Abstract
Aims:
This cross-sectional study was conducted to correlate the clinical picture, causative factors of leukoplakia with its histopathology in the patients of Garhwal hill region.
Materials and Methods:
The study was carried out on indoor and outdoor patients of Department of Otorhinolaryngology, HNB Base Hospital, Srinagar, Garhwal, Uttarakhand. Patients were interviewed by a predesigned questionnaire and clinically examined. Finally, histopathological examination was done by using proper technique.
Statistical Analysis:
The data were analyzed by using SPSS version 15.
Results:
The sample consisted of 90 patients were evaluated. Minimum age of presentation was 18 years while the maximum was 65 years. The majority of patients were in age group of 31-40 years, with male predominance. Majority of cases were of minimum dysplasia and minimum of carcinoma in situ (CIS). Buccal mucosa is the most common site for leukoplakia, while hard palate is the least common site. One case of CIS was reported in buccal mucosa, while two cases of CIS were found in specialized mucosa. Smoking and pan masala (in both types with or without tobacco mixed) had a direct relation with the histological type of leukoplakia, as the amount and duration of consumption increased, the severity of dysplasia increased.
Conclusions:
Majority of cases were males in age group of 31-40 years. Probably, it was due to the addiction to smoking and pan masala started early in this region. Severity of dysplasia was related to the amount and duration of exposure to smoking and pan masala. Buccal mucosa was commonly involved because of general human tendency of keeping pan masala in buccal region for a long duration.
Keywords: Carcinoma in situ, histopathology, leukoplakia, oral hygiene, white patch
INTRODUCTION
Leukoplakia is defined as a white patch on the mucosa that cannot be rubbed off and is not ascribable to any other condition. The diagnosis is descriptive one, with no etiological definition and a negative differentiation from other conditions. All known conditions presenting with whitish change in the mucosa need to be excluded. A more recent WHO workshop,[1] recommended abandoning the distinction between the terms “potentially malignant lesions” and “potentially malignant conditions” and to use the term “potentially malignant disorders” instead. These diagnoses are still defined by exclusion of other known white or red lesions. Hence, it is important to remember that all white patches in the mouth are not leukoplakia and not every leukoplakia patch is precancerous. But still, leukoplakia and erythroplakia are the most common potentially malignant disorders. A variety of factors are attributed to the etiology of oral leukoplakia, of which tobacco consumption in any form is the most important factor. Others being alcohol, syphilis, nutritional deficiency, Candida, hormones, galvanism, industrial hazards, and also, repeated mucosal trauma caused by irregular and sharp teeth.
MATERIALS AND METHODS
The study was carried out on indoor and outdoor patients of Department of Otorhinolaryngology, HNB Base Hospital, Srinagar, Garhwal, Uttarakhand, having white patch in the oral cavity from September 2010 to August 2011 for the period of 1 year. A predesigned questionnaire was used and patients were interviewed to exclude any other disease. Personal habits like tobacco chewing, smoking, alcohol, and pan masala chewing were noted. A thorough clinically examination of these patients was done, evaluating their oral hygiene, status of their dental structure and oral mucosa, and later, detailed local examination of the lesion was also carried out. Finally, biopsy was taken under aseptic precaution in local anesthesia and was sent for histopathological examination in the pathology department. The collected data were analyzed by using graph pad and SPSS version 15. In this study, those patients who were suffering from the following diseases were excluded:
Nonspecific ulceration of mucosa
Erythroplakia
Submucosal fibrosis
Melanosis
Pemphigus vulgaris
Fordyce spots
White changes in mucosa arising from inflammatory lesion
Lingua geographic.
RESULTS
Ninety patients, both male and female were included in this study. After proper clinical history and thorough examination, histopathological study was done in all cases. The results of this study in relation of history as age, sex, and duration are presented in Tables 1–3, respectively. It was correlated with their clinical presentation. Histopathology relation with smoking and pan masala consumption are presented in Tables 4 and 5. In cases with more than one leukoplakia patches, biopsy was taken from the oldest patch because on practical ground it is not possible all the time to take multiple biopsies. The results so obtained were compiled and tabulated in Table 6. The association between various causative factors and clinical parameters with histopathological findings was performed by performing statistical analysis. Although it is a well-known fact that the histological classification of oral leukoplakia lesions is imperfect, which may involve subjectivity,[1] we have used the classification of leukoplakia histologically, as suggested by Liu et al.[2]
Table 1.
Histopathology in relation to age
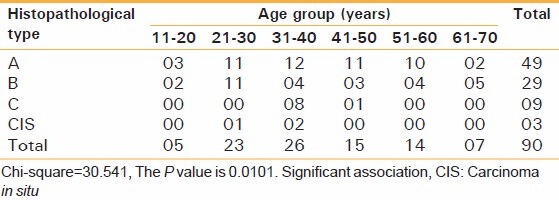
Table 3.
Duration of existence of leukoplakia
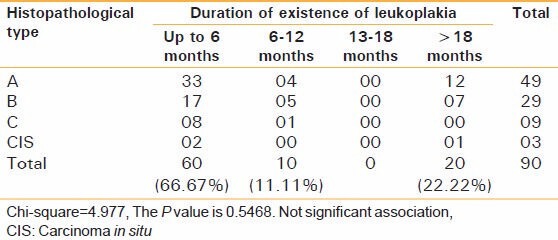
Table 4.
Histopathology and relation smoking
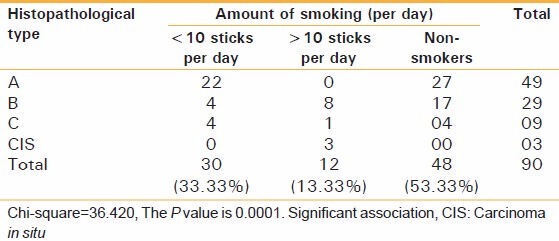
Table 5.
Histopathology and relation with the amount pan masala consumption
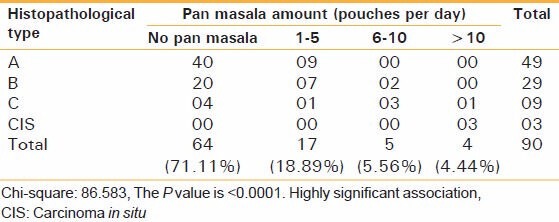
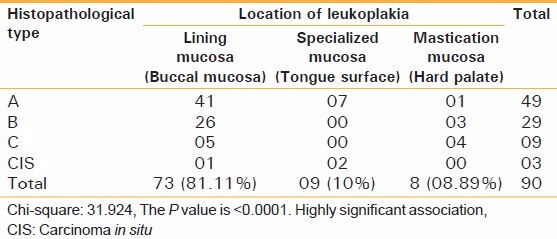
Table 6.
Histopathology in relation to location of leukoplakia
Leukoplakia mild degree of dysplasia (A)
Leukoplakia with moderate degree of dysplasia(B)
Leukoplakia with marked degree of dysplasia (C)
Carcinoma in situ (CIS).
DISCUSSION
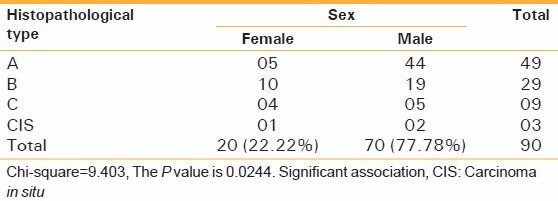
In our study, the majority of patients were between the age group 31 and 40 years (26 cases, 28.8%) with males (77.78%) predominance [Tables 1 and 2]. Higher male percentage is due to higher prevalence of smoking and pan masala chewing habit in them. According to study by Shafer et al., common prevalence was also found in males (69%).[3,4] In the present study, no significant relation between the duration of white patch and its histology could be secured [Table 3] similar to previous studies.[3,4,5] In the present study, 42 cases (46.67%) were smokers. It was also observed that history of smoking of more than 10 sticks/day for more than 10 years was present in all cases of CIS. While only 22 cases (44.9%) of leukoplakia- type A were smokers and all of them smoked less than 10 sticks/day and only one case smoked for more than 10 years. 48 cases (53.3%) in present study were nonsmokers and there was no case of CIS among nonsmokers [Table 4]. We can clearly conclude that smokers have a clear cut and exposure related association with leukoplakia development and later malignant transformation. Peterson et al. observed that 15% of smokers had leukoplakia, while only 0.3% of nonsmokers had leukoplakia.[6]
Table 2.
Histopathology in relation to sex
In this region, endemic of pan masala chewing caused a new trend. The pan masala is basically a flavored and sweetened dry mixture of areca nut, catechu, and slaked lime with or without tobacco. It has been strongly implicated in recent increase in the incidence of leukoplakia and other precancerous lesions even after a short period of use.[7] In the present study, 26 cases (28.8%) were addicted to pan masala. It was observed that the severity of dysplasia increased as the amount and duration of pan masala chewing increased. There were four cases (4.44%) who consumed more than 10 pouches/day for over 10 years, out of which three (3.33%) developed CIS and one case (1.76%) developed type C histopathology [Table 5]. These findings are in contradictory of the study of Gupta, who did not find significant relation between the risk for leukoplakia and the duration of exposure to the quid.[8]
The present study showed buccal mucosa is the most common site of leukoplakia comprising 73 cases (81%), while mastication mucosa (hard palate) being the least common site. Axell also reported that buccal mucosa and commissure was the most frequently involved site for leukoplakia followed by alveolar mucosa, tongue, hard palate, and soft palate.[9] These findings are supported by Silverman who also observed that buccal mucosa as the commonest site of Leukoplakia and together with labial mucosa accounted for 91.5% of the lesion.[10] In buccal mucosa (lining mucosa), only one case (1.36%) was of CIS, while in specialized mucosa (tongue surface) two cases (2.2%) were of CIS [Table 6]. These findings are also supported by Silverman, who observed that the floor of mouth, ventral, and lateral border of tongue were at higher risk for malignant transformation.[10]
CONCLUSION
The results showed that leukoplakia was observed more in males than in females (77.78%), and majority of patients belonged to age group of 31-40 years. It was seen that buccal mucosa is the most common site of leukoplakia (81%). In buccal mucosa, only 1.36% cases (only 1) were of CIS, while in specialized mucosa 22.2% cases were of CIS. A clear cut and direct relation was observed between the duration of smoking and its amount had a positive relation with leukoplakia further, it was seen that 28.8% of cases were addicted to pan masala and the severity of dysplasia increased as the amount and duration of pan masala chewing increased. Lack of any documentary and supportive evidences related to this regional area regarding etiopathology and causative factors prompted us to carry out this study. The result of the present study provides information on the prevalence of leukoplakia and causative factors in the region of Garhwal region, showing alarmingly increasing trend resembling to other places and call for early preventive measures. Government, NGO, and social reforms should be taken up for stopping the tobacco menace in this area.
ACKNOWLEDGMENT
We are highly thankful to our Principal Dr. V. L. Jahagirdar, who allowed us to conduct this study and provided us necessary support for the same. We are also very thankful to our staff for necessary technical support to conduct the study.
Finally, we express deep appreciation to the patients who willing provided us information utilized in the study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36:575–80. doi: 10.1111/j.1600-0714.2007.00582.x. [DOI] [PubMed] [Google Scholar]
- 2.Liu W, Wang YF, Zhou HW, Shi P, Zhou ZT, Tang GY. Malignant transformation of oral leukoplakia: A retrospective cohort study of 218 Chinese patients. BMC Cancer. 2010;10:685. doi: 10.1186/1471-2407-10-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shafer WG, Waldron CA. Oral carcinoma in situ. Oral Surg Oral Med Oral Pathol. 1975;39:227–38. doi: 10.1016/0030-4220(75)90224-8. [DOI] [PubMed] [Google Scholar]
- 4.Waldron CA, Shafer WG. Leukoplakia revisited. A clinico-pathologic study of 3256 oral leukoplakias. Cancer. 1975;36:1386–92. doi: 10.1002/1097-0142(197510)36:4<1386::aid-cncr2820360430>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 5.Bouquot JE. Reviewing oral leukoplakia-clinical concepts for the 1990s. J Am Dent Assoc. 1991;122:80–2. doi: 10.1016/s0002-8177(91)26024-9. [DOI] [PubMed] [Google Scholar]
- 6.Roed-Petersen B, Gupta PC, Pindborg JJ, Singh B. Association between oral Leukoplakia and sex, age, and tobacco habits. Bull World Health Organ. 1972;47:13–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Bedi R, Jones P. Betel-quid chewing among Bangladeshi community in the United Kingdom. London: Centre for Trans-Culture Oral Health; 1995. pp. 11–25. [Google Scholar]
- 8.Gupta PC. A study of dose- response relationship between tobacco habit and oral Leukoplakia. Br J Cancer. 1984;50:527–31. doi: 10.1038/bjc.1984.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Axell T. Occurrence of Leukoplakia and some other oral white lesions among 2033 adult Swedish people. Community Dent Oral Epidemiol. 1987;15:46–51. doi: 10.1111/j.1600-0528.1987.tb00479.x. [DOI] [PubMed] [Google Scholar]
- 10.Silverman S, Bhargava K, Mani NJ. Malignant transformation and natural history of oral leukoplakia in 57518 industrial workers in Gujarat, India. Cancer. 1976;38:1790–5. doi: 10.1002/1097-0142(197610)38:4<1790::aid-cncr2820380456>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]


