Abstract
Aims:
The present study was undertaken to evaluate the efficacy of biodegradable plating system for fixation of maxillofacial fractures and to study the morbidity associated with the use of biodegradable plates and screws.
Materials and Methods:
This prospective study consisted of 10 patients with maxillofacial fractures requiring open reduction and internal fixation. Fractures with infection, comminuted and pathological fractures were excluded. All were plated with biodegradable system (Inion CPS) using standard plating principles and observed for a total period of 24 weeks. Characteristics of the fractures, ease of use of bioresorbable plate/screw system and post operative complications were assessed.
Results:
Of total 10 patients, eight patients were of midface fracture and two pediatric patients with mandibular fracture, with nine male and one female. The mean age was 32.8 years. Out of 20 plates and 68 screws applied to the 10 fractures sites; there were three incidences of screw breakage with no other intraoperative difficulties. Paresthesia of the infraorbital nerve was present in two patients, and recovered completely in four weeks after surgery. Fracture reduction was considered to be satisfactory in all cases. One patient developed postsurgical infection and was managed with oral antibiotics and analgesics.
Conclusions:
Favorable healing can be observed through the use of biodegradable plates and screws to stabilize selected midface fractures in patients of all ages, as well as mandible fractures in early childhood, however further studies with more sample size are required.
Keywords: Biodegradable plate/screw system, internal fixation, maxillofacial fractures
INTRODUCTION
Rigid internal fixation with metallic materials is a standard technique, in use for the last 35 years and performed to align bone segments during healing periods. First osteosynthesis plate was described by Sir William Lane[1] over a hundred years ago. Rigid fixation methods have till now, relied almost exclusively upon metallic components because of their high strength and contourability. However, there are inherent drawbacks associated with metallic devices, as susceptibity to corrosion, need to remove these plates/screws due to factors like infection, stress shielding, plate palpability, temperature sensitivity; interference with advanced imaging technique,[2] possible growth restrictions and implant migration in pediatric population and problem in patients who have to be irradiated as they may cause backscatter.[3]
In an effort to overcome the disadvantages of metallic osteofixation devices, various biodegradable polymers have been developed.[4] The advantages of biodegradable osteosynthesis devices include the gradual transference of physiological forces to the healing bone, the reduced need for a second operation to remove the material, its potential to serve as a vehicle to deliver bone-healing proteins to fracture/osteotomy sites[5] and no growth restrictions or possible migration in growing patients. The implant degrades naturally and totally after fracture has healed thus preventing the stress shielding effect[6] while fibrous tissues or bone fills the space previously occupied by the implant.[7] Ideally, these materials are sufficiently rigid, biocompatible, provide stability without affecting bone healing and bone strength adversely, with no interference with post-operative imaging techniques or radiotherapy. Today most commercially available materials which have optimal characteristics for use as a fixation modality in maxillofacial trauma are co-polymers consisting of polylactide acid (80-82%) and polyglycolic acid (18-20%). Polylactide acid/polyglycolic acid ratio affects degradation rate.
However, these have not been recommended for use in loaded and functional bone such as adult mandible because of the lesser strength and stiffness of the material.[8] The present study was undertaken to evaluate the efficacy of biodegradable plates and screws as a method for internal fixation in patients of midface fracture and children with fractures of the mandible and to study the morbidity associated with the use of these devices.
MATERIALS AND METHODS
Study design
This study is a prospective study. All patients with maxillofacial trauma reporting to the outpatient clinic of the Department of Oral and Maxillofacial Surgery of our institute were screened for inclusion in the present study. Patients with major systemic diseases, presence of infection at fracture site, pathologic fractures, comminuted fractures, fractures with extensive bone loss and with history of hypersensitivity reaction to bioresorbable material were excluded. Finally, eight adult patients with midface fractures requiring open reduction and internal fixation and two pediatric patients with mandibular fractures (excluding condylar fractures) were included in the study. The patients participating in this study were thoroughly informed of the advantages and disadvantages of this treatment, and their consent was documented. The study design was approved by the Board of Studies, Pt. BD Sharma University of Health Science, Rohtak, India.
The patients were evaluated preoperatively and post operatively for the following information: Location and type of fracture (displaced vs. nondisplaced), Derangement of occlusion, paraesthesia along the distribution of infra-orbital nerve (in case of midface fractures) or mental nerve (in case of mandible fractures), presence or absence of diplopia, enopthalmos/exopthalmos in case of mid face fractures. On radiological assessment the site, nature and displacement of fractures were assessed using Sub-mento-vertex view and Occipitomental view for mid-face and Orthopantomograph for mandible [Figure 1]. Dental impressions were taken in all patients and arch bars were placed in patients with deranged occlusion.
Figure 1.

Orthopantomogram showing right angle fracture
Materials and methods
Biodegradable Inion CPS (2.0 mm) plating system (Inion, Tempere, Finland) approved by the Food and Drug Administration, was used as a method of internal fixation [Figure 2]. The material is copolymer of L-lactide acid (LPLA), poly D-lactide acid (DLPLA) and trimethyl carbonate (TMC) and polygycolic acid (PGA). These plates have been reported to resorb slowly, maintaining 70% of their initial strength at nine to 14 weeks, with 42% bulk resorption by 40 weeks, and are completely resorbed by two to four years (in vitro data performed by Inion for the US Food and Drug Administration). Plates are malleable after activation in the Inion Thermo™ water bath (55°C). After water bath treatment, plates are most malleable for 10-15 seconds for easy adaptation. They can also be re-heated for further contouring or bent once cooled. Plates can be easily cut with scissors.
Figure 2.

Bioresorbable plate
Operative technique
Surgical access was gained either through an existing skin laceration or a standardized surgical approach, reduction of fracture segments was achieved and segments were stabilized for plate fixation under general anesthesia. Appropriate biodegradable plate of required configuration was selected depending on the site of fracture. The patients with zygomatic complex fractures were stabilized with one or two point fixation at the maxillary buttress and frontozygomaic suture, using 2 mm four hole and two hole plates respectively. Pediatric patients with developing or mixed dentition, presenting with fractures of mandible were stabilized with 2 mm plates and screws placed at the inferior border, below the developing tooth buds, for angle and parasymphysis fracture. The plate was placed into a water bath at 55°C for one to two minutes, allowing the plate to become malleable. Plate was contoured and adapted to the site. Once the plate was adapted across the fracture line, a screw hole was created by using 1.75 mm drill bit at a speed of 2000 rpm with constant irrigation. The screw heads were tapped manually with a two mm manual bone tap. The screw was selected depending on the site of application (2 mm diameter and 5-7 mm length). The screw with the screw driver was inserted and tightened. In the event of screw head fracture during placement of the screw, the head was removed and the previously drilled osteotomy was re-drilled through the remnant of the previous screw shank. The site was re-tapped in standard fashion with placement of a new screw of equal size. No emergency screws were used. The area was copiously irrigated with saline and haemostasis was achieved. Wound was closed in layers and pressure dressing was given. Intra-operative details like time taken for plate fixation, plate fracture, and screw breakage was noted. Intermaxillary fixation was done for a variable period of time ranging from two-four weeks. No intraoral/extraoral drains were placed. All patients received amoxicillin with clavulanate and metrogyl in the perioperative period, continuing for seven days postoperatively [Figures 3 and 4].
Figure 3.
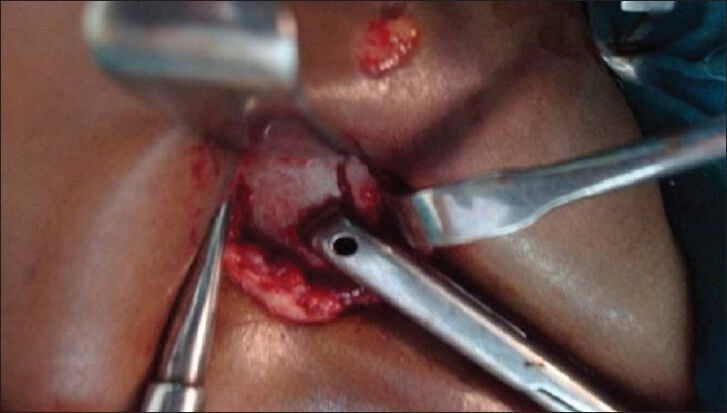
Fracture site exposed and fracture segments reduced
Figure 4.

A 4-hole bioresorbable plate fixed to the fractured segments
RESULTS
Ten patients of maxillofacial fractures were treated by this method including nine males (90%) and one female (10%). They ranged in age from six to 45 years and the mean age was 32.8 years. The most common etiological factor was road traffic accident (60%) followed by interpersonal violence (30%) and fall (10%). Two pediatric patients with angle (10%) and parasymphysis (10%) fracture and eight patients with midface fractures, out of which 5 (50%) were zygomatico-maxillary complex fractures, two (20%) were Le Fort II and one (10%) patient was of Le Fort III fracture, were included in this study [Graph 1].
Graph 1.
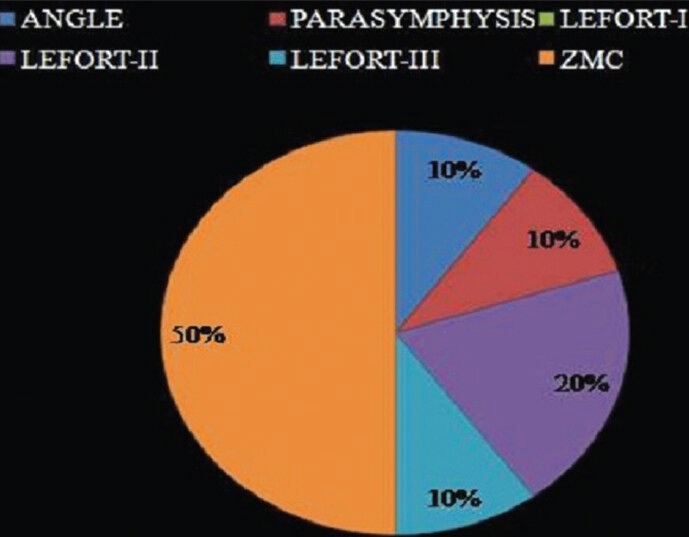
Distribution of patients according to fracture site
In preoperative evaluation, displacement of fracture segments was noticed in five (50%) patients and five (50%) patients had deranged occlusion. Two patients (20%) (1 with Le Fort II and 1 with Le Fort III) reported paraesthesia along the distribution of infra-orbital nerve. Diplopia was present in two patients (25%) and one patient presented with enophthalmos (12.5%) who had Le Fort II fracture.
Intraoperatively, the adaptability of the plate to the reduced fracture segments was satisfactory. Time taken to fix one plate with the required number of screws varied from 20-40 minutes. A total of 20 plates were used and there was no incidence of intra-operative plate fracture. Out of the total number of 68 screws used, only three screws broke during fixation (4.14%).
Post-operatively, all the patients were reviewed clinically and radiographically after 24 hrs, one week, four weeks, 12 and 24 weeks for adequate reduction, stability of fracture segments, centricity of occlusion and post operative complications [Figure 5]. Reduction of the fracture segments was satisfactory and occlusion relationships were judged as normal in all the cases at every follow up. Adequate stability was maintained throughout the post-operative period in all the patients (100%). There was no incidence of (0%) post-operative paraesthesia, diplopia, enopthalmos/exopthalmos, wound dehiscence and plate exposure. In one patient (10%), signs of post-operative infection were noticed including swelling and pain, which was managed conservatively with administration of oral antibiotics and analgesics [Graph 2].
Figure 5.

Post-operative orthopantomogram showing radiolucent bur holes of bioresorbable plate
Graph 2.
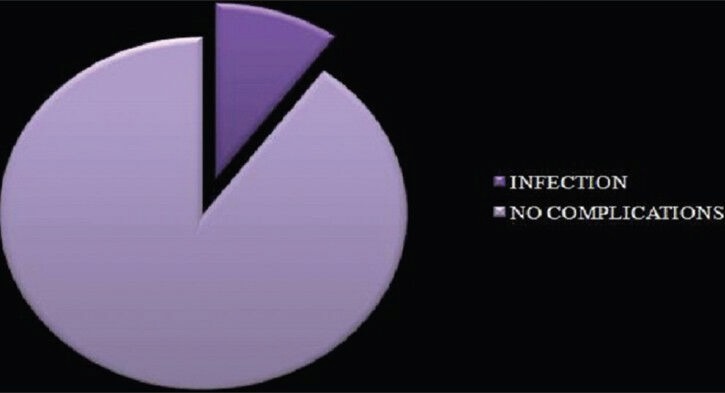
Postoperative complications
DISCUSSION
In modern maxillofacial surgery, rigid osteosynthesis has become one of the major breakthroughs. For 25 years now, titanium has shown its excellent qualities[9] and is currently regarded as the golden standard. When using metallic materials; sometimes it is necessary to perform a second operation for the removal of these screws. All the disadvantages inherent to metallic materials such as palpation, sensitivity, migration, obstruction in the X-ray, possible bone resorption, allergies, and growth delays in children have led to the development of resorbable materials.[10] Since the introduction of biodegradable devices in 1966, the development of their mechanical properties and degradation characteristics has been extensive.
Bioresorbable materials mostly used in maxillofacial surgery are a mixture of rigid and elastic polymers selected for their strength, malleability, and degradation properties. The degradation profiles have been tailored to provide initial stability and then progressively load bone to stimulate regeneration. The results of various studies suggested that the use of biodegradable fixation in selected patients with facial fractures is acceptable.[11]
In the present study, ten cases of maxillofacial fractures were treated with internal fixation using Inion CPS biodegradable plates and screws. Eight patients with mid face fractures and two pediatric patients with developing or mixed dentition presented with fractures of mandible. In two of the adult patients where midface fractures were associated with mandible fractures, the mandibular fractures were managed with titanium plates and screws because the strength of the bioresorbable system is not sufficient to provide stability for fracture mandible in adults as it is a load bearing bone. This was in accordance with observations of Bryan Bell R,[11] Cavusoglu T[12] and Wood GD.[8] Although the tensile strength of a biodegradable plate is less as compared to the titanium,[13] it provides enough stability to the fracture segments in the non-load bearing areas so that healing can take place.
No intra-operative late fracture occurred during this study which in accordance with study by Enislidis G.[14] Out of the total number of 68 screws used for plate fixation, three screws broke, intra-operatively (4.41%) during screw tightening. This is more than the 1.87% incidence of screw fracture noted in the study conducted by Enislidis G.[14] This was probably due to the inadequate pre-tapping of screw holes and consequently excessive friction between the screw and the bone. Bell and Kindsfater[11] recommended that these screws need only be"finger tight," and care must be taken when placing them, especially in thin bones. If excessive torque is applied, the screw head will break. The angulation and the pressure at the time of drilling and tapping are important factors in this system. Post-operative reduction and stability of the fracture segments was maintained in all the patients throughout the follow-up period which reflects upon the strength of the bioresorbable plates and screws which maintains reduction and provides enough stability for healing to take place. In literature, in two series, authors could achieve and maintain reduction ranging from acceptable to excellent in 100% of patients.[15,16] This is in complete agreement with the present study. Centricity of occlusion was observed from immediate post-operative till 24 weeks and was maintained in all the patients which further indicated the stability provided by this system.
Pre-operative paraesthesia along the distribution of infra-orbital nerve, present in two patients of mid face fractures (Le Fort II and Le Fort III), was found to recover completely at four weeks post operative period which is in accordance to study by Benoliel et al.[16] At 12 weeks follow up, one patient of zygomatic fracture presented with pain and swelling at operative site. In this patient, plate was placed at zygomatic buttress approached through an intra-oral buccal vestibule incision. The symptoms resolved with oral antibiotics and analgesics. The infection at the intra-oral surgical site could be attributed to the wound contamination in the oral cavity. This finding goes in agreement with incidence of infection reported in literature, where one in ten patients had symptoms of mild infection according to a study conducted by Wittwer et al.[17]
In the present study, none of the patient had wound dehiscence and plate exposure in the post-operative period. This is somewhat contradictory to incidence of wound dehiscence reported in literature which varies from 2%[15] to as high as 6%.[17] These results can be attributed to the tight closure of the incision obtained with meticulous suturing, adequate soft tissue cover over the implant site and the newer thinner implants. No local tissue reaction and foreign body type of reaction was noticed in the evaluation of surgical site during the follow up period which is contrary to study by Wittwer et al.[17] This difference is probably related to small sample size, compared to other series, which had larger number of patients.
Although, implant material could not be seen on radiographs, yet these were obtained in all patients, post-operatively, at predecided follow-up intervals. Satisfactory reduction was seen in all patients, as judged with the position of fracture segments in 24 hrs post operative radiographs and compared with all subsequently obtained images. The undisturbed reduction was considered as a marker of the stable fixation provided by the bioresorbable system. The screw holes visible as radiolucencies on the radiograph, were also seen to maintain their position throughout the observed period of follow up. This again was considered as a marker for maintenance of reduction which is in accordance with Ferretti[18] and Bell et al.[11] Rozema et al.,[3] studied the effect of these plates and screws when radiation is applied. They concluded that these can be regarded as tissue equivalents that do not interfere with the dose distribution of radiotherapy and can safely be used for fracture fixation of bone segments when post operative radiotherapy is needed.
Bioresorbable fracture fixation has been in clinical use in humans for twenty five years. Still, there are apprehensions to the use of these materials and they have not been able to find place in the armamentarium of the common practicing surgeon. Their exorbitant cost and questionable ability to be used in load bearing areas remains a major hurdle. Another significant factor of the limited use is the resistance by surgeons to modify their conventional, well experienced, treatment techniques. However, if these problems could be completely overcome and these implants could offer the same benefits as metallic implants, they would be able to find a greater place in craniofacial fracture fixation. Since it was a short term study and sample size was very small, the possibility of late reaction to biodegradable implants needs to be evaluated and there is always a scope for long term follow up in such cases.
CONCLUSIONS
Biodegradable plates and screw system provided satisfactory stabilization when used as internal fixation for fractures of midface fractures in patients of all ages and mandibular fractures in early childhood.
The biodegradable implant material did not evoke any significant immune response and is not toxic.
The fixation system did not alter the healing process.
The fixation technique was not difficult to master.
A second surgical procedure was not carried out in any of the patients to remove the implant as the bioresorbable implant resorbed over a period of time. This is more beneficial in case of children where removal of a metallic implant is recommended even in asymptomatic cases because of growth restrictions.
Meticulous procedures along with special instruments provided by the manufacturer were mandatory to achieve the best results. The study had few shortcomings in terms of its small sample size and short term follow up. The encouraging results as obtained in this study seem to reinforce the use of biodegradable plates and screws in fixation of maxillofacial fractures.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lane WA. Some Remarks on the Treatment of Fractures. Br Med J. 1895;1:861–3. doi: 10.1136/bmj.1.1790.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubin JP, Yaremchuk MJ. Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery: A comprehensive review of the literature. Plast Reconstr Surg. 1997;100:1336–53. doi: 10.1097/00006534-199710000-00043. [DOI] [PubMed] [Google Scholar]
- 3.Rozema FR, Levendag PC, Bos RR, Boering G, Pennings AJ. Influence of resorbable poly (L-lactide) bone plates and screws on the dose distributions of radiotherapy beams. Int J Oral Maxillofac Surg. 1990;19:374–6. doi: 10.1016/s0901-5027(05)80086-4. [DOI] [PubMed] [Google Scholar]
- 4.Wiltfang J, Merten HA, Schultze-Mosgau S, Schrell U, Wénzel D, Kessler P. Biodegradable miniplates (Lacto Sorb): Long-term results in infant minipigs and clinical results. J Craniofac Surg. 2000;11:239–43. doi: 10.1097/00001665-200011030-00006. [DOI] [PubMed] [Google Scholar]
- 5.Turvey TA, Proffit WP, Phillips C. Biodegradable fixation for craniomaxillofacial surgery: A 10-year experience involving 761 operations and 745 patients. Int J Oral Maxillofac Surg. 2011;40:244–9. doi: 10.1016/j.ijom.2010.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suuronen R, Haers PE, Lindqvist C, Sailer HF. Update on bioresorbable plates in maxillofacial surgery. Facial Plast Surg. 1999;15:61–72. doi: 10.1055/s-2008-1064301. [DOI] [PubMed] [Google Scholar]
- 7.Enislidis G, Pichorner S, Lambert F, Wagner A, Kainberger F, Kautzky M, et al. Fixation of zygomatic fractures with a new biodegradable copolymer osteosynthesis system: Preliminary results. Int J Oral Maxillofac Surg. 1998;27:352–5. doi: 10.1016/s0901-5027(98)80063-5. [DOI] [PubMed] [Google Scholar]
- 8.Wood GD. Inion biodegradable plates: The first century. Br J Oral MaxillofacSurg. 2006;44:38–41. doi: 10.1016/j.bjoms.2005.07.026. [DOI] [PubMed] [Google Scholar]
- 9.Araujo MM, Waite PD, Lemons JE. Strength analysis of Le Fort I osteotomy fixation: Titanium versus resorbable plates. J Oral Maxillofac Surg. 2001;59:1034–9. doi: 10.1053/joms.2001.25832. [DOI] [PubMed] [Google Scholar]
- 10.Yerit KC, Enislidis G, Schopper C, Turhani D, Wanschitz F, Wagner A, et al. Fixation of mandibular fractures with biodegradable plates and screws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:294–300. doi: 10.1067/moe.2002.122833. [DOI] [PubMed] [Google Scholar]
- 11.Bell RB, Kindsfater CS. The use of biodegradable plates and screws to stabilize facial fractures. J Oral Maxillofac Surg. 2006;64:31–9. doi: 10.1016/j.joms.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Cavusoglu T, Yavuzer R, Basterzi Y, Tuncer S, Latifoglu O. Resorbable plate-screw systems: Clinical applications. Ulus Travma Acil Cerrahi Derg. 2005;11:43–8. [PubMed] [Google Scholar]
- 13.Buijs GJ, van der Houwen EB, Stegenga B, Bos RR, Verkerke GJ. Mechanical strength and stiffness of biodegradable and titanium osteofixation systems. J Oral Maxillofac Surg. 2007;65:2148–58. doi: 10.1016/j.joms.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 14.Enislidis G, Yerit K, Wittwer G, Köhnke R, Schragl S, Ewers R. Self-reinforced biodegradable plates and screws for fixation of zygomatic fractures. J Craniomaxillofac Surg. 2005;33:95–102. doi: 10.1016/j.jcms.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Bessho K, Iizuka T, Murakami K. A bioabsorbable poly-L-lactideminiplate and screw system for osteosynthesis in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1997;55:941–5. doi: 10.1016/s0278-2391(97)90065-3. [DOI] [PubMed] [Google Scholar]
- 16.Benoliel R, Birenboim R, Regev E, Eliav E. Neurosensory changes in the infraorbital nerve following zygomatic fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:657–65. doi: 10.1016/j.tripleo.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 17.Wittwer G, Adeyemo WL, Yerit K, Voracek M, Turhani D, Watzinger F, et al. Complications after zygoma fracture fixation: Is there a difference between biodegradable materials and how do they compare with titanium osteosynthesis? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:419–25. doi: 10.1016/j.tripleo.2005.07.026. [DOI] [PubMed] [Google Scholar]
- 18.Ferretti C. A prospective trial of poly-L-lactic/polyglycolic acid co-polymer plates and screws for internal fixation of mandibular fractures. Int J Oral Maxillofac Surg. 2008;37:242–8. doi: 10.1016/j.ijom.2007.11.015. [DOI] [PubMed] [Google Scholar]


