrement in the number of monitor units (MUs), VMAT has gained widespread acceptance as the technique of choice for prostate cancer patients undergoing EBRT.[14,15] However, to our best knowledge, no previous studies have been carried out focusing on RA planning for low-risk prostate cancer involving two metallic hips. In this study, we compared the VMAT techniques in the form of RA consisting of two or multiple arcs for treating low-risk prostate cancer patient with bilateral metallic hips (henceforth referred to simply as prostheses).
Materials and Methods
This study describes the treatment of a 58-year-old man with bilateral prostheses, and the patient was diagnosed with adenocarcinoma of the prostate, clinical stage T1cN0M0, Gleason 6, and prostate-specific antigen of 6.2 ng/mL. The patient underwent CT simulation in a supine position with full bladder, and the CT images were acquired with 3 mm spacing using Phillips Brilliance CT Scanner (Philips Health-care, Andover, MA, USA). The CT data set was transferred to the Eclipse TPS, version 11.1 (Varian Medical Systems, Palo Alto, CA). A magnetic resonance imaging (MRI) scan of the patient was then fused with the planning CT scan in order to assist in contouring prostate, seminal vesicles, rectum, bladder, and prostheses on the axial slices of the CT. The clinical target volume (CTV) was defined as the prostate and seminal vesicles, whereas the planning target volume (PTV) was determined by an expansion of the CTV by 5 mm in all other directions. The CT image artifacts from the bilateral prostheses were contoured and assigned with Hounsfield density value of 0 [Figure 2].
Figure 2.
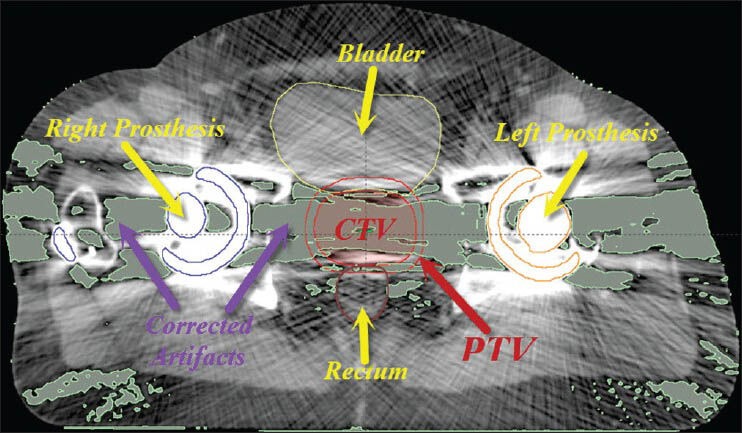
A transversal view of computed tomography slice of prostate cancer patient showing bilateral metallic hip prostheses, corrected artifacts, clinical target volume, planning target volume, bladder, and rectum
The RA planning parameters were set up in the Eclipse TPS using Varian Clinac iX 6 MV X-ray beams. Three RA treatment plans were created with each plan designed for total dose of 79.2 Gy prescribed to the PTV with a daily dose of 1.8 Gy over 44 fractions. First, a RA treatment plan using 2 arcs (2-RA plan) was created using 1st arc in a clockwise direction (arc angle: 181°→179°; collimator angle: 5°) and the 2nd arc in an anti-clockwise direction (arc angle: 179°→181°; collimator angle: 355°). The beam's-eye-view graphics (BEV) in the Eclipse TPS was used to determine the left and right avoidance sectors that would avoid radiation beams entering through left and right prostheses, respectively. However, beams may deliver exit dose to the prostheses. Additionally, the BEV was used to better define the field sizes of coplanar arcs according to the location of the PTV and organs at risk (OARs). The isocenter of the plan was placed at the center of the PTV. Second, a RA treatment plan was created using 3 arcs (3-RA plan) and the planning parameters were same as that of 2-RA plan with an addition of 3rd arc that was identical to the1st arc. Third, a final RA treatment plan was created using 4 arcs (4-RA plan) and the planning parameters were same as that of 2-RA Plan with additions of 3rd and 4th arcs that were identical to the 1st and 2nd arcs, respectively. Furthermore, all 3 RA plans were generated using Progressive resolution optimizer (version 11.1) in the Eclipse TPS, and no modifications of dose-volume constraints and weightings were made during the optimization processes. The optimized RA plans were calculated with Anisotropic Analytical Algorithm, version 11.1, using 2.5 mm dose calculation grid size.
The dose-volume histograms (DVHs) of calculated plans (2-RA, 3-RA, and 4-RA) were generated in the Eclipse TPS. For the PTV, following DVH parameters were evaluated: Mean dose, maximum dose, conformity index (CI) defined as the ratio of volume of the isodose cloud receiving 100% of the prescription dose (V100%) to volume of the PTV, and homogeneity index defined as the ratio of dose at 5% of the PTV (D5%) to dose at 95% of the PTV (D95%). For rectum and bladder, the volumes that received 70 Gy, 60 Gy, 50 Gy, 40 Gy, 30 Gy, and 20 Gy, (V70Gy, V60Gy, V50Gy, V40Gy, V30Gy, and V20Gy, respectively) as well as mean dose were compared. Additionally, the number of MUs and integral dose were compared among 3 RA plans.
Results
The volumes of the PTV, rectum, and bladder were 231.5 cc, 45.6 cc, and 303.4 cc, respectively. Table 1 summarizes the results of the dosimetric parameters of the PTV for the 2-RA, 3-RA, and 4-RA plans. Table 2 and Table 3 summarize the dosimetric results of OARs for the 2-RA, 3-RA, and 4-RA plans. A comparison of DVHs of all 3 RA plans is presented in Figure 3.
Table 1.
Comparison of dosimetric parameters of planning target volume for the 2-RA, 3-RA, and 4-RA plans in a prostate cancer patient with bilateral prostheses
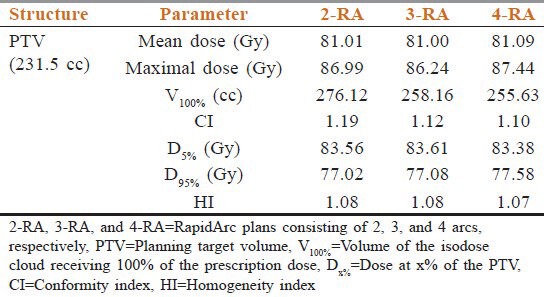
Table 2.
Comparison of dosimetric parameters of rectum for the 2-RA, 3-RA, and 4-RA plans in a prostate cancer patient with bilateral prostheses
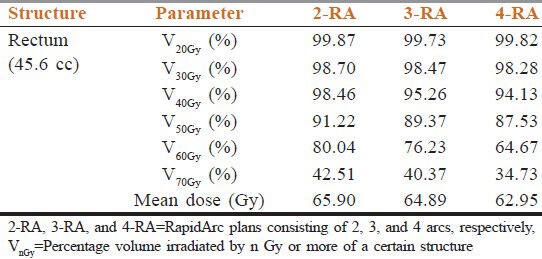
Table 3.
Comparison of dosimetric parameters of bladder for the 2-RA, 3-RA, and 4-RA plans in a prostate cancer patient with bilateral prostheses
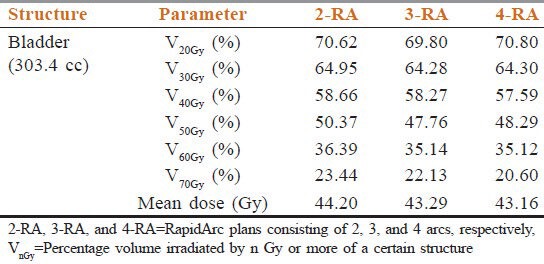
Figure 3.
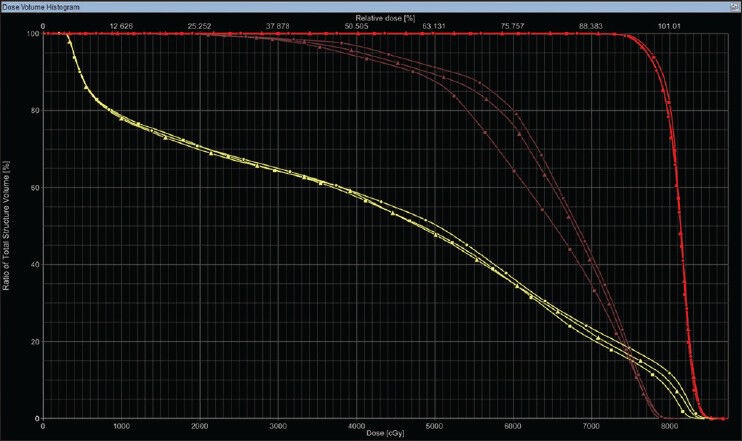
Comparison of dose-volume histograms of rectum (brown color), bladder (yellow color), and planning target volume (red color) of a prostate cancer patient with bilateral prostheses. This figures presents the DVHs among three treatment plans: 2-RapidArc (RA) (circle), 3-RA (triangle), and 4-RA (square) (2-RA, 3-RA, and 4-RA = RapidArc plans consisting of 2, 3, and 4 arcs, respectively)
PTV
The mean PTV dose among 2-RA (81.01 Gy), 3-RA (81.00 Gy), and 4-RA (81.09 Gy) plans were comparable. Similarly, the difference in maximum PTV doses among 2-RA (86.99 Gy), 3-RA (86.24), and 4-RA (86.44 Gy) plans was small too. The plan conformity index was highest in the 2-RA plan (1.19) and lowest in the 4-RA plan (1.10), and this result indicates that the 4-RA plan was more conformal in comparison with the 2-RA and 3-RA plans. No significant difference in homogeneity index values was obtained among 2-RA (1.08), 3-RA (1.08), and 4-RA (1.07) plans.
Rectum
Low dose region (V20Gy and V30Gy)
The V20Gy and V40Gy values were comparable among all three RA plans with an average difference value within ± 0.16%.
Medium dose region (V40Gy and V50Gy)
The V40Gy and V50Gy values were always highest in the 2-RA plan and always lowest in the 4-RA plan. Specifically, in comparison to the 3-RA and 4-RA plans, the medium dose region values were higher in the 2-RA plan by an average difference of 2.64% (2-RA vs. 3-RA) and 4.22% (2-RA vs. 4-RA).
High dose region (V60Gy and V70Gy)
Similar to the results of the medium dose region, the V60Gy and V70Gy values were always highest in the 2-RA plan and always lowest in the 4-RA plan. Specifically, in comparison to the 3-RA and 4-RA plans, the high dose region values were higher in the 2-RA plan by an average difference of 4.89% (2-RA vs. 3-RA) and 18.76% (2-RA vs. 4-RA).
Mean dose
The mean dose to the rectum was lowest in the 4-RA plan with difference of 4.48% in comparison with the 2-RA plan and difference of 2.99% in comparison with the 3-RA plan.
Bladder
Low dose region (V20Gy and V30Gy)
The V20Gy and V40Gy values were comparable among all three plans with an average difference value within ± 0.16%.
Medium dose region (V40Gy and V50Gy)
The V40Gy and V50Gy values were always highest in the 2-RA plan, whereas the V40Gy was lowest in the 4-RA plan and the V50Gy was lowest in the 3-RA plan. In comparison to the 3-RA and 4-RA plans, the medium dose region values were higher in the 2-RA plan by an average difference of 2.92% (2-RA vs. 3-RA) and 2.98% (2-RA vs. 4-RA). In comparison to the 3-RA plan, the 4-RA plan produced lower V40Gy value by difference of 1.17% and higher V50Gy value by difference of 1.09%.
High dose region (V60Gy and V70Gy)
The V60Gy and V70Gy values were always highest in the 2-RA plan and always lowest in the 4-RA plan. Specifically, in comparison to the 3-RA and 4-RA plans, the high dose region values were higher in the 2-RA plan by an average difference of 4.51% (2-RA vs. 3-RA) and 7.81% (2-RA vs. 4-RA).
Mean dose
The mean dose to the bladder was lowest in the 4-RA plan with difference of 2.35% in comparison with the 2-RA plan and difference of 0.30% in comparison with the 3-RA plan.
MUs and integral dose
The number of MUs was higher in the 4-RA plan than that of 2-RA plan (594 MUs vs. 506 MUs) and 3-RA plan (594 MUs vs. 516 MUs). The integral dose was lowest in the 2-Arc plan (1.33 × 105 cc-Gy) in comparison with the 3-RA plan (1.35 × 105 cc-Gy) and 4-RA plan (1.36 × 105 cc-Gy).
Discussion
In this study, we compared treatment planning for low-risk prostate cancer patient with bilateral prostheses treated with RA technique consisting of 2, 3, and 4 arcs. One of the challenges of RA planning involving prostheses is the inability to use the primary beams passing through the prostheses, resulting in reduced number of available beam angles. Thus, the use of avoidance sectors for each prosthesis in this study caused the dose streaking in the anterior-posterior and posterior-anterior directions with an increase in dose to bladder and rectum. Another challenge is the difficulty in visualizing the organs due to the presence of large amount of streak artifacts coming from the prostheses. Generally, a mega-voltage computed tomography (MVCT) scan or an MRI scan is needed to fuse it with the planning CT for accurate delineation of the target volume and OARs.
The use of 4 arcs in this study indicates that it has the potential to improve dose conformity and homogeneity across the PTV and reduce doses to rectum and bladder when compared with the 2-RA and 3-RA techniques. While, the 4-RA plan produced the favorable dosimetric results, plan optimization parameters can generally be adjusted to yield the treatment plan that meets the planning objectives. The tight dose constraints placed on the OARs can also force the TPS to lower the dose to the OARs but for the reduced PTV coverage and decreased dose homogeneity across the PTV. However, since this was a comparative study, same set of optimization parameters were used for all three RA treatment plans.
The patient presented in this study had low-risk prostate cancer. If the patient with bilateral prostheses has high-risk prostate cancer involving lymph nodes, a RA planning may require an increased number of arcs to generate the optimal plan. Furthermore, since high-risk prostate cancer generally requires irradiation of larger pelvis area, plan optimization constraints may require adjustment to achieve the clinical objectives. In this study, we used one set of beam parameters as well as same optimization constraints for planning purpose. In the future, we aim to test different beam parameters and optimization dose constraints that can yield the optimal RA treatment plan for prostate patients involving prostheses.
Conclusion
Based on the RA techniques investigated for a low-risk prostate cancer patient with bilateral prostheses, the 4-RA plan produced lower rectal and bladder dose and better dose conformity across the PTV when compared with the 2-RA and 3-RA plans.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Atlanta: American Cancer Society; 2013. American Cancer Society. Cancer facts and figures 2013; pp. 19–20. [Google Scholar]
- 2.Hankey BF, Feuer EJ, Clegg LX, Hayes RB, Legler JM, Prorok PC, et al. Cancer surveillance series: Interpreting trends in prostate cancer - Part I: Evidence of the effects of screening in recent prostate cancer incidence, mortality, and survival rates. J Natl Cancer Inst. 1999;91:1017–24. doi: 10.1093/jnci/91.12.1017. [DOI] [PubMed] [Google Scholar]
- 3.Alecu R, Alecu M, Loomis T, Ochran T, He T. Traditional and MLC based dose compensator design for patients with hip prostheses undergoing pelvic radiation therapy. Med Dosim. 1999;24:33–7. doi: 10.1016/s0958-3947(98)00044-2. [DOI] [PubMed] [Google Scholar]
- 4.Carolan M, Dao P, Fox C, Metcalfe P. Effect of hip prostheses on radiotherapy dose. Australas Radiol. 2000;44:290–5. doi: 10.1046/j.1440-1673.2000.00816.x. [DOI] [PubMed] [Google Scholar]
- 5.Eng TY. Dose attenuation through a titanium alloy hip prosthesis. Med Dosim. 2000;25:7–8. doi: 10.1016/s0958-3947(99)00021-7. [DOI] [PubMed] [Google Scholar]
- 6.Su A, Reft C, Rash C, Price J, Jani AB. A case study of radiotherapy planning for a bilateral metal hip prosthesis prostate cancer patient. Med Dosim. 2005;30:169–75. doi: 10.1016/j.meddos.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Hazuka MB, Ibbott GS, Kinzie JJ. Hip prostheses during pelvic irradiation: Effects and corrections. Int J Radiat Oncol Biol Phys. 1988;14:1311–7. doi: 10.1016/0360-3016(88)90412-9. [DOI] [PubMed] [Google Scholar]
- 8.Reft C, Alecu R, Das IJ, Gerbi BJ, Keall P, Lief E, et al. Dosimetric considerations for patients with HIP prostheses undergoing pelvic irradiation. Report of the AAPM Radiation Therapy Committee Task Group 63. Med Phys. 2003;30:1162–82. doi: 10.1118/1.1565113. [DOI] [PubMed] [Google Scholar]
- 9.Erlanson M, Franzén L, Henriksson R, Littbrand B, Löfroth PO. Planning of radiotherapy for patients with hip prosthesis. Int J Radiat Oncol Biol Phys. 1991;20:1093–8. doi: 10.1016/0360-3016(91)90210-u. [DOI] [PubMed] [Google Scholar]
- 10.Brooks C, Cheung RM, Kudchadker RJ. Intensity-modulated radiation therapy with noncoplanar beams for treatment of prostate cancer in patients with bilateral hip prosthesis: A case study. Med Dosim. 2010;35:87–91. doi: 10.1016/j.meddos.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Martin DA, Hruby G, Whitaker MK, Foo KY. Constrained-beam inverse planning for intensity-modulated radiation therapy of prostate cancer patients with bilateral hip prostheses. J Med Imaging Radiat Oncol. 2012;56:703–7. doi: 10.1111/j.1754-9485.2012.02456.x. [DOI] [PubMed] [Google Scholar]
- 12.Fattahi S, Ostapiak OZ. An opposed matched field IMRT technique for prostate cancer patients with bilateral prosthetic hips. J Appl Clin Med Phys. 2012;13:3347. doi: 10.1120/jacmp.v13i1.3347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kung JH, Reft H, Jackson W, Abdalla I. Intensity-modulated radiotherapy for a prostate patient with a metal prosthesis. Med Dosim. 2001;26:305–8. doi: 10.1016/s0958-3947(01)00079-6. [DOI] [PubMed] [Google Scholar]
- 14.Otto K. Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys. 2008;35:310–7. doi: 10.1118/1.2818738. [DOI] [PubMed] [Google Scholar]
- 15.Kjaer-Kristoffersen F, Ohlhues L, Medin J, Korreman S. RapidArc volumetric modulated therapy planning for prostate cancer patients. Acta Oncol. 2009;48:227–32. doi: 10.1080/02841860802266748. [DOI] [PubMed] [Google Scholar]


