Abstract
Some orthopoxviruses including cowpox virus embed virus particles in dense bodies, comprised of the A-type inclusion (ATI) protein, which may provide long-term environmental protection. This strategy could be beneficial if the host population is sparse or spread is inefficient or indirect. However, the formation of ATI may be neutral or disadvantageous for orthopoxviruses that rely on direct respiratory spread. Disrupted ATI open reading frames in orthopoxviruses such as variola virus, the agent of smallpox, and monkeypox virus suggests that loss of this feature provided positive selection. To test this hypothesis, we constructed cowpox virus mutants with deletion of the ATI gene or another gene required for embedding virions. The ATI deletion mutant caused greater weight loss and higher replication in the respiratory tract than control viruses, supporting our hypothesis. Deletion of the gene for embedding virions had a lesser effect, possibly due to known additional functions of the encoded protein.
Keywords: Poxvirus pathogenicity, Cowpox virus inclusions, Respiratory virus infection
Introduction
Poxviruses are widely dispersed within vertebrate and insect species and have evolved alternative strategies for survival and spread (Damon, 2013, Moss, 2013). Some poxviruses form large inclusions in the cytoplasm in which mature virions (MVs) are embedded. Such structures called A-type inclusions (ATIs), Downie bodies and Marchal bodies by different investigators (Downie, 1939, Goodpature and Woodruff, 1931, Kato et al., 1959, Marchal, 1930) occur within several genera of chordopoxviruses and entomopoxviruses (Bergoin et al., 1971). It is thought that these structures prolong infectivity by protecting the embedded virions from ultraviolet irradiation and other environmental stresses. Many poxviruses, however, lack the ability to embed virions in inclusions and depend on the intrinsic stability of the MVs in the environment or direct animal-to-animal spread. In this regard orthopoxviruses are notable because some species including cowpox virus (CPXV), ectromelia virus, volepox virus and raccoon poxvirus have ATIs whereas others such as monkeypox virus, variola virus, vaccinia virus (VACV) and horsepox virus do not. The gene encoding the ATI protein has been identified (Funahashi et al., 1988, Patel and Pickup, 1987) allowing detection of disrupted ATI open reading frames (ORFs) in many orthopoxviruses that do not make inclusions. The latter observation suggests that the common orthopoxvirus ancestor encoded the ATI protein and that under some circumstances the loss of this feature was a positive or neutral selection factor that occurred during speciation.
CPXV strains that spontaneously lost the ability to produce ATI have been isolated by plaque picking (Amano and Tagaya, 1981). However, no differences in the hemorrhagic and necrotic lesions in rabbit skin were noted in that brief study. In a more detailed report, Leite and coworkers (Leite et al., 2011) deleted the gene encoding the ATI from the Brighton strain of CPXV and compared replication and pathogenicity of the mutant and parent viruses. In that study, deletion of the ATI gene had no effect on virus replication in cell culture but reduced the size and decreased the histopathology of lesions produced in the ear pinnae. However, the Brighton strain of CPXV was extensively passaged in cell culture and has a mutated copy of the gene encoding the p4c protein (corresponding to the A26L gene of VACV) such that it cannot produce a full-length protein capable of directing MVs into the ATIs (McKelvey et al., 2002). Therefore neither the parent CPXV Brighton nor the mutant embedded virus particles in ATI. In addition, the antibiotic-resistance and reporter genes used to replace the ATI ORF were retained in the deletion mutant and could impact host responses and pathogenicity.
We chose a CPXV strain with intact ATI and A26L homolog genes that had been isolated from a human infection (Carroll et al., 2011) for construction of ATI and A26L gene deletion mutants. Following intranasal (i.n.) infection, the ATI mutant caused greater weight loss and increased replication in the respiratory tract than control viruses providing a possible explanation for positive selection of orthopoxvirus mutants with disruptions of ATI. Enhanced replication to a lesser degree was observed with the A26L mutant.
Results
Initial characterization of the CPXV isolate
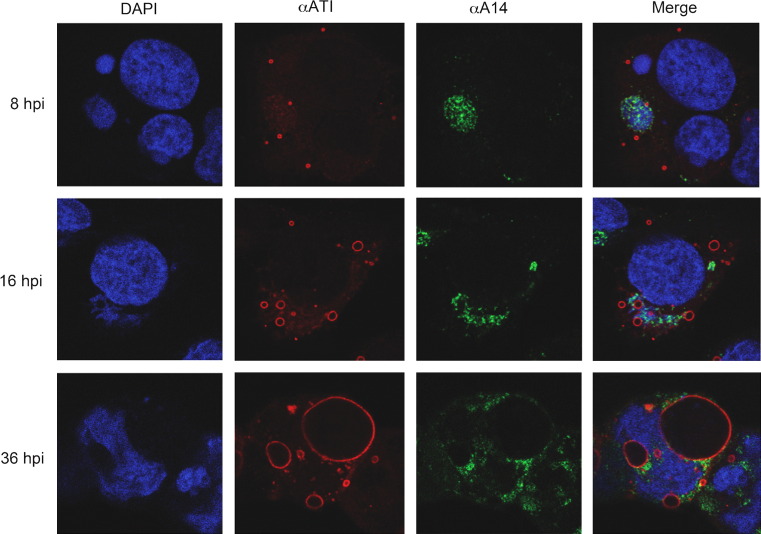
The virus chosen for this study, CPXV_GER1991_3 (abbreviated CPXV 91/3), caused local lesions in humans (Carroll et al., 2011) and was kindly provided by H. Meyer. Complete genome sequencing had indicated that both the ATI gene (CPXV 149) and the A26L VACV homolog (CPXV 150) were intact. To demonstrate ATI formation and the embedding of MVs, HeLa cells were infected and examined by confocal microscopy. DAPI was used to visualize DNA in the nucleus and virus factories and the ATI protein was stained with specific antibody provided by D. Pickup (Patel et al., 1986). The ATIs appeared as circles rather than discs within the cytoplasm because of the inability of the antibody to penetrate the interior of the structures after chemical fixation (Howard and Moss, 2012). The ATIs increased in diameter as the infection progressed ( Fig. 1). At 36 h after infection, large ATI occasionally appeared to be pressing into the nucleus and distorting its shape. Antibody to the homolog of the VACV A14 protein, which is a membrane component of MVs, stained particles in factories and adjacent to ATIs but also could not penetrate the latter structures after fixation (Fig. 1). ATIs and embedded MVs, however, were visualized by electron microscopy of infected cell sections and will be shown below.
Fig. 1.
Confocal microscopy images of cells infected with CPXV 91/3 showing ATI. HeLa cells were prepared for confocal imaging at 8, 16 and 36 h after infection (hpi). DNA in nuclei and cytoplasmic factories was stained with DAPI; ATI were stained with a specific polyclonal antibody; and virus factories and particles were stained with a MAb to the A14 membrane protein.
CPXV 91/3 was propagated in BS-C-1 cells and virus from individual plaques was clonally purified. Stocks were prepared from three of the clones and compared to the parental virus following i.n. infection of BALB/c mice. At a dose of 106 plaque-forming units (PFU), neither the parental virus nor the clonal isolates caused significant weight loss (data not shown). Therefore, one clonal isolate was chosen as representative for further studies. In contrast, we confirmed that the commonly used Brighton strain of CPXV, which is missing the gene needed for embedding MVs in ATIs, had an LD50 of 2 × 105 PFU in BALB/c mice (data not shown), similar to that previously reported (Thompson et al., 1993). We considered that the low pathogenicity of CPXV 91/3 might provide a sensitive model for testing our hypothesis that loss of ATI formation would enhance virulence.
Construction of ATI and A26 null mutants
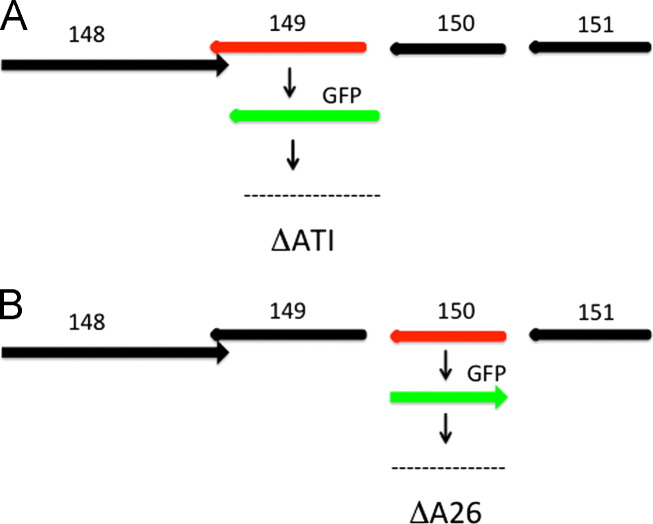
We employed a two-step procedure to make ATI (CPXV A149) and A26L (CPXV A150) gene deletion mutants of the CPXV 91/3 clone ( Fig. 2). The first step was to replace ORF 149 or ORF 150 with the gene encoding green fluorescent protein (GFP) by homologous recombination. In order to avoid truncation of ORF 148, which encodes a large subunit of the RNA polymerase and slightly overlaps ORF 149, the C-terminal six amino acids of ORF 149 were retained. Following homologous recombination, plaques containing recombinant viruses were identified by green fluorescence and clonally purified. For the second step we deleted the GFP ORF of the recombinant viruses to create ATI and A26R null mutants without the reporter gene. In parallel, we replaced the GFP ORF with the original ORF to make two revertant controls from the same clones. The two deletion mutants were named ΔATI and ΔA26 and the revertants ATIRev and A26Rev. DNA sequencing (not shown) and Western blotting ( Fig. 3) were performed to verify the absence or presence of the ORFs and protein expression, respectively. The cloned 91/3 parental virus and the revertants were indistinguishable in all subsequent experiments suggesting the absence of extraneous alterations that would affect the phenotypes of either mutant virus.
Fig. 2.
Construction of ATI and A26 deletion mutants by homologous recombination: (A) deletion of ORF 149. The arrangement of ORF 148 (RPO132 RNA polymerase subunit), ORF 149 (ATI), ORF 150 (VACV A26 homolog) and ORF 151 (VACV A27 homolog) within the CPXV genome is shown. ORF 149 overlaps ORF 148 by 22 nt; ORF 149 is separated by 44 nt from ORF 150; ORF 150 is separated by 51 nt from ORF 151. The first step was replacement of the region, from 39 nt to the right of the start codon including the ATI promoter to 21 nt preceding the 148 ORF, by the GFP ORF regulated by the P11 late promoter. In the next step, GFP was removed to create the ΔATI deletion mutant, in which the stop codon of ORF 148 was separated from the stop codon of ORF 150 by 5 nt. (B) Deletion of ORF 150. The first step was replacement of the region, from 51 nt upstream of the start codon of ORF 150 including the promoter to the stop codon, by GFP regulated by the P11 late promoter. The GFP ORF was then removed to create the ΔA26 deletion mutant, in which the stop codon of gene 151 was separated from the stop codon of 149 by 44 nt.
Fig. 3.
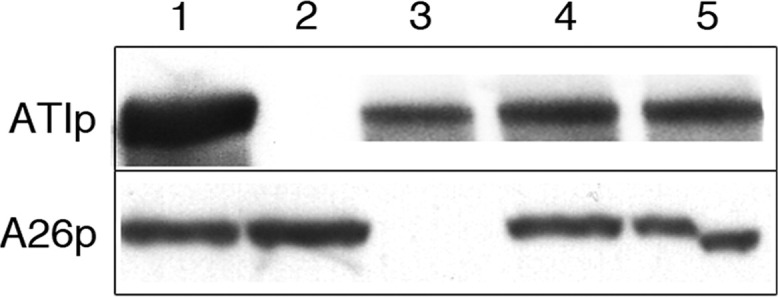
Western blot of cells infected with mutant viruses. BS-C-1 cells were infected with 5 PFU/cell of CPXV 91/3 (lane 1), ΔATI (lane 2), ΔA26 (lane 3), ATIRev (lane 4), A26Rev (lane 5). After 24 h, the cells were lysed and Western blots were prepared. Antibody to the ATI protein (ATIp) and the A26 protein (A26p) were used to detect the corresponding proteins.
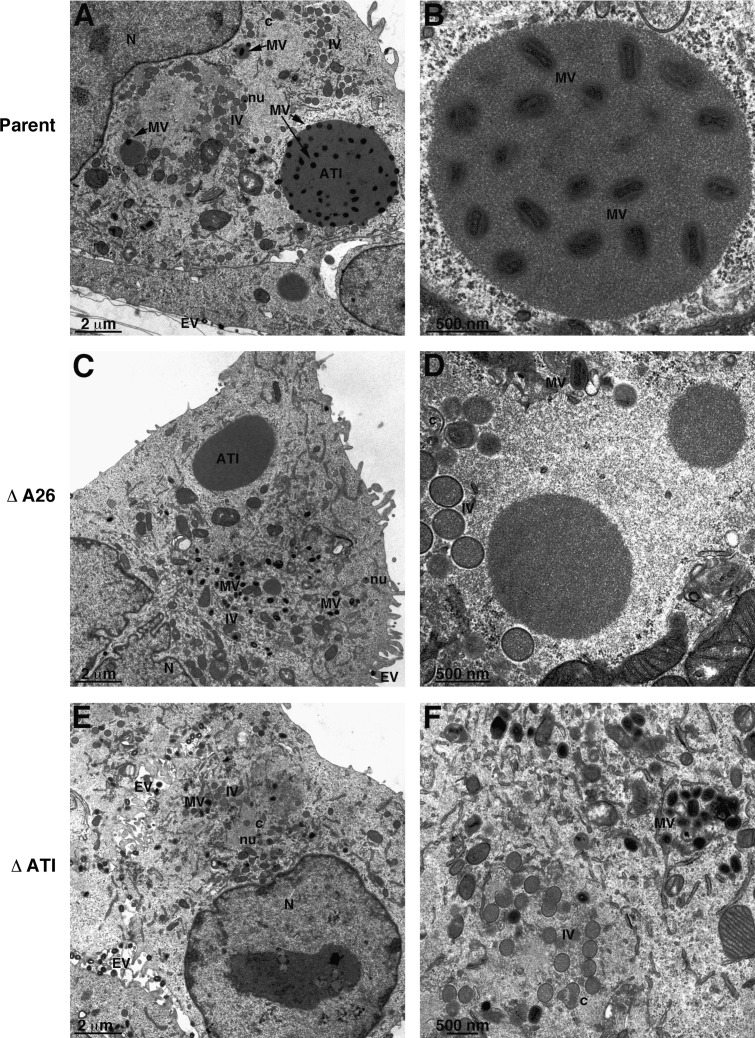
Electron microscopy of cells infected with CPXV 91/3 and mutants
The production of ATIs by the cloned parental virus was confirmed by transmission electron microscopy of thin cell sections ( Fig. 4A). Immature virus forms (including crescents, immature virions, and immature virions with nucleoids) and mature forms (including MVs and enveloped virions) were present. A higher magnification image of an ATI with embedded MVs is shown in Fig. 4B. ATI formed in cells infected with ΔA26, but no MVs were embedded even though they were present elsewhere in the cytoplasm (Fig. 4C and D). Immature and mature virions were found in cells infected with ΔATI, but no ATIs were detected (Fig. 4E and F). Thus, the mutants behaved precisely as predicted (McKelvey et al., 2002).
Fig. 4.
Transmission electron microscopy of cells infected with parental and mutant viruses. BS-C-1 cells were infected with CPXV 91/3 (A, B), ΔA26 (C, D) and ΔATI (E, F) for 18 h and thin sections were imaged by transmission electron microscopy. Abbreviations: MV, mature virion; IV, immature virion; Nu, IV with a nucleoid; c, crescent; N, nucleus. Magnifications are indicated at the bottom of each panel.
Replication of deletion mutants in cell culture
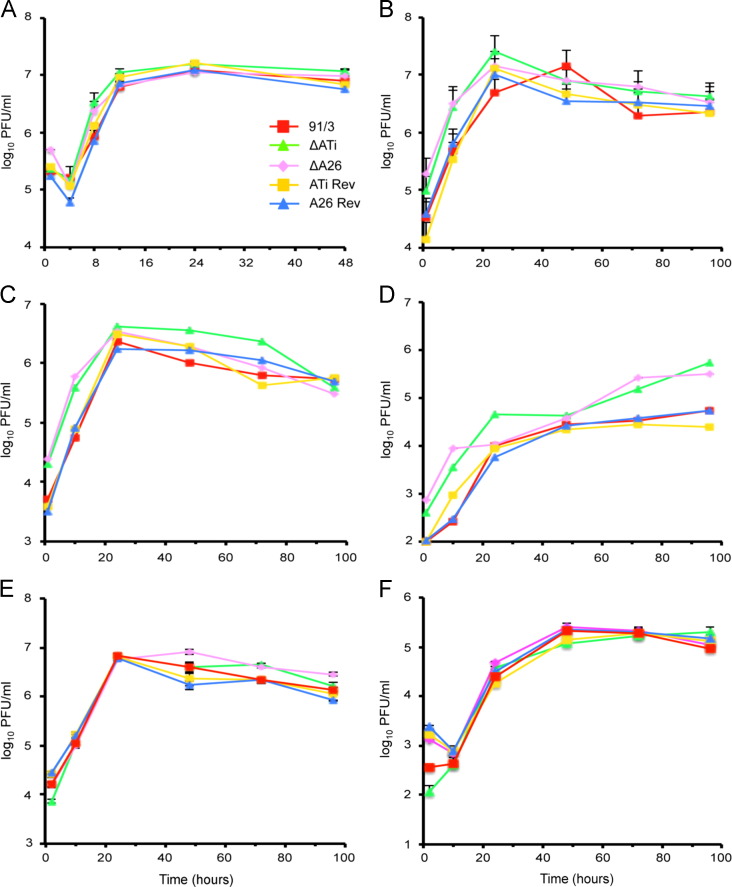
The replication of the two null mutants and revertants were similar during a single cycle infection of BS-C-1 cells ( Fig. 5A). Replication was also similar under low multiplicity infection conditions in which cell to cell spread could occur (Fig. 5B). The amounts of intracellular and extracellular virus after a low multiplicity infection of BS-C-1 (Fig. 5C and D) and mouse embryonic fibroblasts (MEFs; Fig. 5E and F) were also compared. Replication in MEFs was investigated in view of the mouse experiments described below. There was no consistent difference in either intracellular or extracellular titers of mutant and control viruses.
Fig. 5.
Replication of parental CPX 91/3, mutants and revertants in BS-C-1 cells and MEFs: (A) BS-C-1 cells were infected with 5 PFU/cell of parental 91/3 clone, ΔATI, ΔA26, ATIRev or A26Rev. At the indicated times, the cells were lysed and combined with the medium and virus titered. (B) BS-C-1 cells were infected with 0.05 PFU/cell of the indicated viruses and the cells and media were obtained at the indicated times and titered. (C, D) BS-C-1 cells were infected as in panel B but virus yields of cells alone and medium alone are shown in panels C and D, respectively. (E, F) MEFs were infected with 0.05 PFU/cell of the indicated viruses and virus yields of cells alone and medium alone are shown in panels E and F, respectively. Virus titers were obtained by plaque assay on BS-C-1 cells in duplicate from three separate infections (panels A, B, E, F) or two separate infections (panels C, D). Standard error bars (plus) are shown for panels A, B, E and F.
Pathogencity of deletion mutants in mice
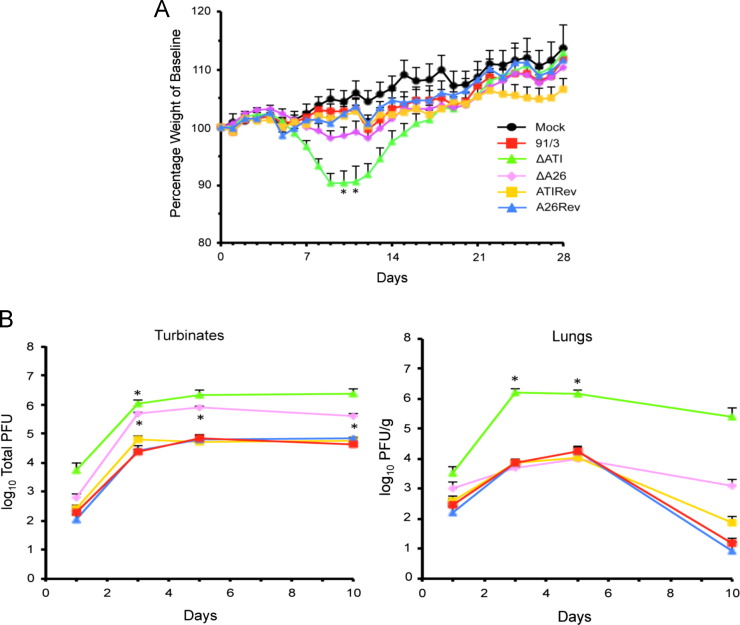
Mice infected i.n. with 106 PFU of parental CPX 91/3, mutant viruses or revertants exhibited signs of disease including hunched posture, piloerection and failure to groom. Weight loss data from two independent experiments were combined for Fig. 6A. During the second week, mice infected with ΔATI and ΔA26 exhibited more weight loss than the parental and revertant viruses but this was statistically significant only for ΔATI. There were no deaths and recovery including weight gain occurred between two and three weeks. A similar, statistically significant pattern of weight loss for ΔATI compared to the controls was obtained in a third independent experiment carried out for 10 days (data not shown) in conjunction with the organ titrations described below.
Fig. 6.
Virulence of CPXV mutant and revertant strains in mice: (A) weight loss comparison. BALB/cJ (5–7 weeks old) mice were inoculated i.n. with PBS (mock) or 106 PFU of the cloned CPXV 91/3, the two deletion mutants (ΔATI and ΔA26) and the two revertants (ATIRev and A26Rev). The weight loss data (average weight loss with standard error of the means) was generated from two independent experiments with a total of 15 mice and plus error bars are shown. The baseline used for calculation was obtained by weighing each mouse on the two successive days prior to infection. The asterisks indicate significant difference (p<0.05) between the weight loss of mice infected with ΔATI and each of the other viruses. (B) Virus titers in organs. Mice (n=5 per group) were infected as in panel A and sacrificed on days 1, 3, 5 and 10. The lungs and nasal turbinates were homogenized and the virus titers determined by plaque assay on BS-C-1 cells. The average titers (total for the turbinates and per gram for the lung) with standard error of the means were calculated and the plus bars are shown. For turbinates, asterisks on day 3 of ΔATI infection and 3, 5 and 10 of ΔA26 infection indicate significant differences (p<0.05) from CPXV 91/3, ATIRev and A26Rev. For lungs, asterisks on days 3, 5 and 10 of ΔATI infection indicate significant differences (p<0.05) from CPXV 91/3, ATIRev, A26Rev and ΔA26.
We also determined the extent of virus replication in the nasal turbinates and lungs after i.n. infection of BALB/c mice with 106 PFU of each mutant and the three control viruses. Groups of mice were sacrificed on day 1, 3, 5 and 10 and virus titers in the nasal turbinates and lungs were determined by plaque assay. With each virus, replication in the turbinates increased during the first 3–5 days and then plateaued (Fig. 6B). The titers of the clonal parent 91/3 and the two revertants were nearly superimposable. The titers of both deletion mutants were higher than the control viruses (p<0.05) but were not significantly different from each other.
The lung titers of the clonal parent and the two revertants were also nearly superimposable, increasing up to day 5 and then declining (Fig. 6B). In contrast, the ΔATI lung titers were significantly higher (p<0.05) than the controls and were still three logs higher on day 10. In the experiment depicted in Fig. 5B, the ΔA26 lung titers were not significantly different from the controls. In an independent experiment (not shown), the ΔATI lung titers were significantly higher than the parental virus and ΔA26; however, the ΔA26 lung titers were also significantly higher than the parental virus. Other organs titered (liver, brain, spleen and ovary) had no or few PFUs for any of the infections (data not shown). Overall, the replication of the viruses in mice were as follows: ΔATI>ΔA26>ATIRev=A26Rev=91/3.
Discussion
Why some species of orthopoxviruses embed virions in dense proteinaceous bodies and others do not have been subject to speculation. It is reasonable to consider that the ATI provides protection in the environment and that this contributes to the survival of the species. This strategy would be particularly important if the host population were sparse, host-to-host spread was inefficient or a host species became locally extinct. However, ATI may be unnecessary and even disadvantageous at least in the short term for orthopoxviruses such as variola virus, the agent of smallpox, that rely on respiratory spread in dense communities. To test this hypothesis, we obtained a recently isolated CPXV strain and demonstrated that it made ATIs with embedded virions and produced relatively mild disease in mice by the i.n. route. Mutants were constructed with a deletion of the gene encoding the ATI protein or the VACV A26 homolog that is required for embedding virions (McKelvey et al., 2002). In addition, revertant viruses were constructed to use as controls. Care was taken to avoid effects on neighboring genes and a reporter gene, used for initial isolation of the mutants, was removed at the final construction step. Consequently, we could infer that phenotypic changes were due to the gene deletions exclusively. Electron microscopy confirmed that the ATI gene deletion virus made no inclusions and that the A26L gene deletion virus made inclusions but did not embed MVs. To determine total yields of virus, the infected cell lysates and medium were sonicated to disperse virus particles. Plaque assays indicated similar replication of the mutants, parental virus and revertants in monkey BS-C-1 cells and MEFs.
Although CPXV may spread from rodents to other animals via skin lesions, we were interested in respiratory spread for the reason outlined above. The i.n. route of infection has previously been used to assess CPXV pathogenicity (Bray et al., 2000, Smee et al., 2008, Thompson et al., 1993). CPXV 91/3 caused only a mild disease when administered i.n. to BALB/c mice as also recently found by others using a different mouse strain (Duraffour et al., 2013). However, mice inoculated i.n. with ΔATI lost significantly more weight by days 10 and 11 than mice inoculated with the parent or revertant. The ΔA26 mutants caused slightly more weight loss than the controls but this did not reach significance at the dose (106 PFU) used. In addition, more virus was recovered from the nasal turbinates of both mutants compared to the parent and revertant viruses. The lungs of animals infected with ΔATI contained more virus than those infected with control viruses or ΔA26, corresponding to the greater weight loss of the ΔATI mutant. These results were consistent with our hypothesis that forming ATI and embedding virions might be disadvantageous for animals that are infected by the respiratory route. To dispel dual-use concerns, we point out that ATI mutants occur spontaneously during propagation of CPXV in cell culture (Amano and Tagaya, 1981) and the 91/3 ATI mutant caused no deaths in BALB/c mice at 106 PFU whereas the commonly used Brighton strain of CPXV has a LD50 of 2 × 105 PFU.
Leite and coworkers (Leite et al., 2011) constructed and characterized an ATI deletion mutant of the Brighton strain of CPXV. There are several important differences between their study and ours. First, since the Brighton strain has a disrupted A26R ORF, their parental virus would be comparable to our A26R deletion mutant and their ATI mutant would be equivalent to a double ATI/A26R deletion, which we did not make. Second, in the earlier study, pathogenicity was evaluated following an intradermal injection of 105 PFU into the ear pinna, rather than by a respiratory route. The skin lesions produced by the ATI deletion mutant had a smaller area of necrosis that healed faster than those of the parent virus, and had more inflammatory cells. More virus was recovered from ear pinnae of the parent virus than the ATI deletion mutant on days 5 and 8 and less virus on day 11, although there was no correlation between lesion severity and virus titer. The authors (Leite et al., 2011) suggested that an immune response to the ATI protein may account for the greater necrosis.
We considered several explanations to account for the increased virus replication in mice infected i.n. with ΔATI and ΔA26 CPXV mutants. It seems likely that virions embedded in the dense ATI would be less infectious within a host than free MVs. Even a small increase in virus spread, not readily detected in cell culture, over multiple rounds of infection in an animal might significantly enhance virulence. However, if that were the sole effect, then one might expect the ΔATI and ΔA26 mutants to be equivalent. The apparently greater virulence of the ATI mutant suggests that additional factors may have a role for ΔA26. It is known that the A26 protein has multiple functions. For example, A26 on MVs binds to the extracellular protein laminin to enhance attachment to some cells (Chiu et al., 2007) and to the A27 protein (Ching et al., 2009, Howard et al., 2008), which binds to glycosaminoglycans to mediate cell attachment (Ching et al., 2009, Chung et al., 1998). The A26 protein may also regulate fusion of viral and cell membranes (Chang et al., 2010, Chang et al., 2012). Thus, additional roles for A26 may attenuate the otherwise positive effect of the deletion and may account for its preservation in all orthopoxvirus species. Another possibility to account for the greater replication of the ΔATI than ΔA26 is that synthesis of the abundant ATI protein consumes resources that could be used for synthesis of other proteins in its absence. Purified ATIs are immunogenic (Patel et al., 1986), but whether antibody or cell mediated immune responses to ATI during an infection contributes to clearing of virus is unknown.
In conclusion, our hypothesis that deletion of the ATI gene enhances orthopoxvirus respiratory infections was supported by studies of CPXV infection of mice. This advantage could have provided selective pressure during the evolution of variola virus in humans and monkeypox virus in rodents.
Materials and methods
Virus
CPXV_GER1991_3 (abbreviated CPXV 91/3) (Carroll et al., 2011), kindly provided by H. Meyer, was propagated in BS-C-1 or HeLa cells grown in Earle's minimal essential media (EMEM) supplemented with 2 mM glutamine, 100 µg/ml streptomycin, 100 U/ml penicillin, and 2% fetal bovine serum.
Construction of virus mutants by recombination
PCR products containing GFP regulated by the P11 late promoter flanked by 400–500 bp of DNA corresponding to the sequences flanking the ATI and A26R ORFs of CPXV 91/3 were prepared by standard methods. HeLa or BS-C-1 cells were infected with 0.05 PFU/cell of CPXV 91/3 and 2 h later were transfected with the PCR products complexed with lipofectamine 2000 in Optimem medium (Invitrogen). The Optimem was replaced with EMEM without antibiotics or serum after an additional 6 h. The cells were harvested and lysed after 2 days and dilutions were plated on BS-C-1 cells, which were overlaid with agar. Virus was isolated from fluorescent plaques and the procedure was repeated until the virus was clonally pure. The next step was to delete GFP by recombination, with the same ATI or A26L flanking sequences used above, to create the null mutants ΔATI and ΔA26 without an exogenous reporter gene. In addition, revertant viruses were made by replacing GFP with the original ATI or A26L ORFs. PCR and DNA sequencing were used to confirm clonal purity.
Virus yields
BS-C-1 cells and MEFs were infected at a multiplicity of 5 or 0.05 PFU/cell as indicated in figure legends. After 1.5 h, the cells were washed twice with phosphate buffered saline and fresh medium was added. Cells were collected by scraping and resuspending them in the culture medium and lysed by three freeze and thaw cycles with vortexing. In other experiments, the cells and medium were collected separately. Tubes containing the lysates were immersed in wet ice in a bath sonicator and pulsed three times. Virus titers were determined by diluting duplicates in supplemented EMEM and plaque titration on BS-C-1 cells. After a 2 h adsorption, the cells were overlaid with medium containing methylcellulose. Cells were stained with crystal violet after 2 days and plaques were counted. Statistical analysis was done using Prism with 2-way ANOVA with multiple comparisons and Tukey's correction for multiple comparisons with significance set at values less than 0.05.
Western blotting
BS-C-1 cells were infected with 5 PFU/cell of virus. After 24 h the cells were resuspended in 2× NuPage lithium dodecyl sulfate loading buffer with 1× reducing agent (Invitrogen). The lysates were dispersed by sonication, heated at 70 °C and loaded on a 4–12% Bis-Tris sodium dodecyl sulfate polyacrylamide gel in NuPage morpholinepropanesulfonic acid running buffer (Invitrogen). Proteins were transferred electrophoretically to a nitrocellulose membrane (Invitrogen iBLOT) and detected with either polyclonal antibody to an A26 peptide or antiATI polyclonal antibody (McKelvey et al., 2002) received from D. Pickup (Duke University) and anti-rabbit IgG conjugated with peroxidase (Thermo Scientific). Blots were developed using the Femto detection system.
Confocal microscopy
HeLa cells adhered to cover slips were infected with 5 PFU/cell for 36 h and fixed with 4% paraformaldehyde and permeabilized with 0.1% Triton X-100. Primary staining was performed using antiA26 and antiATI polyclonal antibody (McKelvey et al., 2002), and mouse antiA14 MAb (Meng et al., 2011). Secondary staining was with anti-rabbit IgG and anti-mouse IgG (Invitrogen). Coverslips were stained with DAPI and mounted on glass slides using Prolong Gold mounting media (Invitrogen). Images were acquired using a Leica SP2 inverted four-channel microscope.
Electron microscopy
BS-C-1 cells in 60 mm diameter plates were infected with virus at 5 PFU/cell and incubated for 21 h prior to fixation with 2% glutaraldehyde/0.1 M sodium cacodylate buffer, washed in 0.1 M sodium cacodylate buffer, post-fixed with reduced osmium tetroxide, and washed in buffer. Cells were dehydrated in a series of ethyl alcohol: 50%, 70%, 100% and then propylene oxide. The samples were embedded in EMbed 812 and sections were cut on a Leica EM UC7 ultramicrotome (Leica Microsystems Inc., Buffalo Grove, IL). Thin sections were stained with 7% uranyl acetate in 50% ethanol and then 0.01% lead citrate. Sections were reviewed and photographed on the Tecnai G2 Spirit transmission electron microscope (FEI, Hillsboro, Oregon) fitted with a Gatan CCD camera. Chemicals were purchased from Electron Microscopy Sciences (EMS), Hatfield, PA.
Mouse infection and necropsy
Virus was purified from infected cell lysates by sedimentation through a 36% sucrose cushion. Groups (n=5–10) of 7-week old BALB/c mice were anesthetized with isoflurane and infected i.n. with 10 µl of virus diluted in phosphate buffered saline with 0.05% bovine serum albumin. Mock-infected mice were anesthetized and inoculated with 10 µl of the diluent. Mice were weighed daily for 2 days before infection and each day after infection. Weight loss was analyzed for significance using PRISM 2-way ANOVA with Tukey's correction for multiple comparisons. Mice were sacrificed by carbon dioxide and cervical dislocation for necropsy and collection of the spleen, ovary, liver, lung, cervical lymph nodes, brain, and nasal turbinates. Tissues collected were placed in a balanced salt solution containing 0.1% bovine serum albumin, weighed, and stored at −80 °C. The organs, were thawed, homogenized with a tissue grinder and sonicated on ice. Dilutions were made in supplemented EMEM and a plaque assay was performed on BS-C-1 cells. Statistical analysis of tissue viral titers was conducted using PRISM multiple t-tests with Sidak-Bonferroni correction for multiple comparisons.
Acknowledgments
We thank Catherine Cotter for help with cell culture and Linda Wyatt for discussions. Herman Meyer and David Pickup kindly provided CPXV_GER1991_3 and antibody to the ATI protein, respectively. The research was supported by the Division of Intramural Research, NIAID, NIH.
References
- Amano H., Tagaya I. Isolation of cowpox virus clones deficient in production of type A inclusions: relationship to the production of diffusible LS antigen. J. Gen. Virol. 1981;54:203–237. doi: 10.1099/0022-1317-54-1-203. [DOI] [PubMed] [Google Scholar]
- Bergoin M., Devauchelle G., Vago C. Electron microscopy study of Melolontha poxvirus: the fine structure of occluded virions. Virology. 1971;43:453–467. doi: 10.1016/0042-6822(71)90317-5. [DOI] [PubMed] [Google Scholar]
- Bray M., Martinez M., Smee D.F., Kefauver D., Thompson E., Huggins J.W. Cidofovir protects mice against lethal aerosol or intranasal cowpox virus challenge. J. Infect. Dis. 2000;181:10–19. doi: 10.1086/315190. [DOI] [PubMed] [Google Scholar]
- Carroll D.S., Emerson G.L., Li Y., Sammons S., Olson V., Frace M., Nakazawa Y., Czerny C.P., Tryland M., Kolodziejek J., Nowotny N., Olsen-Rasmussen M., Khristova M., Govil D., Karem K., Damon I.K., Meyer H. Chasing Jenner’s vaccine: revisiting cowpox virus classification. Plos One. 2011;6:e23086. doi: 10.1371/journal.pone.0023086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang S.J., Chang Y.X., Izmailyan R., Tang Y.L., Chang W. Vaccinia virus A25 and A26 proteins are fusion suppressors for mature virions and determine strain-specific virus entry pathways into HeLa, CHO-K1, and L cells. J. Virol. 2010;84:8422–8432. doi: 10.1128/JVI.00599-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang S.J., Shih A.C., Tang Y.L., Chang W. Vaccinia mature virus fusion regulator A26 protein binds to A16 and G9 proteins of the viral entry fusion complex and dissociates from mature virions at low pH. J. Virol. 2012;86:3809–3818. doi: 10.1128/JVI.06081-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching Y.C., Chung C.S., Huang C.Y., Hsia Y., Tang Y.L., Chang W. Disulfide bond formation at the C termini of vaccinia virus A26 and A27 proteins does not require viral redox enzymes and suppresses glycosaminoglycan-mediated cell fusion. J. Virol. 2009;83:6464–6476. doi: 10.1128/JVI.02295-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu W.L., Lin C.L., Yang M.H., Tzou D.L. M., Chang W. Vaccinia virus 4c (A26L) protein on intracellular mature virus binds to the extracellular cellular matrix laminin. J. Virol. 2007;81:2149–2157. doi: 10.1128/JVI.02302-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung C.-S., Hsiao J.-C., Chang Y.-S., Chang W. A27L protein mediates vaccinia virus interaction with cell surface heparin sulfate. J. Virol. 1998;72:1577–1585. doi: 10.1128/jvi.72.2.1577-1585.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damon I. In: Sixth ed. Knipe D.M., Howley P.M., editors. vol. 2. Wolters Kluwer/Lippincott Williams & Wilkins; Philadelphia: 2013. Poxviruses; pp. 2160–2184. (Fields Virology). (2 vols) [Google Scholar]
- Downie A.W. A study of the lesions produced experimentally by cowpox virus. J. Pathol. Bact. 1939;48:361–379. [Google Scholar]
- Duraffour S., Mertens B., Meyer H., van den Oord J.J., Mitera T., Matthys P., Snoeck R., Andrei G. Emergence of cowpox: study of the virulence of clinical strains and evaluation of antivirals. Plos One. 2013;8:e55808. doi: 10.1371/journal.pone.0055808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funahashi S., Sato T., Shida H. Cloning and characterization of the gene encoding the major protein of the A-type inclusion body of cowpox virus. J. Gen. Virol. 1988;69:35–47. doi: 10.1099/0022-1317-69-1-35. [DOI] [PubMed] [Google Scholar]
- Goodpature E.W., Woodruff C.E. A comparison of the inclusion bodies of fowlpox and Molluscum contagiosum. Am. J. Pathol. 1931;7:1–7. [PMC free article] [PubMed] [Google Scholar]
- Howard A.R., Moss B. Formation of orthopoxvirus cytoplasmic A-type inclusion bodies and the embedding of virions are dynamic processes requiring microtubules. J. Virol. 2012;86:5905–5914. doi: 10.1128/JVI.06997-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard A.R., Senkevich T.G., Moss B. Vaccinia virus A26 and A27 proteins form a stable complex tethered to mature virions by association with the A17 transmembrane protein. J. Virol. 2008;82:12384–12391. doi: 10.1128/JVI.01524-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato S., Takahashi M., Kameyama S., Kamahora J. A study on the morphological and cyto-immunological relationship between the inclusions of variola, cowpox, rabbitpox, vaccinia (variola origin) and vaccinia IHD, and a consideration of the term “Guarnieri body“. Biken’s J. 1959;2:353–363. [Google Scholar]
- Leite J.A., da Fonseca F.G., Trindade G.D., Abrahao J.S., Arantes R.M. E., de Almeida-Leite C.M., dos Santos J.R., Guedes M., Ribeiro B.M., Bonjardim C.A., Ferreira P.C.P., Kroon E.G. A-type inclusion bodies: a factor influencing cowpox virus lesion pathogenesis. Arch. Virol. 2011;156(617–628) doi: 10.1007/s00705-010-0900-0. [DOI] [PubMed] [Google Scholar]
- Marchal J. Infectious ectromelia. A hitherto undescribed virus disease of mice. J. Pathol. Bacteriol. 1930;33:713–728. [Google Scholar]
- McKelvey T.A., Andrews S.C., Miller S.E., Ray C.A., Pickup D.J. Identification of the orthopoxvirus p4c gene, which encodes a structural protein that directs intracellular mature virus particles into A-type inclusions. J. Virol. 2002;76:11216–11225. doi: 10.1128/JVI.76.22.11216-11225.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng X., Zhong Y., Embry A., Yan B., Lu S., Zhong G., Xiang Y. Generation and characterization of a large panel of murine monoclonal antibodies against vaccinia virus. Virology. 2011;409:271–279. doi: 10.1016/j.virol.2010.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss B. In: sixth ed. Knipe D.M., Howley P.M., editors. vol. 2. Wolters Kluwer/Lippincott Williams &Wilkins; Philadelphia: 2013. Poxviridae; pp. 2129–2159. (Fields Virology). (2 vols.) [Google Scholar]
- Patel D.D., Pickup D.J. Messenger RNAs of a strongly-expressed late gene of cowpox virus contains a 5'-terminal poly(A) leader. EMBO J. 1987;6:3787–3794. doi: 10.1002/j.1460-2075.1987.tb02714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel D.D., Pickup D.J., Joklik W.K. Isolation of cowpox virus A-type inclusions and characterization of their major protein component. Virology. 1986;149:174–189. doi: 10.1016/0042-6822(86)90119-4. [DOI] [PubMed] [Google Scholar]
- Smee D.F., Gowen B.B., Wandersee M.K., Wong M.H., Skirpstunas R.T., Baldwin T.J., Hoopes J.D., Sidwell R.W. Differential pathogenesis of cowpox virus intranasal infections in mice induced by low and high inoculum volumes, and effects of cidofovir treatment. Int. J. Antimicrob. Agents. 2008;31:352–359. doi: 10.1016/j.ijantimicag.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson J.P., Turner P.C., Ali A.N., Crenshaw B.C., Moyer R.W. The effects of serpin gene mutations on the distinctive pathobiology of cowpox and rabbitpox virus following intranasal inoculation of Balb/c mice. Virology. 1993;197:328–338. doi: 10.1006/viro.1993.1594. [DOI] [PubMed] [Google Scholar]