Abstract
We present a case of a 33-year-old woman who presented with phlyctenular conjunctivitis while on treatment for spinal intramedullary tuberculosis. She was treated with topical steroids along with continuation of antitubercular therapy, and improved on this treatment.
Background
We present a case of a 33-year-old woman who presented with phlyctenular conjunctivitis while on treatment for spinal intramedullary tuberculosis. She was treated with topical steroids along with continuation of antitubercular therapy, and improved on this treatment.
Phlyctenular conjunctivitis is a type IV cell-mediated hypersensitivity reaction to endogenous microbial proteins. It is more commonly reported from developing countries in the paediatric age group in association with pulmonary and lymph node tuberculosis.1 2 An association with intramedullary tuberculoma has not been reported in the existing literature.
A young woman being treated for spinal intramedullary tuberculomas (figure 1) developed phlyctenular conjunctivitis (figure 2A, B), which was asymptomatic, although its appearance was alarming for the patient and her family. Her neurological examination was normal except for bilateral extensor plantars.
Figure 1.
T1-weighted sagittal contrast MRI of the spinal cord depicting hyperintense irregularly enhancing intramedullary lesions at D2 and D4 vertebral level suggestive of tuberculomas.
Figure 2.
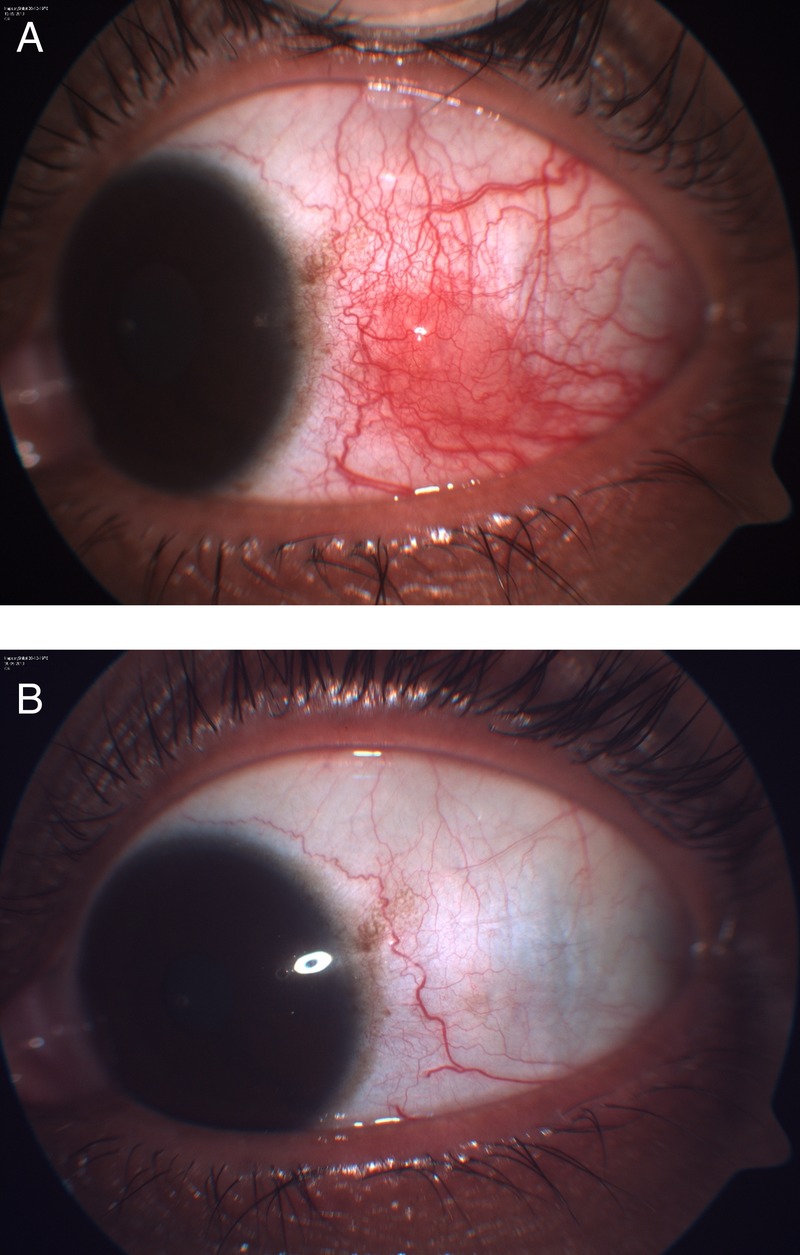
(A) Slit-lamp photograph of the left eye before treatment showing nodule near the limbus with surrounding hyperaemic and engorged conjunctival vessels suggestive of phlyctenular conjunctivitis. (B) Slit-lamp photograph of the left eye after treatment depicts resolution.
A timely diagnosis of this condition is important. Delay in diagnosis might lead to corneal ulceration, secondary infection and perforation. The treatment comprises topical steroids and antibiotics or antitubercular therapy in case of a tubercular aetiology.
Learning points.
Although usually described with cutaneous and lymph node tuberculosis, phlyctenular conjunctivitis can also be associated with central nervous system tuberculosis.
A high index of suspicion is required for the diagnosis and timely treatment of this condition to prevent possible complications such as corneal ulcer and perforation.
Recurrences are common in phlyctenular conjunctivitis and every episode should be treated.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rohatgi J, Dhaliwal U. Phlyctenular eye disease: a reappraisal. Jpn J Ophthalmol 2000;44:146–50 [DOI] [PubMed] [Google Scholar]
- 2.Kinsey HI. Phlyctenular conjunctivitis in relation to tuberculosis in children. Can Med Assoc J 1932;26:298–301 [PMC free article] [PubMed] [Google Scholar]


