Abstract
Background
Smoking and overweight are principal determinants of poor health for which individual-level interventions are at best modestly effective. This limited effectiveness may be partly because these risk factors are patterned by parents’ experiences preceding the individual’s birth.
Purpose
To determine whether women’s experience of abuse in childhood was associated with smoking and overweight in their children.
Methods
In 2012, data were linked from two large longitudinal cohorts of women (Nurses’ Health Study II [NHSII], N=12,666) and their children (Growing Up Today [GUTS] Study, N=16,774), 1989–2010. Odds ratios of children following higher-risk smoking trajectories and risk ratios (RR) of children’s overweight and obesity by their mother’s childhood experience of physical, emotional, and sexual abuse were calculated. The extent to which mother’s smoking and overweight, socioeconomic indicators, family characteristics, and child’s abuse exposure accounted for possible associations was ascertained.
Results
Children of women who experienced severe childhood abuse had greater likelihood of higher-risk smoking trajectories (OR=1.40, 95% CI=1.21, 1.61), overweight (RR=1.21, 95% CI = 1.11, 1.33), and obesity (RR=1.45, 95% CI=1.21, 1.74) across adolescence and early adulthood compared with children of women who reported no abuse. Mother’s smoking and overweight and children’s abuse exposure accounted for more than half of the elevated risk of following the highest-risk smoking trajectory and overweight in children of women abused.
Conclusions
These findings raise the possibility that childhood abuse may not only adversely affect the health of the direct victim but may also affect health risk factors in her children decades after the original traumatic events.
Introduction
Smoking and overweight are principal determinants of poor health across the life course. Although these risk factors have long been recognized to contribute to poor health, they are stubbornly resistant to intervention. Policy measures such as indoor smoking bans and cigarette taxes have been successful at reducing smoking, but individual-level interventions for these risk factors are ineffective or only modestly effective over the longer term.1,2 This limited effectiveness may be because determinants of smoking and overweight extend beyond the individual and are difficult to change in the short term.3–5
Recent statements by the American Heart Association and the American Academy of Pediatrics have emphasized that early life events, such as excessive psychosocial (“toxic”) stressors, including childhood abuse, begin the health-risk processes that culminate in chronic disease in adulthood.6,7 It has also been hypothesized that health risk factors are in part consequences of events in prior generations.8 Better understanding of the roots of health risk factors may lead to better design of interventions to reduce their prevalence.
In the present study, data from two large longitudinal cohorts of women, the Nurses’ Health Study II (NHSII), and their adolescent and young adult children, the Growing Up Today Study (GUTS), were linked to examine whether mother’s experience of childhood abuse is associated with two sentinel health risk factors in her children: smoking and overweight. We hypothesize that mother’s experience of abuse in childhood may increase risk of her child’s smoking and overweight through three pathways. First, individuals who experience abuse in childhood are known to be at higher risk for smoking9 and overweight.10,11 As parents’ smoking and overweight are known to affect their children’s smoking and overweight,12,13 women’s abuse may be associated with her children’s smoking and overweight through the transmission of risk-related behaviors from mother to child. Second, abuse is associated with reduced educational attainment and lower socioeconomic status in adulthood,14 and persons abused in childhood are more likely to divorce as adults.15 Smoking16 and overweight17 are more common in persons with lower SES, and children in single-parent households are more likely to smoke9 and be overweight.18 Thus, women’s abuse may be associated with child’s health risks through socioeconomic and family factors. Finally, mothers who have experienced abuse are more likely to have children who are themselves abused,19–21 and abuse is associated with smoking9 and overweight.10,11,22
Methods
Sample
NHSII is a cohort of 116,430 nurses enrolled in 1989 and followed biennially. GUTS is a cohort of their children, enrolled in 1996 and followed annually or biennially. Investigators initially contacted the 34,174 NHSII participants with children aged 9 to 14 years to request consent for their children to participate; 18,526 mothers (54%) consented. Children whose mothers had consented were invited to participate (N=26,765). Approximately 63% of children (N=16,882) returned completed questionnaires.
Measures
Women’s childhood abuse
In 2001, participants of the NHSII were queried regarding childhood abuse experiences. Women’s exposure to physical and emotional abuse before age 11 years was assessed with the Physical and Emotional Abuse Subscale of the Child Trauma Questionnaire23 and was coded in quintiles. Women’s exposure to sexual abuse before age 18 years was assessed with four questions regarding unwanted or coerced sexual activity by an adult or older child, and was coded as none, mild, moderate, or severe.24 Because exposure to multiple types of abuse has been associated with worse health outcomes, a measure of combined exposure to physical, emotional, and sexual abuse ranging from zero (no abuse) to four (severe abuse) was created of which details have been previously published.25 To ascertain the relationship between women’s missing childhood abuse information and her children’s health risk factors, missing data indicators were included in our measures of women’s abuse.
Women’s smoking and BMI
Women’s lifetime smoking was assessed in 1989 with the question, “Have you ever smoked 20 packs of cigarettes or more in your lifetime?” Response options included: “no,” “yes, currently smoke,” and “yes, smoked in past but quit.” Current smoking was assessed biennially (1991–2009). Women’s BMI was calculated as kg2/m from self-reported weight and height, assessed biennially (1989–2009). Self-reported weight was highly reliable (r = 0.97) in a validation study.26
Child’s smoking and weight status
Cigarettes smoked per day during the past year was assessed in seven waves (1997–2007). Four smoking trajectories occurring from ages 12 to 23 years were determined using general growth mixture modeling27 based on average numbers of cigarettes smoked per week at each age. These trajectories were, in order of lowest to highest risk: nonsmoker, experimenter, late initiator leading to moderate consumption, and early initiator leading to high consumption. Participants were assigned to the trajectory group for which they had the highest posterior probability of membership.28
BMI was calculated in kg/m2 from child’s self-reported weight and height without shoes in 11 waves (1996–2010). BMI calculated from adolescent’s self-reported height and weight has been validated in two large national studies.29,30 International Obesity Task Force standards were used to determine age-and-sex-specific BMI cutoffs for overweight and obesity for respondents younger than age 18 years.31 For respondents aged 18– 30 years, BMI > 25kg/m2 was considered overweight and >30kg/m2 was considered obese.
Child’s childhood abuse
Children’s exposure to physical, emotional, and sexual abuse was measured similarly to mothers’.23,24,32
Socioeconomic indicators
Socioeconomic standing in the community and the U.S., validated measures of subjective social status previously associated with health outcomes,33 and family income were self-reported by mothers in 2001. Residential U.S,-Census–tract median income and percent college educated were obtained biennially (1989–2009) from women’s geocoded addresses.
Family characteristics
In 1996, children were asked which adults they live with most of the time. Responses were coded as: both parents, one parent, or one parent and a step-parent. Mother’s age at child’s birth was calculated by subtracting child’s birth year from mother’s birth year. Child’s parity was by mother’s report, coded as first-, second-, third-, or fourth-or-later-born.
Included participants
Of GUTS children, 16,774 (99%) reported weight and height in at least one wave, and 15,828 children (94%) reported whether or not they smoked in at least one wave. GUTS children who did versus did not report smoking behavior in at least one wave had mothers who were similar in smoking prevalence (9.0% versus 9.2%), childhood abuse (10.3% severe abuse versus 12.5%), and U.S. and community SES (both, median=4).
Analyses
The proportion of children following each smoking trajectory across adolescence by their mother’s exposure to combined physical, emotional, and sexual abuse was examined. To assess whether women’s experience of childhood abuse was associated with their child’s higher-risk smoking trajectory, odds ratios of following a higher-risk smoking trajectory were calculated using ordinal logistic regression models (the ordinal logistic model produces only odds ratios). Risk ratios for children following the highest-risk trajectory (early initiation leading to high cigarette consumption) versus not smoking by their mother’s experience of abuse were then calculated.
To examine whether women’s childhood abuse was associated with their child’s weight status, risk ratios for child’s overweight with women’s abuse as the independent variable were calculated. Finally, child’s risk of obesity by mother’s experience of childhood abuse was examined, excluding children who were overweight.
To determine whether mother’s health risks, socioeconomic indicators, family characteristics, and child’s experience of abuse accounted for possible associations among mother’s experience of abuse and child’s health risks, the association among mother’s experience of abuse and her health risks, socioeconomic indicators, family characteristics, and child’s experience of abuse was first examined. Next, mother’s respective health risk (e.g., her smoking to the model of child’s smoking, her BMI to the model of child’s overweight), socioeconomic indicators, family characteristics, and child’s experience of abuse were added to models, and the percent of the association that was accounted for by these factors was calculated using the Mediate macro in SAS.34 The percent of the association accounted for by the intermediate variables is: 100*(1−(exposure coefficient estimate with intermediaries/exposure coefficient estimate without intermediaries)). For mother’s health risks and tract-level socioeconomic indicators, measures from each NHSII wave prior to the start of GUTS (i.e., 1989–1995, as available) were added. In this way factors occurring during the six years before children’s outcomes were first measured were adjusted for. For child’s overweight, women’s BMI in each wave prior to the first child’s BMI measurement (i.e., 1989–1995) were entered as separate variables as well as an additional time-varying measure of women’s most recent BMI in the wave immediately prior each child’s BMI measure (i.e., mother’s measure in 2001 for child’s 2003 BMI).34 The same approach was followed for tract-level socioeconomic indicators. As smoking was conceptualized as a single trajectory across adolescence, beginning in 1996, mother’s smoking and tract-level socioeconomic indicators only before the start of GUTS (i.e., 1989–1995) were entered and not an additional most recent measure of mother’s smoking or socioeconomic indicators. As child’s exposure to abuse was assessed in 2007, the ninth year of the GUTS study, abuse data was available for only a subset of respondents (n=8,453). To assess the relationship between mother’s abuse and children’s health risk factors in the group of children who did not respond to abuse questions, a missing data indicator in models including children’s abuse was used.
Some women enrolled more than one child in GUTS; therefore generalized estimating equations were used to account for family clustering of exposures and outcomes and for repeated measures of child’s BMI. As smoking trajectory was an ordinal variable in four levels, ordered logistic regression with a cumulative logit link and a multinomial distribution was used to estimate odds ratios of following a worse trajectory. To estimate risk ratios of children following the highest-risk trajectory versus not smoking, a binomial distribution and a log link was used. For models of overweight, a log link and Poisson distribution was used to estimate risk ratios. All models were adjusted for child’s age, sex, race, and mother’s childhood SES, measured by the maximum of parents’ education at her birth, and coded categorically.
As factors affecting enrollment in the GUTS cohort may have biased effect estimates, the estimates weighted for mother’s probability of enrolling her child in GUTS were additionally calculated using inverse probability weights.35 Analyses were conducted in 2012.
Results
Approximately one-third of children had mothers who reported no physical, emotional, or sexual abuse (36.1%, N=4,631, Table 1). Approximately 10% of children had mothers who reported the most severe exposure to combined physical, emotional, and sexual abuse (10.2%, N=1,319). Women exposed to the most severe childhood abuse compared to those who did not experience abuse had higher prevalence of smoking (11.6% versus 7.5%) and higher BMI (24.3 versus 23.0kg/m2) (eTable). Mother’s experience of childhood abuse was also associated with living in a Census tract with slightly lower socioeconomic indicators, her child being less likely to live with both parents, and her child experiencing physical, emotional, or sexual abuse (eTable).
Table 1.
Child’s smoking by mother’s childhood experience of abuse, adjusted for mediators (N= 15,828 children)†
| Model 1a: Worse smoking trajectory |
Model 1b: Adjusted for mother’s smoking |
Model 1c: Adjusted for mother’s smoking, socioeconomic indicators, and family characteristics |
Model 1d: Adjusted for mother’s smoking, socioeconomic indicators, family characteristics, and child’s abuse |
||
|---|---|---|---|---|---|
| N | Odds ratio (95% confidence interval) | ||||
| Mother’s abuse | |||||
| 0: None | 4631 | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] | |
| 1 | 2984 | 1.17 (1.05, 1.30) | 1.16 (1.04, 1.29) | 1.15 (1.03, 1.29) | 1.15 (1.02, 1.28) |
| 2 | 1951 | 1.16 (1.02, 1.31) | 1.12 (0.99, 1.27) | 1.09 (0.96, 1.23) | 1.06 (0.94, 1.21) |
| 3 | 1938 | 1.26 (1.11, 1.43) | 1.21 (1.06, 1.37) | 1.16 (1.02, 1.32) | 1.13 (1.00, 1.29) |
| 4: Severe | 1319 | 1.40 (1.21, 1.61) | 1.30 (1.13, 1.50) | 1.23 (1.07, 1.42) | 1.17 (1.02, 1.22) |
| Missing | 3005 | 1.02 (0.91, 1.14) | 0.97 (0.86, 1.08) | 1.08 (0.96, 1.22) | 1.08 (0.96, 1.22) |
| Linear trend†† | Χ2=28.5, P<.0001 | Χ2=16.7, P<.0001 | Χ2=9.4, P<.01 | Χ2=4.8, P<.05 | |
| Child’s physical/emotional abuse | |||||
| 1st quintile | 1.0 [Reference] | ||||
| 2nd quintile | 1.21 (1.03, 1.42) | ||||
| 3rd quintile | 1.31 (1.11, 1.55) | ||||
| 4th quintile | 1.39 (1.18, 1.63) | ||||
| 5th quintile (worst) | 2.05 (1.73, 2.42) | ||||
| Missing | 2.07 (1.62, 2.63) | ||||
| Child’s sexual abuse | |||||
| None | 1.0 [Reference] | ||||
| Moderate | 1.36 (1.07, 1.74) | ||||
| Severe | 2.00 (1.62, 2.47) | ||||
| Missing | 0.57 (0.46, 0.71) | ||||
All models adjusted for child’s age, sex, and race and mother’s childhood SES. Smoking trajectories were assessed 1997–2007. Child’s worse smoking trajectory is modeled with a cumulative logistic model. Models of child’s overweight are generalized estimating equations with log links and Poisson distributions.
Linear trends were calculated excluding mothers missing abuse data.
Smoking
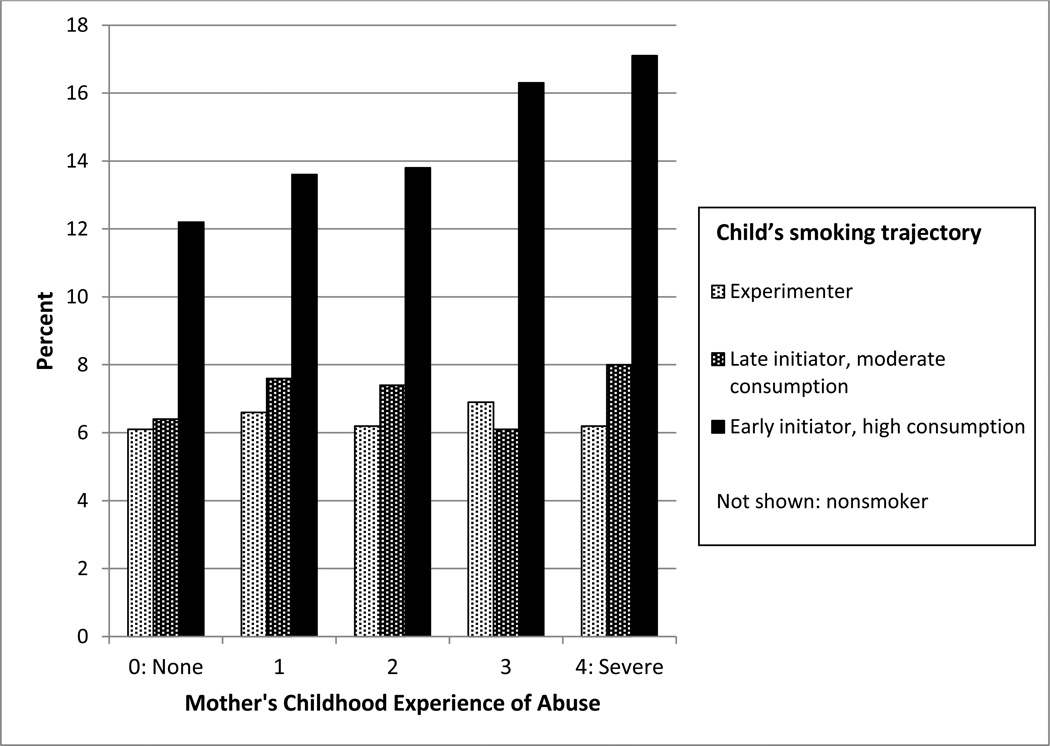
Children of women exposed, versus those not exposed, to childhood abuse were more likely to follow the highest-risk smoking trajectory of early initiation leading to high cigarette consumption (Figure 1). Prevalence of children following this trajectory increased monotonically with severity of women’s abuse experience.
Figure 1.
Child’s smoking trajectory across adolescence and early adulthood, ages 12–23 years, by mother's childhood experience of physical, emotional, and sexual abuse, Nurses’ Health Study II and Growing Up Today Study, 1997–2007
Note: N=12,548, 48,017 observations
Women’s exposure to childhood abuse was a strong predictor of her child’s higher-risk smoking trajectory (Table 1, Model 1a). In models adjusted for women’s past and current smoking, these associations were slightly attenuated (Table 1, Model 1b). Further adjustment for socioeconomic indicators and family characteristics further attenuated these associations (Table 1, Model 1c), as did adjustment for child’s own experience of abuse (Table 1, Model 1d). In the fully adjusted model, mother’s experience of abuse remained a statistically significant predictor of her child following a worse smoking trajectory. Children of women exposed to the highest level of abuse, versus those unexposed, were at greatest risk of following the highest-risk trajectory (RR=1.41, 95% CI=1.21, 1.64, P<.0001). In the fully adjusted model, mother’s smoking accounted for 33.6%, socioeconomic indicators 4.7%, family characteristics 6.8%, and child’s abuse 27.2% of the association between mother’s abuse and child’s likelihood of following the worst smoking trajectory.
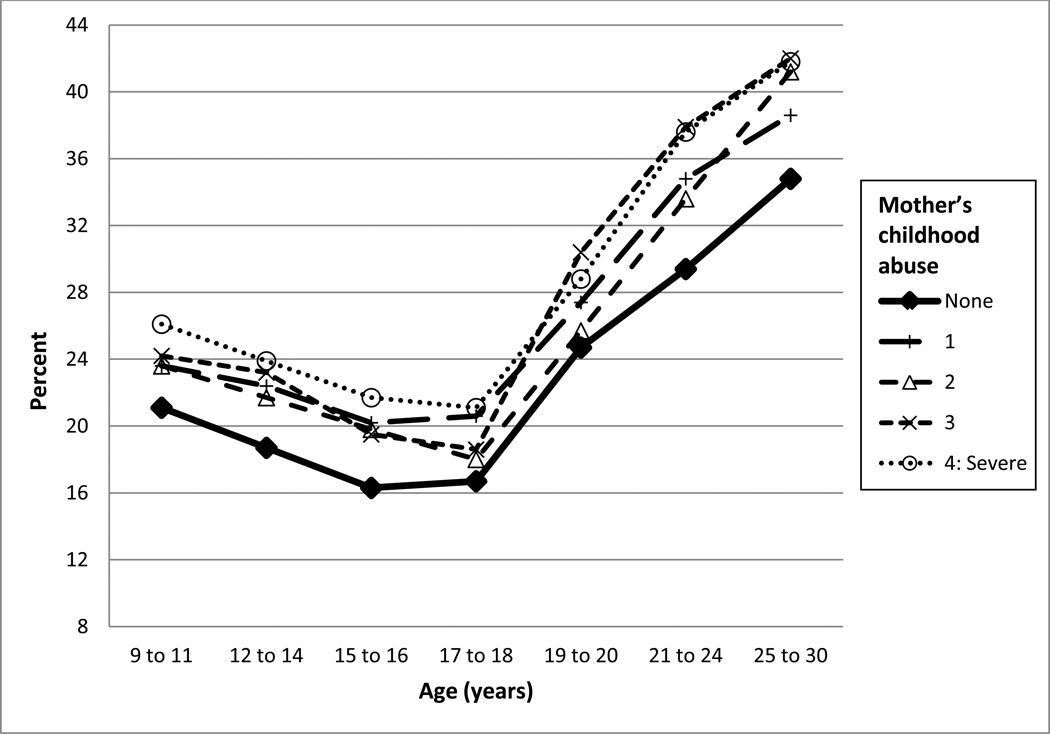
Weight status
Prevalence of overweight was higher in children of women exposed to childhood abuse, although there was not a uniform dose–response relationship between severity of abuse and prevalence of overweight (Figure 2). Women’s exposure to abuse was also associated with child’s increased risk of overweight. Children of women who experienced abuse were at greater risk of being overweight than children of women not abused (RR range, 1.14–1.21, Table 2, Model 2a). Adding women’s BMI to models attenuated the association between her experience of childhood abuse and her child’s overweight status (Table 2, Model 2b). Adding socioeconomic indicators and family characteristics to the model additionally attenuated effect estimates only slightly (Table 2, Model 2c). Child’s physical and emotional abuse was strongly associated with overweight but did not further account for the association between mother’s abuse and child’s overweight (Table 2, Model 2d). In the fully adjusted model, women’s BMI accounted for 57.8%, socioeconomic indicators 11.8%, family characteristics 3.9%, and child’s abuse 17.5% of the association between mother’s abuse and child’s likelihood of being overweight or obese. Risk of obesity was associated with mother’s abuse experiences, with children of women who experienced abuse at higher risk of being obese compared with children of women who did not experience abuse (RR range, 1.23–1.45; RR severe abuse=1.45, 95% CI=1.21, 1.74).
Figure 2.
Child’s overweight by mother's childhood experience of physical, emotional, and sexual abuse, Nurses’ Health Study II and Growing Up Today Study, 1996–2010
Note: N=13,385, 91,274 observations
Table 2.
Child’s overweight by mother’s childhood experience of abuse, adjusted for mediators (N=16,774 children; 108,469 observations)†
| Model 2a: Overweight |
Model 2b: Adjusted for mother’s BMI |
Model 2c: Adjusted for mother’s BMI, socioeconomic indicators, and family characteristics |
Model 2d: Adjusted for mother’s BMI, socioeconomic indicators, family characteristics, and child’s abuse |
||
|---|---|---|---|---|---|
| N | Risk ratio (95% confidence interval) | ||||
| Mother’s abuse | |||||
| 0: None | 3587 | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| 1 | 2328 | 1.17 (1.09, 1.26) | 1.11 (1.03, 1.19) | 1.10 (1.03, 1.18) | 1.10 (1.02, 1.18) |
| 2 | 1544 | 1.14 (1.05, 1.23) | 1.07 (0.99, 1.16) | 1.06 (0.97, 1.15) | 1.05 (0.97, 1.14) |
| 3 | 1525 | 1.20 (1.11, 1.31) | 1.13 (1.04, 1.22) | 1.11 (1.03, 1.21) | 1.10 (1.02, 1.19) |
| 4: Severe | 1045 | 1.21 (1.11, 1.33) | 1.09 (0.99, 1.19) | 1.07 (0.98, 1.18) | 1.06 (0.96, 1.16) |
| Missing | 2637 | 1.09 (1.02, 1.18) | 1.01 (0.94, 1.09) | 0.99 (0.91, 1.07) | 0.97 (0.90, 1.12) |
| Linear trend†† | Χ2=23.4, P<.0001 | Χ2=5.9, P<0.05 | Χ2=4.3, P<0.05 | Χ2=4.0, P<0.05 | |
| Child’s physical/emotional abuse | |||||
| 1st quintile | 1.0 [Reference] | ||||
| 2nd quintile | 1.02 (0.92, 1.12) | ||||
| 3rd quintile | 1.08 (0.98, 1.20) | ||||
| 4th quintile | 1.18 (1.07, 1.30) | ||||
| 5th quintile (worst) | 1.31 (1.19, 1.45) | ||||
| Missing | 1.09 (0.94, 1.27) | ||||
| Child’s sexual abuse | |||||
| None | 1.0 [Reference] | ||||
| Moderate | 1.07 (0.92, 1.25) | ||||
| Severe | 0.97 (0.84, 1.11) | ||||
| Missing | 1.03 (0.90, 1.18) | ||||
All models adjusted for mother’s childhood SES and child’s age, sex, and race.
Linear trends were calculated excluding persons missing abuse data.
In models separately examining mother’s physical, emotional, and sexual abuse, children’s worse smoking trajectory was strongly associated with mother’s sexual abuse and moderately associated with mother’s physical and emotional abuse. Children’s overweight and obesity were similarly associated with mother’s physical/emotional or sexual abuse (Table 3). For both outcomes, effect estimates in models weighted for probability of enrollment were nearly identical to estimates without weights.
Table 3.
Mother’s childhood exposure to physical/emotional or sexual abuse and child’s health risk factors†
| Child’s smoking trajectory |
Child’s overweight | Child’s obesity | |
|---|---|---|---|
| Odds ratio (95% CI) | Risk ratio (95% confidence interval) | ||
| Model 1a | Model 2a | Model 3a | |
| Mother’s physical/emotional abuse | |||
| 1st quartile | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| 2nd quartile | 1.04 (0.93, 1.17) | 1.12 (1.04, 1.21)** | 1.22 (1.05, 1.41)** |
| 3rd quartile | 1.04 (0.92, 1.17) | 1.11 (1.02, 1.20)** | 1.15 (0.97, 1.36) |
| 4th quartile (worst) | 1.16 (1.04, 1.29)** | 1.15 (1.07, 1.23)*** | 1.22 (1.05, 1.41)** |
| Missing | Not estimable | 1.04 (0.97, 1.12) | 1.06 (0.91, 1.22) |
| Model 1b | Model 2b | Model 3b | |
| Mother’s sexual abuse | |||
| None | 1.0 [Reference] | 1.0 [Reference] | 1.0 [Reference] |
| Mild | 1.14 (1.03, 1.25)** | 1.13 (1.06, 1.20)*** | 1.24 (1.10, 1.42)*** |
| Moderate | 1.50 (1.27, 1.76)*** | 1.07 (0.96, 1.20) | 1.12 (0.91, 1.39) |
| Severe | 1.73 (1.38, 2.19)*** | 1.09 (0.93, 1.27) | 1.29 (0.97, 1.71) |
| Missing | 0.85 (0.17, 4.14) | 1.01 (0.95, 1.09) | 1.03 (0.89, 1.18) |
Adjusted for child’s age, sex, and race, and mother’s parents’ education. Models of child’s worse smoking trajectory are cumulative logistic models. Models of child’s overweight and obesity are generalized estimating equations with log link and Poisson distributions. All models are calculated using SAS PROC GENMOD.
=Wald χ2 P<0.05;
=Wald χ2 P<0.01;
=Wald χ2 P<0.001
Discussion
We found an intergenerational association between a woman’s childhood experience of abuse and two sentinel health risk factors in her children: smoking and overweight. For children of abused women, excess prevalence of these major health determinants was observable as early as middle childhood and persisted into early adulthood. Additionally, the association of mothers’ abuse with the health risk factors in their children was strongest in children of women exposed to the most severe abuse. Women’s childhood abuse remained associated with child’s smoking and overweight after adjusting for women’s own smoking and BMI, socioeconomic indicators, family characteristics, and child’s abuse exposure.
Within individuals, the association between adversity in childhood and increased physical morbidity and mortality across the lifecourse is well documented.22 Trauma and violence have been associated with increased risk across generations for mental illness, including depression and posttraumatic stress disorder.32,36,37 However, to our knowledge, no prior studies have shown associations of trauma and violence with physical health risks across generations.
Women’s experience of abuse was associated with her children’s health risks through three pathways. The first pathway was through women’s own health risks. Women’s smoking and BMI accounted for the largest proportion of the association between her abuse experience and her children’s smoking and overweight. Parents who smoke model smoking behavior and establish smoking as normative for their children.12 Children of smokers versus nonsmokers have greater access to cigarettes and more lenient house rules regarding smoking, factors which increase children’s likelihood of initiating and maintaining smoking.12,38 Similarly, research suggests that obesogenic behaviors, including higher sugar sweetened beverage consumption, lower consumption of fruits and vegetables, and lack of physical activity partly account for associations between parents’ overweight and children’s overweight.39,40 In addition to smoking and overweight, parent-children concordance has been observed across a broad range of behaviors, including drug and alcohol use,41–43 sexual infidelity,44,45 and speeding.46
The second pathway was through SES and family characteristics. Children of abused mothers had lower socioeconomic indicators and were less likely to live with both parents than children of nonabused mothers, factors that also accounted for part of the associations between mother’s abuse and children’s health risks. Low SES in adolescence has been associated with poor diet and less physical activity, which increase risk of overweight.47 In addition to smoking and overweight, low SES has also been associated in adolescents with worse health generally, more school and activity limitations, and more injuries, but not with increased marijuana or alcohol use.48 Children living in single-parent versus two-parent families have higher prevalence of behaviors that increase risk of overweight, such as eating unstructured meals, not eating breakfast, and having more screen time.18,49 Children of divorced parents experience more family conflict,50 and have less maternal support and supervision,51 which may increase health-risk behaviors.
Finally, children of abused mothers were themselves more likely to experience abuse than children of nonabused mothers, which accounted for an additional proportion of the associations we found. Experience of abuse is associated not only with smoking and overweight in adolescence, but also with substance use, sexual risk-taking, violence and criminality.52,53 Hypothesized pathways include poorer mental health, increased stress reactivity,54 difficulties with emotional regulation,55 and adverse peer selection.56 Taken together, women’s health risk factors, SES and family characteristics, and child’s own abuse experiences accounted for 72.3% of the association between mother’s abuse and child’s risk of following the highest-risk smoking trajectory, and 91.0% of the association between mother’s abuse and child’s overweight. In addition to these pathways, father’s smoking and BMI may account for an additional proportion of the associations we found. Smoking and BMI in women and their spouses are correlated, in part due to assortative mating,57 and father’s smoking and overweight may increase risk for child’s smoking58,59 and overweight.60–62 Women’s experience of abuse may also affect her children through gestational exposures, possibly operating in part through epigenetic mechanisms. During pregnancy, women exposed to childhood abuse have higher prevalence of a wide array of perinatal risk factors compared with women not exposed to abuse, including gestational diabetes, intimate partner violence victimization, and smoking.25 Exposure to suboptimal circumstances,63 maternal stress,64 and harmful substances during gestation65,66 may cause epigenetic changes in the fetus that lead to alterations in stress response and metabolic function,67–70 which could increase risk for later smoking and overweight.
Our study has three key limitations. First, the NHSII cohort enrolled registered nurses and is predominantly white, reflecting the race/ethnic composition of the nursing profession at the time of study enrollment. Thus, our results may not apply to other race/ethnic or occupational groups. Second, women’s experience of abuse and children’s health risk factors were self-reported; misreporting, particularly of child’s weight,29,71 may have biased our results. Separate report by mothers of abuse and by children of health risk factors may minimize associations due to reporting bias, however. Third, due to the multigenerational and longitudinal nature of the study, data were available for only 34% of eligible children, potentially biasing results. However, results were nearly identical in analyses weighted for probability of enrollment.
Our findings provide further evidence that forces beyond the individual—even events occurring before his or her birth—may shape individual health behavior and that interventions may need to account for the deep roots of health behavior to improve efficacy. Phelan and Link (1995)72 identified social conditions as fundamental causes of disease because they affect multiple disease outcomes through diverse mechanisms and thereby are associated with disease, even when some intervening pathways are altered. Childhood abuse may be another such fundamental cause of disease. Our findings suggest diverse pathways through which women’s abuse experience may affect her children. Further research is needed to determine to what extent children’s gestational exposures or other factors account for the part of the associations not explained by the factors we examined.
Treatment and prevention of childhood abuse may be an efficacious approach to improving health not only in the present generation but also in the subsequent generation, across multiple domains. The risk factors we examined are major contributors to cancer, heart disease, and diabetes, leading causes of mortality, disability and health-care expenditures. Thus, calculations of benefit from and cost-effectiveness of childhood abuse prevention measures should consider effects across as well as within generations.
Supplementary Material
Acknowledgments
AL Roberts is supported by NIH MH078928 and MH093612. S Galea is supported by NIH MH095718, MH082598, MH 082729, DA013336, and DA034244 and by the Department of Defense W81XWH-07-1-0409. SB Austin is supported by the Leadership Education in Adolescent Health project, Maternal and Child Health Bureau, HRSA 6T71-MC00009. HL Corliss is supported by NIDA K01 DA023610. KC Koenen is supported by the NIH MH078928 and MH093612. The Nurses' Health Study II is funded in part by NIH CA50385. We acknowledge the Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School for its management The Nurses' Health Study II and the Growing Up Today Study. The funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Lemmens V, Oenema A, Knut IK, Brug J. Effectiveness of smoking cessation interventions among adults: a systematic review of reviews. European journal of cancer prevention. 2008;17:535. doi: 10.1097/CEJ.0b013e3282f75e48. [DOI] [PubMed] [Google Scholar]
- 2.Brown T, et al. Systematic review of long-term lifestyle interventions to prevent weight gain and morbidity in adults. Obesity Reviews. 2009;10:627–638. doi: 10.1111/j.1467-789X.2009.00641.x. [DOI] [PubMed] [Google Scholar]
- 3.Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obesity Reviews. 2009;10:110–141. doi: 10.1111/j.1467-789X.2008.00515.x. [DOI] [PubMed] [Google Scholar]
- 4.Kling JR, Liebman JB, Katz LF, Sanbonmatsu L. Moving to opportunity and tranquility: Neighborhood effects on adult economic self-sufficiency and health from a randomized housing voucher experiment. Harvard University: John F. Kennedy School of Government; 2004. [Google Scholar]
- 5.Modin B, Fritzell J. The long arm of the family: are parental and grandparental earnings related to young men's body mass index and cognitive ability? International journal of epidemiology. 2009;38:733–744. doi: 10.1093/ije/dyp001. [DOI] [PubMed] [Google Scholar]
- 6.Lloyd-Jones DM, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 7.Garner AS, Shonkoff JP. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129:e224–e231. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- 8.Galobardes B, Lynch JW, Smith GD. Review: Is the association between childhood socioeconomic circumstances and cause-specific mortality established? Update of a systematic review. Journal of Epidemiology and Community Health (1979-) 2008;62:387–390. doi: 10.1136/jech.2007.065508. [DOI] [PubMed] [Google Scholar]
- 9.Anda RF, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282:1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 10.Gustafson TB, Sarwer DB. Childhood sexual abuse and obesity. Obesity Reviews. 2004;5:129–135. doi: 10.1111/j.1467-789X.2004.00145.x. [DOI] [PubMed] [Google Scholar]
- 11.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Molecular psychiatry. 2013 doi: 10.1038/mp.2013.54. [DOI] [PubMed] [Google Scholar]
- 12.Jackson C, Henriksen L. Do as I say: Parent smoking, antismoking socialization, and smoking onset among children. Addictive Behaviors. 1997;22:107–114. doi: 10.1016/0306-4603(95)00108-5. doi: http://dx.doi.org/10.1016/0306-4603(95)00108-5. [DOI] [PubMed] [Google Scholar]
- 13.Drake AJ, Reynolds RM. Impact of maternal obesity on offspring obesity and cardiometabolic disease risk. Reproduction. 2010;140:387–398. doi: 10.1530/REP-10-0077. [DOI] [PubMed] [Google Scholar]
- 14.Olds D, et al. Long-term effects of nurse home visitation on children's criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial. Journal of the American Medical Association. 1998;280:1238–1244. doi: 10.1001/jama.280.14.1238. [DOI] [PubMed] [Google Scholar]
- 15.Colman RA, Widom CS. Childhood abuse and neglect and adult intimate relationships: a prospective study. Child Abuse & Neglect. 2004;28:1133–1151. doi: 10.1016/j.chiabu.2004.02.005. doi: http://dx.doi.org/10.1016/j.chiabu.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Flint AJ, Novotny TE. Poverty status and cigarette smoking prevalence and cessation in the United States, 1983–1993: the independent risk of being poor. Tobacco Control. 1997;6:14–18. doi: 10.1136/tc.6.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miech RA, et al. TRends in the association of poverty with overweight among us adolescents, 1971–2004. JAMA. 2006;295:2385–2393. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- 18.Yannakoulia M, et al. Association Between Family Divorce and Children's BMI and Meal Patterns: The GENDAI Study. Obesity. 2008;16:1382–1387. doi: 10.1038/oby.2008.70. [DOI] [PubMed] [Google Scholar]
- 19.McCloskey LA, Bailey JA. The Intergenerational Transmission of Risk for Child Sexual Abuse. J. Interpers. Violence. 2000;15:1019–1035. [Google Scholar]
- 20.Pears KC, Capaldi DM. Intergenerational transmission of abuse: a two-generational prospective study of an at-risk sample. Child Abuse & Neglect. 2001;25:1439–1461. doi: 10.1016/s0145-2134(01)00286-1. [DOI] [PubMed] [Google Scholar]
- 21.Cort NA, Toth SL, Cerulli C, Rogosch F. Maternal Intergenerational Transmission of Childhood Multitype Maltreatment. Journal of Aggression, Maltreatment & Trauma. 2011;20:20–39. [Google Scholar]
- 22.Felitti VJ, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 23.Bernstein DP, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 24.Moore D, Gallup G, Schussel R. Disciplining children in America: A Gallup poll report. Princeton, NJ: The Gallup Organization; 1995. [Google Scholar]
- 25.Roberts AL, Lyall K, Rich-Edwards JW, Ascherio A, Weisskopf MG. Association of maternal exposure to childhood abuse with elevated risk for autism in offspring. Journal of the American Medical Association Psychiatry. 2013;70:508–515. doi: 10.1001/jamapsychiatry.2013.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rimm EB, et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–473. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Muthen B, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;55:463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- 28.Nagin DS, Tremblay RE. Analyzing developmental trajectories of distinct but related behaviors: a group-based method. Psychological methods. 2001;6:18–34. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 29.Strauss RS. Comparison of measured and self-reported weight and height in a cross-sectional sample of young adolescents. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 1999;23:904–908. doi: 10.1038/sj.ijo.0800971. [DOI] [PubMed] [Google Scholar]
- 30.Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106:52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- 31.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roberts AL, et al. Posttraumatic stress disorder across two generations: Concordance and mechanisms in a population-based sample. Biological Psychiatry. 2012;72:505–511. doi: 10.1016/j.biopsych.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: its determinants and its association with measures of ill-health in the Whitehall II study. Social Science & Medicine. 2003;56:1321–1333. doi: 10.1016/s0277-9536(02)00131-4. doi: http://dx.doi.org/10.1016/S0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- 34.The SAS mediate macro. Boston: Brigham and Women's Hospital, Channing Laboratory; 2009. [Google Scholar]
- 35.Rotnitzky A, Robins JM. Semiparametric Regression Estimation in the Presence of Dependent Censoring. Biometrika. 1995;82:805–820. [Google Scholar]
- 36.Hammen C, Brennan PA, Le Brocque R. Youth depression and early childrearing: Stress generation and intergenerational transmission of depression. J. Consult. Clin. Psychol. 2011;79:353–363. doi: 10.1037/a0023536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gershon A, et al. Life stress and first onset of psychiatric disorders in daughters of depressed mothers. J. Psychiatr. Res. 2011;45:855–862. doi: 10.1016/j.jpsychires.2011.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maggi S, et al. Adolescents’ Perceptions of Parental Influences on Their Smoking Behavior: A Content Analysis. Youth & Society. 2012 [Google Scholar]
- 39.Kosti RI, et al. Parental Body Mass Index in association with the prevalence of overweight/obesity among adolescents in Greece; dietary and lifestyle habits in the context of the family environment: The Vyronas study. Appetite. 2008;51:218–222. doi: 10.1016/j.appet.2008.02.001. doi: http://dx.doi.org/10.1016/j.appet.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 40.Tibbs T, et al. The relationship between parental modeling, eating patterns, and dietary intake among African-American parents. Journal of the American Dietetic Association. 2001;101:535–541. doi: 10.1016/S0002-8223(01)00134-1. doi: http://dx.doi.org/10.1016/S0002-8223(01)00134-1. [DOI] [PubMed] [Google Scholar]
- 41.Yule AM, Wilens TE, Martelon MK, Simon A, Biederman J. Does exposure to parental substance use disorders increase substance use disorder risk in offspring? A 5-year follow-up study. The American Journal on Addictions. 2013;22:460–465. doi: 10.1111/j.1521-0391.2013.12048.x. [DOI] [PubMed] [Google Scholar]
- 42.Fergusson DM, Boden JM, Horwood LJ. The developmental antecedents of illicit drug use: Evidence from a 25-year longitudinal study. Drug and Alcohol Dependence. 2008;96:165–177. doi: 10.1016/j.drugalcdep.2008.03.003. doi: http://dx.doi.org/10.1016/j.drugalcdep.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 43.Brook JS, et al. The Relationship between Parental Alcohol Use, Early and Late Adolescent Alcohol Use, Young Adult Psychological Symptoms: A Longitudinal Study. The American Journal on Addictions. 2010;19:534–542. doi: 10.1111/j.1521-0391.2010.00083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Havlicek J, Husarova B, Rezacova V, Klapilova K. Correlates of extra-dyadic sex in Czech heterosexual couples: does sexual behavior of parents matter? Arch. Sex. Behav. 2011;40:1153–1163. doi: 10.1007/s10508-011-9869-3. [DOI] [PubMed] [Google Scholar]
- 45.L. Platt RA, Nalbone DP, Casanova GM, Wetchler JL. Parental conflict and infidelity as predictors of adult children's attachment style and infidelity. The American Journal of Family Therapy. 2008;36:149–161. [Google Scholar]
- 46.Fleiter JJ, Lennon A, Watson B. How do other people influence your driving speed? Exploring the ‘who’ and the ‘how’ of social influences on speeding from a qualitative perspective. Transportation research part F: traffic psychology and behaviour. 2010;13:49–62. [Google Scholar]
- 47.Hanson M, Chen E. Socioeconomic Status and Health Behaviors in Adolescence: A Review of the Literature. Journal of Behavioral Medicine. 2007;30:263–285. doi: 10.1007/s10865-007-9098-3. [DOI] [PubMed] [Google Scholar]
- 48.Chen E, Martin AD, Matthews KA. Socioeconomic status and health: Do gradients differ within childhood and adolescence? Social Science & Medicine. 2006;62:2161–2170. doi: 10.1016/j.socscimed.2005.08.054. doi: http://dx.doi.org/10.1016/j.socscimed.2005.08.054. [DOI] [PubMed] [Google Scholar]
- 49.Pearson N, Biddle SJH, Gorely T. Family correlates of breakfast consumption among children and adolescents. A systematic review. Appetite. 2009;52:1–7. doi: 10.1016/j.appet.2008.08.006. doi: http://dx.doi.org/10.1016/j.appet.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 50.Kristjansson AL, Sigfusdottir ID, Allegrante JP, Helgason AR. Parental divorce and adolescent cigarette smoking and alcohol use: assessing the importance of family conflict. Acta Pædiatrica. 2009;98:537–542. doi: 10.1111/j.1651-2227.2008.01133.x. [DOI] [PubMed] [Google Scholar]
- 51.Brown SL, Rinelli LN. Family Structure, Family Processes, and Adolescent Smoking and Drinking. J. Res. Adolesc. 2010;20:259–273. doi: 10.1111/j.1532-7795.2010.00636.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hussey JM, Chang JJ, Kotch JB. Child Maltreatment in the United States: Prevalence, Risk Factors, and Adolescent Health Consequences. Pediatrics. 2006;118:933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- 53.Gilbert R, et al. Burden and consequences of child maltreatment in high-income countries. The Lancet. 373:68–81. doi: 10.1016/S0140-6736(08)61706-7. doi: http://dx.doi.org/10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 54.Heim C, Nemeroff CB. The impact of early adverse experiences on brain systems involved in the pathophysiology of anxiety and affective disorders. Biol Psychiatry. 1999;46:1509–1522. doi: 10.1016/s0006-3223(99)00224-3. [DOI] [PubMed] [Google Scholar]
- 55.Loman MM, Gunnar MR. Early experience and the development of stress reactivity and regulation in children. Neuroscience & Biobehavioral Reviews. 2010;34:867–876. doi: 10.1016/j.neubiorev.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fergusson DM, Horwood LJ. Prospective Childhood Predictors of Deviant Peer Affiliations in Adolescence. Journal of Child Psychology and Psychiatry. 1999;40:581–592. [PubMed] [Google Scholar]
- 57.Di Castelnuovo A, Quacquaruccio G, Donati MB, de Gaetano G, Iacoviello L. Spousal concordance for major coronary risk factors: A systematic review and meta-analysis. American Journal of Epidemiology. 2009;169:1–8. doi: 10.1093/aje/kwn234. [DOI] [PubMed] [Google Scholar]
- 58.Conrad KM, Flay BR, Hill D. Why children start smoking cigarettes: predictors of onset. British Journal of Addiction. 1992;87:1711–1724. doi: 10.1111/j.1360-0443.1992.tb02684.x. [DOI] [PubMed] [Google Scholar]
- 59.Murray M, Kiryluk S, Swan AV. Relation between parents' and children's smoking behaviour and attitudes. Journal of Epidemiology and Community Health. 1985;39:169–174. doi: 10.1136/jech.39.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maffeis C, Talamini G, Tatò L. Influence of diet, physical activity and parents' obesity on children's adiposity: a four-year longitudinal study. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 1998;22:758–764. doi: 10.1038/sj.ijo.0800655. [DOI] [PubMed] [Google Scholar]
- 61.Danielzik S, Langnäse K, Mast M, Spethmann C, Müller MJ. Impact of parental BMI on the manifestation of overweight 5–7 year old children. Eur J Nutr. 2002;41:132–138. doi: 10.1007/s00394-002-0367-1. [DOI] [PubMed] [Google Scholar]
- 62.Lake JK, Power C, Cole TJ. Child to adult body mass index in the 1958 British birth cohort: associations with parental obesity. Archives of Disease in Childhood. 1997;77:376–380. doi: 10.1136/adc.77.5.376. [DOI] [PubMed] [Google Scholar]
- 63.Dunn GA, Bale TL. Maternal High-Fat Diet Effects on Third-Generation Female Body Size via the Paternal Lineage. Endocrinology. 2011;152:2228–2236. doi: 10.1210/en.2010-1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.de Kloet ER, Sibug RM, Helmerhorst FM, Schmidt MV. Stress, genes and the mechanism of programming the brain for later life. Neurosci Biobehav Rev. 2005;29:271–281. doi: 10.1016/j.neubiorev.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 65.Breton C, et al. Prenatal tobacco smoke exposure affects global and gene-specific DNA methylation. American journal of respiratory and critical care medicine. 2009:200901. doi: 10.1164/rccm.200901-0135OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dolinoy DC, Huang D, Jirtle RL. Maternal nutrient supplementation counteracts bisphenol A-induced DNA hypomethylation in early development. Proc Natl Acad Sci U S A. 2007;104:13056–13061. doi: 10.1073/pnas.0703739104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bale TL. Sex differences in prenatal epigenetic programing of stress pathways. Stress. 2011;14:348–356. doi: 10.3109/10253890.2011.586447. [DOI] [PubMed] [Google Scholar]
- 68.Bale TL, et al. Early Life Programming and Neurodevelopmental Disorders. Biological Psychiatry. 2010;68:314–319. doi: 10.1016/j.biopsych.2010.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Franklin TB, Mansuy IM. Epigenetic inheritance in mammals: evidence for the impact of adverse environmental effects. Neurobiol Dis. 2010;39:61–65. doi: 10.1016/j.nbd.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 70.Branchi I, Francia N, Alleva E. Epigenetic control of neurobehavioural plasticity: the role of neurotrophins. Behav Pharmacol. 2004;15:353–362. doi: 10.1097/00008877-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 71.Nieto-Garcia FJ, Bush TL, Keyl PM. Body mass definitions of obesity: sensitivity and specificity using self-reported weight and height. Epidemiology. 1990:146–152. [PubMed] [Google Scholar]
- 72.Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.