Abstract
The adoption of health behaviors characterized by minimal energy expenditure and overconsumption of energy has led to cardiometabolic risk factors in pregnancy, childhood, and youth, all of which increase the prevalence of cardiovascular disease in adulthood. The propensity to develop abdominal obesity and cardiometabolic risk factors appears to disproportionally affect non-white ethnic groups. While the majority of observational research has been conducted in populations of European origin, studies in non-white ethnic groups across the life-course are underway and there is evidence that unique ethnic-specific differences exist. This review will focus on the life-course determinants of obesity and its related cardio-metabolic risk factors among diverse ethnic groups including people of Afro-Caribbean origin, South Asian, East Asian, and indigenous ancestry.
Keywords: Obesity, Ethnicity, Cardiometabolic risk factors
Introduction
Globally, the most common causes of mortality are noncommunicable diseases (NCDs) of which the most prevalent is cardiovascular disease (CVD) [1]. Identifiable risk factors for CVD include dietary factors, sedentary behaviors, low physical activity, psychosocial stress, hypertension, tobacco use, abnormal lipids, glucose intolerance, and obesity [2]. Emerging as an epidemic in recent years, obesity has hastened the progress of CVD prevention efforts [3, 4]. The etiology of obesity across the lifespan is complex. Differences in the prevalence of obesity [5], its related cardio-metabolic risk factors, and CVD between ethnic groups [6] has uncovered unique ethno-cultural differences associated with the etiology, type, and consequences of obesity. With globalization, adoption of a westernized lifestyle, namely one characterized by minimal energy expenditure and overconsumption of energy has led to higher prepregnancy body weight, greater gestational weight gain, more overweight and obese children, and more young adults with cardio-metabolic risk factors. The distribution of this excess adiposity and adverse metabolic consequences appears to disproportionally affect non-white ethnic groups. This review will focus on the life-course determinants of obesity and related cardio-metabolic risk factors among diverse ethnic groups including Afro-Caribbean, South Asians, East Asians, and indigenous people of North America.
The life course perspective refers to the interaction of biological factors and environmental exposures during different stages of life (ie, prepregnancy, gestation, infancy, adolescence, and adulthood) and the impact on health outcomes [7]. A life course perspective of obesity is established by evidence that exposures as early as pregnancy/in utero and early childhood impacts the development of obesity later in life [8] (Fig. 1). While the majority of observational research has been conducted in populations of European origin, studies in non-white ethnic groups have been developed, and there is emerging evidence that unique ethnic-specific differences exist in maternal health behaviors [9], prevalence of gestational diabetes [10], birth weight [10], postnatal growth [9], and propensity to develop overweight/obesity and associated metabolic risk factors [11] (Table 1). This review will focus on the key sensitive periods over the lifespan, and within each important risk factors and health behaviors will be explored, including pregnancy/in utero (maternal obesity and gestational weight gain [GWG]), infancy (rapid weight gain and breastfeeding), and childhood/adolescence (diet, physical activity, and sedentary behavior) into adulthood. In all ethnic comparisons when risk factors are compared with a reference population, most commonly white Caucasians, it is important to (1) consider the method of sampling with population-based studies of large size producing the most reliable results, and (2) take into account the socioeconomic differences between the groups which may suggest an apparent ethnic difference. Failure to consider the latter may lead to erroneous conclusions that ethnic differences exist when in fact they are due to a socioeconomic imbalance [9, 24].
Fig. 1.
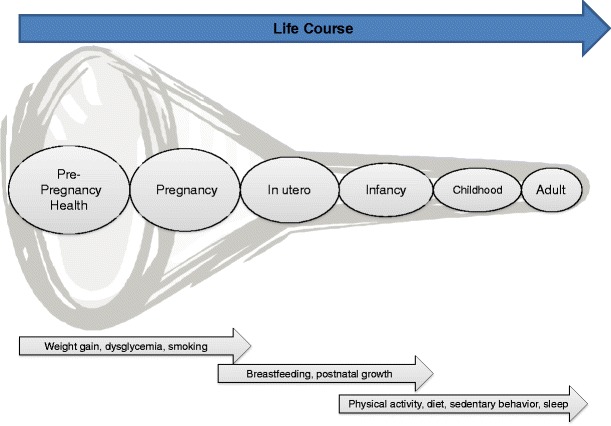
A life-course approach to obesity: key health behaviors and risk factors
Table 1.
Overweight, obesity, and related early life determinants from diverse ethnic groups in North America
| Factor | White Caucasian | South Asian | African Origin | East Asian | Indigenous |
|---|---|---|---|---|---|
| Maternal pre-pregnancy BMI >30 kg/m2 (obese) | 14.9 % [12] | U/A | 26.1 % [12] | Asian/PI: 8.8 % [12] | 27.7 % [13] |
| Gestational weight gain exceeded IOM recommendations | 47.3 % [12] | U/A | 52.1 % [12] | Asian/PI: 40 % [12] | 52 % [14] |
| Prevalence of GDM | 3.4 % [12] | Canada: 10 % [15] | 3.4 % [12] | Asian/PI: 9 % [12] | 8.1 % to 11.7 % [16–18] |
| Prevalence of maternal smoking | 18.5 % [19] | U/A | 10.1 % [19] | Asian/PI: 5.4 % [19] | Alaska Native: 36.3 % |
| American Indians: 20.6 % [19] | |||||
| Birth weight (@40 weeks) | Canada: 3030 g [10] | Canada: 2863 g [10] | Canada: 2900 g [10] | Canada: 2920 g [10] | Male: 4030 g [10] |
| US: 3326 g [12] | US: 3120 g [12] | US, Asian/PI: 3252 g [12] | Female: 3900 g [16] | ||
| Breastfeeding @ 6 months | US: 47 % [20] | Canada, Asian: 30.2 % [21] | US: 30 % [20] | Canada, Asian: 30.2 % [21] | Canada 16.6 % [21] |
| Canada: 25.8 % [21] | Canada: 27 % [21] | ||||
| %Overweight/obese (>85th percentile) during childhood | 27.9 % [4] | Asian: 12.5 % [22] | 39.1 % [4] | Asian: 12.5 % [22] | US: 48.7 % [23] |
U/A unavailable
The following sections will review the evidence of overweight, obesity, and associated cardio-metabolic risk factors and their associated health behaviors at different stages of the life-course for 4 ethnic groups—African-origin, South Asian, indigenous peoples, and East Asian.
African Origin
African origin includes people who originate from Africa and/or the Caribbean islands.
Pregnancy/In Utero
Most observational data of African-origin mothers/offspring originate from the United Kingdom (UK) and the United States (US). Population-based studies indicate that Black women are more obese than White Caucasian women [25] and have higher rates of excessive GWG [12]. However, they are also more likely to have inadequate GWG compared with White Caucasian women [26]. Further, the risk of gestational diabetes among Black women has been historically higher than White Caucasian women [27, 28]. Rates of smoking among pregnant African American women are traditionally lower than White Caucasian women in the US [29]. Disparities exist for neonatal outcomes with African Americans experiencing higher rates of infant mortality and low birth weight [30]. The etiology for these observations is complex, however, biological and socioeconomic factors likely play a role [31].
Infancy
Health behaviors in early infancy, including postnatal growth and infant diet, increase the risk of obesity in those of African ancestry. Rapid weight gain during the first year of life increased the risk of being obese (BMI ≥ 30) by age 20 years in a cohort of 300 African American infants [32]. This trajectory of growth in early infancy has been linked to breastfeeding [33]. Positive gains in rates of breastfeeding in the US between 2000 and 2008, are lower than breastfeeding rates in W.C. [20] where 59 % of African American infants ever breastfed compared with 75 % of White Caucasian infants, and 30 % of African American women breastfed until 6 months compared with 47 % White Caucasian women [20]. Reasons for these differences include continued ethno-cultural and socioeconomic factors.
Childhood/Adolescence
Table 1 illustrates the rates of childhood overweight/obesity among different ethnic groups. Black children in the US suffer a high prevalence of overweight and obesity compared with other groups, with the exception of Indigenous children. A constellation of health behaviors including physical inactivity, poor diet quality, and time spent in sedentary behaviors places children at risk of developing obesity. Data to date suggests that while Black children engage in more vigorous physical activity compared with White Caucasian children, they also are more likely to display sedentary behaviors. For example, data from the US National Health and Nutrition Examination Survey (NHANES) showed that Black children spend 8 min/day greater participating in moderate-vigorous physical activity compared with White Caucasian children, however, they also spent more time (25 min/day) in sedentary activities [34]. This observation is reinforced by the Child Heart Health Study in England (CHASE Study), which compared White Caucasian, South Asian, and African-Caribbean 9- to 10-year-olds and found African-Caribbean children spent more time (4 min/day greater) in moderate-vigorous physical activity than White Caucasian children [35]. However, in this same cohort, Black children also spent more sedentary time (26 min/day more) [35]. Interventions to promote activity (ie, culturally-tailored dance) and reduce screen time among African American girls, a particularly high-risk group, have had minimal impact on BMI [36]. Adverse dietary practices among Black children include excess high caloric and sugar sweetened beverage consumption compared with White Caucasian children [37] with a rising consumption in quantity between 1988 and 2004, in the US [38]. On balance consideration of activity, inactivity, and food consumption among Black children is complex, while there are some positive health behaviors displayed by African origin youth including vigorous activity, others are less desirable and suggest that population-based studies are required to track how these behaviors change and influence obesity rates over time.
South Asian
South Asian includes people who originate from the Indian subcontinent, including India, Pakistan, Bangladesh, and Sri Lanka.
Pregnancy/In Utero
South Asian adults have a higher burden of cardiovascular disease-related risk factors for the same BMI compared with White Caucasians [11]. This is explained by the higher percent body fat (ie, adiposity per unit BMI) and South Asians propensity to develop abdominal fat. A birth cohort from rural villages in India compared the anthropometric characteristics mothers and babies of European origin recruited from Southampton, UK [39]. This comparison revealed that South Asian mothers had a lower BMI (18 vs 23) compared with the European mothers, and South Asian babies were lighter (2.7 kg vs 3.5 kg) yet had comparable subscapular skin fold thickness, suggesting that for their weight they had relatively more adipose tissue. These South Asian babies were also found to have increased adiposity, glucose, and insulin at age 6–8 years [40]. Adding to this risk profile, is the observation that GDM is higher among South Asian women and is a predictor of infant weight gain and adiposity in the first year postpartum [41]. Predisposition for smaller weight at birth, may lead to an inherent risk of misclassifying South Asian infants as small for gestational age (SGA) (Table 1). Prospective longitudinal studies are ongoing to understand the prepregnancy, pregnancy, and in utero determinants for the thin-fat phenotype among South Asians [42, 43].
Infancy
South Asian babies are observed as “short, underweight, but fat,” which is referred to as the “thin-fat” phenotype [40]. The potential of assigning pathology to this observation may lead to unnecessary health visits and interventions when South Asian infants’ weights are plotted on growth charts derived from data from White Caucasian infants. It has been shown, when plotted on ethnicity-based birth weight growth centiles, 29–46 per 1000 South Asian newborns from Ontario, Canada were misclassified as SGA [44]. In light of this observation the early postnatal life is important and is modified by the observation that South Asian infants have a propensity toward a higher rate of growth compared with White Caucasian infants [45]. This compounds the risk later in life of obesity related complications. A protective health behavior is demonstrated by South Asian mothers being more likely to breastfeed compared with Caucasian women [46, 47]. This may impact on the risk of developing of obesity and related complications later in life.
Childhood/Adolescence
Physical activity, diet, and sedentary behavior during childhood all impact the risk of developing obesity among those of South Asian ancestry. Data among South Asian children are limited from North America. In the UK, school-aged, South Asian children have lower levels of physical activity compared with White Caucasian children [35] and have demonstrated higher caloric and total fat intake [48] and increased adiposity, compared with White Caucasian children [49]. Reducing sedentary behaviors such as screen time has been associated with improving obesity [50]. South Asian children in the UK have been observed to participate in high, (ie, greater than 4 h per day) sedentary activities which is similar to White Caucasian children [51]. Similar trends of low levels of physical activity exist among South Asian adults in North America [52, 53]. Cultural attitudes promoting sedentary activities rather that sports-related leisure activities are thought to play a role in this health behavior pattern [53].
Indigenous Peoples of North America
Indigenous peoples of North America include those who originate from American Indian, Alaska Native, First Nations, Metis, or Inuit ancestry.
Pregnancy/In Utero
The presence of multiple risk factors including higher gestational weight gain, higher gestational dysglycemia, and smoking undoubtedly influence obesity and its related risk factors among Indigenous peoples. Evidence suggests the average pre-pregnancy BMI is significantly higher among Indigenous women compared with non-Indigenous women, in the US and Canada [13, 54]. Further, higher gestational weight gain among Indigenous mothers has been significantly associated with obesity during childhood years [14]. The effect of dysglycemia during pregnancy is particularly relevant to Indigenous women for whom the prevalence of gestational diabetes is high [55]. In Canada previous studies have estimated the rate of gestational diabetes in Indigenous people ranges from 8.1 % to 11.7 % [16–18] compared with 3.0 % to 4.8 % in non-Indigenous people [17, 18]. Furthermore, data from the Pima Indians in the US show that the effects of dysglycemia during pregnancy is associated with obesity later in life [56]. The prevalence of smoking during pregnancy among Indigenous women is substantially higher than among non-Indigenous women (Table 1) [19, 57]. While one may expect that higher smoking in pregnancy will result in more SGA newborns, this has not been observed in Indigenous populations. The presence of smoking in pregnancy with higher birth weight newborns increases the risk of childhood obesity and insulin resistance (OR = 14.0, 95 % CI 3.8, 51.1) [58].
Infancy
Infants of Indigenous ancestry have a high risk for obesity based on their early life weight trajectory and nutritional exposures. Indigenous children are more likely to be born large for gestational age [16], have rapid postnatal growth [59], and those who have high BMI at age 1 year are 3 times more likely to be obese during childhood [14]. Each of these factors independently increases the risk of obesity later in life. Nutritional exposures during infancy also place infants at risk. Breastfeeding rates among Indigenous populations remain low in the United States (at 6 months 17 %) [59] and Canada (at 6 months 27 % [47, 60]) with cultural factors contributing to this disparity [61]. Further, among Indigenous children in the United States the absence breastfeeding imposes an increased risk of obesity by age 8 years [14].
Childhood/Adolescence
Although cultural heterogeneity exists among Indigenous peoples in North America there have been repeated observations from various tribes and reservations in North America documenting the high prevalence of risk factors for obesity. Among a cohort Pima Indian children in the US higher BMI has been associated with 2 times higher rates of premature death [62]. Children of Indigenous ancestry in Canada living on-Reserves have lower rates of physical activity participation than Indigenous children living off-Reserves [63]. Similar findings have been observed among populations in the US [64]. Furthermore, the risk of obesity associated with a high consumption of sugary beverages [65] has also been seen among Indigenous children in rural US [66]. Indigenous youth in the US tend watch more television, a form of sedentary behavior, compared with White Caucasian youth [67]. This is concerning as sedentary behaviors among Indigenous youth has been significantly correlated with risk for overweight and obesity [68]. Specific multi-component interventions tailored to Indigenous youth in the US have not been successful in reducing body weight among children aged 8 to 10 years [69].
East Asian
East Asian refers to people who originate from China, Japan, Taiwan, Vietnam, and Korea.
Pregnancy/In Utero
East Asian children whose mothers were obese during pregnancy were more likely to be overweight by age 6–7 years [70]. Further, East Asian women with higher pre-pregnancy BMI demonstrate more insulin resistance than White Caucasian women [71], and dysglycemia during pregnancy has been shown to increase the risk of cardio-metabolic risk in offspring of East Asian women [72]. The Chinese famine of 1959–1961 illustrates an adapted response to undernutrition in utero, where fetal exposure to severe famine led to an increased risk of dysglycemia in adulthood (OR = 3.92; 95 % CI: 1.64, 9.39) [73]. Finally, among a cohort of Taiwanese children, exposure to cigarette smoking in utero was associated with an increased risk of childhood obesity (OR 1.4 (95 % CI: 1.1–1 1.8) [74].
Infancy
The postnatal environment is important in shaping the trajectory of health. However, postnatal weight gain and breastfeeding, show diverging associations among East Asian children. Japanese adolescents who experienced greater weight gain in the first 18 months of life were more often overweight, compared with those who had a slower velocity of growth [75]. In contrast, there is evidence that breastfeeding may not be associated with obesity at age 6 to 7 years among a group of East Asian children in Hong Kong [70]. Although both are important observations the heterogeneity of the samples being compared makes a definitive conclusion difficult.
Childhood/Adolescence
The consequences of health behaviors among East Asian children are similar to other populations. Physical inactivity among a sample of Asian children in China showed an increased risk of obesity [76]. Further it has been shown that Asian children who spent more time participating in sedentary behaviors were more likely to be obese than those who spent less time engaging in similar activities [77]. Another study of East Asian children from China, showed a strong association between the consumption of sugar-sweetened beverages and obesity [78].
Adults, Obesity, and ethnicity
Overweight and obesity is associated with hypertension, type 2 diabetes, and abnormal lipids, which are strongly associated with the development of MI and stroke and may stall the decline in CVD in high-income countries [79]. Population-based studies from North America and the UK indicate that the prevalence of overweight and obesity differs substantially between ethnic populations. For example, using similar BMI cut-offs, overweight and obesity are highest among African origin and Hispanic populations, intermediate amongst White Caucasians, and lowest among South Asians and East Asians (Table 2). However, BMI as a measure of adiposity is limited and may over or underestimate adiposity differently in different ethnic groups. Whether BMI or another metric of adiposity is used to compare ethnic populations, or to study the association with cardio-metabolic risk factors, it is important to consider the following: (1) for some populations, there is greater adiposity per same given level of BMI, (2) adipose tissue distribution is important when considering metabolic consequences of overweight/obesity, and (3) adjustment for socio-economic and sex differences is crucial. The propensity to develop abdominal adiposity is a risk factor for cardio-metabolic risk factors, diabetes, coronary artery calcification, and CVD [102]. Even among individuals with abdominal obesity who show no signs of abnormal risk factors, ie, metabolically healthy, abdominal obese (MHAO), are at higher risk of mortality compared with their non-abdominally obese metabolically healthy counterparts (mortality risk for MHAO was around 40 % higher (hazard ratio 1.43; 95 % CI: 1.00–2.04) [103]. Certain non-White populations have a higher prevalence of abdominal adiposity including people of South Asian, African origin, and Indigenous people. Some studies also suggest that East Asians also have greater abdominal and visceral adiposity compared with White Caucasians [104]. However, indirect comparisons in which detailed measures of visceral fat area using CT or MRI suggest that South Asian men and women have particularly high amounts visceral fat compared with other ethnic groups, although more data using direct comparisons and similar measurements techniques are required. Visceral fat is strongly associated with the presence of fatty liver, which is then in turn associated with cardio-metabolic risk factors and CVD (Table 2). Sex differences in visceral adipose tissue (VAT) consistently show that men have greater VAT than women. However, more research to identify the VAT (in cm2) thresholds above which metabolic risk factors develop in each ethnic group are required as the cut points may differ [105].
Table 2.
Overweight, obesity and adiposity comparing adults from diverse ethnic groups
| African Americans | Chinese | Hispanic/Latino | South Asian | White Caucasian | |
|---|---|---|---|---|---|
| Prevalence of overweight (%) (BMI ≥25 <30) | 73.7 (71.2–76.2) [5] | 15.7 (0.4) [80] | 77.9 (74.5–81.4) [5] | Men: 40.9 [6] Women: 45.8 [6] |
66.7 (64.1–69.3) [5] |
| Prevalence of obesity (%) (BMI ≥30) | 44.1 (40.0–48.2) [5] | 10.7 (0.3) [80] | 38.7 (33.5–43.9) [5] | Men: 12.96
Women: 16.1 [6] |
32.4 (28.9–35.9) [5] |
| Greater body fat per given BMI compared with White Caucasians (Yes/No) | No [81] | Yes [82] | Yes [83] | Yes [82, 84] | N/A |
| Abdominal obesity % | Men: 34.6 [85] Women: 75.8 [85] (>102 cm in men and >88 cm in women) |
Men: 44 [6] Women: 22 [6] (>90 cm for men and >80 cm for women) |
Men: 37.8 [85] Women: 73.6 [85] (>102 cm for men and >88 cm for women) |
Men: 64.7 [6] Women: 72.7 [6] (>90 cm for men and >80 cm for women) |
Men: 45.1 [85] Women: 58.0 [85] (>102 cm for men and >88 cm for women) |
| Mean W/H circumference (cm) in population based studies | Men: 0.94 (0.07) [86] Women: 0.89 (0.08) [86] |
Men: 0.90 (0.1) [6] Women: 0.81 (0.1) [6] |
Men: 0.99 (0.06) [86] Women: 0.90 (0.07) [86] |
Men: 0.93 (0.06) [6] Women: 0.84 (0.08) [6] |
0.85 ± 0.01 [87] |
| Mean VAT measured by MRI or CT in population based sample (cm2) | Men: 108 ± 63 [88] | 100.0 (72.7, 126.6) [82] | Men: 127 ± 62 [88] | Men: 153.5 ± 8.8 [87] | Men: 134.5 ± 12.1 [87] |
| Women: 94 ± 58 [88] | Women: 107 ± 59 [88] | Women: 97.3 ± 7.3 [87] | Women: 95.6 ± 6.8 [87] | ||
| Fatty liver % in population based sample | Men: 23 [89] Women: 24 [89] |
Men: 36.8 [90] Women: 22.7 [90] |
Men: 45 [89] Women: 45 [89] |
Men: 10.8 [87]–31.1 [91] Women: 9.4 [87]–37.4 [91] |
Men: 42 [89] Women: 24 [89] |
| VAT and/or Fatty liver linked to T2D (Yes/No) | VAT: Yes [92] Fatty liver: Yes [89, 93] |
VAT: Yes [94] Fatty Liver: Yes [95] |
VAT: Yes [96] Fatty Liver: Yes [89] |
VAT: Yes [97, 98] Fatty liver: Yes [98] |
VAT: Yes [99] Fatty liver: Yes [99] |
| VAT and/or fatty liver linked to heart disease | VAT: Yes [100] Fatty liver: Yes [101] |
VAT: Yes [82] Fatty liver: Yes [95] |
VAT: Yes [99] Fatty liver: Yes [99] |
VAT: Yes [97] Fatty liver: Yes [98] |
VAT: Yes [99] Fatty liver: Yes [99] |
CT computed tomography, MRI magnetic resonance imaging, T2D type 2 diabetes, VAT visceral adipose tissue, W/H waist/hip
Genetics, Epigenetics and Microbiome Life-Course Studies of Obesity
Recently, genome wide association studies (GWAS) have identified multiple genetic variants associated with increased CVD risk, lipid traits, diabetes, adiposity, body weight, and hypertension, demonstrating that CVD is a complex disease with both polygenic and environmental influences [106–108]. Most GWAS have been performed in adults, and we have only started to elucidate the possible impacts of these genetic variants on metabolic factors early in life. Recently, in the ALSPAC birth cohort, a gene score made up of 8 SNPs (in/near: FTO, MC4R, TMEM18, GNPDA2, KCTD15, NEGR1, BDNF, and etV5) showed little association with birth weight per se (regression coefficient: 0.01 standard deviation score per allele; 95 % CI 0.00–0.02), but did have a large positive effect on early infancy weight gain (within first 6 weeks of life) (0.119 standard deviation scores/allele/year) but not on subsequent childhood weight gain (0.004 standard deviation scores/allele/year) [109]. These data suggest that it is possible that different genes influence a trait at different developmental stages, or that the same genes can have a differential impact on a trait as it develops. In support of this concept SNPs associated with lipid levels harbour a 2-fold higher effect size in children than in adults [110]. The situation is different for glucose and hypertension-associated SNPs, where similar effect sizes are observed in children and adults for genetic variants associated with these traits [111, 112]. These recent data reveal a complex pattern of association during childhood for SNPs modulating cardio-metabolic risk factors that require further investigation, especially in diverse ethnic populations, ideally in prospective birth cohorts.
Although studies of gene–environment interactions require even larger sample sizes than genetic studies, some early investigations are underway. For example, in 2 Greek birth cohorts, while the FTO SNP was associated with increased body weight, this effect was reduced among children who were breastfed for at least 1 month. In contrast, this interaction of FTO and breastfeeding was not replicated in the UK-based ALSPAC cohort [113]. Furthermore emerging technologies have enabled life-course studies of epigenetic patterning and infant microbiome as related to obesity [114–117]. Offspring of mothers exposed to the Dutch Famine have low birth weight and adult onset central adiposity and insulin resistance. Famine exposure is associated with widespread but modest differential DNA methylation in genes involved in growth and metabolic diseases including insulin like growth factor 2 and the insulin promoter in famine exposed offspring compared with their non-exposed siblings [118]. The recent development of chip-based technology enables the study of genome-wide epigenetic marks that is reliable and accurate, and together with detailed environmental exposures, opens up unprecedented possibilities for epigenetic research in human populations [119, 120].
Infant gut microflora composition is emerging as a host factor which may play an important role in the development of responses to food intake. Several factors shape gut microflora during infancy, including mode of nourishment delivery, type of infant feeding, hospitalization, antibiotic use, type of delivery (vaginal vs Caesarean section), and prematurity [117]. The gut microbiota is profoundly altered in humans during pregnancy [121]. This suggests that the microbiome of the pregnant mother may be associated with metabolic changes in pregnancy, and its transfer to the newborn may influence the metabolic response of the developing infant. Furthermore, recent studies suggest that nutritive and non-nutritive components of breast milk, formula, and solid foods, and feeding practices may also shape the infant microbiome, programming growth rates and body composition and shape behavioral responses to foods and eating [122–124]. “Western” diets may also play a role in promoting “obesogenic” gut microbiota, but this has not been comprehensively studied early in life [122, 125–127]. Thus genetic, epigenetic and microbiome studies across the life-course are underway and are expected to shed new light on the etiology of overweight and obesity in human populations. Such investigations in diverse ethnic groups are also needed, as in addition to adding new etiologic knowledge to high risk populations, are an efficient research strategy which capitalizes on their wide diversity in health behaviors and cultural practices.
Conclusions
To mitigate the global epidemic of obesity, a sustained effort is needed toward better understanding the increasingly complex scope of risk factors and the role they play in promoting disease. Because the etiology and related complications of obesity span multiple stages of the life-course, a robust and coordinated approach to capturing information across these stages is needed. This can be accomplished by (1) repeated observations over sensitive periods in the life course such as through birth cohorts, and (2) by observing and comparing different ethnic groups, as this has the potential to advance knowledge about the pathophysiology of obesity.
There have been many attempts to reduce the burden of obesity in adults, with few having long-term success. With the burden of obesity-related diseases being shifted earlier in life [3], the need to develop and test of interventions that impact the trajectory of obesity early in life is critical. The impact of promoting healthy lifestyles to women during pregnancy may lead to intergenerational benefits. Further a life course approach to obesity prevention should be multi-generational, family-focused, and consider unique ethno-cultural influences.
Acknowledgments
Compliance with ethics Guidelines
ᅟ
Conflict of Interest
Gita Wahi declares that she has no conflict of interest. Sonia S. Anand declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.World Health Organization. Noncommunicable diseases burden: mortality, morbidity and risk factors. Available at: http://www.who.int/nmh/publications/ncd_report_chapter1.pdf. Accessed May 1, 2013.
- 2.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet. 2004;364:937–52. [DOI] [PubMed]
- 3.Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–45. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 6.Anand SS, Yusuf S, Vuksan V, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in ethnic groups (SHARE) Lancet. 2000;356:279–84. doi: 10.1016/S0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 7.Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annu Rev Public Health. 2005;25:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- 8.John JR, Julie A, Ahmad RD, et al. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005;330:1357. doi: 10.1136/bmj.330.7503.1330-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010;125:686–95. doi: 10.1542/peds.2009-2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ray JG, Sgro M, Mamdani MM, et al. Birth weight curves tailored to maternal world region. J Obstet Gynaenol Can. 2012;34:159–71. doi: 10.1016/S1701-2163(16)35159-3. [DOI] [PubMed] [Google Scholar]
- 11.Razak F, Anand SS, Shannon H, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115:2111–8. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]
- 12.Bowers K, Laughon SK, Kiely M, Brite J, Chen Z, Zhang C. Gestational diabetes, pre-pregnancy obesity and pregnancy weight gain in relation to excess fetal growth: variations by race/ethnicity. Diabetologia. 2013;56:1263–71. doi: 10.1007/s00125-013-2881-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams AK, Harvey HE, Prince RJ. Association of maternal smoking with overweight at age 3 y in American Indian children. Am J Clin Nutr. 2005;82:393–8. doi: 10.1093/ajcn.82.2.393. [DOI] [PubMed] [Google Scholar]
- 14.Lindberg S, Adams A, Prince R. Early predictors of obesity and cardiovascular risk among American Indian children. Matern Child Health J. 2012;16:1879–86. doi: 10.1007/s10995-012-1024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Urquia ML, Glazier RH, Berger H, Ying I, DeSouza L, Ray JG. Gestational diabetes among immigrant women. Epidemiology. 2011;22:879–80. doi: 10.1097/EDE.0b013e31823199ee. [DOI] [PubMed] [Google Scholar]
- 16.Willows ND, Sanou D, Bell RC. Assessment of Canadian Cree infants’ birth size using the WHO Child Growth Standards. Am J Hum Biol. 2011;23:126–31. doi: 10.1002/ajhb.21115. [DOI] [PubMed] [Google Scholar]
- 17.Aljohani N, Rempel BM, Ludwig S, et al. Gestational diabetes in Manitoba during a twenty-year period. Clin Invest Med. 2008;31:E131–7. doi: 10.25011/cim.v31i3.3470. [DOI] [PubMed] [Google Scholar]
- 18.Rodrigues S, Robinson EJ, Kramer MS, Gray-Donald K. High rates of infant macrosomia: a comparison of a Canadian native and a non-native population. J Nutr. 2000;130:806–12. doi: 10.1093/jn/130.4.806. [DOI] [PubMed] [Google Scholar]
- 19.Tong VT, Jones JR, Dietz PM, D’Angelo D, Bombard JM. Trends in smoking before, during and after pregnancy—Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 31 sites, 2000–2005. MMWR Morb Mortal Wkly Rep. 2009;58:1–29. [PubMed] [Google Scholar]
- 20.Morb Mortal Wkly Rep MMWR. Progress in increasing breastfeeding and reducing racial/ethnic differences—United States, 2000–2008 Births. Vol 62: Centers for Disease Control and Prevention, (C.D.C.). 2013:77–80. [PMC free article] [PubMed]
- 21.Health Canada. Duration of exclusive breastfeeding in Canada: key statistics and graphics (2009–2010). Available at: http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/prenatal/initiation-eng.php - ref5. Accessed October 5, 2012.
- 22.Shabbir S, Kwan D, Wang MC, Shih M, Simon PA. Asians and Pacific Islanders and the growing childhood obesiy epidemic. Ethn Dis. 2010;20:129–35. [PubMed] [Google Scholar]
- 23.Ness M, Barradas DT, Irving J, Manning SE. Correlates of overweight and obesity among American Indian/Alaska Native and Non-Hispanic White children and adolescents: National Survey of Children’s Health, 2007. Matern Child Health J. 2012;16:S268–77. doi: 10.1007/s10995-012-1191-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anand SS, Razak F, Davis AD, et al. Social disadvantage and cardiovascular disease: development of an index and analysis of age, sex, and ethnicity effects. Int J Epidemiol. 2006;35:1239–45. doi: 10.1093/ije/dyl163. [DOI] [PubMed] [Google Scholar]
- 25.Heslehurst NRJ, Wilkinson JR, Summerbell CD. A nationally representative study of maternal obesity in England, UK: trends in incidence and demographic inequalities in 619 323 births, 1989–2007. Int J Obes. 2010;34:420–8. doi: 10.1038/ijo.2009.250. [DOI] [PubMed] [Google Scholar]
- 26.Headen IE, Davis EM, Mujahid MS, Abrams B. Racial-ethnic differences in pregnancy related weight. Adv Nutr. 2012;3:83–94. doi: 10.3945/an.111.000984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Savitz DA, Janevic TM, Engel SM, Kaufman JS, Herring AH. Ethnicity and gestational diabetes in New York City, 1995–2003. BJOG. 2008;115:969–78. doi: 10.1111/j.1471-0528.2008.01763.x. [DOI] [PubMed] [Google Scholar]
- 28.Hedderson MM, Darbinian JA, Ferrara A. Disparities in the risk of gestational diabetes by race-ethnicity and country of birth. Paediatr Perinatal Epidemiol. 2010;24:441–8. doi: 10.1111/j.1365-3016.2010.01140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Center for Behavioral Health Statistics and Quality. National survey on drug use and health. 2012. Available at: http://www.samhsa.gov/data/spotlight/Spot062PregnantRaceEthnicity2012.pdf. Accessed May 21, 2013.
- 30.Mathews TJ, MacDorman MF. Infant mortality statistics from the 2007 period linked birth/infant death data set Vol 59: National Vital Statistics Reports. 2011. [PubMed]
- 31.David RJ, Collins JW. Differing birth weight among infants of U.S.-born Blacks, African-born Blacks, and U.S.-born Whites. N Engl J Med. 1997;337:1209–14. doi: 10.1056/NEJM199710233371706. [DOI] [PubMed] [Google Scholar]
- 32.Stettler N, Kumanyika SK, Katz SH, Zemel BS, Stallings VA. Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am J Clin Nutr. 2003;77:1374–80. doi: 10.1093/ajcn/77.6.1374. [DOI] [PubMed] [Google Scholar]
- 33.Crume TL, Ogden LG, Mayer-Davis EJ, et al. The impact of neonatal breast-feeding on growth trajectories of youth exposed and unexposed to diabetes in utero: the EPOCH Study. Int J Obes. 2012;36:529–34. doi: 10.1038/ijo.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou C, Spuijt-Metz D. Physical activity in us youth: impact of race/ethnicity, age, gender, & weight status. Med Sci Sports Exerc. 2010;42:2211–21. doi: 10.1249/MSS.0b013e3181e1fba9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Owen CG, Nightingale CM, Rudnicka AR, Cook DG, Ekelund U, Whincup PH. Ethnic and gender differences in physical activity levels among 9-10-year-old children of white European, South Asian and African-Caribbean origin: the Child Heart Health Study in England (CHASE Study) Int J Epidemiol. 2009;38:1082–93. doi: 10.1093/ije/dyp176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robinson TN, Matheson DM, Kraemer HC, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med. 2010;164:995–1004. doi: 10.1001/archpediatrics.2010.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet. 2013;113:43–53. doi: 10.1016/j.jand.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121:e1604–14. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 39.van Steijn L, Karamali N, Kanhai H, et al. Neonatal anthropometry: thin-fat phenotype in fourth to fifth generation South Asian neonates in Suriram. Int J Obes. 2009;33:1326–9. doi: 10.1038/ijo.2009.154. [DOI] [PubMed] [Google Scholar]
- 40.Yajnik C, Fall C, Coyaji K, et al. Neonatal anthropometry: the thin-fat Indian baby. The Pune Maternal Nutrition Study. Int J Obes Relat Metab Disord. 2003;27:173–80. doi: 10.1038/sj.ijo.802219. [DOI] [PubMed] [Google Scholar]
- 41.Hamilton J, Odrobina E, Hanley A, Zinman B, Retnakaran R. Maternal insulin sensitivity during pregnancy predicts infant weight gain and adiposity at 1 year of age. Obesity. 2010;18(2):340–6. [DOI] [PubMed]
- 42.Anand SS, Vasudevan A, Gupta M, et al. Rationale and design of South Asian Birth Cohort (START) a Canada–India collaborative study. BMC Public Health. 2013;13. [DOI] [PMC free article] [PubMed]
- 43.Raynor P, Born in Bradford Collaborative Group. Born in Bradford, a cohort study of babies born in Bradford, and their parents: protocol for the recruitment phase. BMC Public Health. 2008;23. [DOI] [PMC free article] [PubMed]
- 44.Ray JG, Jiang D, Sgro M, Shah R, Singh G, Mamdani MM. Thresholds for small for gestational age among newborns of East Asian and South Asian ancestry. J Obstet Gynaenol Can. 2009;31:322–30. doi: 10.1016/S1701-2163(16)34149-4. [DOI] [PubMed] [Google Scholar]
- 45.Bansal N, Ayoola O, Gemmell I, et al. Effects of early growth on blood pressure of infants of British European and South Asian origin at one year of age: the Manchester children’s growth and vascular health study. J Hypertens. 2008;26:412–8. doi: 10.1097/HJH.0b013e3282f3168e. [DOI] [PubMed] [Google Scholar]
- 46.Lawton R, Ashley L, Dawson S, Waiblinger D, Conner M. Employing an extended Theory of Planned Behaviour to predict breastfeeding intention, initiation, and maintenance in White British and South-Asian mothers living in Bradford. Br J Health Psychol. 2012;17:854–71. doi: 10.1111/j.2044-8287.2012.02083.x. [DOI] [PubMed] [Google Scholar]
- 47.Health Canada. Breastfeeding initiation in Canada: Key statistics and graphics (2009–2010). Available at: http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/prenatal/initiation-eng.php - ref5. Accessed October 5, 2012.
- 48.Nightingale CM, Rudnicka AR, Owen CG, Cook DG, Whincup PH. Patterns of body size and adiposity among UK children of South Asian, black African-Caribbean and white European origin: Child Heart And health Study in England (CHASE Study) Int J Epidemiol. 2011;40:33–44. doi: 10.1093/ije/dyq180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Donin AS, Nightingale CM, Owen CG, et al. Nutritional composition of the diets of South Asian, black African-Caribbean and white European children in the United Kingdom: the Child Heart and Health Study in England (CHASE) Br J Nutr. 2010;104:276–85. doi: 10.1017/S000711451000070X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tremblay MS, LeBlanc AG, Kho ME, et al. Systematic review of sedentary behaviour and health indictators in school-aged childrena and youth. Int J Behav Nutr Phys Act. 2011;8. [DOI] [PMC free article] [PubMed]
- 51.Khunti K, Stone MA, Bankart J, et al. Physical activity and sedentary behaviors of South Asian and white European children in inner city secondary schools in the UK. Fam Pract. 2007;24:237–44. doi: 10.1093/fampra/cmm013. [DOI] [PubMed] [Google Scholar]
- 52.Bryan SN, Tremblay MS, Perez CE, Katzmarzyk PT. Physical activity and ethnicity: evidence for the Canadian Community Health Survey. Can J Public Health. 2006;97:271–6. doi: 10.1007/BF03405602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kandula NR, Lauderdale DS. Leisure time, non-leisure time, and occupational physical activity in Asian Americans. Ann Epidemiol. 2005;15:257–65. doi: 10.1016/j.annepidem.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 54.Lowell H, Miller DC. Weight gain during pregnancy: adherence to Health Canada’s guidelines. Health Rep. 2010;21:31–6. [PubMed] [Google Scholar]
- 55.Porter C, Skinner T, Ellis I. The current state of Indigenous and Aboriginal women with diabetes in pregnancy: a systematic review. Diabetes Res Clin Pract. 2012;98:209–25. doi: 10.1016/j.diabres.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 56.Pettitt DJ, Nelson RG, Saad MF, Bennett PH, Knowler WC. Diabetes and obesity in the offspring of Pima Indian women with diabetes during pregnancy. Diabetes Care. 1993;16:310–4. doi: 10.2337/diacare.16.1.310. [DOI] [PubMed] [Google Scholar]
- 57.First Nations Centre. First Nations Regional Longitudinal Health Survey (RHS) 2002/03: results for adults, youth and children living on First Nations Reserves. 2005; Available at: http://rhs-ers.ca/sites/default/files/ENpdf/RHS_2002/rhs2002-03-technical_report.pdf. Accessed June 1, 2011.
- 58.Huang RC, Burke V, Newnham JP, Stanley FJ, Kendall GE, Landau LI. Perinatal and childhood origins of cardiovascular disease. Int J Obes. 2007;31:236–44. doi: 10.1038/sj.ijo.0803394. [DOI] [PubMed] [Google Scholar]
- 59.Lindsay RS, Cook V, Hanson RL, Salbe AD, Tataranni A, Knowler WC. Early excess weight gain of children in the Pima Indian population. Pediatrics. 2002;109:E33. doi: 10.1542/peds.109.2.e33. [DOI] [PubMed] [Google Scholar]
- 60.Chapman DJ, Perez-Escamilla R. Breastfeeding among minority women: moving from risk factors to interventions. Adv Nutr. 2012;3:95–104. doi: 10.3945/an.111.001016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Black R, Godwin M, Ponka D. Breastfeeding among the Ontario James Bay Cree: a retrospective study. Can J Public Health. 2008;99:98–101. doi: 10.1007/BF03405453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–93. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Findlay LC, Kohen DE. Aboriginal children’s sport participation in Canada. Pimatisiwin. 2007;5:186–206. [Google Scholar]
- 64.Story M, Stevens J, Himes J, et al. Obesity in American-Indian children: prevalence, consequences, and prevention. Prev Med. 2003;37(Suppl 1(0)):S3–12. doi: 10.1016/j.ypmed.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 65.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505–8. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 66.Stroehla BC, Malcoe LH, Velie EM. Dietary sources of nutrients among rural Native American and White Children. J Am Diet Assoc. 2005;105:1908–16. doi: 10.1016/j.jada.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 67.Babey SH, Hastert TA, Wolstein J. Adolescent sedentary behaviors: correlates differ for television viewing and computer use. J Adolesc Health. 2013;52:70–6. doi: 10.1016/j.jadohealth.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hanley A, Harris SB, Gittelsohn J, Wolever TMS, Saksvig B, Zinman B. Overweight among children and adolescents in a Native Canadian community: prevalence and associated factors. Am J Clin Nutr. 2000;71:693–700. doi: 10.1093/ajcn/71.3.693. [DOI] [PubMed] [Google Scholar]
- 69.Caballero B, Clay T, Davis SM, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hui LL, Nelson EAS, Yu LM, Li AM, Fok TF. Risk factors for childhood overweight in 6- to 7-yr-old Hong Kong children. Int J Obes. 2003;27:1411–8. doi: 10.1038/sj.ijo.0802423. [DOI] [PubMed] [Google Scholar]
- 71.Retnakaran R, Hanley A, Connelly P, Sermer M, Zinman B. Ethnicity modifies the impact of obesity on insulin resistance in pregnancy: a comparison of Asian, South Asian and Caucasian women. J Clin Endocrinol Metab. 2006;91:93–7. doi: 10.1210/jc.2005-1253. [DOI] [PubMed] [Google Scholar]
- 72.Tam WH, Ma RCW, Yang X, et al. Glucose intolerance and cardiometabolic risk in children exposed to maternal gestational diabetes mellitus in utero. Pediatrics. 2008;122:1229–34. doi: 10.1542/peds.2008-0158. [DOI] [PubMed] [Google Scholar]
- 73.Li Y, He Y, Qi L, et al. Exposure to the Chinese famine in early life and the risk of hyperglycemia and type 2 diabetes in adulthood. Diabetes. 2010;59:2400–6. doi: 10.2337/db10-0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen YC, Chen PC, Hsieh WS, Portnov BA, Chen YA, Le YL. Environmental factors associated with overweight and obesity in Taiwanese children. Paediatr Perinatol Epidemiol. 2012;26:561–71. doi: 10.1111/ppe.12001. [DOI] [PubMed] [Google Scholar]
- 75.Fujita Y, Kouda K, Nakamura H, Iki M. Association of rapid weight gain during early childhood with cardiovascular risk factors in Japanese adolescents. J Epidemiol. 2013;23:103–8. doi: 10.2188/jea.JE20120107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Andegiorgish A, Wang J, Zhang X, Liu X, Zhu H. Prevalence of overweight, obesity, and associated risk factors among school children and adolescents in Tianjin, China. Eur J Pediatr. 2012;171:697–703. doi: 10.1007/s00431-011-1636-x. [DOI] [PubMed] [Google Scholar]
- 77.Yi X, Yin C, Chang M. Prevalence and risk factors of obesity among school-aged children in Xi’an, China. Eur J Pediatr. 2012;171:289–94. doi: 10.1007/s00431-011-1566-7. [DOI] [PubMed] [Google Scholar]
- 78.Shang XW, Liu AL, Zhang Q, et al. Report on childhood obesity in China: sugar-sweetened beverages consumption and obesity. Biomed Environ Sci. 2012;25:125–32. doi: 10.3967/0895-3988.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 79.Capewell S, Ford ES, Croft JB, Critchley JA, Greenlund KJ, Labarthe DR. Cardiovascular risk factor trends and potential for reducing coronary heart disease mortality in the United States of America. Bull World Health Organ. 2010;88:120–30. doi: 10.2471/BLT.08.057885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xi B, Liang Y, He T, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obes Rev. 2012;13:287–96. doi: 10.1111/j.1467-789X.2011.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72:694–701. doi: 10.1093/ajcn/72.3.694. [DOI] [PubMed] [Google Scholar]
- 82.Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: results of the Muticultural Community Health Assessment Trial (M-CHAT) Am J Clin Nutr. 2007;86:353–9. doi: 10.1093/ajcn/86.2.353. [DOI] [PubMed] [Google Scholar]
- 83.Casas YG, Schiller BC, DeSouza CA, Seals DR. Total and regional body composition across age in healthy Hispanic and white women of similar socioeconomic status. Am J Clin Nutr. 2001;73:13–8. doi: 10.1093/ajcn/73.1.13. [DOI] [PubMed] [Google Scholar]
- 84.Misra A, Khurana L. Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes. 2011;35:167–87. doi: 10.1038/ijo.2010.135. [DOI] [PubMed] [Google Scholar]
- 85.Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity. 2007;15:216–23. doi: 10.1038/oby.2007.505. [DOI] [PubMed] [Google Scholar]
- 86.Bell A, Adair LS, Popkin BM. Ethnic differences in the association between body mass index and hypertension. Am J Epidemiol. 2002;155:346–53. doi: 10.1093/aje/155.4.346. [DOI] [PubMed] [Google Scholar]
- 87.Anand SS, Tarnopolsky MA, Rashid S, et al. Adipocyte hypertrophy, fatty liver and metabolic risk factors in South Asians: the Molecular Study of Health and Risk in ethnic Groups (mol-SHARE) PLoS One. 2011;6:1–8. doi: 10.1371/journal.pone.0022112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hairston KG, Scherzinger A, Foy C, et al. Five-year change in visceral adipose tissue quantity in a minority cohort: the insulin resistance atherosclerosis study (IRAS) family study. Diabetes Care. 2009;32:1553–5. doi: 10.2337/dc09-0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–95. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 90.Wong VW, Chu WC, Wong GL, et al. Prevalence of non-alcoholic fatty liver disease and advanced fibrosis in Hong Kong Chinese: a population study using proton-magnetic resonance spectroscopy and transient elastography. Hepatology. 2012;61:409–25. doi: 10.1136/gutjnl-2011-300342. [DOI] [PubMed] [Google Scholar]
- 91.Dassanayake AS, Kasturiatne A, Rajindrajith S, et al. Prevalence and risk factors for non-alcoholic fatty liver disease among adults in an urban Sri Lankan population. Hepatology. 2009;24:1284–8. doi: 10.1111/j.1440-1746.2009.05831.x. [DOI] [PubMed] [Google Scholar]
- 92.Bidulescu A, Liu K, Hickson DA, et al. Gender differences in the association of visceral subcutaneous adiposity with adiponectin in African Americans: the Jackson Heart Study. BMC Cardiovasc Disord. 2013;13:1–10. doi: 10.1186/1471-2261-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–31. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 94.Jia W, Wu H, Bao Y, et al. Association of serum retinol-binding protein 4 and visceral adiposity in Chinese subjects with and without type 2 diabetes. JCEM. 2007;92:3224–9. doi: 10.1210/jc.2007-0209. [DOI] [PubMed] [Google Scholar]
- 95.Fan J, Farrell GC. Epidemiology of non-alcoholic fatty liver disease in China. J Hepatol. 2009;50:204–10. doi: 10.1016/j.jhep.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 96.Kim JS, Le KA, Mahurkar S, Davis JN, Goran MI. Influence of elevated liver fat on circulating adipocytokines and insulin resistance in obese Hispanic adults. Pediatr Obes. 2012;7:158–64. doi: 10.1111/j.2047-6310.2011.00014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Banerji M, Faridi N, Atluri R, Chaiken RL, Lebovitz HE. Body composition, visceral fat, leptin, and insulin resistance in Asian Indian men. JCEM. 1999;84:137–44. doi: 10.1210/jcem.84.1.5371. [DOI] [PubMed] [Google Scholar]
- 98.Kanaya AM, Wassel CL, Mathur D, et al. Prevalence and correlates of diabetes in South Asian Indians in the United States: findings from the Metabolic Syndrome and Atherosclerosis in South Asians Living in American Study and the Multi-Ethnic Study of Atherosclerosis. Metab Syndr Relat Disord. 2010;8:157–63. doi: 10.1089/met.2009.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nazare J, Smith JD, Borel A, et al. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the international study of prediction of inta-abdominal adiposity and its relationship with cardiometabolic risk/intra-abdominal adiposity. Am J Clin Nutr. 2012;96:714–26. doi: 10.3945/ajcn.112.035758. [DOI] [PubMed] [Google Scholar]
- 100.Liu J, Fox CS, Hickson DA, et al. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. J Clin Endocrinol Metab. 2010;95:5419–26. doi: 10.1210/jc.2010-1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Liu J, Musani SK, Bidulescu A, et al. Fatty liver, abdominal adipose tissue and atherosclerotic calcification in African Americans: the Jackson Heart Study. Atherosclerosis. 2012;224:521–5. doi: 10.1016/j.atherosclerosis.2012.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Neeland IJ, Turer AT, Ayers CR, et al. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA. 2012;308:1150–9. doi: 10.1001/2012.jama.11132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.van der A DL, Nooyens AC, van Duijnhoven FJ, Verschuren WM, Boer JM. All-cause mortality risk of metabolically healthy abdominal obese individuals: The EPIC-MORGEN study. Obesity. 2013;17. [DOI] [PubMed]
- 104.He W, Zhang S, Song A, et al. Greater abdominal fat accumulation is associated with higher metabolic risk in Chinese than in White people: an ethnicity study. PLoS One. 2013;8:e58688. doi: 10.1371/journal.pone.0058688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Katzmarzyk PT, Heymsfield SB, Bouchard C. Clinical utility of visceral adipose tissue for the identification of cardiometabolic risk in white and African American adults. Am J Clin Nutr. 2013;97:480–6. doi: 10.3945/ajcn.112.047787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.McPherson R. From genome-wide association studies to functional genomics: new insights into cardiovascular disease. Can J Cardiol. 2012. [DOI] [PubMed]
- 107.Deloukas P, Kanoni S, Willenborg C, et al. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet. 2012. [DOI] [PMC free article] [PubMed]
- 108.Samani NJ, Erdmann J, Hall AS, et al. Genomewide association analysis of coronary artery disease. N Engl J Med. 2007;357:443–53. doi: 10.1056/NEJMoa072366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Elks CE, Loos RJ, Sharp SJ, et al. Genetic markers of adult obesity risk are associated with greater early infancy weight gain and growth. PLoS Med. 2010;7:e1000284. doi: 10.1371/journal.pmed.1000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tikkanen E, Tuovinen T, Widen E, et al. Association of known loci with lipid levels among children and prediction of dyslipidemia in adults. Circ Cardiovasc Genet. 2011;4:673–80. doi: 10.1161/CIRCGENETICS.111.960369. [DOI] [PubMed] [Google Scholar]
- 111.Barker A, Sharp SJ, Timpson NJ, et al. Association of genetic Loci with glucose levels in childhood and adolescence: a meta-analysis of over 6,000 children. Diabetes. 2011;60:1805–12. doi: 10.2337/db10-1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Taal HR, Verwoert GC, Demirkan A, et al. Genome-wide profiling of blood pressure in adults and children. Hypertension. 2012;59:241–7. doi: 10.1161/HYPERTENSIONAHA.111.179481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dedoussis GV, Yannakoulia M, Timpson NJ, et al. Does a short breastfeeding period protect from FTO-induced adiposity in children? Int J Pediatr Obes. 2011;6:e326–35. doi: 10.3109/17477166.2010.490269. [DOI] [PubMed] [Google Scholar]
- 114.Gluckman PD, Hanson MA, Buklijas T, Low FM, Beedle AS. Epigenetic mechanisms that underpin metabolic and cardiovascular diseases. Nat Rev Endocrinol. 2009;5:401–8. doi: 10.1038/nrendo.2009.102. [DOI] [PubMed] [Google Scholar]
- 115.Lund G, Andersson L, Lauria M, et al. DNA methylation polymorphisms precede any histological sign of atherosclerosis in mice lacking apolipoprotein E. J Biol Chem. 2004;279:29147–54. doi: 10.1074/jbc.M403618200. [DOI] [PubMed] [Google Scholar]
- 116.Wren JD, Garner HR. Data-mining analysis suggests an epigenetic pathogenesis for type 2 diabetes. J Biomed Biotechnol. 2005;5:104–12. doi: 10.1155/JBB.2005.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Buddington RK, Sangild PT. Companion animals symposium: development of the mammalian gastrointestinal tract, the resident microbiota, and the role of diet in early life. J Anim Sci. 2011;89:1506–19. doi: 10.2527/jas.2010-3705. [DOI] [PubMed] [Google Scholar]
- 118.Heijmans BT, Tobi EW, Stein AD, et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc Natl Acad Sci U S A. 2008;105:17046–9. doi: 10.1073/pnas.0806560105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Feil R, Fraga MF. Epigenetics and the environment: emerging patterns and implications. Nat Rev Genet. 2011;13:97–109. doi: 10.1038/nrg3142. [DOI] [PubMed] [Google Scholar]
- 120.Petronis A. Epigenetics as a unifying principle in the aetiology of complex traits and diseases. Nature. 2010;465:721–7. doi: 10.1038/nature09230. [DOI] [PubMed] [Google Scholar]
- 121.Koren O, Goodrich JK, Cullender TC, et al. Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell. 2012;150:470–80. doi: 10.1016/j.cell.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wu GD, Chen J, Hoffmann C, et al. Linking long-term dietary patterns with gut microbial enterotypes. Science. 2011;334:105–8. doi: 10.1126/science.1208344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Azad MB, Kozyrskyj AL. Perinatal programming of asthma: the role of gut microbiota. Clin Dev Immunol. 2012;2012:932072. doi: 10.1155/2012/932072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Abrahamsson TR, Jakobsson HE, Andersson AF, Bjorksten B, Engstrand L, Jenmalm MC. Low diversity of the gut microbiota in infants with atopic eczema. J Allergy Clin Immunol. 2012;129(434–40):e431–2. doi: 10.1016/j.jaci.2011.10.025. [DOI] [PubMed] [Google Scholar]
- 125.de Wit N, Derrien M, Bosch-Vermeulen H, et al. Saturated fat stimulates obesity and hepatic steatosis and affects gut microbiota composition by an enhanced overflow of dietary fat to the distal intestine. Am J Physiol Gastrointest Liver Physiol. 2012;303:G589–99. doi: 10.1152/ajpgi.00488.2011. [DOI] [PubMed] [Google Scholar]
- 126.Fava F, Gitau R, Griffin BA, Gibson GR, Tuohy KM, Lovegrove JA. The type and quantity of dietary fat and carbohydrate alter faecal microbiome and short-chain fatty acid excretion in a metabolic syndrome ‘at-risk’ population. Int J Obes (Lond). 2012. [DOI] [PubMed]
- 127.Turnbaugh PJ, Ridaura VK, Faith JJ, Rey FE, Knight R, Gordon JI. The effect of diet on the human gut microbiome: a metagenomic analysis in humanized gnotobiotic mice. Sci Transl Med. 2009;1:6ra14. doi: 10.1126/scitranslmed.3000322. [DOI] [PMC free article] [PubMed] [Google Scholar]


