Abstract
Odontogenic cysts comprise a diverse group of exceptional lesions derived from epithelial elements of the tooth-forming apparatus. Calcifying cystic odontogenic tumor is a rare odontogenic lesion, which represents about 2% of all odontogenic tumors and cysts. It may occur in a central (intraosseous) or peripheral (extraosseous calcifying cystic odontogenic tumor [ECCOT]) location. ECCOT in contrast to central, tends to affect the older patients, commonly located in the anterior lower jaw, is less aggressive and the recurrence is rare. Here, we report clinico-pathological and radiographic features of ECCOT located in relation to 48 (posterior lower jaw) measuring about 1 cm in the greatest diameter in a 17-year-old male.
Keywords: Extraosseous calcifying cystic odontogenic tumor, odontogenic cyst, odontogenic tumor
INTRODUCTION
The calcifying odontogenic cyst (COC) is an uncommon odontogenic lesion, which was described by Gorlin et al. in 1962 as a distinct entity.[1] Since then, literature shows a large controversy regarding terminology and classification in spite of the currently acceptation of Gorlin's original designation by the World Health Organization (WHO) in 1971.[2] COC is thought to represent a non-neoplastic lesion, but it has a potential for continuous growth.[3] A lot of confusion and disagreement is present in the terminology and classification of COC. Some investigators have considered COC as a tumor with a tendency for marked cyst formation. This concept, called “monistic” by Toida[4] has led some researchers to substitute the terms “calcifying ghost cell odontogenic tumor” or “cystic calcifying odontogenic tumor” for that of COC. In addition, a “dualistic” approach has been suggested that COC can contain two entities:[4]
Cyst: calcifying ghost cell odontogenic cyst
Neoplasm (benign: Calcifying ghost cell odontogenic tumor; or malignant: Malignant calcifying ghost cell odontogenic tumor); and combined lesion: Each of the categories described above associated with odontoma, ameloblastoma, or other odontogenic lesions.
The Calcifying cystic odontogenic tumor (CCOT) represents less than 2% of all odontogenic tumors and cysts.[5] CCOT presents both intraosseous (central) and extraosseous (peripheral) locations. The intraosseous CCOT (ICCOT) is an unilocular or multilocular destructive radiolucent lesion that may contain irregular calcifications.[5,6] extraosseous CCOT (ECCOT) represents less than 25% of the COC.[7] CCOT is usually an asymptomatic slow growing swelling of the jaws or gingival tissues, depending upon whether the lesion is intra or extraosseous. The ECCOT is less common, comprising 12% to 20% of the reported cases.[3] It has been reported to be found between the 1st and 9th decades of life, with a highest incidence occurring in the 6-7th decades and tends to appear with equal frequency amongst males and females. The incisor, canine or premolar regions of the mandible are most frequently involved.[6] Clinically it appears as a localized or pedunculated gingival mass with no distinctive features and radio graphically it shows no or only superficial bone involvement with surface erosion.[8]
The histological features of ECCOT are similar to the ICCOT characteristics, and include an epithelial lining of varied thickness, composed of a distinct columnar (and occasionally cuboidal) basal layer, with cells that contain darkly staining nuclei, polarized away from the basement membrane and palisading, similar to the ameloblasts. Within the epithelial lining, there is an irregular collection of cells, including sheets of stellate reticulum and eosinophilic cells so called ghost cells. Next to the basal layer, irregular or dysplastic dentin and osteoid can also be found.[6,7,8,9]
Treatment involves enucleation of the lesion and long-term follow-up. Recurrences are uncommon and probably related to incomplete cyst removal.[6,10,11] The present paper reports a case of an ECCOT in a 17-year-old male with the brief review of relevant literature.
CASE REPORT
A 17-year-old male patient reported with a chief complaint of swelling in relation to the right region of the lower jaw, since 4 months. Patient denied any family, medical, dental or personal (habit) history. Extra-oral examination was insignificant. On intra-oral examination, a pinkish dome-shaped, oval nodular growth was seen measuring about 1 × 1 cm in diameter, in relation to 48 region. On palpation, it was asymptomatic, fluctuant and sessile. The overlying mucosa was normal with superficial blood vessels, giving a pinkish appearance [Figure 1]. No other intraoral deformity was noted. Intra-oral periapical radiograph (IOPA) shows no osseous involvement, but vertically impacted 48 [Figure 2]. All other teeth showed normal development and eruption. Based on these features a differential diagnosis of hyperplastic or reactive lesions arising from the gingival and eruption cyst was made.
Figure 1.
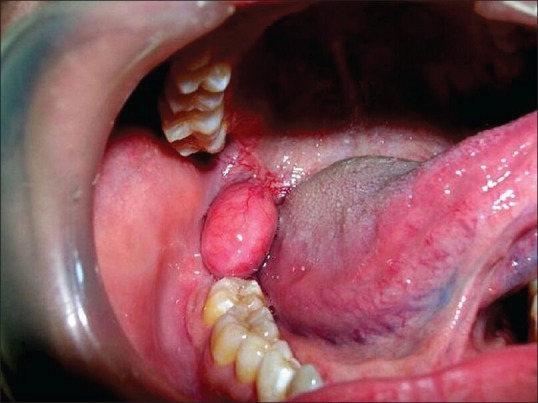
Clinical appearance of the growth
Figure 2.

Radiograph Intra-oral periapical radiograph in relation to 48
Excisional biopsy under local anesthesia was performed. Microscopic examination showed a cyst lined by an epithelium with numerous ghost cells and few calcified masses. The basal cells were cuboidal to columnar with darkly staining nuclei, polarized away from the basement membrane, and showed palisading appearance similar to ameloblasts [Figure 3]. Based on these features a definite microscopic diagnosis of ECCOT was made. No recurrence was noted at a one-year follow-up.
Figure 3.
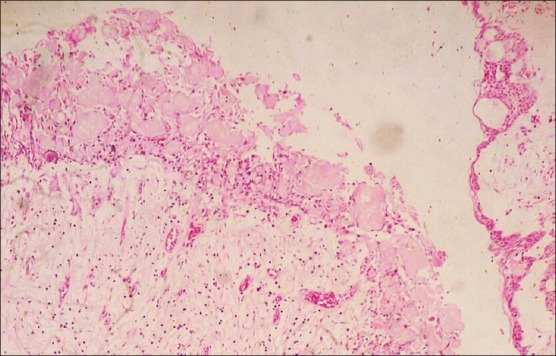
Photomicrograph showing cyst epithelium with numerous ghost cells and few calcified masses. Basal cells are cuboidal to columnar in shape showing hyperchromatism, few showing reverse polarity with palisading appearance (H and E, ×10)
DISCUSSION
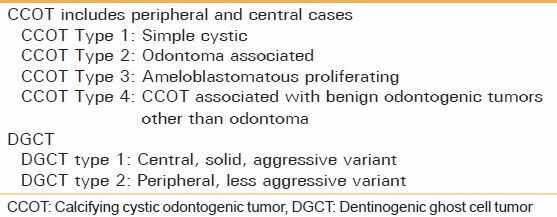
COC or gorlin cyst was described first by Gorlin[8] and Pretarious[5] as a definite pathologic entity. A rare developmental odontogenic lesion (less than 2% of jaw cysts) is described as having features of both cystic and solid neoplasm. The latest WHO classification 2005 of odontogenic tumors [Table 1] renamed the cystic type of this entity as CCOT with four subtypes.[9]
Table 1.
World health organization calcification (2005) of calcifying cystic odontogenic tumor and dentinogenic ghost cell tumor
The term dentinogenic ghost cell tumor was retained for neoplastic type.[10] Most cases of CCOT arise centrally from within the bone, but occasionally they may occur peripherally.[4,8] Peripheral CCOT also known as the “ECCOT”. ECCOT is extremely rare as compared to its intraosseous counterpart.[9]
ECCOT has been reported to be found between the 1st and 9th decades of life, with a highest incidence occurring in the 6-7th decades, and tends to appear with equal frequency amongst males and females.[6,7] It is usually present as a slowly enlarging asymptomatic mass with smooth surface in the gingiva or alveolar mucosa.[9] The clinical differential diagnosis of ECCOT includes common gingival growths of non-neoplastic nature and other peripheral odontogenic tumors.[7]
The mandible is described as the most common site for the ECCOT. The most common locations included the incisor-cuspid and the premolar regions, with only a few lesions located in the molar-retromolar region.[7] About 55% of ECCOT have been found between the canines.[8] The size of the lesion ranged from 0.5 to 4 cm in greatest diameter and the majority of cases were less than 1.5 cm.[9]
Clinically, a variety of diagnosis are made by clinicians, the most common being the fibroma or fibrous hyperplasia. Other differential diagnoses are gingival cyst of adult and peripheral ameloblastoma.[7] However, currently the origin of ECCOT is not known but regarding to the histogenesis of ECCOT two major sources of origin may be considered. The lesion which are located entirely within connective tissue of gingiva and separated from the surface epithelium by a band of connective tissue (just like present case) probably arise from remnants of the dental lamina whereas other lesions appear arising from the surface epithelium. A similar histogenesis has been suggested for peripheral ameloblastoma and gingival cyst of adult.[9,12]
Radio graphically, it has been reported that ECCOT appears as a radiolucent area with scattered amounts of calcification.[13] It may cause erosion of the underlying alveolar bone.[6,7] Microscopically four variants of ECCOT like CCOT were distinguished:[6]
Type 1 (Simple cystic),
Type 2 (Odontoma associated),
Type 3 (Ameloblastomatous proliferating),
Type 4 (ECCOT associated with benign odontogenic tumors other than Odontoma).
Type 1 is the most common pattern characterized by cystic epithelial lining in which a well-defined basal layer of columnar cells and overlying layers resemble stellate reticulum of enamel organ with masses of ghost cells, which may be located within the epithelial lining or fibrous capsule.[9] Mineralization of the ghost cells may be seen. They may also invade the connective tissue, causing a foreign body reaction. The presence of ghost cells in CCOT is not pathognomonic, having been described in ameloblastoma, ameloblastic fibroma, ameloblastic fibro-odontoma, and odontomas.[8,14]
Sometimes variable quantities of dentinoid material are laid down adjacent to epithelial lining. In some instances, melanin or clear cells could be identified.[10] The microscopic differential diagnosis, especially type 1 and 3 must be made with peripheral Ameloblastoma. Both lesions share the presence of prominent elongated basal cells and Stellate reticulum zone, but the presence of ghost cells is rare in ameloblastoma.[3]
ECCOT has a less aggressive behavior than the intraosseous counterpart and a simple excision biopsy is curative.[7,14] Recurrence in case of ECCOT is rare. Follow-up treatment ranged from 9 months to 60 months, only one case of recurrence could be observed.[10]
In summary, the current paper presents a case of ECCOT (Type 1) in an 17-year-old male patient, located in the posterior alveolar mucosa in relation to 48 region, measuring about 1 × 1 cm in diameter. It should be included by the general dentists in the differential diagnosis of other oral hyperplastic/reactive lesions or cystic lesion arising from the gingiva or alveolar mucosa due to its clinical similarities. Currently, the origin of ECCOT is questionable. More data are needed to draw conclusion relative to any differences in their nature and behavior.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Gorlin RJ, Pindborg JJ, Odont, Clausen FP, Vickers RA. The calcifying odontogenic cyst - A possible analogue of the cutaneous calcifying epithelioma of Malherbe. An analysis of fifteen cases. Oral Surg Oral Med Oral Pathol. 1962;15:1235–43. doi: 10.1016/0030-4220(62)90159-7. [DOI] [PubMed] [Google Scholar]
- 2.Pindborg JJ, Kramer IR, Torlini H. Histological Typing of Odontogenic Tumours, Jaw Cysts, and Allied Lesions. Geneva: WHO; 1971. Definitions and explanatory notes. [Google Scholar]
- 3.Orsini G, Fioroni M, Rubini C, Piattelli A. Peripheral calcifying odontogenic cyst. J Clin Periodontol. 2002;29:83–6. doi: 10.1034/j.1600-051x.2002.290113.x. [DOI] [PubMed] [Google Scholar]
- 4.Toida M. So-called calcifying odontogenic cyst: Review and discussion on the terminology and classification. J Oral Pathol Med. 1998;27:49–52. doi: 10.1111/j.1600-0714.1998.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 5.Praetorius F, Ledesma-Montes C. Calcifying cystic odontogenic tumor. In: Barnes EL, Everson JW, Reichart P, Sidransky D, editors. Pathology and Genetics of Head and Neck Tumours. World Health Organization Classification of Tumours. Lyon France: IARC Press; 2005. p. 313. [Google Scholar]
- 6.Resende RG, Brito JA, Souza LN, Gomez RS, Mesquita RA. Peripheral calcifying odontogenic cyst: A case report and review of the literature. Head Neck Pathol. 2011;5:76–80. doi: 10.1007/s12105-010-0213-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buchner A, Merrell PW, Hansen LS, Leider AS. Peripheral (extraosseous) calcifying odontogenic cyst. A review of forty-five cases. Oral Surg Oral Med Oral Pathol. 1991;72:65–70. doi: 10.1016/0030-4220(91)90191-e. [DOI] [PubMed] [Google Scholar]
- 8.Seyedmajidi M, Feizabadi M. Peripheral calcifying odontogenic cyst. Arch Iran Med. 2009;12:309–12. [PubMed] [Google Scholar]
- 9.Taghavi N, Khodayari A, Sargolzaei S, Mashhadiabbas F, Moshref M, Lotfi A, et al. Recurrent peripheral calcifying cystic odontogenic tumor (Calcifying odontogenic cyst) Iranian. J Pathol. 2009;4:141–14. [Google Scholar]
- 10.Ledesma-Montes C, Gorlin RJ, Shear M, Prae Torius F, Mosqueda-Taylor A, Altini M, et al. International collaborative study on ghost cell odontogenic tumours: Calcifying cystic odontogenic tumour, dentinogenic ghost cell tumour and ghost cell odontogenic carcinoma. J Oral Pathol Med. 2008;37:302–8. doi: 10.1111/j.1600-0714.2007.00623.x. [DOI] [PubMed] [Google Scholar]
- 11.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. 3rd ed. St Louis, Missouri: WB Saunders; 2009. Odontogenic cyst and tumor; pp. 695–7. [Google Scholar]
- 12.Manor Y, Mardinger O, Katz J, Taicher S, Hirshberg A. Peripheral odontogenic tumours - Differential diagnosis in gingival lesions. Int J Oral Maxillofac Surg. 2004;33:268–73. doi: 10.1006/ijom.2003.0508. [DOI] [PubMed] [Google Scholar]
- 13.Praetorius F, Hjørting-Hansen E, Gorlin RJ, Vickers RA. Calcifying odontogenic cyst. Range, variations and neoplastic potential. Acta Odontol Scand. 1981;39:227–40. doi: 10.3109/00016358109162284. [DOI] [PubMed] [Google Scholar]
- 14.Odell EW, Morgan PR. Biopsy Pathology of the Oral Tissues. London: Chapman and Hall Medical; 1998. Benign tumor of odontogenic epithelium; pp. 399–403. [Google Scholar]


