Abstract
Introduction:
Arthrocentesis is a method of irrigating the temporomandibular joint (TMJ) with a therapeutic substance. It is usually performed by dual puncture with two needles to the joint space. Several studies have shown that arthrocentesis of the upper compartment of the TMJ may be a highly effective method to restore normal maximal mouth opening and functioning. Nonetheless, the classical two needle technique has some limitations, such as the low tolerability and difficulty in performing it in the presence of intra-articular adherences. The adoption of a single puncture technique for both fluid injection and aspiration might have some advantages with respect to the traditional two needle approach in terms of time of execution, tolerability, and retention of medication.
Materials and Methods:
A single puncture technique with a self fabricated device is used to assess the efficacy of this device. This study involved 20 patients of age ranging between 20- 64 years diagnosed with TMD. Patients follow up done at 3rd, 14th, 45th and 90th day and assessment of pain, mouth opening, clicking and deviation done with comparison of pre and post-operative data.
Results:
The procedure was successful in all the patients. Most of the patients reported reduction in pain more than half of the previous value and two patients reported only moderate reduction. There was a clinically significant improvement in mouth opening, clicking and deviation.
Conclusion:
Arthrocentesis is effective in treating TMJ internal derangement and restoring its function. Single puncture arthrocentesis, is a minimally invasive, simple, inexpensive & highly efficient procedure that can be performed under local anaesthesia.
Keywords: Single puncture arthrocentesis, single puncture arthrocentesis of temporomandibular joint, temporomandibular joint internal derangement
INTRODUCTION
Temporomandibular joint (TMJ) is subjected to many disorders commonly addressed as temporomandibular joint disorders (TMD). These disorders are accompanied by pain, limitation, and deviation in mandibular range of motions, TMJ sounds, headache, and facial pain. Among these internal derangement and TMJ osteoarthritis are the most common disorders. These range from a normal mouth opening and clicking to varying degree of pain and restricted mouth opening and loss of functional activity.
When conservative methods which are used to treat these disorders fail, surgery of TMJ becomes inevitable. Surgery in this region is associated with morbidity and fraught with many risks. More often surgery does not produce expected results. Arthrocentesis of TMJ was introduced by Nitzan et al., in 1991,[1] which bridged the gap between surgical and nonsurgical treatment.[2] It involved irrigation of upper joint compartment with therapeutic substance, releasing adhesions, and flushing out inflammatory substrates relieving pain and improving function. In the traditional procedure two needles[3] with double puncture technique were used for arthrocentesis.
In our study we have used single puncture technique using landmarks described by McCain.[3] The objective of the study was to assess efficacy of device.
MATERIALS AND METHODS
The present study was conducted in the Department of Oral and Maxillofacial Surgery, Darshan Dental College and Hospital, Udaipur. This study involved 20 patients of age ranging between 20-64 years diagnosed with TMD. Approval of the ethics committee was obtained for the study.
All the cases were examined clinically and radiographically with proper consent prior to the procedure.
The patents who met the following criteria were selected for the study.
Typical clinical presentation of pain in TMJ region on movement of mandible.
Restriction of mouth opening 30 mm or less.
Audible clicking present during various mandibular movements.
Deviation of mandible on opening the mouth.
Magnetic resonance imaging (MRI) findings suggesting internal derangement of TMJ.
Pain assessment was done using visual analog scale (VAS), rated 1-10 (Emshoff Rudiger[4]).
The mouth opening was measured using digital vernier calliper.
Exclusion criteria
Medically compromised patients.
Traumatic arthritis.
Fabrication of device
Device for arthrocentesis is fabricated using two 18 gauge needles soldered together using orthodontic solder along the long axis and a divergent angulation made near its hub for ease of use [Figure 1]. The soldering is done in the most proximal part which is not required to be introduced into the tissues. The device is then sterilized by autoclaving as per a standard protocol.
Figure 1.
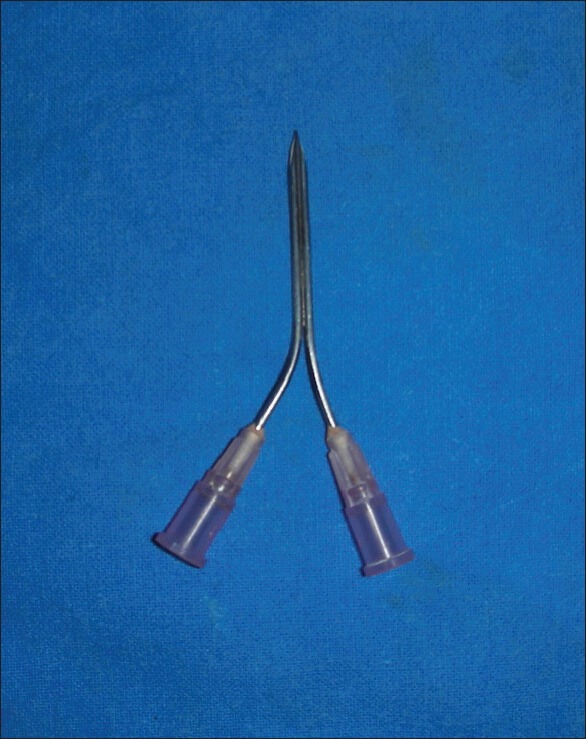
Indigenously fabricated device
Procedure
Patient is seated inclined at 45° angle with head turned towards the unaffected side to provide an easy approach to the joint to be treated. The side to be treated is prepared. The external auditory meatus is blocked with a sterile cotton plug.
The points of insertion are marked on the skin (according to the method suggested by McCain[3]). The line is drawn from middle of tragus to outer canthus of eye. The posterior entrance point is located along canthotragal line, 10 mm from middle of tragus, and 2 mm below the line. The anterior entrance point is placed 10 mm further forward along the line and 10 mm below it. These markings over the skin indicate the location of articular fossa and eminence of TMJ.
Then lignocaine hydrochloride 2% without vasoconstrictor is injected to distend the upper joint space and anesthetize the adjacent tissues. The device is inserted into upper compartment of the joint through posterior entrance point [Figure 2] to enable free flow of normal saline through superior compartment. The joint is irrigated with 200 ml normal saline, through the joint space [Figures 2 and 3]. During lavage, the mandible is moved through opening, excursive and protrusive movements to facilitate lysis of adhesions. On termination of procedure, device is removed and patient is advised restricted jaw movements and soft diet for the following 24 h and nonsteroidal anti-inflammatory drugs (NSAIDs) prescribed to be used in case of pain for a period not more than 3 days. Physiotherapy involving active mouth opening is recommended after 3 days. Patients follow-up done at 3rd, 14th, 45th, and 90th day and assessment of pain, mouth opening, clicking, and deviation done with comparison of pre- and postoperative data.
Figure 2.

Landmarks
Figure 3.

Arthrocentesis procedure
Statistical analysis
Postoperative changes in pain, clicking, deviation, and mouth opening were compared with the preoperative values using paired t-test.
RESULTS
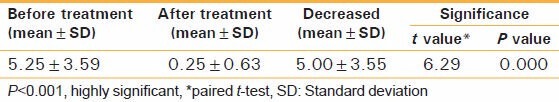
The statistical analysis was done for the 20 patients using paired t-test. The intensity of pain was evaluated pre and posttreatment using VAS. The mean pain on the first visit was 5.25 ± 3.59. The mean and standard deviation (SD) on the 90th day was found to be 0.25 ± 0.63. Most of the patients reported reduction in pain more than half of previous value and two patients reported only moderate reduction. The result is statistically highly significant, which is tested by student paired t-test as shown in Table 1.
Table 1.
Degree of pain (pre- and postoperative)
The increase in mouth opening was calculated for each patient at day 1, 3, 14, 45, and at the end of 90 days. In eight patients, mouth opening increased significantly more than 12 mm. In seven patients it remained the same as they had sufficient mouth opening, but were treated for other symptoms. The mean increase was found to be 7.87 mm with SD of 7.21 mm using Student's paired t-test and was found to be statistically highly significant (t = 4.483, P < 0.001) [Table 2 and Figure 4].
Table 2.
Comparison of mouth opening (pre- and postoperative)
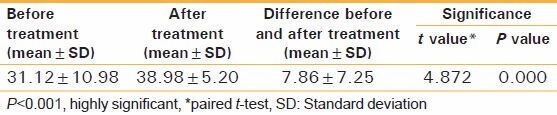
Figure 4.
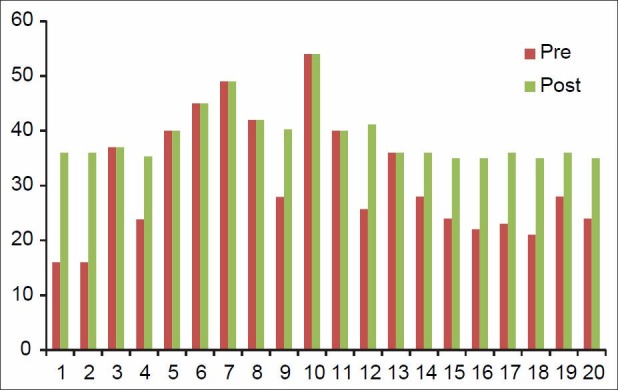
Comparison of mouth opening pre- and –post-treatment
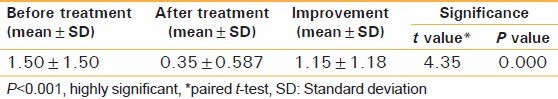
There was a clinically significant improvement in deviation. For each patient the decrease in deviation is calculated and average improvement is found to be 1.15 with SD of 1.18. The Student's paired t-test shows that there is highly significant improvement at the end of 90 days of follow-up as shown in Table 3.
Table 3.
Comparison of deviation towards unaffected joint
The effect of treatment for clicking was decided on the basis of proportion of improvement at end of treatment. The mean clicking on the first visit was 0.85 with SD of 0.37 and at 90 day follow-up it was 0.40 with SD of 0.51. The mean decrease was 0.45 ± 0.51. The result is statistically highly significant.
DISCUSSION
TMD comprises a wide variety of disorders of TMJ, masticatory muscles, or both;[5,6] have pain and dysfunction as main symptoms. Pain associated with TMJ disorders may be due to vasoconstriction, release of nitric oxide, reactive oxygen species (ROS), and thiobarbituric acid. ROS levels in synovial fluid may result from mechanical stress and high pressures directed to upper compartment during clenching and jaw movement.[7] Lavage of upper compartment by TMJ arthrocentesis forces apart the flexible disc from fossa, washes away degraded particles with inflammatory components, and decrease intra-articular pressure. Elimination of nitric oxide and ROS relieves the pain.[8]
In our study there is marked relief from pain in all patients with TMD with short-term follow up of 3 months. This is in accordance with study done by Nitzan et al., and Nishimura et al.[3,8]
In case of closed lock, the central portion of healthy disc indeed separates from the fossa, leaving rims fastened to surface of eminence and bringing in its wake, increased negative pressure in closed space between fossa and disc. This pressure differences constitutes a force sufficient to keep the disc compressed against the fossa (suction cup effect).[3,9]
In this study we found that arthrocentesis abolishes negative pressure, loosens adhered disc, and reinstitutes its free sliding movement. It is also instrumental in removing inflammatory constituents and pain mediators from the joint. It helps the joint to reassume its normal movement bringing about recovery of intra-articular pressure fluctuations, which in turn allows perfusion of nutrients and medications. Thus, in patients with disc adhesions there was marked improvement in mouth opening and decreased deviation.
Patients of TMJ osteoarthritis complains of early morning stiffness in TMJ, severe joint pain, and limitation in mouth opening and function along with swelling in respective area.[3] These symptoms arise due to joint overloading and increased intra-articular pressure, which leads to sclerosis of subchondral bone,[7] compromised blood supply which is due to pain, and absence of elimination of inflammatory substrates which are removed during normal joint mobilization.[3]
Arthrocentesis forces apart the joint constituents and washes away inflamed synovial fluid, thereby reducing pain and loading effect thus in turn increasing mouth opening.[4,10] There was marked improvement in pain and mouth opening in patients treated with arthrocentesis in our study. Clicking could be intermittent or constant which is caused by displacement of the disc. Arthrocentesis distends the upper joint compartment thereby relieving the lag, and disc condyle complex moves synchronously reducing the clicking.[4]
In our study, follow-up was done on a short-term basis for only 90 days following which patients were advised to continue with physiotherapy. There was a significant improvement in condition of patients on the 90th day with regards to pain, clicking, and mouth opening.
The traditional method of TMJ arthrocentesis is done using two needles following the method suggested by McCain, but in our study the technique used is single puncture technique in which indigenously fabricated device is used for irrigating upper compartment of TMJ.
The device was first unveiled by us in a letter addressed to the editor, Journal of Oral and Maxillofacial Surgery.[1]
The use of single puncture technique has some advantages:[11,12]
Reduced time of execution.
The use of a single needle is easier to perform as controlling two ports is cumbersome.
As the procedure involves single puncture it is minimally traumatic.
CONCLUSION
This pilot study was designed to assess efficacy of indigenously fabricated device.
It was observed that
Mouth opening was significantly improved.
In terms of pain, 96% had reduction of pain on postoperative follow-up.
Clicking was found to be reduced nearly to 85%.
Lateral motion towards the unaffected joint significantly improved.
It was concluded that arthrocentesis was effective in treating TMJ internal derangement and restoring its function. Thus, single puncture arthrocentesis, is a minimally invasive, simple, inexpensive, and highly efficient procedure that can be performed under local anesthesia. A study with a larger sample size and long term follow-up is warranted.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: A simplified treatment for severe limitation of mouth opening. J Oral Maxillofac Surg. 1991;49:1163–70. doi: 10.1016/0278-2391(91)90409-f. [DOI] [PubMed] [Google Scholar]
- 2.Singh S, Shivamurthy DM, Varghese D, Re: Rahal A, et al. Single-puncture arthrocentesis--introducing a new technique and a novel device. J Oral Maxillofac Surg. 2011;69:311–3. doi: 10.1016/j.joms.2009.12.041. [DOI] [PubMed] [Google Scholar]
- 3.Nitzan DW. Arthrocentesis--incentives for using this minimally invasive approach for temporomandibular disorders. Oral Maxillofac Surg Clin North Am. 2006;18:311–28. doi: 10.1016/j.coms.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Emshoff R, Puffer P, Rudisch A, Gassner R. Temporomandibular joint pain: Relationship to internal derangement type, osteoarthrosis, and synovial fluid mediator level of tumor necrosis factor-alpha. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:442–9. doi: 10.1067/moe.2000.108801. [DOI] [PubMed] [Google Scholar]
- 5.Greene CS. The etiology of temporomandibular disorders implications for treatment. J Orofac Pain. 2001;15:93–105. [PubMed] [Google Scholar]
- 6.Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain. 1999;13:232–7. [PubMed] [Google Scholar]
- 7.Alpaslan C, Bilgihan A, Alpaslan GH, Güner B, Ozgür Yis M, Erbaº D. Effect of arthrocentesis and sodium hyaluronate injection on nitrite, nitrate and thiobarbituric acid-reactive substance levels in the synovial fluid. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:686–90. doi: 10.1067/moe.2000.105518. [DOI] [PubMed] [Google Scholar]
- 8.Nishimura M, Segami N, Kaneyama K, Sato J, Fujimura K. Comparison of cytokine level in synovial fluid between successful and unsuccessful cases in arthrocentesis of the temporomandibular joint. J Oral Maxillofac Surg. 2004;62:284–7. doi: 10.1016/j.joms.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 9.Nitzan DW. Arthrocentesis for management of severe closed lock of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 1994;6:245–55. [Google Scholar]
- 10.Emshoff R, Rudisch A. Are internal derangements and osteoarthrosis linked to changes inclinical outcome measures of arthrocentesis of the temporomandibular joint? J Oral Maxillofac Surg. 2003;61:1162–7. doi: 10.1016/s0278-2391(03)00676-1. [DOI] [PubMed] [Google Scholar]
- 11.Guarda-Nardini L, Manfredini D, Ferronato G G. Arthrocentesis of the temporomandibular joint: A proposal for a single-needle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:483–6. doi: 10.1016/j.tripleo.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Alkan A, Baº B. The use of double-needle canula method for temporomandibular joint arthrocentesis: clinical report. Eur J Dent. 2007;1:179–82. [PMC free article] [PubMed] [Google Scholar]


