Abstract
Objective
Identify clinical conditions associated with a large increase (spike) in the heart rate characteristics index in VLBW infants.
Study design
Retrospective medical record review within a day of all large heart rate characteristics index spikes (increase of ≥3 from prior 5 day average) in VLBW infants at a single center enrolled from 2007–2010 in a multicenter trial of heart rate characteristics monitoring. In the trial, infants were randomized to having their heart rate characteristics index displayed to clinicians or not displayed.
Results
Of 274 eligible infants, 224 large heart rate characteristics spikes occurred in 105 infants. Thirty-three spikes were associated with surgery or procedures requiring anesthetic or anticholinergic medications, and infection-related conditions were the most common clinical association with the other spikes. Of the first spikes in 47 infants randomized to conventional monitoring (heart rate characteristics index not displayed to clinicians), 53% were associated with suspected or proven infection. Respiratory deterioration without suspected infection occurred with 34%, and no association was identified in 13%. Infants randomized to having their heart rate characteristics index displayed were more likely to have antibiotics initiated around the time of a large heart rate characteristics index spike.
Conclusions
Sepsis, other infectious or systemic inflammatory conditions, respiratory deterioration, and surgical procedures are the most common clinical associations with a large increase in the heart rate characteristics index in VLBW infants. This information may improve use of heart rate characteristics monitors in NICU patients.
Abnormal heart rate characteristics (heart rate characteristics) of decreased variability and transient decelerations occur in preterm infants with sepsis, often before any clinical signs are recognized(1). This observation led to the development of a monitor that displays heart rate characteristics as an index representing the fold-increase in risk of clinical deterioration from sepsis in the next 24 hours (2–3). A mathematical algorithm uses electrocardiogram signals from standard bedside monitors in the neonatal intensive care unit (NICU) to continuously calculate and display the heart rate characteristics index, which reflects heart rate variability (normal small accelerations and decelerations) and presence of larger-than-normal decelerations occurring over the previous 12 hours(4–7). The heart rate characteristics index added to laboratory tests(8) and clinical signs(9) for diagnosis of sepsis. Displaying infants’ heart rate characteristics index to clinicians reduced mortality in a randomized clinical trial of 3003 very low birth weight (VLBW) infants(10).
Abnormal heart rate characteristics may occur in sepsis or in other conditions that cause disturbances in autonomic nervous system function (5, 11–14). Heart rate is controlled by sympathetic (norepinephrine) and parasympathetic (acetylcholine) signaling to cardiac pacemaker cells, leading to frequent small accelerations and decelerations in rate, respectively(15). Sepsis leads to decreased heart rate variability, usually represented as low standard deviation of inter-heartbeat time intervals, in part through effects of cytokines released during a systemic inflammatory response(16). Transient decelerations of heart rate also occur in infants with sepsis, sometimes in association with apnea, and sometimes during regular spontaneous breathing or mechanical ventilation. Vagus nerve firing is one cause of these heart rate decelerations(17). Pathophysiologic conditions other than sepsis may lead to a systemic inflammatory response or altered autonomic nervous system function. In our prior work we have reported increases in the heart rate characteristics index (reflecting low heart rate variability and/or transient decelerations) in NICU patients with urinary tract infection(5) , necrotizing enterocolitis(18), respiratory deterioration leading to intubation(19) and following surgical or other procedures requiring administration of anesthetic or anticholinergic medications(20–21).
Optimizing the clinical utility of heart rate characteristics monitoring requires that clinicians understand the various clinical conditions associated with abnormal heart rate characteristics. Toward this goal, the aim of the current study was to quantify the occurrence of and clinical conditions associated with all abrupt, large increases (spikes) in the heart rate characteristics index in VLBW infants at the University of Virginia NICU enrolled in the multicenter randomized trial of heart rate characteristics monitoring.
Methods
We performed a retrospective medical record review of clinical events around the time of large heart rate characteristics index spikes in VLBW (<1500g birth weight) infants. We included all VLBW infants at the University of Virginia NICU during a 3-year period (2007–2010) enrolled in the multicenter clinical trial of heart rate characteristics index monitoring (HeRO study). In the trial, infants were randomized to having their heart rate characteristics index displayed to clinicians or to conventional monitoring only (heart rate characteristics index recorded but not displayed). Clinicians were instructed about how the monitor was developed and were encouraged to evaluate infants whose heart rate characteristics index was rising, but there were no mandated interventions for a specific score or rate of rise. Results of the clinical trial, in which 3003 VLBW infants in 9 NICUs underwent continuous heart rate characteristics index monitoring, were published in 2011(10). The Institutional Review Board approved the RCT, which required parental consent, and this retrospective review.
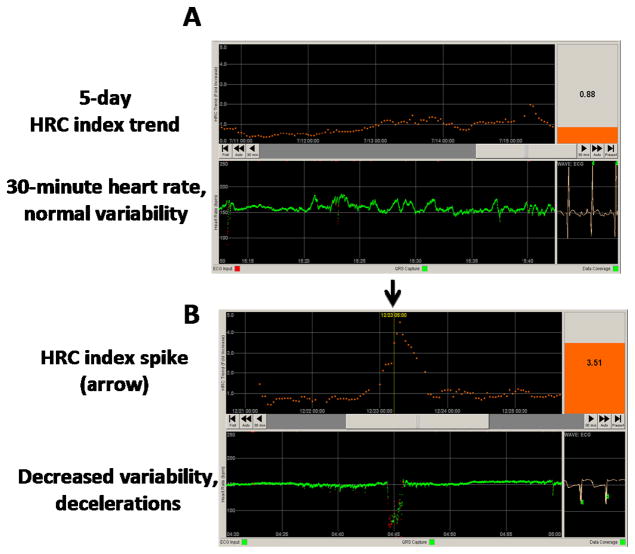
The heart rate characteristics index monitor (HeRO, Medical Predictive Science Corporation, Charlottesville, Virginia) uses existing electrocardiogram or heart rate data from standard bedside monitors to calculate the heart rate characteristics index, which is derived from an externally validated logistic regression calculation that relates decreased HR variability and transient HR decelerations to the fold increased risk over baseline risk that an infant will be diagnosed with sepsis in the next 24 hours. The monitor displays each infant’s current heart rate characteristics index, which is updated every hour and represents heart rate characteristics over the previous 12 hours, and also displays the 5-day heart rate characteristics index trend (Figure 1).
Figure 1. heart rate characteristics index monitor showing normal and abnormal heart rate characteristics.
The heart rate characteristics monitor analyzes electrocardiogram signals from bedside monitors for abnormal heart rate characteristics of decreased variability and transient decelerations and presents a number which is the fold increased risk an infant will experience a clinical deterioration consistent with sepsis in the next 24 hours. The monitor displays the last 5 days of the heart rate characteristics index (top, orange) and the last 30 minutes of heart rate (bottom, green, beats per minute). A) Normal heart rate characteristics reflected by a low heart rate characteristics index. The current index, 0.88, is shown in the top right panel, and the 5-day trend is generally <1 with a small transient rise to 2. B) Large transient rise (“spike”) in the heart rate characteristics index from baseline <1 to 3.51 at the arrow, reflecting decreased heart rate variability and transient decelerations.
We analyzed hourly heart rate characteristics index values and identified all large, abrupt increases in the heart rate characteristics index (“spikes”), defined as an increase in magnitude of at least 3 compared with the prior 5-day average, excluding the 12 hours before the peak (Figure 1, B). Spikes were excluded if they occurred within 5 days of a previous large spike or if there were not at least 24 hours of heart rate characteristics index baseline data prior to the spike.
Medical records were reviewed for birth weight, gestational age, and day of age at the time of the spike. Progress notes were reviewed on the day of the spike and the day before and after for descriptions of clinical status and events. Surgical or other procedures involving anesthetic or anticholinergic administration, including therapy for retinopathy of prematurity, were recorded. Dates of antibiotic administration and results of cultures and complete blood counts and leukocyte differential within 24h of the spike were collected. Infants who had antibiotics initiated or changed within a day of the spike were further classified as having septicemia (signs of sepsis, blood culture positive and at least 5 days of antibiotics), clinical sepsis (signs of sepsis, negative cultures and at least 5 days of antibiotics), or sepsis ruled out (signs of sepsis, negative cultures and <5 days of antibiotics). Urinary tract infection was defined as a positive urine culture for which clinicians decided to continue antibiotics at least 5 days. Necrotizing enterocolitis was defined as clinical and radiographic signs consistent with Bell’s stage II or III NEC. For infants who did not have antibiotics started or changed within a day of the spike, indications of respiratory deterioration were recorded. Respiratory deterioration was defined as a 50% increase in number of documented apnea events, supplemental oxygen, or ventilator support over the infant’s prior 24h baseline.
Two clinicians independently reviewed medical records and assigned a clinical association to each spike. There was 80% agreement on the above designations on independent chart review by two clinicians and 100% agreement after joint review.
Because it was possible to have more than one clinical event temporally associated with the heart rate characteristics index spike, we established the following hierarchy of associations: (1) surgery or procedure requiring anesthetic or anticholinergic medication; (2) antibiotics initiated or changed for a suspected infection-related condition (further classified based on culture results and antibiotic duration); (3) respiratory deterioration, no antibiotics initiated; and (4) unknown (including infants already on antibiotics with no change in agent within a day of the spike)
Continuous variables were assessed by Student T test and categorical variables by Fisher exact test. Mean and standard deviation are given, unless otherwise indicated. Statistical analyses were performed in GraphPad Prism (GraphPad Software, San Diego, CA) with two-tailed significance set at p<0.05
RESULTS
Of 274 infants enrolled in the heart rate characteristics monitoring randomized clinical trial at the University of Virginia from 2007–2010, 224 large heart rate characteristics index spikes occurred in 105 infants (38%). Gestational age of infants with spikes was 25.8 ± 2.1 weeks (mean, SD) and birth weight 828 ± 228 grams. Infants without spikes were of significantly higher gestational age and birth weight (28.9 ± 2.9 weeks, p< 0.001 and 1082 ± 281g, p<0.001). Fifty-two infants had a single spike, 43 had 2–4, and 10 had 5 or more spikes. Mortality before NICU discharge of infants with and without large heart rate characteristics index spikes was 12% (16/138) and 7% (9/136) (p=0.45), and mortality within 30 days of a large spike was 9% (5/53) for infants with heart rate characteristics index displayed and 12% (6/52) for non-display infants (p=0.76).
Heart rate characteristics spikes associated with surgical procedures
Because anesthetic and anticholinergic medications are known to acutely and transiently decrease heart rate variability(22), we first investigated whether spikes in the heart rate characteristics index followed a surgical procedure. Thirty-three of the 224 spikes occurred within a day following a surgical or other procedure for which anesthetic and/or anticholinergic agents were given (6 laser photoablation for retinopathy of prematurity, 7 ligation of patent ductus arteriosus, 14 gastrointestinal surgery, 3 ventricular shunt for post-hemorrhagic hydrocephalus, and 3 intubation and anesthesia for miscellaneous procedures).
Comparison of spikes in heart rate characteristics display versus non-display infants
Of the 191 spikes unrelated to surgery, 89 occurred in 47 infants randomized to having their heart rate characteristics index displayed, and 102 in 47 infants with conventional monitoring only (Table I). Birth weight and estimated gestational age were similar in the two groups. The median age at first spike in the display infants was 20 days (interquartile range13–34) compared with 16 days (12–23) in the non-display infants (p=0.02). For all spikes, the median age was 33 days (19–55) in display and 26 days (16–41) in non-display infants (p=0.05).
Table 1.
Clinical associations with large HRC index spikes not associated with surgical procedures, based on randomization to HRC display or non-display
| HRC Display (89 spikes) | Non-Display (102 spikes) | p= | |
|---|---|---|---|
| Infants with spikes, n (% of all infants) | 47 (34.1%) | 47 (34.6%) | 1.0 |
| Spikes per infant | 1.9 ± 1.3 | 2.2 ± 1.8 | 0.40 |
| Gestational age, weeks | 25.8 ± 2.3 | 25.8 ± 2.0 | 0.64 |
| Birth weight, grams | 831 ± 238 | 825 ± 220 | 0.85 |
| Day of age at spike, median (IQR) | 33 (19–55) | 26 (16–41) | 0.05 |
| Antibiotics started | 63/89 (71%) | 45/102 (44%) | <0.001 |
| Sepsis, blood culture positive | 10 | 10 | 0.81 |
| Sepsis, clinical | 22 | 14 | 0.06 |
| Sepsis ruled out | 19 | 9 | 0.02 |
| Urinary tract infection | 5 | 4 | 0.74 |
| Necrotizing enterocolitis | 5 | 6 | 1.00 |
| Other infection | 2 | 2 | 1.00 |
| Total antibiotic days during NICU stay | 31.4 ± 23.9 | 25.7 +/− 20.3 | 0.21 |
Infection was suspected and antibiotics started within a day of the spike in 71% of infants in the heart rate characteristics index display compared with 44% of infants in the non-display group (p=<0.001; Table I). Sepsis was ruled out in significantly more infants in the display than in the non-display group (19 vs. 9, p=0.02). The total number of days on antibiotics for display and non-display infants in the 120 days in the NICU after randomization was 31.4 +/− 23.9 versus 25.7 +/− 20.3 days (p = 0.21).
Laboratory tests may be used in decisions about antibiotic therapy in infants with non-specific signs, and we found that complete blood counts were more likely to be performed within 24h of a spike in infants with heart rate characteristics index displayed (CBC performed in 85% of spikes in heart rate characteristics display versus 56% of spikes in non-display, p<0.01). The immature:total neutrophil ratio was significantly higher in infants with antibiotics initiated in both groups, and lower in those with sepsis subsequently ruled out than in those with clinical or culture-positive sepsis or NEC (Table II).
Table 2.
Immature:total neutrophil ratio within 24h of HRC index spike
| I:T HRC Display | I:T Non-Display | |
|---|---|---|
| All | 0.16 ± 0.15 | 0.19 ± 0.21 |
| Antibiotics started | 0.18 ± 0.16 | 0.22 ± 0.24 |
| Sepsis, blood culture positive | 0.26 ± 0.20 | 0.24 ± 0.25 |
| Clinical sepsis | 0.17 ± 0.10 | 0.26 ± 0.23 |
| Sepsis ruled out | 0.11 ± 0.10 | 0.09 ± 0.08 |
| Other infection or NEC | 0.23 ± 0.20 | 0.27 ± 0.26 |
| Antibiotics not started | 0.07 ± 0.07* | 0.10 ± 0.05** |
| No association | 0.10 ± 0.07 | 0.14 ± 0.19 |
| Respiratory deterioration | 0.03 ± 0.03 | 0.08 ± 0.05 |
p < 0.01 versus antibiotics started HRC display
p = 0.06 versus antibiotics started non-display
Clinical correlations of spikes in heart rate characteristics non-display infants
Display of an infant’s heart rate characteristics index to clinicians is likely to affect management decisions. We therefore analyzed clinical correlations of large heart rate characteristics index spikes in the 47 patients randomized to conventional monitoring (clinicians blinded to the heart rate characteristics index). Considering only the first spike for each of these infants, infection-related conditions (culture-positive, clinical, or suspected sepsis, urinary tract infection, or necrotizing enterocolitis) were temporally associated with 53% (Figure 2). Considering all 102 spikes in the non-display infants, 44% were associated with suspected or proven infection or NEC.
Figure 2. Clinical correlations of the first non-surgical heart rate characteristics index spike in non-display infants.
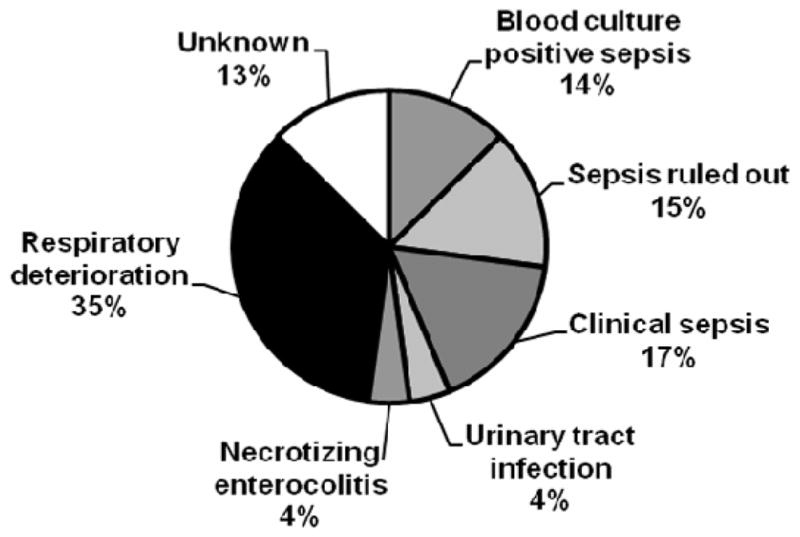
Forty-seven very low birth weight infants with the heart rate characteristics index continuously monitored but not displayed to clinicians had at least one large heart rate characteristics index spike of 3 over the prior 5 day average that was not associated with a surgical procedure. Clinical associations with the first spike were blood culture positive sepsis, sepsis suspected but ruled out (negative cultures, <5 days antibiotics), clinical sepsis (negative cultures, >5 days antibiotics), urinary tract infection, necrotizing enterocolitis, and respiratory deterioration without antibiotics initiated. In 13% of cases, the cause of the spike could not be identified
Respiratory deterioration without suspected infection (no antibiotics started) occurred around 34% of first spikes and 27% of all spikes in the non-display infants. No clinical association could be identified in the remaining spikes (13% of first spikes and 28% of all spikes in the non-display infants).
DISCUSSION
Although the heart rate characteristics monitor was designed to show clinicians the fold increased risk of imminent clinical deterioration from sepsis, other conditions can cause depressed heart rate variability and transient decelerations and lead to a rise in the heart rate characteristics index. We found that large increases in the heart rate characteristics index occurred following surgical procedures, around the time of sepsis and other infection-related conditions such as necrotizing enterocolitis, and in association with acute deterioration in respiratory status without apparent infection. In a small fraction of cases, no change in an infant’s clinical status was discerned around the time of an heart rate characteristics index spike.
This analysis included a subset of infants in a large multicenter randomized clinical trial of heart rate characteristics index monitoring for VLBW infants(10). Among all infants at our center enrolled during a 3-year period, 38% experienced at least one large heart rate characteristics index spike, and the most common clinical association was suspected or proven infection, irrespective of whether or not the heart rate characteristics index was displayed to clinicians. Infection involves proliferation of pathogens which can stimulate vagus nerve pathways leading to transient heart rate decelerations(17), and in some cases infection leads to a systemic inflammatory response with release of proinflammatory cytokines that can depress heart rate variability(16, 23). Although we focused the current analysis on large increases in the heart rate characteristics index, smaller increases may also herald impending sepsis. In a prior analysis of all 974 episodes of septicemia in all 3003 VLBW infants in the randomized clinical trial, we found that 92% of infants with septicemia had an heart rate characteristics index >1 and 79% >2 near the time of clinical diagnosis(24). In that analysis we also found that a large heart rate characteristics index spike defined as in the current analysis (increase of 3 over the infants’ prior 5 day average) commonly occurred in the days leading up to diagnosis of septicemia. These pre-diagnosis spikes were significantly more common in infants whose heart rate characteristics index was not displayed to clinicians (22% of septicemia episodes had large pre-diagnosis spikes in display infants compared with 34% of septicemia episodes in non-display infants). Large spikes occurring prior to clinical diagnosis of septicemia may represent a sepsis prodrome and an opportunity for earlier intervention with antibiotics if the heart rate characteristics index is displayed at the bedside.
In the clinical trial there were no mandated interventions based on a specific threshold value or rate of rise of the heart rate characteristics index; instead, clinicians were instructed about how the heart rate characteristics index was developed and encouraged to evaluate an infant when the score was rising. We found, not surprisingly, that infants with heart rate characteristics index displayed were more likely to have antibiotics initiated and to have sepsis ruled out or clinical sepsis diagnosed around the time of a large spike. The difference in overall antibiotic administration through the NICU stay did not reach statistical significance for the display versus non-display infants in the current analysis, but in a recent analysis of 700 infants with septicemia from the 3003 VLBW infants enrolled in the clinical trial, total antibiotic days were significantly increased by 10% (3 days) in infants with heart rate characteristics index displayed (24).
Other than infection, the two major clinical associations with a large rise in the heart rate characteristics index were surgery and acute respiratory deterioration. Surgical interventions may induce a self-limited systemic inflammatory response, and anesthetic and anticholinergic medications may transiently decrease heart rate variability. In uncomplicated cases, the heart rate characteristics index generally rises and returns to baseline within 12 to 24 hours of surgery. We found a substantial number of cases in which a large spike in the heart rate characteristics index was temporally associated with acute respiratory deterioration without suspected infection (no antibiotics initiated). Respiratory deterioration may involve worsening apnea, hypoxia, acidosis, or hypercapnia, which can impact the heart rate characteristics index by increasing the frequency of heart rate decelerations or by dampening heart rate variability. We were not able to identify specific patterns of heart rate characteristics index spikes that distinguish infection from acute respiratory failure.
A small fraction of large heart rate characteristics index spikes had no apparent clinical correlation in this analysis. The constraints of a retrospective chart review are such that we were not able to reliably identify the many possible clinical events and clinician thought processes around the time of each spike. We did, however, find that a CBC was obtained around the time of a majority of heart rate characteristics index spikes, and that the immature:total neutrophil ratio was lower in infants not started on antibiotics, suggesting that this information may have been incorporated into the decision to withhold antibiotics in infants whose clinical presentation was equivocal. Our group previously showed that combining analysis of heart rate characteristics index and blood test results improves the diagnostic accuracy for sepsis over either test alone(8). Measuring a biomarker such as C-reactive protein at the time of an heart rate characteristics index spike, or when non-specific signs develop without heart rate characteristics index changes, might facilitate decisions about initiation and discontinuation of antibiotics.
Although use of the heart rate characteristics monitor was shown to reduce sepsis-associated mortality in VLBW infants(24), experience and clinical judgment are essential to properly use this technology to optimize patient outcomes. Increased understanding of the causes of a high heart rate characteristics index will help establish a balance between early detection and treatment of infection and judicious use of antibiotics in the NICU.
Footnotes
The other authors declare no conflicts of interest.
Registered with ClinicalTrials.gov: ≪≫
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Brynne A. Sullivan, Email: bsa4m@hscmail.mcc.virginia.edu, Department of Pediatrics, University of Virginia.
Stephanie M. Grice, Email: smgrice.md@gmail.com, Department of Pediatrics, University of Virginia.
Douglas E. Lake, Email: del2k@hscmail.mcc.virginia.edu, Department of Medicine, University of Virginia.
J. Randall Moorman, Email: rm3h@hscmail.mcc.virginia.edu, Department of Medicine, University of Virginia.
Karen D. Fairchild, Email: Kdf2n@virginia.edu, Department of Pediatrics Box 800386 University of Virginia Health System Hospital Drive Charlottesville, VA 22908 Phone: (434) 924-5496 Fax: (434) 982-8347.
References
- 1.Fairchild KD, O'Shea TM. Heart rate characteristics: physiomarkers for detection of late-onset neonatal sepsis. Clin Perinatol. 2010 Sep;37(3):581–98. doi: 10.1016/j.clp.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griffin MP, O'Shea TM, Bissonette EA, Harrell FE, Jr, Lake DE, Moorman JR. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr Res. 2003 Jun;53(6):920–6. doi: 10.1203/01.PDR.0000064904.05313.D2. [DOI] [PubMed] [Google Scholar]
- 3.Griffin MP, Moorman JR. Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics. 2001 Jan;107(1):97–104. doi: 10.1542/peds.107.1.97. [DOI] [PubMed] [Google Scholar]
- 4.Moorman JR, Lake DE, Griffin MP. Heart rate characteristics monitoring for neonatal sepsis. IEEE Trans Biomed Eng. 2006 Jan;53(1):126–32. doi: 10.1109/TBME.2005.859810. [DOI] [PubMed] [Google Scholar]
- 5.Griffin MP, Lake DE, Bissonette EA, Harrell FE, Jr, O'Shea TM, Moorman JR. Heart rate characteristics: novel physiomarkers to predict neonatal infection and death. Pediatrics. 2005 Nov;116(5):1070–4. doi: 10.1542/peds.2004-2461. [DOI] [PubMed] [Google Scholar]
- 6.Kovatchev BP, Farhy LS, Cao H, Griffin MP, Lake DE, Moorman JR. Sample asymmetry analysis of heart rate characteristics with application to neonatal sepsis and systemic inflammatory response syndrome. Pediatr Res. 2003 Dec;54(6):892–8. doi: 10.1203/01.PDR.0000088074.97781.4F. [DOI] [PubMed] [Google Scholar]
- 7.Lake DE, Richman JS, Griffin MP, Moorman JR. Sample entropy analysis of neonatal heart rate variability. Am J Physiol Regul Integr Comp Physiol. 2002 Sep;283(3):R789–97. doi: 10.1152/ajpregu.00069.2002. [DOI] [PubMed] [Google Scholar]
- 8.Griffin MP, Lake DE, Moorman JR. Heart rate characteristics and laboratory tests in neonatal sepsis. Pediatrics. 2005 Apr;115(4):937–41. doi: 10.1542/peds.2004-1393. [DOI] [PubMed] [Google Scholar]
- 9.Griffin MP, Lake DE, O'Shea TM, Moorman JR. Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr Res. 2007 Feb;61(2):222–7. doi: 10.1203/01.pdr.0000252438.65759.af. [DOI] [PubMed] [Google Scholar]
- 10.Moorman JR, Carlo WA, Kattwinkel J, Schelonka RL, Porcelli PJ, Navarrete CT, et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J Pediatr. 2011 Dec;159(6):900–6. e1. doi: 10.1016/j.jpeds.2011.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Griffin MP, O'Shea TM, Bissonette EA, Harrell FE, Jr, Lake DE, Moorman JR. Abnormal heart rate characteristics are associated with neonatal mortality. Pediatr Res. 2004 May;55(5):782–8. doi: 10.1203/01.PDR.0000119366.21770.9E. [DOI] [PubMed] [Google Scholar]
- 12.Moorman JR, Rusin CE, Lee H, Guin LE, Clark MT, Delos JB, et al. Predictive monitoring for early detection of subacute potentially catastrophic illnesses in critical care. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:5515–8. doi: 10.1109/IEMBS.2011.6091407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bravi A, Green G, Longtin A, Seely AJ. Monitoring and identification of sepsis development through a composite measure of heart rate variability. PLoS One. 2012;7(9):e45666. doi: 10.1371/journal.pone.0045666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seely AJ, Green GC, Bravi A. Continuous Multiorgan Variability monitoring in critically ill patients--complexity science at the bedside. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:5503–6. doi: 10.1109/IEMBS.2011.6091404. [DOI] [PubMed] [Google Scholar]
- 15.Gang Y, Malik M. Heart rate variability in critical care medicine. Curr Opin Crit Care. 2002 Oct;8(5):371–5. doi: 10.1097/00075198-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Fairchild KD, Saucerman JJ, Raynor LL, Sivak JA, Xiao Y, Lake DE, et al. Endotoxin depresses heart rate variability in mice: cytokine and steroid effects. Am J Physiol Regul Integr Comp Physiol. 2009 Oct;297(4):R1019–27. doi: 10.1152/ajpregu.00132.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fairchild KD, Srinivasan V, Moorman JR, Gaykema RP, Goehler LE. Pathogen-induced heart rate changes associated with cholinergic nervous system activation. Am J Physiol Regul Integr Comp Physiol. 2011 Feb;300(2):R330–9. doi: 10.1152/ajpregu.00487.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stone ML, Tatum PM, Weitkamp JH, Mukherjee AB, Attridge J, McGahren ED, et al. Abnormal heart rate characteristics before clinical diagnosis of necrotizing enterocolitis. J Perinatol. 2013 May 30; doi: 10.1038/jp.2013.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark MT, Vergales BD, Paget-Brown AO, Smoot TJ, Lake DE, Hudson JL, et al. Predictive monitoring for respiratory decompensation leading to urgent unplanned intubation in the neonatal intensive care unit. Pediatr Res. 2013 Jan;73(1):104–10. doi: 10.1038/pr.2012.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Griffin MP, Lake DE, Siadaty MS, Moorman JR. Heart rate characteristics are abnormal after surgery in neonates. Pediatr Res. 2003;53(4):31A. [Google Scholar]
- 21.Fairchild K, Aschner JL. HeRO monitoring to reduce mortality in NICU patients. Research and Reports in Neonatology. 2012 Aug 14;2:65–76. [Google Scholar]
- 22.Mazzeo AT, La Monaca E, Di Leo R, Vita G, Santamaria LB. Heart rate variability: a diagnostic and prognostic tool in anesthesia and intensive care. Acta Anaesthesiol Scand. 2011 Aug;55(7):797–811. doi: 10.1111/j.1399-6576.2011.02466.x. [DOI] [PubMed] [Google Scholar]
- 23.Tateishi Y, Oda S, Nakamura M, Watanabe K, Kuwaki T, Moriguchi T, et al. Depressed heart rate variability is associated with high IL-6 blood level and decline in the blood pressure in septic patients. Shock. 2007 Nov;28(5):549–53. doi: 10.1097/shk.0b013e3180638d1. [DOI] [PubMed] [Google Scholar]
- 24.Fairchild KD, Schelonka RL, Kaufman DA, Carlo WA, Kattwinkel J, Porcelli PJ, et al. Septicemia mortality reduction in neonates in a heart rate characteristics monitoring trial. Pediatr Res. 2013 Aug 13; doi: 10.1038/pr.2013.136. [DOI] [PMC free article] [PubMed] [Google Scholar]