Abstract
Purpose
Activation of Toll like receptors (TLRs) signaling has been implicated in promoting malignant cell invasion and metastatic potential. Previously we demonstrated that increased TLR-9 expression predicted poor survival in oral cancer patients. The objective of this study is to further investigate the roles and potential molecular mechanisms of TLR-9 signaling in human oral cancer cell invasion.
Methods
Cell migration, invasion and protein expression were detected by wound healing assay, Transwell chambers model and western blot. The secretion and activity levels of metalloproteinases-2/9 were quantified by ELISA and Gelatin zymography. EMSA and ChIP assays were employed to detect the activity of AP-1signal pathway. TLR-9 siRNA transfection was used to regulate the expression and activity of TLR-9 in oral cancer cell line HB cells.
Result
The results of both wound healing assay and in vitro Transwell assay revealed that activation of TLR-9 induced dose- and time- dependent migration and invasion of HB cells. An increased expression, secretion and activity of MMP-2 were observed upon the treatment of CpG-ODN. The TLR-9 signaling-mediated MMP-2 expression appeared to be a consequence of AP-1 activation, because that their DNA binding activity was enhanced by CpG-ODN treatment. All these influences were efficiently repressed by the knockdown of TLR-9 through siRNA or pretreatment of an AP-1 inhibitor.
Conclusion
Activation of TLR-9 signaling could promote human oral cancer HB cells invasion with the induction of MMP-2 presentation by attenuating AP-1 binding activity, suggesting a novel anti-metastatic application for TLR-9 targeted therapy in oral cancer in the future.
Introduction
Oral Squamous Cell Carcinoma (OSCC) is the most common malignancy in the head and neck region, presenting approximately 389,000 new cases yearly [1], [2]. Although treatment methods such as chemotherapy, radiotherapy, and surgical therapy have advanced in recent years, the 5-year survival rate of patients with OSCC has remained less than 60% [3]. Local invasion, widespread lymphatic, and distal metastases are the most prevalent causes of death in these patients [4]. This highlights the urgent need for a better understanding of the mechanisms of metastasis in oral squamous cell carcinoma.
Toll-like receptors (TLRs) are members of the interleukin-1 receptor superfamily and play a crucial role in the activation of innate immunity and the subsequent inflammatory process [5], [6]. However, increasing evidence indicates that TLRs signaling pathway was not only involved in human immune response but also play an important role in tumor cell initiation and migration [7], [8]. For example, TLR-2 and TLR-9 signaling were found to promote tumor cell migration in breast cancer[9], [10], TLR-4 and TLR-9 signaling were demonstrated to accelerate cell invasion in prostate cancer[11], [12], and activation of TLR-2 and TLR-4 signaling were also shown to stimulate tumor cell movement in colon cancer[13], [14]. These findings suggest that investigation of the relationship between TLRs signaling and tumor invasion may shed new light for effective prevention of cancer metastatic spread.
To date, there are 12 members of the TLR family that have been identified in mammals. As the only TLR that located intracellularly, TLR-9 could recognize the special DNA sequence of a bacteria or virus via cell pinocytosis [15]. Our prior work found that TLR-9 protein was abnormally high expressed in oral cancer tissue and cell lines, and TLR-9 activation could stimulate tumor cell proliferation through increased Cyclin D1 expression [16], [17]. However, little is known about the effect of TLR-9 signaling on oral cancer cell invasion as well as the possible underlying molecular mechanisms.
The purpose of this study is to investigate the influence of TLR-9 signaling on in-vitro invasiveness of HB cells, a human oral cancer cell line; with special emphasis on synthesis and secretion of MMP-2 and MMP-9. Possible molecular mechanisms underlying TLR-9-mediated tumor cell invasion were also investigated, including two pathways related to inflammation: NF-κB and AP-1 pathway.
Materials and Methods
Ethics Statement
This study was approved by the Ethics Committee of Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine and carried out according to the recommendations of the Declaration of Helsinki. No informed consent (written or verbal) was obtained for use of retrospective tissue samples from the patients within this study, some of whom were deceased, since the Ethics Committee, who waived the need for consent, did not deem this necessary. All samples were anonymous.
Materials
Unmethylated phosphorothioate modified, human specific CpG-ODN 2006 (5′-TCGTCGTTTTGTCGTTTTGTCGTT-3′) and respective GpC-ODN negative controls were purchased from InVivoGen (San Diego, CA). They were dissolved into endotoxin-free sterile distilled deionized H2O according to the manufacturer's suggestion and used at the indicated concentrations. The anti-TLR-9 antibody was purchased from Imgenex (CA, USA). AP-1 specific inhibitor curcumin and selective MMP-2 inhibitor ARP101 were obtained from Calbiochem (San Diego, CA, USA).
Cell culture
A human oral squamous cell carcinoma cell line, HB cell, as previous described was used [18]. Cells were cultured in the DMEM (Dulbecco's modified Eagle's medium, Gibco, USA) supplemented with 10% fetal bovine serum, 1% glutamine, and 1% penicillin–streptomycin and cultured in a humidified atmosphere of 5% CO2 at 37°C.
Cell migration assay (Scratch wound healing assay)
Cells were treated with CpG-ODN (0.8 μM) after creating a wound across the cell monolayer with a plastic tip. Cell migration into the wound surface was then measured after 24 h using ProgRes Capture Pro v2.8.0 software and reported as the width of the remaining relative to the initial wound area (in micrometers).
Transwell invasion assays
The invasion of tumor cells was assessed in Transwell chambers with a 6.5-mm-diameter polyvinyl/pyrrolidone–free polycarbonate filter of 8-μm pore size. Each filter was coated with 100 μL of a 1∶20 diluted matrigel in cold DMEM to form a thin continuous film on the top of the filter. The number of cells was adjusted to 5×108/L and a 100 μL aliquot containing 5×104cells was added to each of the triplicate wells in DMEM containing 10% FBS. After incubation for 24∼48 h, cells were stained and counted as described above, and the number of cells invading the lower side of the filter was measured for invasive activity.
Cytoselect Cell invasion assays
To further investigate if CpG-ODN hold the character to promote HB cell invasion, the CytoSelect 96-well Cell Invasion Assay Kit, which provides a robust system for the quantitative determination of cell invasion, were used according to the manufacturer's recommendations (Cell Biolabs, San Diego, CA, USA). Briefly, HB cells were pretreated with CpG-ODN at different concentration for 24 h. Basement membranes of Boyden chambers were rehydrated with 300 μl serum-free RPMI, and 2.5×106 cells were then seeded into the upper area of the chamber in serum-free RPMI. Bottom wells were filled with RPMI supplemented with 10% FBS containing CpG-ODN or no CpG-ODN. After 48 h incubation (37°C, 5% CO2), noninvasive cells were removed from the upper chamber and cell invasion was assessed by colorimetric analysis. For colorimetric quantification of invasion, inserts were then placed in extraction buffer (200 μl, 10 min), and absorbance at 560 nm was determined after transfer to a 96-well plate (100 μl per well) using a VersaMax microtiter plate reader (Molecular Devices, Sunnyvale, CA, USA)
Westernblot analysis
The procedure was performed as previously used [19]. The following antibodies(Santa Cruz, USA) were used: anti-MMP-2 antibody (dilution 1∶150), anti-MMP-9 antibody (dilution 1∶200), anti-p50 antibody (dilution 1∶200), anti-p65 antibody (dilution 1∶200), anti-IκBα antibody(dilution 1∶300), anti-phospho-IκBα antibody(dilution 1∶200), anti-c-jun antibody (dilution 1∶200)), anti-jun-B antibody (dilution 1∶150), anti-jun-D antibody (dilution 1∶200), anti-c-Fos antibody (dilution 1∶200), anti-Fos-B antibody (dilution 1∶250).β-actin was used as internal control protein. Experiments were repeated at least three times.
ELISA analysis
MMP-2 and-9 secretions were measured using a fluorometric analysis kit according to the manufacturer's recommendations (Chemicon, Temecula, CA, USA). Briefly, the detached and attached cells were collected, washed with PBS, and lysed in 200 μL of ice-cold cell lysis buffer provided by the manufacturers. The cell extracts were centrifuged, and supernatants were collected. Equal amounts of cell protein extracts (300 μg) were incubated in reaction buffer containing MMP-2 substrate or MMP-9 substrate at 37°C for 2 to 3 hrs. The samples were analyzed with a plate reader by the measurement of optical density (OD) at a wavelength of 405 nm. Each experiment was conducted three times.
Gelatin zymography
Protein concentrations in conditioned media were determined using the bicinchoninic acid method (BCA kit) (Pierce, IL, USA). Conditioned media was mixed with an equal volume of 4× sample buffer (200 mM Tris-HCl, 8% SDS, 0.4% bromophenol blue, 40% glycerol), and electrophoresed on 8% SDS polyacrylamide gels containing 2 mg/ml of gelatin (Sigma, St. Louis, MO, USA). Gels were then washed twice for 30 min in 2.5% Triton X-100 at room temperature, and incubated for 18 hours at 37°C in incubation buffer (50 mM Tris-HCl (pH 7.5), 5 mM CaCl2, and 200 mM NaCl). Gels were then stained for 1 hour with 0.25% (w/v) Coomassie brilliant blue R-250 (Bio-Rad) and then destained in destaining buffer (10% acetic acid and 20% methanol).
Nuclear extract and electrophoretic mobility shift assay (EMSA)
HB Cells were treated with 0.8 μM CpG-ODN at indicated period time (0∼24 h), and nuclear extracts were prepared as described previously [20]. Synthetic complementary oligonucleotides were 3′-biotinylated using the biotin 3′-end DNA labeling kit (Pierce, Rockford, Illinois, USA), according to the manufacturer's instructions, and annealed for 2 h at room temperature. The sequences of the oligonucleotides used are 5′-CGCTTGATGAGTCAGCCGGAA-3′ for AP-1. Binding reactions were carried out for 20 min at room temperature in the presence of 50 ng/μL poly(dI-dC), 0.05% Nonidet P-40, 5 mM MgCl2, 10 mM EDTA and 2.5% glycerol in 1×binding buffer (LightShiftTM chemiluminescent EMSA kit, Pierce) using 20 μmol of biotin-end-labeled target DNA and 5 μg of nuclear extract. Unlabeled target DNA (4 pmol) or 2 μL of anti-CREB or anti-ATF-1 antibody (TransCRUZ, Santa Cruz Biotechnology, Inc.) was added per 20 μL of binding reaction where indicated. Assays were loaded onto native 4% polyacrylamide gels pre-electrophoresed for 60 min in 0.5×Tris borate/EDTA and electrophoresed at 100 V before being transferred onto a positively charged nylon membrane (HybondTM-N+) in 0.5×Tris borate/EDTA at 100 V for 30 min. Transferred DNAs were cross-linked to the membrane at 120 mJ/cm2 and detected using horseradish peroxidase-conjugated streptavidin (LightShiftTM chemiluminescent EMSA kit) according to the manufacturer's instructions. Specific binding was controlled by competition with a 100-fold excess of non-labeled AP-1 oligonucleotide probes.
Chromatin immunoprecipitation (ChIP) assays
Chromatin immunoprecipitation (ChIP) assays and subsequent real-time PCR analysis was performed as described [21]. Briefly, cells were washed twice with PBS and cross-linked with 1% formaldehyde at room temperature for 10 minutes. Cells were rinsed with ice-cold PBS twice and resuspended into 100 mmol/L of Tris-HCl (pH 9.4), 10 mmol/L of DTT and incubated for 15 minutes at 30°C. Cells were washed and resuspended in lysis buffer (1% SDS, 10 mmol/L of EDTA, 50 mmol/L of Tris-HCl, pH 8.1, 1× protease inhibitor cocktail (Roche) and sonicated 3 times for 10 seconds each pulse at the maximum setting (Fisher Sonic Dismembrator, Model 300), followed by centrifugation for 10 minutes. Immunoprecipitations were performed overnight at 4°C with anti-c-Fos, anti-JunD, anti-p50 or anti-p65 (Santa cruz, USA). Precipitates were washed and heated at 65°C to reverse cross-linking and DNA fragments purified using QIAquick Spin Kit (Qiagen) for subsequent PCR. The PCR primers specific to the AP-1 binding region of the human MMP-2 promoter were: 5′-ATCTCTGGGCCATTGTCA-3′ (sense) and 5′-TGTGACAACGTCTCTCA-3′ (antisense).
Small interfering RNA preparation and transfection
Chemically synthesized human TLR-9-specific siRNAs (sense CUGUCCUUCAAUUACCAAAtt; antisense GUAAUUGAAGGACAGgt) and the control non-silencing siRNA (sense UUCUCCGAACGUGUCACGUtt, antisense ACGUGACACGUUCGGAGAA) were purchased from MWG (Ebersberg, Germany). For siRNA transfection, 3×105 HB cells/well were plated in 6-well plates and transfected by using Amaxa Nucleofector (Amaxa, Köln, Germany) according to the manufacturer's protocol (Nucleofector Solution V, Nucleofector program G-16) with 2 μg siRNA per 106 cells. After 48 hr of transfection, TLR-9 expression was tested by Western blot and further experiments were carried out.
Statistical analysis
Data were presented as means±standard deviation from at least three independent experiments. Differences between experimental groups were assessed by non-parametric analysis using SPSS software, version 12 (SPSS, Chicago). Statistical significance was defined as P<0.05 for all tests.
Results
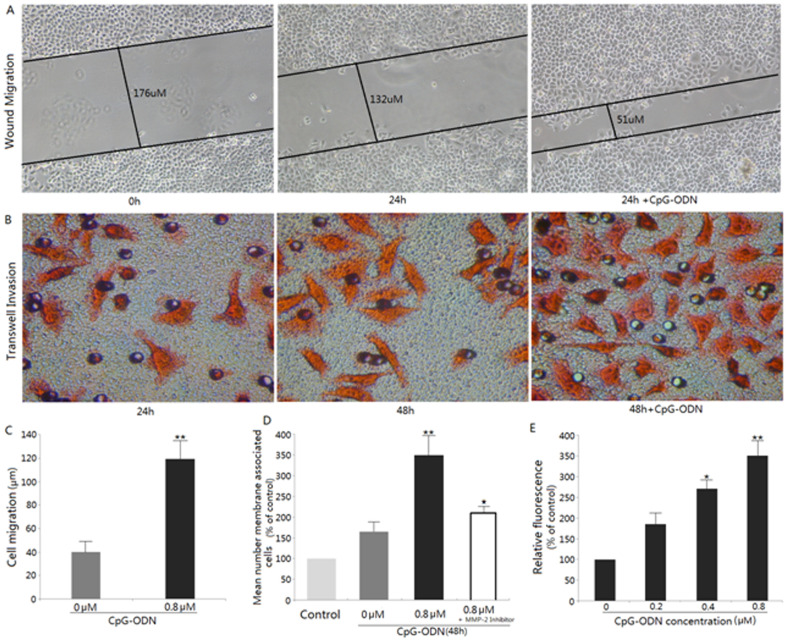
CpG-ODN promotes migration in HB cells
We first examined the effect of CpG-ODN on the migratory and invasive ability of HB cells in vitro. Scratch wound migration assay shown 0.8 μM CpG-ODN effectively promoted the migration of HB cells into the wounded area in 24 h, which was determined as movement of cells (in μm) into the wound (Fig. 1A and C). The Transwell results showed that the number of cells that invaded the lower chamber was significantly increased 48 h after treatment by 0.8 μM CpG-ODN (Fig. 1B and D). A similarly result was also achieved when CytoSelect 96-well Cell Invasion Assay, which provides a robust system for the quantitative determination of cell invasion, was used to further certificate the stimulate-invasion effect of CpG-ODN(0.2∼0.8 μM) on HB cells by a concentration-dependent manner(Fig. 1E).
Figure 1. Analysis of migration and invasion of CpG-ODN treated HB cells.
(A) Evaluation of cell migration by scratch wound healing assay: Cells were allowed to migrate with and without 0.8 μM CpG-ODN. Cell migration into the wound surface was then monitored by microscopy after 24 h of the CpG-ODN treatment and reported as the width of remaining wounded area relative to the initial wound area. (B)Evaluation of cell invasion by transwell assay. Representative photomicrographs of the membrane-associated cells (jacinth part) were assayed by Eosin staining (×400). (C)Graphical representation of scratch wound assay. The average distance of cell invasion was significantly greater in the CpG-ODN treated sample. **P<0.01. (D)Semi-quantitative analysis of the stimulate-invasion effects of CpG-ODN on HB cells. “% of control” denotes the mean number of the cells expressed as a proportion of the control group and the average of three independent experiments ± S.D. **p<0.01, compared with the lane 2; ★p<0.05, compared with the lane 3. (E)Colorimetric analysis of CpG-ODN modulation of HB cell invasiveness with different concentrations (0∼0.8 μM) for 48 h by the CytoSelect cell invasion assay. *p<0.05; **p<0.01, compared with lane 1. The 48h+CpG-ODN panel of Figure 1B is excluded from this article's CC-BY license. See the accompanying retraction notice for more information.
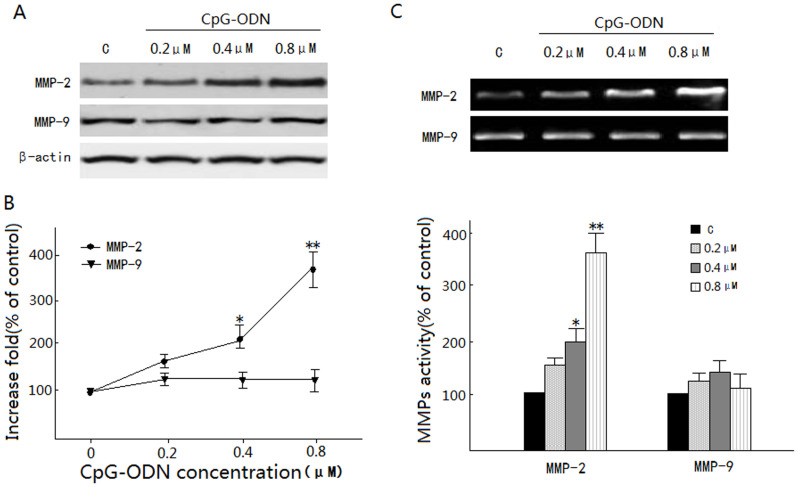
CpG-ODN up-regulated the MMP-2 activity in HB cells
Since MMP-2 and MMP-9 play a critical role in tumor cell invasion, we examined the effect of CpG-ODN on MMP-2 and MMP-9 expression by Western Blot. As shown in Fig 2A, CpG-ODN tremendously increased MMP-2 expression in a concentration-dependent manner, whereas MMP-9 expression was not affected. To further elucidate the up-regulatory effects of CpG-ODN on MMP-2 and-9, ELISA analysis and Gelatin zymography test were performed to evaluate MMP-2 and-9 secretion and activity respectively. It was revealed that the treatment of 0.8 μM CpG-ODN for 24 h significantly increased the secretion level of MMP-2 as well as its in vitro activity compared with control, while no significant increase was shown in MMP-9 (Fig 2B and 2C).
Figure 2. Effects of CpG-ODN on MMP-2 and MMP-9 expressions.
(A) Analysis of MMP-2 and -9 protein expression in cells treated with indicated doses of CpG-ODN and harvested at 24 h. β-actin served as an internal control. (B) Determined secretion of MMP-2 and -9 was subsequently quantified by ELISA analysis, and presented as means ± S.D. of three repeats from one independent study. (C) HB cells in serum-free medium were treated with various concentrations (0∼0.8 μM) of CpG-ODN for 24 h. The culture medium of cells after treatment was subjected to gelatin zymography to analyze the activity of MMP-2 and -9; *p<0.05; **p<0.01, compared with the control.
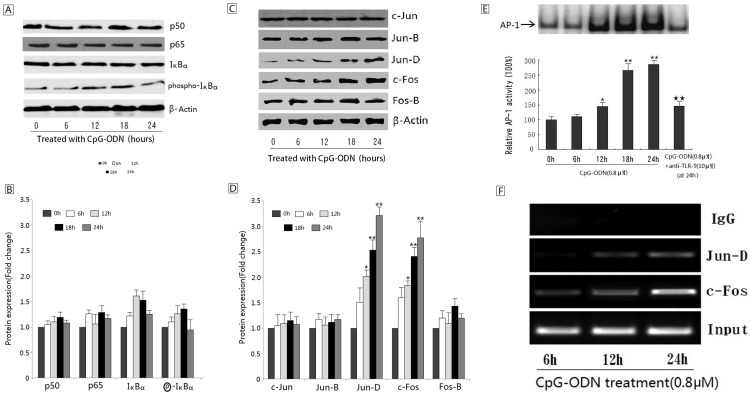
AP-1 activation is involved in CpG ODN-mediated MMP-2 induction
Since NF- κB and AP-1 are two of the well known transcriptional factors which regulate MMP-2 expression, we first employed the NF-κB and AP-1 Westernblot assay. Results showed that treatment with CpG-ODN led to an elevated expression of c-Fos and Jun-D, indicating an increased AP-1 activity in CpG-ODN-treated HB cells (Figure 3C, D). However, no significant change was found in p50, p65, IκBα or phosphor-IκBα expression, which means that activation of TLR-9 signaling, did not significantly influence the NF-κB activity (Figure 3A, B). Next, we detected AP-1 activity by EMSA analysis. As shown in Figure 3E, almost 3 fold-increased AP-1 activities were observed 24 h after 0.8 μM CpG ODN treatment. Further ChIP analysis also demonstrated that CpG-ODN treatment enhanced the DNA-binding activity of AP-1(c-Fos/Jun-D) to the promoter of MMP-2 in a time dependent manner (Figure 3F). Finally, curcumin, an AP-1 inhibitor, was found to significantly block CpG-ODN-induced MMP-2 expression, indicating that AP-1 activation is required for the TLR-9 activated MMP-2 expression in HB cells (Figure 4B).
Figure 3. Effect of CpG-ODN on NF- κB and AP-1 activity.
(A) Effects of CpG-ODN on the expression of NF- κB subunit. HB cells were treated with 0.8 μM CpG-ODN at indicated time period (0∼24 h) and the protein levels were determined using Western blot. β-actin was used as an internal control. (B) Changes in NF- κB subunit protein levels compared with the control as determined by densitometric scanning of the immunoreactive bands. (C) Effects of CpG-ODN on the expression of AP-1 subunit. (D) Changes in AP-1 subunit protein levels compared with control as determined by densitometric scanning of the immunoreactive bands. (*P<0.05; **P<0.01, compare with the control) (E) Electrophoretic mobility shift analysis (EMSA) analysis of AP-1 in HB cell lines before and after treatment with 0.8 μM CpG-ODN at indicated time period (0∼24 h). (*P<0.05; **P<0.01, compared with the panel 1), (★★P<0.01, compared with the panel 5). (F) CpG-ODN treatment enhances the DNA-binding activity of AP-1(c-Fos/Jun-D) to the promoter of MMP-2 in a time-dependent manner. Figures 3A, C, E, and F are excluded from this article's CC-BY license. See the accompanying retraction notice for more information.
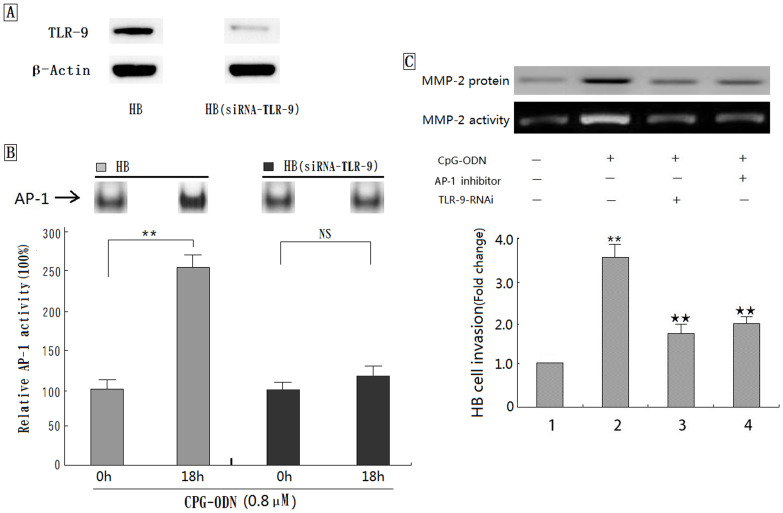
Figure 4. Role of MMP-2 in TLR-9/AP-1 mediated cancer cell invasion.
(A) Expression of TLR-9 protein in HB cells before and after 48 hr of transfection. β-actin was used as an internal control. (B) CpG-ODN treatment does not enhance AP-1 activity in HB cells transfected with special siRNA against TLR-9. (**P<0.01, NS: no significant) (C) The interferon effect of AP-1 inhibitor and/or TLR-9-RNAi on the CpG-ODN induced MMP-2 expression/activity as well as subsequent cancer cell invasion. (**P<0.01, compared with the panel 1), (★★P<0.01, compared with the panel 2). Figure 4B is excluded from this article's CC-BY license. See the accompanying retraction notice for more information.
TLR-9/AP-1 pathway is involved in MMP-2 mediated HB cells invasion
To further confirm the role of TLR-9/AP-1 pathway in MMP-2 mediated HB cell invasion, both anti-TLR-9 protein and special siRNA against TLR-9 were used. Results showed that increased AP-1 activity in CpG-ODN treated HB cells was significantly decreased by utilization of anti-TLR-9 protein or specific siRNA against TLR-9 (Figure 3E, 4A, 4B). In addition, blockade of TLR-9 with RNA interference could significantly decreased CpG-ODN-stimulated MMP-2 expression as well as HB cell invasion, indicating that AP-1 activation is required for the TLR-9 activated MMP-2 expression and subsequent cell invasion (Fig. 4C). Moreover, the increased MMP-2 expression and secretion by CpG-ODN and subsequent cell invasion were also significantly suppressed by treatment with curcumin (an AP-1 inhibitor), which further confirmed that TLR-9/AP-1 pathway was involved in CpG-ODN induced MMP-2 expression in HB cells (Figure 4C).
Discussion
Metastasis is a multi-step process that requires cancer cells to detach from the main tumor, to migrate, invade and grow at the secondary site [22]. Clinically, more than 90% of mortalities in tumor patients are caused by metastases [23], [24]. Therefore, identification of key signal pathway involved in the processes is vital for understanding this process and devising new therapies.
Growing evidence reveals that TLRs signaling regulate tumor invasion in variety of cancer cells, including breast cancer, prostate cancer and colorectal cancer [9]–[14]. Currently little is known about the effect of TLRs signaling in invasion and migration of oral cancer. In the present study, we examined our hypothesis that TLR-9 signaling may induce the invasiveness of oral cancer cells via up-regulating MMPs in HB cells. We showed that the invasiveness of oral cancer HB cells was strongly enhanced by incubated with the CpG-ODN, a special TLR-9 agonist, in a concentration (0.2∼0.8 μM)-dependent manner. By contrast, direct incubation of TLR-9 silenced HB cells with CpG-ODN did not affect the invasive property. These findings are consistent with previous reports, in which activation of TLR-9 signaling in breast cancer and prostate cancer were both demonstrated to enhance tumor cell migration in vitro[10], [12]. However, the underlying mechanisms, including the possible role matrix metalloproteinases (MMPs) plays in this process is unclear. To our knowledge, this is the first study that focuses on the molecular mechanisms of TLR-9-mediated cancer cell invasion.
It is well known that tumor invasion and metastasis require increased expressions of MMPs. Among the MMPs, MMP-2 and MMP-9 have been thought to be key enzymes in this process, because they degrade type IV collagen, which is one of the important components of extracellular matrix [25]. Both MMP-2 and MMP-9 have been demonstrated to play a central role in the process of invasion and metastasis of oral cancer. An immunohistochemical study of MMP-2 in 46 patients with OSCC found a high level of expression in 77% of patients with lymph node metastases, but only in 25% of patients without lymph node metastases[26].Another two immunostaining researches of MMPs also revealed a strong expression of MMP-2 and MMP-9 in OSCC patients with lymph node metastasis[27], [28]. Our present study demonstrates that TLR-9 activation slightly promotes MMP-9 activity in HB cells, whereas it strongly increases the expression of MMP-2 protein in a dose-dependent way. The elevated active MMP-2 enzyme in HB cells, which was clearly demonstrated by gelatin zymographic assay, was then released into the medium and, in turn, enhanced the invasiveness of HB cells. However, it cannot be excluded that HB cells may secrete some unknown factors that are involved in cell invasion. This is implicated by our results that pretreatment of HB cells with a high concentration of MMP-2 inhibitor ARP101 followed by incubation with CpG-ODN (0.8 μM) markedly, but did not completely, inhibit HB cell invasiveness.
We also have studied the possible mechanism underlying the enhancing effect of TLR-9 signaling on MMP-2 expression in HB cells. Several lines of evidence have demonstrated that the MMP-2 promoter contains binding sites for several transcription factors, including NF-κB and AP-1[29], [30]. As the most frequent involved inflammatory signal transduction pathway, both NF-κB and AP-1 was found to participate in the TLRs signaling pathway during cancer cell migration [31]. Therefore, the NF-κB and AP-1 signal transduction pathway may play an important role in the regulation of MMP-2 expression by TLR-9 activation. Previously it was reported that increased activity of NF-κB was associated with increased MMP-2 expression and in-vitro migration in human renal cancer cells [32]. However, our data showed that TLR-9 activation by CpG-ODN promotes DNA-binding activity of AP-1 but not that of NF-κB in HB cells. Utilization of anti-TLR-9 antibody could reduce the CpG-ODN stimulated MMP-2 expression as well as AP-1 DNA binding activity. Moreover, blockade of AP-1 activity with a special inhibitor significantly reduced CpG-ODN stimulated-TLR-9 mediated MMP-2 expression and subsequent cell migration. These results are consistent with recent report in that special stimulators can up-regulate MMP-2 secretion level through the activation of AP-1 signal transduction pathway in human lung cancer [33]. Although the regulatory mechanisms involved in MMP-2 have not been fully elucidated yet, both AP-1 and NF-κB were likely to play important roles depend on different cellular contexts [34], [35].
In summary, the present study provides evidence that TLR-9 signaling could directly promote cancer cell invasion via, at least in part, AP-1 activated MMP-2 secretion in HB cells. These interesting findings provide not only an important basis for a further exploration toward understanding the action mechanisms of TLR-9/AP-1/MMP-2 signaling-mediated cancer invasion, but also a promising target for the new therapeutic as well as preventive approaches of tumor metastasis in the future.
Acknowledgments
We thank Dr. Yanhua Ren for commenting on the manuscript, and we also thank Prof. Guoqing Zhang for statistics analysis.
Funding Statement
This study was supported by Project of National Natural Science Foundation of China (Grant No. 81102049) (URL: http://www.nsfc.gov.cn/Portal0/default152.htm); the Natural Science Foundation of Shanghai (Grant No. 11ZR1420600) to MR (URL: http://www.stcsm.gov.cn/); and Shanghai Leading Academic Discipline Project (Project Number: S30206) to CZ (URL: http://www.shec.edu.cn/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55: 74–108. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Shin HR, Bray F, Forman D, Mathers C. GLOBOCAN 2008, cancer incidence and mortality worldwide: IARC Cancer Base No. 10. International Agency for Research on Cancer: Available: http://globocan.iarc.fr. Accessed 2012 Jul 20.
- 3.Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, et al. (2003) Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med 349: 2091–2098. [DOI] [PubMed] [Google Scholar]
- 4.Myoung H, Kim MJ, Hong SD, Lee JI, Lim CY, et al. (2002) Expression of membrane type I-matrix metalloproteinase in oral squamous cell carcinoma. Cancer Lett 185: 201–209. [DOI] [PubMed] [Google Scholar]
- 5.O'Neill LA (2002) Signal transduction pathways activated by the IL-1 receptor/Toll-like receptor super family. Curr Top Microbiol Immunol 270: 47–61. [PubMed] [Google Scholar]
- 6.Takeda K, Akira S (2005) Toll-like receptors in innate immunity. Int Immunol 17: 1–14. [DOI] [PubMed] [Google Scholar]
- 7.Rakoff-Nahoum S, Medzhitov R (2009) Toll-like receptors and cancer. Nat Rev Cancer 9: 57–63. [DOI] [PubMed] [Google Scholar]
- 8.Chen R, Alvero AB, Silasi DA, Mor G (2007) Inflammation, cancer and chemoresistance: taking advantage of the toll-like receptor signalingpathway. Am J Reprod Immunol 57: 93–107. [DOI] [PubMed] [Google Scholar]
- 9.Xie W, Wang Y, Huang Y, Yang H, Wang J, et al. (2009) Toll-like receptor 2 mediates invasion via activating NF-kappaB in MDA-MB-231 breast cancer cells. Biochem Biophys Res Commun 379: 1027–1032. [DOI] [PubMed] [Google Scholar]
- 10.Merrell MA, Ilvesaro JM, Lehtonen N, Sorsa T, Gehrs B, et al. (2006) Toll-like receptor 9 agonists promote cellular invasion by increasing matrix metalloproteinase activity. Mol Cancer Res 4: 437–447. [DOI] [PubMed] [Google Scholar]
- 11.Hua D, Liu MY, Cheng ZD, Qin XJ, Zhang HM, et al. (2009) Small interfering RNA-directed targeting of Toll-like receptor 4 inhibits human prostate cancer cellinvasion, survival, and tumorigenicity. Mol Immunol 46: 2876–2884. [DOI] [PubMed] [Google Scholar]
- 12.Ilvesaro JM, Merrell MA, Swain TM, Davidson J, Zayzafoon M, et al. (2007) Toll like receptor-9 agonists stimulate prostate cancer invasion in vitro. Prostate 67: 774–781. [DOI] [PubMed] [Google Scholar]
- 13.Killeen SD, Wang JH, Andrews EJ, Redmond HP (2009) Bacterial endotoxin enhances colorectal cancer cell adhesion and invasion through TLR-4 and NF-κB-dependent activation of the urokinase plasminogen activator system. Br J Cancer 100: 1589–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo H, Chen Y, Hu X, Qian G, Ge S, et al. (2013) The regulation of toll-like receptor 2 by miR-143 suppresses the invasion and migration of a subset of human colorectal carcinoma cells. Molecular Cancer 12: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Neill LA, Golenbock D, Bowie AG (2013) The history of Toll-like receptors - redefining innate immunity. Nat Rev Immunol 13: 453–460. [DOI] [PubMed] [Google Scholar]
- 16.Ruan M, Zun Z, Siyi L, Wenjun Y, Lizheng W, et al. (2011) Increased expression of Toll-like receptor-9 has close relation with tumour cell proliferation in oral squamous cell carcinoma. Arch Oral Biol 56: 877–884. [DOI] [PubMed] [Google Scholar]
- 17.Min R, Siyi L, Wenjun Y, Shengwen L, Ow A, et al. (2012) Toll-like receptor-9 agonists increase cyclin D1 expression partly through activation of activator protein-1 in human oral squamous cell carcinoma cells. Cancer Sci 103: 1938–1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhong LP, Pan HY, Zhou XJ, Ye DX, Zhang L, et al. (2008) Characteristics of a cancerous cell line, HIOEC-B(a)P-96, induced by benzo(a)pyrene from human immortalized oral epithelial cell line. Arch Oral Biol 53: 443–452. [DOI] [PubMed] [Google Scholar]
- 19.Ruan M, Ji T, Yang WJ, Duan WH, Zhou XJ, et al. (2008) Growth Inhibition and Induction of Apoptosis in Human Oral Squamous Cell Carcinoma Tca-8113 Cell Lines by Shikonin was partly through the Inactivation of NF-κB Pathway. Phytother Res 22: 407–415. [DOI] [PubMed] [Google Scholar]
- 20.Kaomongkolgit R, Cheepsunthorn P, Pavasant P, Sanchavanakit N (2008) Iron increases MMP-9 expression through activation of AP-1 via ERK/Akt pathway in human head and neck squamous carcinoma cells. Oral Oncol 44: 587–594. [DOI] [PubMed] [Google Scholar]
- 21.Toualbi-Abed K, Daniel F, Güller MC, Legrand A, Mauriz JL, et al. (2008) Jun D cooperates with p65 to activate the proximal kB site of the cyclin D1 promoter: role of PI3K/PDK-1. Carcinogenesis 29: 536–543. [DOI] [PubMed] [Google Scholar]
- 22.Mantovani A (2009) Cancer: Inflaming metastasis. Nature 457: 36–37. [DOI] [PubMed] [Google Scholar]
- 23.Gupta GP, Massague J (2006) Cancer metastasis: building a framework. Cell 127: 679–695. [DOI] [PubMed] [Google Scholar]
- 24.Steeg PS (2006) Tumor metastasis: mechanistic insights and clinical challenges. Nat Med 12: 895–904. [DOI] [PubMed] [Google Scholar]
- 25.Egeblad M, Werb Z (2002) New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2: 161–174. [DOI] [PubMed] [Google Scholar]
- 26.Kusukawa J, Sasaguri Y, Shima I, Kameyama T, Morimatsu M (1993) Expression of matrix metalloproteinase-2 related to lymph node metastasis of oral squamous cell carcinoma. A clinicopathologic study. Am J Clin Pathol 99: 18–23. [DOI] [PubMed] [Google Scholar]
- 27.Li J, Guo Y, Feng X, Wang Z, Wang Y, Deng P, et al. (2005) Expression and clinical significance of matrix metalloproteinase-2 and matrix metalloproteinase-9 in oral squamous cell carcinoma. Oral Oncol 41: 283–293. [DOI] [PubMed] [Google Scholar]
- 28.Katayama A, Bandoh N (2004) Expressions of Matrix Metalloproteinases in Early-Stage Oral Squamous Cell Carcinoma as Predictive Indicators for Tumor Metastases and Prognosis. Clin Cancer Res 10: 634–640. [DOI] [PubMed] [Google Scholar]
- 29.Bergman MR, Cheng S, Honbo N, Piacentini L, Karliner JS, et al. (2003) A functional activating protein 1 (AP-1) site regulates matrix metalloproteinase 2 (MMP-2) transcription by cardiac cells through interactions with JunB-Fra1 and JunB-FosB heterodimers. Biochem J 369: 485–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Philip S, Kundu GC (2003) Osteopontin induces nuclear factor kappa B-mediated promatrix metalloproteinase-2 activation through I kappa B alpha/IKK signaling pathways, and curcumin (diferulolylmethane) down-regulates these pathways. J Biol Chem 278: 14487–14497. [DOI] [PubMed] [Google Scholar]
- 31.Kawai T, Akira S (2006) TLR signaling. Cell Death and Differentiation 13: 816–825. [DOI] [PubMed] [Google Scholar]
- 32.Yang XC, Wang X, Luo L, Dong DH, Yu QC, et al. (2013) RNA interference suppression of A100A4 reduces the growth and metastatic phenotype of human renal cancer cells via NF-kB-dependent MMP-2 and bcl-2 pathway. Eur Rev Med Pharmacol Sci 17: 1669–1680. [PubMed] [Google Scholar]
- 33.Hsieh YS, Chu SC, Yang SF, Chen PN, Liu YC, et al. (2007) Silibinin suppresses human osteosarcoma MG-63 cell invasion by inhibiting the ERK-dependent c-Jun/AP-1 induction of MMP-2. Carcinogenesis 28: 977–987. [DOI] [PubMed] [Google Scholar]
- 34.Hess J, Angel P, Schorpp-Kistner M (2004) AP-1 subunits: quarrel and harmony among siblings. J Cell Sci 117: 5965–5973. [DOI] [PubMed] [Google Scholar]
- 35.Perkins ND (2007) Integrating cell-signalling pathways with NF-kappaB and IKK function. Nat Rev Mol Cell Biol 8: 49–62. [DOI] [PubMed] [Google Scholar]