Abstract
Background
Acupuncture and other modalities of Chinese/East Asian medicine have been used to treat women’s health for many centuries. Gynecology specialties focus particularly on menstrual and reproductive disorders. Both the adoption of the use of acupuncture outside Asia, and the incorporation of scientific analysis in Asia have challenged biomedical conceptions of what can be achieved with this treatment method. The scale of research activity in relation to acupuncture and women’s health has increased over the last 20 years.
Objective
This review aims to explore the research evidence in relation to acupuncture use for women’s reproductive disorders, focusing on both clinical findings and experimental research on acupuncture’s mechanisms of action in relation to women’s health.
Methods
A narrative literature search was undertaken using searches of electronic databases and manual searches of journals and textbooks. The search included all literature published prior to June 2013. The literature was assessed as to the nature of the study it was reporting and findings synthesized into a commentary.
Results
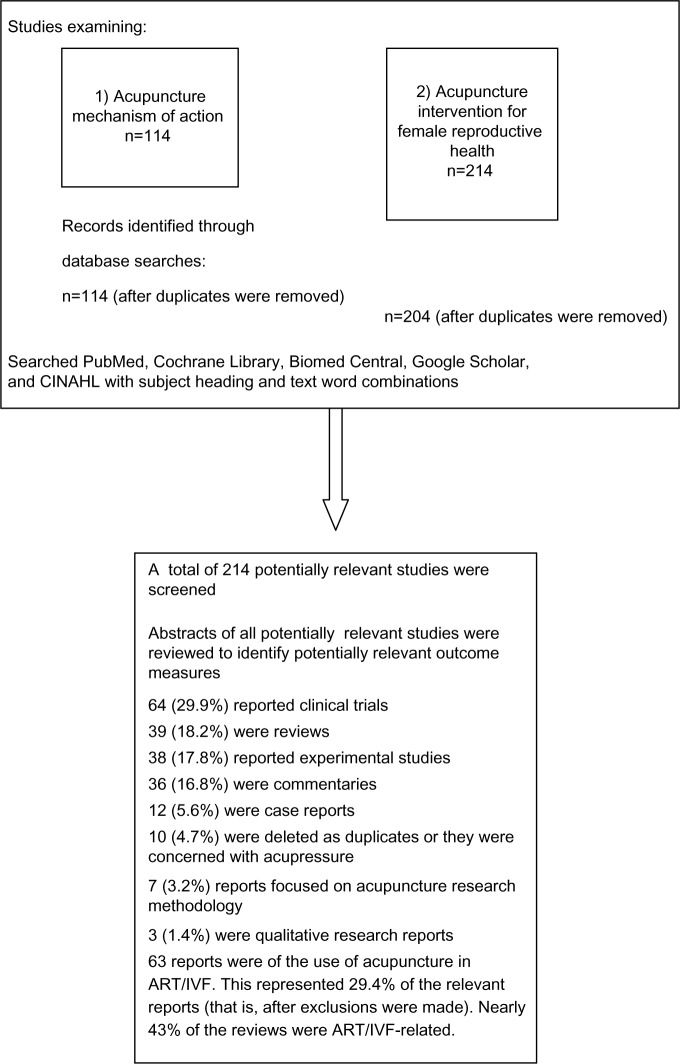
For acupuncture’s mechanism of action the search resulted in 114 relevant documents; in relation to clinical reports on the use of acupuncture for women’s health 204 documents were found and assessed.
Conclusion
There is preliminary data indicating acupuncture may improve menstrual health and coping for women experiencing delays falling pregnant. There is experimental data showing that acupuncture can influence female reproductive functioning, although the actual mechanisms involved are not yet clarified. Further well-conducted clinical research would benefit our understanding of the usefulness of acupuncture to women’s health.
Keywords: reproductive disorders, women, health, Chinese medicine, alternative medicine, acupuncture
Introduction
Gynecological health is recognized as being responsive to traditional East Asian medicine. Traditional Chinese medicine (TCM) includes the modalities of acupuncture and Chinese herbal medicine, which are increasingly utilized outside of Asia for the treatment of women’s health disorders.
This review focuses primarily on the use of acupuncture for female reproductive health. It addresses the current understandings of the physiology of acupuncture’s impact on female reproductive function and contemporary research on acupuncture for reproductive health disorders.
Historical origins of Chinese medical understandings of women’s reproductive health
Historical texts in Chinese medicine originally conceived of the male and female body as androgynous,1 gradually differentiating between treatments for women. As identified by the Song dynasty (960–1279 AD), a gynecological specialty had developed in both text and practice.1 Because of the foundation concepts of yin/yang, reproduction, for example, was not considered an exclusively female province. “The creation of the fetus was seen as an act performed by two equal partners, with yin and yang intermingling and stimulating each other.”2 Wilms2 goes on to quote Sun Si-Miao,3 who stated that “yin and yang blend in harmony, the two qi respond to each other, and yang bestows and yin transforms.” As well as recognizing reproduction as a joint effort, it was also Sun3 who famously said that the disorders of women are ten times more difficult to cure than those of males. Male causes of infertility were largely diagnosed as a result of insufficient qi.
For Chinese medicine, the female body, its health, sickness and treatment was deeply influenced by the idea that blood, as its energetic basis, flows around the body, is discharged through menstruation, feeds the unborn child and transforms into breast milk.4
Interventions to assist health and, therefore, to foster a healthy reproductive life, must nourish and regulate blood, and dispel any pathogens that interfere with or congest its free circulation. From the Song dynasty onwards, it was noted that, “blood is the root of women is the aphorism that guides gynaecological treatment.”2 Chen5 advises:
[…] Whenever treating disease, one first needs to discuss what [a particular case] is ruled by. In men, regulate their qi; in women, regulate their blood […] Thus in women, blood is the foundation. When qi and blood flow freely, their spirit is naturally clear.5
This idea of the primacy of blood in women’s health has not faded, and it is still part of contemporary TCM gynecology, although with a more nuanced and differentiated understanding. By late imperial China,
“Doctors recognized three broad categories of illness that directly impaired a woman’s ability to conceive: menstrual irregularity, ‘girdle discharges’ (dai xia, namely, pathological vaginal flows), and internal accumulations”.6
Weakening of the key foundations of reproductive health in Chinese medical theory – the kidney, blood, and uterus – can be attributed in biomedicine to inherited genetic defects; it can also be accounted for by overwork; too little rest or injury from too much menstrual bleeding; emotional disorders such as anxiety, worry, or depression; improper diet such as an excess of food or alcohol; or too much chilled food. Contemporary TCM practitioners, such as Song,7 also argue that medicines and other medical interventions can seriously damage a woman’s reproductive capacity, such as the long-term use of the contraceptive pill or other hormonal contraceptives, and they can damage the lining of the uterus through (perhaps unnecessary) treatments like dilation and curettage.
The menses cycle at the center of reproduction
Female health and fertility is intimately related to menstrual health. From a Chinese medical perspective, cyclical disorders (“yuejingbing”) are both indicative of and causal in subfertility. “The TCM approach to infertility treatment integrates the menstrual cycle as a simple, non-invasive, sensitive, motivational, diagnostic tool to understanding a woman’s fertility status.”8 Unlike assisted reproductive technologies (ART), which seek to override menstrual cycle difficulties by artificially controlling a woman’s cycle through pharmaceutical and surgical interventions, TCM considers delayed ovulation, excessive or scanty menstrual flow, dysmenorrhea, premenstrual symptoms, and short or long menstrual cycles as diagnostic signs, and a means through which interventions can enhance reproductive health. The idea of varying or staging treatment according to developments in the menstrual cycle has a long history in Chinese medicine and has contemporary expression in the work of Nanjing (Jiangsu, People’s Republic of China) gynecologist, Xia,9 who advocated the use of basal body temperature in identifying the wax and wane of yin, yang, qi, and blood throughout the cycle.
Historically, acupuncture has received less attention as an intervention in women’s health, and the acupuncture department of a TCM hospital usually offers generalized services, and it does not usually specialize in gynecology. Interest in the usefulness of acupuncture in reproductive medicine has come from a range of sources, including from experimental studies on the mechanisms of acupuncture, reports from clinical trials, and the experience of women who incorporate nonconventional practices into their health care.
Literature search strategy
This narrative review included searches of various databases – PubMed (National Center for Biotechnology Information, US National Library of Medicine, Bethesda, MD, USA), CINAHL® (EBSCO Industries, Inc., Ipswich, MA, USA), Biomed Central (London, UK), Cochrane Library (John Wiley & Sons, Ltd, Oxford, UK), and Google Scholar (Google Inc., Menlo Park, CA, USA) – and hand searches of texts and journals (Figure 1). Electronic search strategies were developed to identify English language reports (abstracts or full texts) of studies pertaining to:
Figure 1.
Flow chart of the search strategies used with electronic databases.
Abbreviations: n, number; ART, assisted reproductive technologies; IVF, in vitro fertilization.
Acupuncture mechanism of action, employing the keywords “acupuncture”, “mechanism”, “mechanisms of action”, and “physiology”; and
The use of acupuncture in relation to women’s reproductive health, including the keywords “acupuncture”, “reproduct*”, “*fertil*”, “ovula*”, and “menstru*.”
The searches included all accessible articles that were published until June 2013 with these keyword combinations.
Many of the acupuncture mechanism articles10–14 yielded reports where (in animal and human experimental models) clear physiological effects, and (in animal models) therapeutically relevant outcomes (such as anesthesia) vary as a function of the acupuncture prescription or technique used. While it is acknowledged that the correlation between animal and human physiology has been questioned,15 and that the complexity of human reproduction may not be replicated in animal models, the studies indicate that there are mechanical, neural, hormonal, and immune responses to acupuncture, and the new application of functional magnetic resonance imaging provides compelling evidence regarding how the brain responds to acupuncture needling. These general data have been excluded here, and the focus will be exclusively on the mechanisms of acupuncture research in gynecology.
The clinical research articles are diverse in terms of their research focus and methodology. Historically, most acupuncture research has focused on acupuncture’s possibilities for pain management, and within the last decade, attention has been paid to its effects on reproductive health. Only 30% of the articles retrieved were clinical trial reports, and 18% were reviews attempting to summarize the research. Several reviews were narrative commentaries rather than systematic reviews (SRs). The value of acupuncture in assisting ART/in vitro fertilization (IVF) has become the most dominant research question.
Acupuncture mechanisms of action in female reproduction
In an overview of the use of acupuncture in gynecology, Napadow et al16 stated that in her view, recent basic and clinical research has demonstrated that acupuncture regulates uterine and ovarian blood flow (OBF), and that the effect is most likely mediated as a reflex response via the ovarian sympathetic nerves, and that the response is controlled via the supraspinal pathways. Since this encourages a thicker uterine wall, fertility is improved through embryo implantation being more successful. In a Stener-Victorin et al study17 (number [n] =10 healthy women), compared to the mean baseline pulsatility index, the mean pulsatility index was significantly reduced both shortly after the eighth electroacupuncture (EA) treatment (P<0.0001), and 10–14 days after the EA period (P<0.0001). EA applied to the abdomen and hind limb of laboratory animals modulates the OBF response:
[…] as a reflex response via the ovarian sympathetic nerves, and the response was controlled via supraspinal pathways. Furthermore, the OBF response to segmental abdominal EA stimulation was frequency dependent and amplified in the estrous phase.18
In another animal study of induced polycystic ovarian syndrome (PCOS), ovarian function normalized in response to both exercise and EA (P<0.05 compared to control).19 A further study by Stener-Victorin research group found that low-frequency EA and exercise ameliorate insulin resistance in rats with PCOS. They hypothesized that the effect may involve regulation of adipose tissue metabolism and production because EA and exercise each partially restore divergent adipose tissue gene expression associated with insulin resistance, obesity, and inflammation. In contrast to exercise, they found that EA improves insulin sensitivity and modulates adipose tissue gene expression without influencing adipose tissue mass and cellularity.16,20,21
A more recent animal study of endometrial damage (thin and impaired) induced by clomiphene citrate (which is estimated to cause the majority of implantation failures) found that it was not the endometrial thickness (P=0.07), but the glandular area (P=0.01) of the endometrium that was significantly increased in the acupuncture group compared with the control group. The authors suggest that acupuncture may have the capacity to mainly stimulate the growth of the gland rather than the stoma, which cannot be observed by ultrasound in a clinical setting.22
This study found that acupuncture significantly suppressed the high serum estradiol levels induced by clomiphene citrate to better prepare for implantation, and it also increased the glandular area and the expression of receptivity markers during the implantation period. The acupuncture protocol and technique used were consistent with standard TCM care. These conclusions were not supported by evidence from Smith et al,23 and the inconsistency perhaps can be explained by Fu et al,22 who identified an alternative mechanism by assessing endometrial thickness through dissection rather than ultrasound.
Further, acupuncture causes a significant increase in β-endorphin levels during treatment. A review of Japanese research supports the evidence that the analgesic effects of acupuncture have been well clarified by experimental studies, and that the participation of various endogenous opioids and their receptors has been widely accepted;24 however, they report that this seems to be an incomplete explanation of why, for example, acupuncture treats pain. It has been hypothesized that, because acupuncture impacts β-endorphin levels and thus hypothalamic function,25 which affect gonadotropin-releasing hormone secretion and the menstrual cycle, in turn, it is logical to hypothesize that acupuncture may positively influence ovulation and fertility.26 Zhu et al27 report that, as acupuncture increases endogenous opioids and the neurotransmitters serotonin and dopamine, this would lead to analgesia, sedation, and to the recovery of motor function, thus impacting on, for example, menstrual pain. The review also reported that acupuncture may induce visceral and somatic signals that are transmitted to the central nervous system to induce anti-inflammatory signals through both humoral and neural mechanisms.27
Research detailed by Al-Inany28 has postulated three potential mechanisms for acupuncture’s effects on fertility. Firstly, acupuncture may mediate the release of neurotransmitters, which may, in turn, stimulate secretion of gonadotropin releasing hormone, thereby influencing the menstrual cycle, ovulation, and fertility.29 Secondly, acupuncture may stimulate blood flow to the uterus by inhibiting uterine central sympathetic nerve activity.17 Thirdly, acupuncture may stimulate the production of endogenous opioids, which may inhibit the central nervous system’s outflow and the biological stress response.30 Animal studies indicate that intensive EA can facilitate substantial change in PCOS; that is, systemic and local effects involving intracellular signaling pathways in muscle that may account for the improved insulin sensitivity.12 Repeated low-frequency EA and physical exercise each improves hyperandrogenism and menstrual frequency in women with PCOS more effectively than no active intervention, with low-frequency EA being superior to physical exercise. These findings suggest that low-frequency EA may be used in the reduction of hyperandrogenism and oligo-/amenorrhea in women with PCOS.11
Stress is known to have a negative effect on reproduction and perhaps the menstrual cycle. As acupuncture, for example, aids in lowering stress hormones, which undermine fertility, it is thought that this may be a major mechanism for acupuncture to influence reproductive function and account for fertility-boosting effects. One study examining the levels of “stress hormones” – serum cortisol (CORT) and serum prolactin (PRL) – during an IVF cycle demonstrated biochemical differences in serum levels of CORT and PRL in patients receiving acupuncture along with their IVF treatments.31 CORT levels in the acupuncture group were significantly higher (P<0.05) on IVF medication days 7, 8, 9, 11, 12, and 13 when compared with controls. PRL levels in the acupuncture group were significantly higher (P<0.05) on IVF medication days 5, 6, 7, and 8 when compared with controls. This connection is demonstrated in further clinical studies (detailed in the following sections) of how stress reduction using acupuncture impacts reproductive health.
Acupuncture for female reproductive disorders
An overview of SRs of acupuncture in obstetrics and gynecology32 concluded that the data available in SRs was contradictory and inconclusive. An SR that undertook an overview of studies of acupuncture treatments for reproductive and gynecological disorders found that menopause and dysmenorrhea were the most frequently studied, and acupuncture treatments had shown positive indicators of effectiveness. Smith and Carmady33 found that acupuncture to treat premenstrual syndrome (PMS), PCOS, and other menstrual-related symptoms is understudied, and the evidence for acupuncture to treat these conditions is frequently based on single studies. This SR included all studies conducted prior to September 2009. The literature search undertaken here found 75 additional articles published since that time (including only those that focused on reproductive conditions; that is, excluding menopause). Not all would have met the inclusion criteria for the review, but all would have fallen within the search strategy.
Accumulated clinical experience indicates that acupuncture regulates the menstrual cycle. TCM gynecological textbooks all provide treatment approaches for a range of menstrual irregularities – whether the cycle is too short, too long, or too variable, the bleeding is too scant or too heavy, and menses are accompanied by a range of other symptoms such as abdominal pain, headache, acne, or mood changes.34–37 Those diagnosed with “idiopathic infertility or sterility,” or those with no known cause, often have a “hidden disturbance of gamete interaction,”38 where the ova are not maturing or not fertilizable, or there is disturbed sperm function and women often have accompanying PMS and dysmenorrhea. Kielwin et al38 argue that such couples profit the most from the possibilities of TCM, for example, in the areas of cycle optimization and timed intercourse. In a series of articles published in Nanjing in 1998–1999, Professor Xia Gui-cheng9 identified the importance of menstrual regulation both in the resolution of menstrual disorders and the promotion of fertility. His approach was subsequently adopted by Lyttleton,39 and broadcasted through her teaching and publications throughout the English-speaking TCM community. There are no published clinical trials that test the premise of regulating the menstrual cycle in order to promote fertility. There is a tradition within Western herbalism called multiphasic prescribing for menstruating women that mirrors this approach.40 There are studies, however, that do examine the influence of acupuncture on different aspects of the menstrual experience (discussed in detail in the following sections). Chinese medical theory would posit that an improvement in a single aspect of menstruation, such as dysmenorrhoea, will positively influence other aspects (and the whole menstrual function). Promoting the full discharge of blood, for example, during the menses will positively feedback into egg formation and ovulation. Evidence to support this assertion is not available at this time.
Stener-Victorin and Wu,41 in an overview of contemporary literature, found (as Smith and Carmady33 did) that the use of acupuncture to treat reproductive dysfunction has not been well investigated. They state that only a few clinical studies have been reported, most of which are flawed by poor design and a lack of valid outcome measures and diagnostic criteria, making the results difficult to interpret.41 The incidence of “poor quality” clinical studies perhaps speaks to the difficulty of achieving high-quality clinical research that is acceptable both to acupuncturists and research scientists. The following is a narrative review of clinical evidence for the effectiveness of reproductive/fertility related acupuncture interventions. This narrative review aimed to provide a broader perspective to the current evidence base by including animal and human studies, inclusive of all study designs, to provide a contemporary overview of the evidence.
Menstrual regulation
Menstrual irregularities may originate from a variety of conditions. Frequently in clinic, women have menstrual irregularities that stem from a diagnosis of PCOS. A recent literature review42 of reports of acupuncture use for PCOS found four studies that addressed this subject, although no randomized controlled trials (RCTs) were found. One study led by Stener-Victorin et al43 found that the “dose” of acupuncture influenced the size of the effect. The researcher concluded:
Experimental observations in rat models of steroid-induced polycystic ovaries and clinical data from studies in women with PCOS suggest that acupuncture exert (sic) long-lasting beneficial effects on metabolic and endocrine systems and ovulation.43
Indications are that repeated acupuncture can stimulate the return of ovulation without adverse side effects. An RCT since completed by Lim (personal communication, 2010) indicates that acupuncture, as compared to sham acupuncture (sham acupuncture refers to a control group which may include invasive needling or no invasive needling), is efficacious for initiating ovulation in women with PCOS. Acupuncture and moxibustion have good regulatory effects on the function of endocrine, glucose, and lipid metabolism,44 so they can be hypothesized to be useful in regulating the menstrual cycle. Although unable to discern a difference between the true and sham acupuncture protocols for women with PCOS, both groups had a similar improvement in their luteinizing hormone/follicle-stimulating hormone ratio;45 the findings support acupuncture as a possible nonpharmaceutical treatment for PCOS.
An exploration of the physiological effects on PCOS of major complementary and alternative medicine (CAM) treatments indicates that they could reduce the severity of PCOS and its complications. Acupuncture has been shown to reduce hyperandrogenism and improve menstrual frequency in PCOS.46,47
An analysis of clinical trials48 of the effect of acupuncture-induced weight reduction on menstrual activity identified acupuncture treatment achieving the effects of weight reduction and menstrual improvements via regulating activities of leptin, the thyroid gland system, and the hypothalamus–pituitary–adrenal cortex axis. The authors report that clinical practice has demonstrated that acupuncture stimulation of some commonly-used acupoints for weight reduction also exhibits favorable regulation on menstrual activity in obese women.
Shi et al49 undertook a clinical trial of patients with one defined type of PCOS, comparing a herbal intervention with the same herbal intervention plus acupuncture. The results demonstrated a total effectiveness rate of 93.8% on hormonal and menstrual measures in the combined acupuncture and Chinese herb group, and 80.6% in the simple Chinese herb group, the former being significantly better than the latter (P<0.05). The decrease of testosterone in the combined acupuncture and Chinese herb group was significantly superior to that in the simple Chinese herb group (P<0.01).
In a study contrasting real and sham acupuncture for the symptoms of PCOS, Pastore et al46 found improvements in the luteinizing hormone to follicle-stimulating hormone ratio in both arms, and the increase in menstrual frequency during the trial compared with pre-enrollment suggests that both interventions may have been beneficial. As well as confirming the likelihood of sham acupuncture not being inert, the lack of an observational control and/or of pre-enrollment ovulation data meant that the improvement could not be accurately assessed.
Anovulatory disorders most frequently display with menstrual irregularity. Assisting ovulation can be a way of reestablishing a regular cycle. The use of acupuncture for amenorrhea is supported by case reports and small cohort studies, but there has been insufficient clinical research on this topic to date.50
Ovulation
Acupuncture has been shown to assist ovulation through the early work of Yu Jin who found that 50% of the incidence of chronic anovulation (diagnosed by menstrual disorder history, consecutive monophasic basal body temperature for 3 months, serum hormone, and pelvic ultrasonography data) could be reversed successfully by using acupuncture. She further found:
[…] in pubertal dysfunctional uterine bleeding, 87.7 percent; in pubertal oligomenorrhea, 60 percent; and in PCOS, 36.8 percent […] This correlation suggests patients with sympathetic activity suppressed by acupuncture (a sign of fluent flow of Qi and blood in TCM) are likely to ovulate after acupuncture.51
Yu 52 further comments that acupuncture is especially effective when infertility is caused by a hypothalamic disorder. If patients are screened to include those most likely to respond (for example, those with adequate estrogen levels), the success rate can be as high as 80% in achieving ovulation. Ovulation delay or failure is a common occurrence in women with PCOS and can be an aspect of other subfertility conditions.53
Some investigations have already demonstrated that acupuncture has positive effects on anovulation. Studies include the clinical application of ovulation induction54,55 and the use of EA for women with PCOS over several months to initiate menstrual cycles.56,57 Women in this latter study were carefully monitored for hormonal changes, skin temperature, basal temperature, body mass index, and waist-to-hip ratio, allowing the researchers to hypothesize the mechanisms of action of the acupuncture. The participants who responded best were almost consistently characterized by comparatively low body mass index, waist-to-hip ratio, as well as basal insulin and testosterone serum concentrations, but high serum testosterone/sex hormone-binding globulin concentrations. Consequently, they were less androgenic and had a less pronounced metabolic disturbance. The authors theorized that a higher dose of acupuncture for either a longer time or more frequently may have produced better results in the non-responders.
Menstrual pain
Dysmenorrhea is an important indicator of disturbed menstrual flow. Two recent SRs examine the evidence for acupuncture in alleviating menstrual pain.27,58 One review by Zhu et al of menstrual pain originating from endometriosis could only find one RCT that met the inclusion criteria, and the authors could make no real assessment of the value of acupuncture based on this one study. The other SR conducted by Smith et al59 addressed studies of dysmenorrhea more generally, and included ten trials. Although the authors concluded that the data were insufficient to confidently evaluate acupuncture as a treatment for dysmenorrhea, because of methodological problems in the trials, most reported positive outcomes for acupuncture. Some of the research not covered in the SRs will be discussed.
One experimental blinded crossover study60 explored the impact of “real” and “sham” acupuncture on heart rate variability as an indicator of the autonomic nervous system in women with primary dysmenorrhea. The researchers found that both real and sham acupuncture affected heart rate variability but in different ways. The researchers concluded that manual acupuncture at bilateral acupoints of LI4 and SP6 may play a role in dysmenorrhea treatment with autonomic nervous system involvement.60 One clinical trial of two different acupuncture interventions for dysmenorrhea during menses for three cycles showed significant decreases in the severity and frequency of pain. The study also indicated no significant difference in outcomes between the two interventions, supporting the idea that there may be more than one successful prescription.61 An RCT that explored the timing and point combinations for dysmenorrhea found that treating patients using multiple points before menstruation is better than immediately addressing pain for the improvement in symptoms of dysmenorrhea. In addition, it was also found that a single point is better than multiple points when immediately treating at pain occurrence. This trial suggests that Shiqizhui (EX-B8) should be chosen as a convenient point.62 Another pair of studies suggests that needling at Sanyinjiao SP6 can immediately improve the uterine arterial blood flow of patients with primary dysmenorrhea, thereby relieving the pain.63,64 Further study of the timing of acupuncture for dysmenorrhea65 found no significant difference between applying it premenstrually or during menses, but there was a significant positive difference when compared to the control group, who received no acupuncture at all. In another study66 the importance of timing was further refined to distinguish between those receiving “preconditioning” acupuncture, and those receiving immediate acupuncture, and both groups were compared with a non-treated third arm. Into the second and third month, the outcomes for the preconditioning acupuncture group outstripped those of the immediate acupuncture group, and they both showed significant improvements when compared to the control. Despite encouraging indications, another SR concluded that because of low methodologic quality and small sample size, there is no convincing evidence for acupuncture in the treatment of primary dysmenorrhea.67 A later review58 found more methodologically sound trials and concluded that there is promising evidence in the form of RCTs for the use of acupuncture in the treatment of primary dysmenorrhoea compared with pharmacological treatment or herbal medicine:
The evidence for the effectiveness of acupuncture for the treatment of primary dysmenorrhoea is not convincing compared with sham acupuncture.68
A third review conducted the following year found that acupuncture may reduce period pain; however, there is a need for further well-designed randomized controlled trials.58
Premenstrual syndrome
PMS arises because of imbalances that are triggered in the lead up to a period. A SR of acupuncture interventions found that although the included trials showed that acupuncture may be beneficial to patients with PMS, there is insufficient evidence to support this conclusion due to methodological flaws in the studies.69 In one SR70 of acupuncture use for PMS, the pooled results demonstrated that acupuncture is superior to all controls (eight trials; pooled risk ratio [RR]: 1.55; 95% confidence interval [CI]: 1.33–1.80; P<0.00001). The meta-analysis comparing the effects of acupuncture with different doses of progestin and/or anxiolytics supported the use of acupuncture (four trials; RR: 1.49; 95% CI: 1.27–1.74; P<0.00001). In addition, acupuncture significantly improved symptoms when compared with sham acupuncture (two trials; RR: 5.99; 95% CI: 2.84–12.66; P<0.00001). No evidence of harm resulting from acupuncture emerged. A more recent review71 concurred that the available data included in this review showed that acupuncture may be beneficial for patients with PMS, but it also noted the methodological flaws in many of the studies. Guo and Ma71 also commented on the importance of timing of the treatment for periodic disorders such as PMS. The authors found that an acupuncture intervention for PMS was usually performed 2 weeks prior to menses and stopped shortly after the start of the menstrual flow. The treatment should last 3 months to achieve satisfactory results.71
Infertility
Acupuncture has been a treatment for infertility and menstrual disorders throughout the history of Chinese medicine.72 Differing approaches are evident in the literature,73 and achieving a common consistent TCM diagnosis and treatment is difficult.74
Acupuncture and ART
A major research effort in the last decade has indicated that acupuncture assists IVF. The literature search identified 15 reports that identified themselves as a review of studies of acupuncture interventions as adjuncts to IVF/ART. A recent SR75 includes ten more studies not included in earlier SRs, and concludes that acupuncture improves the clinical pregnancy rate and live birth rate among women undergoing IVF based on the results of the studies that do not include the Streitberger control (the Streitberger is a type of sham needle), and that the Streitberger control may not be an inactive control.75 The meta-analysis results showed that the pooled clinical pregnancy rate from all of the acupuncture groups was significantly higher than that from all of the control groups (P=0.04). The difference was more obvious when the studies that used the Streitberger control were not considered (P=0.007), suggesting that the Streitberger control needs reevaluation. The reviewers further recommend that more positive effects from acupuncture in IVF can be expected if an appropriate control and more individualized acupuncture programs are used. Another review has since challenged this finding, and concluded that there is no pooled benefit of adjuvant acupuncture for IVF.76
Six SRs (including five meta-analyses) have shown that acupuncture on the day of embryo transfer (ET) has improved pregnancy rates in IVF.77 None of the reviews call for a rejection of this intervention and all, in fact, call for more exploration of its value to enhance IVF cycles. Although the intervention is assessed as being relatively painless and causing few side effects, another review78 implies that the cost, invasiveness, and potential for the harm of acupuncture means that it should not be recommended for women receiving IVF treatment. Given that the studies reported very few adverse events and that the cost of acupuncture compared to additional IVF cycles is substantially less, it can only be surmised that these SR authors were in some way biased against the intervention to make such a conclusion. Manheimer et al,79 for example, conclude that the effects are significant and clinically relevant but they are “still somewhat preliminary.” Another meta-analysis shows that acupuncture around the time of the ET achieves a higher live birth rate of 35% compared to 22% without active acupuncture.80
More recent clinical trials since the Cheong SR have thrown this conclusion into doubt. The published studies include those by Domar et al,81 Moy et al,82 So et al,83 and Andersen et al84 and, if the results of these 1,311 patients were added to those of the meta-analysis, it is unlikely that there is conclusive evidence of a major effect of acupuncture accompanying ET.85 Anderson and Rosenthal86 conclude that despite 40 clinical trials and 9 systematic reviews investigating the efficacy of acupuncture for improving IVF outcomes:
[…] evidence-based guidelines are difficult to devise. The methodology used in the clinical trials does not closely resemble the use of acupuncture in real world acupuncture clinics, limiting the applicability of this research.86
In addition to the need for acupuncture protocols to be reviewed and adjusted in response to changing protocols for ET, there are many confounding aspects of these studies that need to be examined, such as the effects of the use of placebo or sham acupuncture, the practice of using minimally trained acupuncturists, and outcome measures that do not include live births. Drawing on experience-based practice and three decades of research, Shi et al87 questioned the value of the Moy et al study on several grounds, including the authors’ failure to document the proficiency of the acupuncturists, their inattention to the multiple causes of infertility displaying uniquely in each participant, and the lack of an appropriate “dose” of acupuncture. While identifying the flaws in the trial design of the included studies (and suggesting that these are general difficulties encountered in evaluating the efficacy of acupuncture in subfertility), another less rigorous SR concluded that the pregnancy rate of IVF treatment is significantly increased when acupuncture is administered on the day of ET.88 Another review,89 while not a systematic appraisal, offers a discussion of how Chinese medicine and, particularly, acupuncture is helpful to infertility. The SRs found sufficient homogeneity between the studies to be able to include them in a review.
The research studies make clear that, despite the consistency across studies, there was also much diversity. The actual acupuncture treatment protocols used varied across studies. Moreover, the person administering the acupuncture was not always trained in acupuncture. Another factor in the studies was that the timing and, therefore, the location of the treatment appears to have impacted on outcomes. Off-site acupuncture treatments, for example (as reported by Craig et al90) failed to show any benefit for the women treated (this was not the case, however, in Johnson’s91 audit of the cases of women treated off-site). In addition, women receiving intracytoplasmic sperm injection and acupuncture, along with agents for ovarian stimulation, produced more follicles than women who did not receive acupuncture.92 There has been additional positive support for acupuncture in conjunction with ET from a retrospective case audit.93
The issue of whether the acupuncture protocols used in these studies reflect good clinical practice is important. If acupuncture is to be included as an adjunct therapy for IVF or other infertility patients, then the study results need to be able to be replicated in practice and adopted by acupuncturists outside IVF clinics. The results of the research studies provide significant support, but not statistically significant results, for acupuncture performed on the day of ET. Beyond this evidence, the dosage or number of acupuncture treatments was very low in these trials. TCM diagnoses were mostly not employed to guide treatment (although Smith94 used it to guide the first treatment and So84 recorded the diagnosis for comparative purposes), which potentially creates a fixed protocol bias and reduces the likelihood that the treatment will be appropriate and effective for individual subjects.95
Despite some recent evidence that CAM use (although acupuncture as a CAM modality was not distinguished from other interventions) may have a negative impact on ART outcomes,96 this has been contradicted by a more recent SR,97 which states that there is preliminary evidence to suggest that some of these CAM modalities may be effective adjuncts in fertility treatments. The suggestion is made that the clinical trials reviewed have not been of a sufficient scale to provide unequivocal evidence for or against acupuncture use during IVF, by showing that acupuncture may increase pregnancy rates and live births. Other criticisms of the SRs themselves include that the findings and conclusions between systematic reviews:
[…] differ on the effect of acupuncture and live birth rates, due to variation in their inclusion criteria, the inclusion of new trials in subsequent meta-analyses, and variations in the quality of the acupuncture intervention which may have contributed to clinical heterogeneity.98
Acupuncture in research has been focused on improving the outcomes of fertility treatments, most notably in IVF cycles, especially at the point of ET. It has been hypothesized on the basis of a small study that acupuncture has a beneficial effect at the time of ET because it is a time of great stress for women, which may cause uterine vasoconstriction; moreover, acupuncture can significantly modify these stress levels.99,100 In support of this view, Domar et al81 found that acupuncture led to reduced anxiety, as well as increased relaxation and optimism, although So et al83 found no differences in anxiety levels between the women receiving acupuncture or placebo.
Acupuncture and natural fertility
Outside the context of IVF clinics, there has been research that supports the role of acupuncture in promoting women’s reproductive health. As reviewed earlier, findings on the physiological mechanisms of acupuncture offer some guidance in understanding the possible contribution that acupuncture makes to menstrual health. A currently unpublished pilot study by the authors found that using a specialist acupuncture protocol101 and applying clinical trial research methodology to acupuncture for natural fertility in women was both feasible and useful for the women receiving the acupuncture intervention. Other research reports of Chinese medicine’s supportive contribution to fertility largely consist of case reports.
Clinical case reports support the value of acupuncture in the lead up to conception, although no clinical trial has been reported to date that either supports or contradicts this case-based evidence.39,91,92,102 Acupuncture has a long history in the treatment of fertility problems, and there is apparently much consistency in the actual points chosen.72.101 Chinese medicine texts and case history books, for example, frequently cite the use of acupuncture to induce ovulation. A study by Qiong using acupuncture in women with endometriosis-induced infertility, reported in a recent publication on infertility,103 indicated significant effectiveness. In the same publication, there is a report of a study undertaken by Ding104 regarding tubal infertility that was effectively treated by acupuncture.
Summary of research
Further clinical trials are required to establish how the experimental results discussed in the previous sections unfold in a clinical context. Theoretically, from a Chinese medicine perspective, an acupuncture approach should prove effective for women with reproductive health problems, whether they are enrolled in an IVF program or not. Acupuncture, even a standardized acupuncture protocol such as the Paulus et al105 protocol, performed before and after an IVF biomedical procedure, represents a complex intervention. A Chinese medical understanding (as opposed to a physiological or a biomedical one) of an adequate acupuncture intervention would require at least the differentiation of patterns of symptoms, individualization of treatments, perhaps an assessment of qi circulation, and/or more extended treatment times, in addition to paying attention to the timing of a surgical procedure. Standardization might reduce the effect of acupuncture in individual patients.106 Little research is available that applies a more traditionally acceptable acupuncture protocol to facilitate fertility.
Both the experimental and clinical research studies have yielded interesting but inconclusive findings. The effects of acupuncture are apparently multimodal using physiological, endocrine, and neurological pathways to precipitate changes in the body, including to women’s reproductive functioning. Similarly, clinical trials offer promising evidence of reproductive outcomes initiated by a variety of acupuncture interventions. Clinical research into acupuncture efficacy has been heavily criticized for methodological flaws and bias. Most SRs find a large proportion of studies that fail to meet inclusion criteria on the basis of their methodology. The evidence within this biomedical framework is certainly not conclusive, and this has led some researchers to reapply their efforts to explaining the physiology of women’s responses to acupuncture more precisely, while others have been focused on better constructing clinical trials that identify whether clinically significant changes are occurring in women’s reproductive health using an acupuncture intervention.
Conclusion
We have preliminary data indicating that acupuncture may improve menstrual health and coping among women experiencing delays in becoming pregnant. There are experimental data indicating that acupuncture can influence female reproductive functioning, although the actual mechanisms involved are not yet clarified. Acupuncture is a complex intervention yet the evaluation of acupuncture research designs and outcome measures expect a level of commensurability difficult to achieve in complex interventions. A focus on effectiveness rather than efficacy may be a solution. Further research that is informed by the experience in the rich traditions of acupuncture practice and the rigorous methods of evidence-based research is needed.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Furth C. A Flourishing Yin: Gender in China’s Medical History, 960–1665. Berkeley, CA: University of California Press; 1999. [Google Scholar]
- 2.Wilms S. Prolegomena. In: Wilms S, editor. Bei Ji Jin Yao Fang – Essential Prescriptions Worth A Thousand in Gold for Every Emergency. Portland, OR: The Chinese Medicine Database; 2011. [Google Scholar]
- 3.Sun S-M. <Bei Ji Qian Jin Yao Fang> Essential Prescriptions worth a Thousand in Gold for every emergency. Wilms S, trans652.
- 4.Valussi E. Blood, tigers, dragons: The physiology of transcendence for women. Asian Med. 2008;4(1):46–85. [Google Scholar]
- 5.Chen Z-M. <Fu Ren Da Quan Liang Fang> ‘Compendium of Good Remedies for Women’. p. 1237.
- 6.Wu YL. Reproducing Women: Medicine, Metaphor, and Childbirth in Late Imperial China. Berkeley, CA: University of California Press; 2010. [Google Scholar]
- 7.Song XK. Treating infertility in traditional Chinese medicine. European Journal of Oriental Medicine. 2009;6(1):10–11. [Google Scholar]
- 8.Ried K, Stuart K. Efficacy of Traditional Chinese Herbal Medicine in the management of female infertility: a systematic review. Complement Ther Med. 2011;19(6):319–331. doi: 10.1016/j.ctim.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Xia GC. Menstrual cycle and menstrual regulation. Journal of Nanjing University of Traditional Chinese Medicine. 1998;4 [Google Scholar]
- 10.Langevin HM, Wayne PM, Macpherson H, et al. Paradoxes in acupuncture research: strategies for moving forward. Evid Based Complement Alternat Med. 2011;2011:180805. doi: 10.1155/2011/180805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jedel E, Labrie F, Odén A, et al. Impact of electro-acupuncture and physical exercise on hyperandrogenism and oligo/amenorrhea in women with polycystic ovary syndrome: a randomized controlled trial. Am J Physiol Endocrinol Metab. 2011;300(1):E37–E45. doi: 10.1152/ajpendo.00495.2010. [DOI] [PubMed] [Google Scholar]
- 12.Johansson J, Feng Y, Shao R, Lönn M, Billig H, Stener-Victorin E. Intense electroacupuncture normalizes insulin sensitivity, increases muscle GLUT4 content, and improves lipid profile in a rat model of polycystic ovary syndrome. Am J Physiol Endocrinol Metab. 2010;299(4):E551–E559. doi: 10.1152/ajpendo.00323.2010. [DOI] [PubMed] [Google Scholar]
- 13.Wu MT, Sheen JM, Chuang KH, et al. Neuronal specificity of acupuncture response: a fMRI study with electroacupuncture. Neuroimage. 2002;16(4):1028–1037. doi: 10.1006/nimg.2002.1145. [DOI] [PubMed] [Google Scholar]
- 14.Cabioglu MT, Surucu HS. Acupuncture and neurophysiology. Medical Acupuncture. 2009;21(1):13–20. [Google Scholar]
- 15.Perel P, Roberts I, Sena E, et al. Comparison of treatment effects between animal experiments and clinical trials: systematic review. BMJ. 2007;334(7586):197. doi: 10.1136/bmj.39048.407928.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Napadow V, Ahn A, Longhurst JC, et al. The status and future of acupuncture mechanism research. J Altern Complement Med. 2008;14(7):861–869. doi: 10.1089/acm.2008.SAR-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stener-Victorin E, Waldenström U, Andersson SA, Wikland M. Reduction of blood flow impedance in the uterine arteries of infertility women with electro-acupuncture. Hum Reprod. 1996;11(6):1314–1317. doi: 10.1093/oxfordjournals.humrep.a019378. [DOI] [PubMed] [Google Scholar]
- 18.Stener-Victorin E, Fujisawa S, Kurosawa M. Ovarian blood flow responses to electroacupuncture stimulation depend on estrous cycle and on site and frequency of stimulation in anesthetized rats. J Appl Physiol (1985) 2006;101(1):84–91. doi: 10.1152/japplphysiol.01593.2005. [DOI] [PubMed] [Google Scholar]
- 19.Manni L, Lundeberg T, Holmäng A, Aloe L, Stener-Victorin E. Effect of electro-acupuncture on ovarian expression of alpha (1)- and beta (2)-adrenoceptors, and p75 neurotrophin receptors in rats with steroid-induced polycystic ovaries. Reprod Biol Endocrinol. 2005;3:21. doi: 10.1186/1477-7827-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mannerås L, Jonsdottir H, Holmäng A, Lönn M, Stener-Victorin E. Low frequency electro-acupuncture and physical exercise improve metabolic disturbances and modulate gene expression in adipose tissue in rats with dihydrotestosterone-induced polycystic ovary syndrome. Endocrinology. 2008;149(7):3559–3568. doi: 10.1210/en.2008-0053. [DOI] [PubMed] [Google Scholar]
- 21.Mannerås L, Cajander S, Holmäng A, et al. A new rat model exhibiting both ovarian and metabolic characteristics of polycystic ovary syndrome. Endocrinology. 2007;148(8):3781–3791. doi: 10.1210/en.2007-0168. [DOI] [PubMed] [Google Scholar]
- 22.Fu H, He Y, Gao Y, Man Y, Liu W, Hao H. Acupuncture on the endometrial morphology, the serum estradiol and progesterone levels, and the expression of endometrial leukaemia-inhibitor factor and osteopontin in rats. Evid Based Complement Alternat Med. 2011;2011:606514. doi: 10.1155/2011/606514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith CA, Coyle M, Norman RJ. Does acupuncture improve the endometrium for women undergoing an embryo transfer: a pilot randomised controlled trial. Australian Journal of Acupuncture and Chinese Medicine. 2009;4(1):7–13. [Google Scholar]
- 24.Okada K, Kawakita K. Analgesic action of acupuncture and moxibustion: a review of unique approaches in Japan. Evid Based Complement Alternat Med. 2009;6(1):11–17. doi: 10.1093/ecam/nem090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petti F, Bangrazi A, Liguori A, Reale G, Ippoliti F. Effects of acupuncture on immune response related to opioid-like peptides. J Tradit Chin Med. 1998;18(1):55–63. [PubMed] [Google Scholar]
- 26.Duggan EA. Acupuncture, endometriosis and in vitro fertilization. Journal of the Association of Chartered Physiotherapists in Women’s Health. 2008;103:45–49. [Google Scholar]
- 27.Zhu X, Hamilton KD, McNicol ED. Acupuncture for pain in endometriosis. Cochrane Database Syst Rev. 2011;(9):CD007864. doi: 10.1002/14651858.CD007864.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Inany H. Acupuncture for infertility: a recently released evidence. Mid East Fertil Soc J. 2008;13(1):67. [Google Scholar]
- 29.Ferin M, Vande Wiele R. Endogenous opioid peptides and the control of the menstrual cycle. Eur J Obstet Gynecol Reprod Biol. 1984;18(5–6):365–373. doi: 10.1016/0028-2243(84)90059-5. [DOI] [PubMed] [Google Scholar]
- 30.Han JS, Chen XH, Sun SL, et al. Effect of low- and high-frequency TENS on Met-enkephalin-Arg-Phe and dynorphin A immunoreactivity in human lumbar CSF. Pain. 1991;47(3):295–298. doi: 10.1016/0304-3959(91)90218-M. [DOI] [PubMed] [Google Scholar]
- 31.Magarelli PC, Cridennda DK, Cohen M. Changes in serum cortisol and prolactin associated with acupuncture during controlled ovarian hyperstimulation in women undergoing in vitro fertilization-embryo transfer treatment. Fertil Steril. 2009;92(6):1870–1879. doi: 10.1016/j.fertnstert.2008.10.067. [DOI] [PubMed] [Google Scholar]
- 32.Ernst E, Lee MS, Choi TY. Acupuncture in obstetrics and gynecology: an overview of systematic reviews. Am J Chin Med. 2011;39(3):423–431. doi: 10.1142/S0192415X11008920. [DOI] [PubMed] [Google Scholar]
- 33.Smith CA, Carmady B. Acupuncture to treat common reproductive health complaints: An overview of the evidence. Auton Neurosci. 2010;157(1–2):52–56. doi: 10.1016/j.autneu.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 34.Maciocia G. Obstetrics and gynecology in Chinese medicine. New York, NY, USA: Churchill Livingstone; 1998. [Google Scholar]
- 35.Marchment R. Gynaecology revisited: Obstetrics and gynaecology for practitioners of Chinese medicine. Sydney: Elsevier Australia; 2007. [Google Scholar]
- 36.Flaws B. My sister the moon: The diagnosis and treatment of menstrual diseases of traditional Chinese medicine. Boulder: Blue Poppy Press; 1992. [Google Scholar]
- 37.Hou Jl., editor. Acupuncture and moxibustion therapy in gynecology and obstetrics. Beijing: Beijing Science & Technology Press; 1995. [Google Scholar]
- 38.Kielwin K, Sulistyo-Winarto FX, Friol K, Gnoth C. Fertility treatment and pregnancy – reproductive medicine and TCM in meaningful cooperation. In: Noll AA, Wilms S, editors. Chinese Medicine in Fertility Disorders. Stuttgart, Germany: Thieme; 2010. pp. 42–71. [Google Scholar]
- 39.Lyttleton J. Treatment of Infertility with Chinese Medicine. 1st ed. Edinburgh, Scotland: Churchill Livingstone; 2004. [Google Scholar]
- 40.Yarnell E, Abascal K. Multiphasic herbal prescribing for menstruating women. Alternative and Complementary Therapies. 2009;15(3):126–134. [Google Scholar]
- 41.Stener-Victorin E, Wu X. Effects and mechanisms of acupuncture in the reproductive system. Auton Neurosci. 2010;157(1–2):46–51. doi: 10.1016/j.autneu.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 42.Lim CED, Wong WSF. Current evidence of acupuncture on polycystic ovarian syndrome. Gynecological Endocrinology. 2010;26(6):473–478. doi: 10.3109/09513591003686304. [DOI] [PubMed] [Google Scholar]
- 43.Stener-Victorin E, Jedel E, Mannerås L. Acupuncture in polycystic ovary syndrome: Current experimental and clinical evidence. Journal of Neuroendocrinology. 2008;20(3):290–298. doi: 10.1111/j.1365-2826.2007.01634.x. [DOI] [PubMed] [Google Scholar]
- 44.Liu ZC, Sun FM, Zhu MH, Wang XZ. Effect of acupuncture on insulin resistance in non-insulin dependent diabetes mellitus. Journal of Acupuncture and Tuina Science. 2004;2(6):8–11. [Google Scholar]
- 45.Pastore LM, Williams CD, Jenkins J, Patrie JT. True and sham acupuncture produced similar frequency of ovulation and improved LH to FSH ratios in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011;96(10):3143–3150. doi: 10.1210/jc.2011-1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raja-Khan N, Stener-Victorin E, Wu X, Legro RS. The physiological basis of complementary and alternative medicines for polycystic ovary syndrome. Am J Physiol Endocrinol Metab. 2011;301(1):E1–E10. doi: 10.1152/ajpendo.00667.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Feng Y, Stener-Victorin E, Chen B. Acupuncture in polycystic ovary syndrome: potential and challenge. In: Xia Y, Ding G, Wu GC, editors. Current Research in Acupuncture. New York, NY: Springer; 2013. pp. 487–515. [Google Scholar]
- 48.Li MY, Wei DY, Wu JM. Analysis on the interrelation between acupuncture-induced weight reduction and menstruation. Zhen Ci Yan Jiu. 2007;32(2):142–144. Chinese. [PubMed] [Google Scholar]
- 49.Shi Y, Feng HJ, Liu HR, Zhu D. Observation on therapeutic effect of acupuncture combined with Chinese herbs on polycystic ovary syndrome of kidney deficiency and phlegm stasis type. Zhongguo Zhen Jiu. 2009;29(2):99–102. Chinese. [PubMed] [Google Scholar]
- 50.Cai C. Acupuncture and moxibustion treatment of amenorrhea. Medical Acupuncture. 2013;25(3):205–208. [Google Scholar]
- 51.Yu J. Induction of ovulation with acupuncture; Poster presented at: NIH Consensus Development Conference on Acupuncture; November 3–5, 1997; Bethesda, MD: National Institutes of Health; Nov 3–5, 1997. [Google Scholar]
- 52.Yu J. Handbook of Obstetrics and Gynecology in Chinese Medicine: An Integrated Approach. Seattle, WA: Eastland Press; 1998. [Google Scholar]
- 53.Azziz R, Carmina E, Dewailly D, et al. The androgen excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 2009;91:456–488. doi: 10.1016/j.fertnstert.2008.06.035. [DOI] [PubMed] [Google Scholar]
- 54.Mo X, Li D, Pu Y, Xi G, Le X, Fu Z. Clinical studies on the mechanism for acupuncture stimulation of ovulation. Journal of Traditional Chinese Medicine. 1993;13(2):115–119. [PubMed] [Google Scholar]
- 55.Mo XM. Clinical study of the mechanism of inducing ovulation with acupuncture. Shanghai Acupuncture and Moxibustion Journal. 1990;3:8–9. Chinese. [Google Scholar]
- 56.Stener-Victorin E, Waldenström U, et al. Effects of electro-acupuncture on anovulation in women with polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2000;79(3):180–188. [PubMed] [Google Scholar]
- 57.Johansson J, Redman L, Veldhuis PP, et al. Acupuncture for ovulation induction in polycystic ovary syndrome: a randomized controlled trial. Am J Physiol Endocrinol Metab. 2013;304(9):E934–E943. doi: 10.1152/ajpendo.00039.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Smith CA, Zhu X, He L, Song J. Acupuncture for primary dysmenorrhoea. Cochrane Database Syst Rev. 2011;(1):CD007854. doi: 10.1002/14651858.CD007854.pub2. [DOI] [PubMed] [Google Scholar]
- 59.Smith CA, Zhu X, He L, Song J. Acupuncture for dysmenorrhoea. Cochrane Collaboration. 2012;(2) [Google Scholar]
- 60.Kim E, Cho JH, Jung WS, Lee S, Pak SC. Effect of acupuncture on heart rate variability in primary dysmenorrheic women. Am J Chin Med. 2011;39(2):243–249. doi: 10.1142/S0192415X11008786. [DOI] [PubMed] [Google Scholar]
- 61.Li YM, Bu YQ, Hou WJ, Chen SZ, Gao SZ. Observation on immediate analgesic effect of acupuncture at Shiqizhui (EX-B 8) only or multi-acupoints in patients with dysmenorrhea: a randomized controlled trial. Zhongguo Zhen Jiu. 2011;31(3):199–202. Chinese. [PubMed] [Google Scholar]
- 62.Ma YX, Ye XN, Liu CZ, et al. A clinical trial of acupuncture about time-varying treatment and points selection in primary dysmenorrhea. J Ethnopharmacol. 2013;148(2):498–504. doi: 10.1016/j.jep.2013.04.045. [DOI] [PubMed] [Google Scholar]
- 63.Yu YP, Ma LX, Ma YX, et al. Immediate effect of acupuncture at Sanyinjiao (SP6) and Xuanzhong (GB39) on uterine arterial blood flow in primary dysmenorrhea. J Altern Complement Med. 2010;16(10):1073–1078. doi: 10.1089/acm.2009.0326. [DOI] [PubMed] [Google Scholar]
- 64.Kashefi F, Ziyadlou S, Khajehei M, Ashraf AR, Fadaee AR, Jafari P. Effect of acupressure at the Sanyinjiao point on primary dysmenorrhea: a randomized controlled trial. Complement Ther Clin Pract. 2010;16(4):198–202. doi: 10.1016/j.ctcp.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 65.Bu YQ. Observation on therapeutic effect of acupuncture at Shiqizhui (Extra) for primary dysmenorrhea at different time. Zhongguo Zhen Jiu. 2011;31(2):110–112. Chinese. [PubMed] [Google Scholar]
- 66.Bu YQ, Du GZ, Chen SZ. Clinical study on the treatment of primary dysmenorrhea with preconditioning acupuncture. Chin J Integr Med. 2011;17(3):224–227. doi: 10.1007/s11655-011-0671-9. [DOI] [PubMed] [Google Scholar]
- 67.Yang H, Liu CZ, Chen X, et al. Systematic review of clinical trials of acupuncture-related therapies for primary dysmenorrhea. Acta Obstet Gynecol Scand. 2008;87(11):1114–1122. doi: 10.1080/00016340802443798. [DOI] [PubMed] [Google Scholar]
- 68.Cho SH, Hwang EW. Acupuncture for primary dysmenorrhoea: a systematic review. BJOG. 2010;117(5):509–521. doi: 10.1111/j.1471-0528.2010.02489.x. [DOI] [PubMed] [Google Scholar]
- 69.Cho SH, Kim J. Efficacy of acupuncture in management of premenstrual syndrome: a systematic review. Complement Ther Med. 2010;18(2):104–111. doi: 10.1016/j.ctim.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 70.Kim SY, Park HJ, Lee H, Lee H. Acupuncture for premenstrual syndrome: a systematic review and meta-analysis of randomised controlled trials. BJOG. 2011;118(8):899–915. doi: 10.1111/j.1471-0528.2011.02994.x. [DOI] [PubMed] [Google Scholar]
- 71.Guo ZR, Ma LX. Acupuncture treatment for premenstrual syndrome. Medical Acupuncture. 2013;25(3):200–204. [Google Scholar]
- 72.Liu LG, Gu J, Yang YH. Analysis of acupuncture treatment characteristics of infertility in ancient times. Literature Journal of TCM. 2005;1:14–16. [Google Scholar]
- 73.Dean KL. Acupuncture in fertility medicine: three integrative methodologies. Alternative and Complementary Therapies. 2004;10(6):316–320. [Google Scholar]
- 74.Birkeflet O, Laake P, Vøllestad N. Low inter-rater reliability in traditional Chinese medicine for female infertility. Acupunct Med. 2011;29(1):51–57. doi: 10.1136/aim.2010.003186. [DOI] [PubMed] [Google Scholar]
- 75.Zheng CH, Huang GY, Zhang MM, Wang W. Effects of acupuncture on pregnancy rates in women undergoing in vitro fertilization: a systematic review and meta-analysis. Fertility and Sterility. 2012;97(3):599–611. doi: 10.1016/j.fertnstert.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 76.Manheimer E, van derWindt Dl, Cheng K, et al. The effects of acupuncture on rates of clinical pregnancy among women undergoing in vitro fertilization: a systematic review and meta-analysis. Hum Reprod Update. 2013;19(6):696–713. doi: 10.1093/humupd/dmt026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kang HS, Jeong D, Kim DI, Lee MS. The use of acupuncture for managing gynaecologic conditions: An overview of systematic reviews. Maturitas. 2011;68(4):346–354. doi: 10.1016/j.maturitas.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 78.El-Toukhy T, Sunkara SK, Khairy M, Dyer R, Khalaf Y, Coomarasamy A. A systematic review and meta-analysis of acupuncture in in vitro fertilisation. BJOG. 2008;115(10):1203–1213. doi: 10.1111/j.1471-0528.2008.01838.x. [DOI] [PubMed] [Google Scholar]
- 79.Manheimer E, Zhang G, Udoff L, et al. Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: systematic review and meta-analysis. BMJ. 2008;336(7643):545–549. doi: 10.1136/bmj.39471.430451.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cheong YC, Hung YU, Ng E, Ledger WL. Acupuncture and assisted conception. Cochrane Database Syst Rev. 2008;(4):CD006920. doi: 10.1002/14651858.CD006920.pub2. [DOI] [PubMed] [Google Scholar]
- 81.Domar AD, Meshay I, Kelliher J, Alper M, Powers RD. The impact of acupuncture on in vitro fertilization outcome. Fertil Steril. 2009;91(3):723–726. doi: 10.1016/j.fertnstert.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 82.Moy I, Milad MP, Barnes R, Confino E, Kazer RR, Zhang X. Randomized controlled trial: effects of acupuncture on pregnancy rates in women undergoing in vitro fertilization. Fertil Steril. 2011;95(2):583–587. doi: 10.1016/j.fertnstert.2010.05.024. [DOI] [PubMed] [Google Scholar]
- 83.So EW, Ng EH, Wong YY, Lau EY, Yeung WS, Ho PC. A randomized double blind comparison of real and placebo acupuncture in IVF treatment. Hum Reprod. 2009;24(2):341–348. doi: 10.1093/humrep/den380. [DOI] [PubMed] [Google Scholar]
- 84.Andersen D, Løssl K, Nyboe Andersen A, et al. Acupuncture on the day of embryo transfer: a randomized controlled trial of 635 patients. Reprod Biomed Online. 2010;21(3):366–372. doi: 10.1016/j.rbmo.2010.03.029. [DOI] [PubMed] [Google Scholar]
- 85.Drake M. The Effects of Acupuncture on In Vitro Fertilization Outcomes: A Systematic Review of the Literature and an Update to the Cochrane Collaboration Review. Phoenix, AZ: College of Medicine, The University of Arizona; 2011. [Google Scholar]
- 86.Anderson B, Rosenthal L. Acupuncture and in vitro fertilization: critique of the evidence and application to clinical practice. Complement Ther Clin Pract. 2013;19(1):1–5. doi: 10.1016/j.ctcp.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 87.Shi Z, Ma L, Yang Y, et al. Acupuncture: when classical meets modern. Fertil Steril. 2011;95(7):e33. doi: 10.1016/j.fertnstert.2011.03.039. author reply e34. [DOI] [PubMed] [Google Scholar]
- 88.Ng EH, So WS, Gao J, Wong YY, Ho PC. The role of acupuncture in the management of subfertility. Fertil Steril. 2008;90(1):1–13. doi: 10.1016/j.fertnstert.2008.02.094. [DOI] [PubMed] [Google Scholar]
- 89.Huang ST, Chen AP. Traditional Chinese medicine and infertility. Curr Opin Obstet Gynecol. 2008;20(3):211–215. doi: 10.1097/GCO.0b013e3282f88e22. [DOI] [PubMed] [Google Scholar]
- 90.Craig LB, Criniti AR, Hansen KR, Marshall LA, Soules MR. Acupuncture lowers pregnancy rates when performed before and after embryo transfer. Fertil Steril. 2007;88(Suppl 1):S40. [Google Scholar]
- 91.Johnson D. Acupuncture prior to and at embryo transfer in an assisted conception unit – a case series. Acupunct Med. 2006;24(1):23–28. doi: 10.1136/aim.24.1.23. [DOI] [PubMed] [Google Scholar]
- 92.Emmons S, Patton P. Acupuncture treatment for infertile women undergoing intracytoplasmic sperm injection. Medical Acupuncture. 2000;12(2):18–20. [Google Scholar]
- 93.Rubin LH, Opsahl M, Ackerman D. P02.15 Acupuncture improves in vitro fertilization live birth outcomes: a retrospective chart review. Scientific Abstracts Presented at the International Research Congress on Integrative Medicine and Health 2012. 2012;12(Suppl 1):P71. [Google Scholar]
- 94.Smith C, Coyle M, Norman RJ. Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer. Fertility & Sterility. 2006;85(5):1352–1358. doi: 10.1016/j.fertnstert.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 95.Rosenthal L, Anderson B. Acupuncture and in vitro fertilisation: recent research and clinical guidelines. Journal of Chinese Medicine. 2007;84:28–35. [Google Scholar]
- 96.Boivin J, Schmidt L. Use of complementary and alternative medicines associated with a 30% lower ongoing pregnancy/live birth rate during 12 months of fertility treatment. Hum Reprod. 2009;24(7):1626–1631. doi: 10.1093/humrep/dep077. [DOI] [PubMed] [Google Scholar]
- 97.Clark NA, Will M, Moravek MB, Fisseha S. A systematic review of the evidence for complementary and alternative medicine in infertility. Int J Gynaecol Obstet. 2013;122(3):202–206. doi: 10.1016/j.ijgo.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 98.de Lacey S, Smith CA, Paterson C. Building resilience: a preliminary exploration of women’s perceptions of the use of acupuncture as an adjunct to In Vitro Fertilisation. BMC Complement Altern Med. 2009;9:50. doi: 10.1186/1472-6882-9-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Balk J, Catov J, Horn B, Gecsi K, Wakim A. The relationship between perceived stress, acupuncture, and pregnancy rates among IVF patients: a pilot study. Complement Ther Clin Pract. 2010;16(3):154–157. doi: 10.1016/j.ctcp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.de Lacey S, Smith C. Acupuncture and infertility treatment: is there more to the outcome for women than pregnancy? Medical Acupuncture. 2013;25(3):195–199. [Google Scholar]
- 101.Cochrane S, Smith CA, Possamai-Inesedy A. Development of a fertility acupuncture protocol: defining an acupuncture treatment protocol to support and treat women experiencing conception delays. J Altern Complement Med. 2011;17(4):329–337. doi: 10.1089/acm.2010.0190. [DOI] [PubMed] [Google Scholar]
- 102.Liang L. Acupuncture and IVF. Boulder, CO: Blue Poppy Press; 2003. [Google Scholar]
- 103.Chen ZQ, Li LY. The Clinical Practice of Chinese Medicine Male and Female Fertility. Beijing, People’s Republic of China: People’s Medical Publishing House; 2008. [Google Scholar]
- 104.Ding HJ. 31 cases of infertility due to salpingemphraxis treated by acupuncture and moxibustion. Journal of Clinical Acupuncture and Moxibustion. 1998;14(10):30. Chinese. [Google Scholar]
- 105.Paulus WE, Zhang M, Strehler E, El-Danasouri I, Sterzik K. Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproduction therapy. Fertil Steril. 2002;77(4):721–724. doi: 10.1016/s0015-0282(01)03273-3. [DOI] [PubMed] [Google Scholar]
- 106.Huang DM, Huang GY, Lu FE, Stefan D, Andreas N, Robert G. Acupuncture for infertility: is it an effective therapy? Chin J Integr Med. 2011;17(5):386–395. doi: 10.1007/s11655-011-0611-8. [DOI] [PubMed] [Google Scholar]