Abstract
Portal vein thrombosis (PVT) following sleeve gastrectomy is rare. There are limited documented cases within the literature. The presentation of PVT varies on a spectrum from mild non-specific abdominal symptoms to life endangering clinical emergencies. This is the case of a 58-year-old woman who presented to the surgical assessment unit with acute onset abdominal pain 2 weeks post laparoscopic sleeve gastrectomy for morbid obesity. The initial diagnosis was that of a gastric sleeve leak. The patient deteriorated clinically and underwent a CT scan of her abdomen. This revealed the presence of an acute thrombus filling the portal vein with extension into the superior mesenteric vein branches. There were radiological changes suggestive of acute small bowel ischaemia. The patient underwent a laparotomy in theatre and 50 cm of the necrotic small bowel was resected. Postoperative care was carried out in the intensive care unit for 15 days.
Background
This case clearly demonstrates the potentially life-threatening presentation of portal vein thrombosis (PVT). The clinical picture was initially obscured by the history of a recent laparoscopic surgery. It demonstrates how rapidly patients can deteriorate with PVT, requiring prompt investigation and treatment. The literature suggests a higher rate of portal vein thrombosis in patients with cirrhotic liver disease1–3 as well as infection, inflammation and malignancy.1 Clinicians should have a lower threshold for investigating PVT in patients with known liver cirrhosis. Despite this patient's deterioration and major surgery, a relatively uneventful postoperative period occurred. The importance of a multidisciplinary approach was paramount to this patient's recovery and will need to continue following discharge. This consists of long-term input from the haematologists regarding appropriate anticoagulation, the gastroenterologists for screening and treatment of any complications of her cirrhosis and portal hypertension, particularly varices, the nutritional team with respect to nutritional support, diabetic specialists for ensuring good glycaemic control, and the surgical team for stoma care and the option of ileostomy reversal in future.
Case presentation
This case presentation is of a 58-year-old woman. Her medical history is extensive; the main health concern is poorly controlled diabetes. She was diagnosed with type 2 diabetes in 1997 and has had persistently poor glycaemic control. Her glycated haemoglobin has been persistently elevated, averaging at 86 mmol/L. She was initiated on insulin in 2005. She subsequently developed a metabolic syndrome: hypertension, hypercholesterolaemia and morbid obesity (weight being 124.1 kg, body mass index 49.6 kg/m2). She also suffered from ulcerative colitis and gastro-oesophageal reflux. She had a hysterectomy for endometriosis and a colonic adenoma removed at colonoscopy.
During 2012, the patient was investigated for pancytopenia due to hypersplenism, and mild lymphadenopathy. A diagnosis of low-grade lymphoma was considered but a trephine bone marrow biopsy was unsuccessful due to her morbid obesity. During this time period, she was struggling with obesity and poor diabetic control. Despite optimising medical treatment, there was no satisfactory weight reduction. The patient was listed for a combined gastric bypass and splenectomy on 18 November 2012. The splenectomy was planned as an aid in diagnosis of her haematological condition, and as a treatment of her hypersplenism. During this surgery an incidental finding of multiple hard, irregular liver lesions suggestive of cirrhosis, were discovered. This led to the abandonment of the gastric bypass, but the surgeon proceeded with a splenectomy. Multiple wedge biopsies were taken from the liver. Subsequently, the liver histology confirmed cirrhosis.
She was referred for an outpatient gastroenterology review. Non alcoholic fatty liver disease (NAFLD), related to her metabolic syndrome, was considered to be the cause of her cirrhosis. Her main symptoms were episodes of brief confusion and excessive daytime tiredness. She had also been investigated for obstructive sleep apnoea, epilepsy and narcolepsy. Each condition was ruled out. In view of her cirrhosis, a low grade encephalopathy was considered to be the cause of her symptoms. Her Child-Pugh grade was A (score of 6, based on a prolonged prothrombin time, mild encephalopathy and low albumin).
Unfortunately, the patient's glycaemic control was still suboptimal and her insulin resistance was increasing. Despite starting on 40 units of lantus and 44 units of humalog, satisfactory glycaemic control was not achieved. The patient was listed for a laparoscopic sleeve gastrectomy on 5 August 2013. The procedure and recovery period were uneventful.
On 22 August 2013 (2 weeks postsurgery), she presented to the accident and emergency department at 2:15. She reported non-specific abdominal pain. There was no history of nausea or vomiting. Her vital signs were stable (temperature 37.6 degrees Celsius, heart rate 95/beats per min, blood pressure 129/68 mmHg, respiratory rate 16 breaths per minute, blood glucose 9.2 mmol/L) and her blood tests were unrevealing (haemoglobin 11.8, white cell count 10.1). She was treated with intravenous analgesia, reassured and discharged. Twelve hours later, she returned to the surgical assessment unit with severe epigastric pain and two episodes of per rectal bleeding. On examination, she was clinically dehydrated and extremely tender over the left abdomen. A digital rectal examination revealed the presence of fresh and altered blood within the rectum. Her haemoglobin had dropped to 9.9, white cell count had increased to 25.9 and her C reactive protein was elevated at 74. Initially, a diagnosis of a gastric sleeve leak was suspected. She was started on intravenous fluid resuscitation and analgesia and was scheduled for an oesophagogastroduodenoscopy the following day to assess for evidence of a leak. At 10:30 on 23 August 2013, the patient clinically deteriorated and the critical outreach team was called. She was clinically shocked and an urgent CT of the abdomen was requested.
Investigations
The CT scan revealed moderate free fluid in the upper abdomen with no obvious features suggestive of a gastric sleeve leak. Most of the portal vein was noted to be occluded with a thrombus, which extended down into the superior mesenteric vein and its branches (figure 1). This was accompanied by a significant proportion of a thickened, non-enhancing and oedematous jejunum and ileum over a distance approximately of 50–60 cm. The features were highly suggestive of venous ischaemia (figure 2). It was likely to be an acute portal vein thrombosis as there was a lack of radiological evidence to suggest it was a chronic thrombus—there was no evidence of collateral portal vessel development and engorgement.
Figure 1.
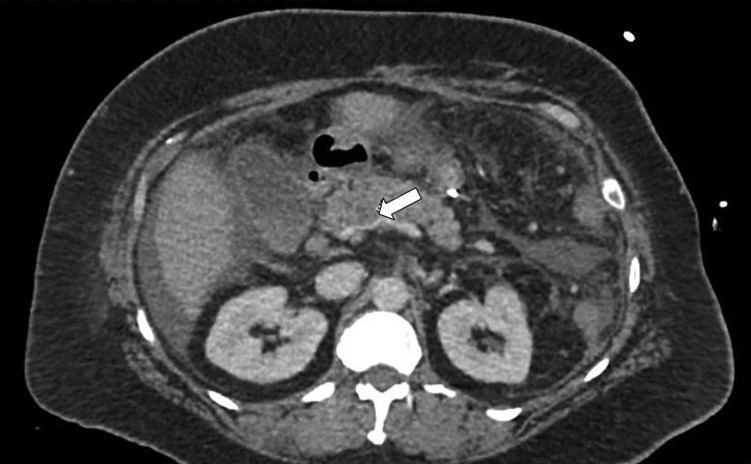
CT of the abdomen—portal vein thrombosis.
Figure 2.

CT of the abdomen—thickened, non-enhancing segment of small bowel.
Treatment
The patient was taken to the intensive care unit for optimisation prior to her surgery. A diagnostic laparoscopy was performed to assess the integrity of the gastric sleeve. There was no evidence of a leak following the insertion of 60 mL of methylene blue dye. Intraoperative findings consisted of bloodstained serous fluid within the abdomen and coils of the ischaemic small bowel. A midline laparotomy incision was created and 50 cm of the necrotic small bowel was resected—105 cm distal to the ligament of treitz and 40 cm proximal to the caecum. Haemostasis was achieved by applying vicryl to the mesentery and to the pedicle. A double-barrelled end ileostomy was formed in the left iliac fossa. The stoma was not everted. A surgical drain was inserted in the left upper quadrant and in the right iliac fossa. It was felt that the placement of a nasogastric or nasojejunal feeding tube would compromise the integrity of the gastric sleeve. Therefore, the patient was started on total parenteral feeding. The patient was in the intensive care unit for 15 days postoperatively. Her care was then de-escalated onto a general surgical ward.
Outcome and follow-up
The patient recovered well postprocedure. She was very driven and engaged heavily with all members of the multidisciplinary team. She regained her core postural strength following intense physiotherapy. She received extensive input from the dieticians—initially, there was great difficulty optimising her nutritional status and correcting electrolyte imbalances. As the patient was at high risk of developing a short gut syndrome, additional supplement adjuncts were prescribed. She received frequent teaching from the stoma care nurses regarding stoma education and management. The diabetic specialist team reviewed the patient and readjusted her insulin dose as required. She was also reviewed by the haematologists and discharged on 200 mg daily of enoxaparin subcutaneously, as a treatment of her PVT. The patient was fit and well on discharge. Gastroenterology and nutritional team follow-up was arranged.
Discussion
PVT is known to be a rare complication of sleeve gastrectomy. This woman also had additional prothrombotic conditions, including liver cirrhosis,3 inflammatory bowel disease and having had a previous splenectomy.1 Previous reports1 4 describe similar cases of PVT. However, these patients did not develop mesenteric ischaemia. Therefore, they did not require surgery and were treated conservatively with a heparin infusion. These patients presented similarly to this case with non-specific abdominal pain and nausea and vomiting.1 4 These vague symptoms, with relatively normal blood results, may cause the severity of the condition to be underestimated and thus result in delayed diagnosis.
A systematic literature review5 in 2009 highlighted 18 documented cases of portomesenteric thrombosis following laparoscopic surgery, of which seven patients had undergone a Roux-en-Y gastric bypass.
Steele et al6 demonstrated a high frequency of venous thromboembolism following bariatric surgery which extended well beyond the initial hospital discharge and 30 days after surgery. The venous thromboembolic rates were higher at 6 months when compared to 1 month postdischarge. In view of the high frequency of thromboembolic episodes up to 6 months following bariatric surgery, the authors have suggested extending the thromboembolic prophylaxis to months after discharge.
In a recent review7 of laparoscopic bariatric surgery of 5706 patients, 17 patients (0.3%) were found to have portomesenteric vein thrombosis—16 after sleeve gastrectomy and 1 following adjustable gastric banding. Although PVT is a rare occurrence after laparoscopic bariatric surgery, it is important to be familiar with it and to have a high index of suspicion for diagnosing it. Prompt diagnosis should help in the improved outcome of this potentially fatal condition.
Learning points.
Portal vein thrombosis (PVT) is a rare complication of sleeve gastrectomy.
A high index of suspicion is required for prompt diagnosis.
Risk of PVT is increased in patients with liver cirrhosis and following splenectomy.
PVT can present with non-specific abdominal pain and normal blood results.
Prompt identification, followed by appropriate treatment, results in a favourable outcome.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rosenberg JM, Tedesco M, Yao DC, et al. Portal vein thrombosis following laparoscopic sleeve gastrectomy for morbid obesity. JSLS 2012;16:639–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grendell JH, Ockner RK. Mesenteric venous thrombosis. Gastroenterology 1982;82:358–72 [PubMed] [Google Scholar]
- 3.Englesbe MJ, et al. Portal vein thrombosis and survival in patients with cirrhosis. Liver Transpl 2010;16:83–90 [DOI] [PubMed] [Google Scholar]
- 4.Franco J, Castillo JD, Veláquez A, et al. Portal thrombosis after laparoscopic bariatric surgery. Description of 3 cases and systematic literature review. Bariátr Metab Ibero Am 2011;1:1–5 [Google Scholar]
- 5.James AW, Rabl C, Westphalen AC, et al. Portomesenteric venous thrombosis after laparoscopic surgery: a systematic literature review. Arch Surg 2009;144: 520–6 [DOI] [PubMed] [Google Scholar]
- 6.Steele KE, Schweitzer MA, Prokopowicz G, et al. The long-term risk of venous thromboembolism following bariatric surgery. Obes Surg 2011;21: 1371–6 [DOI] [PubMed] [Google Scholar]
- 7.Goitein D, Matter I, Raziel A, et al. Portomesenteric thrombosis following laparoscopic bariatric surgery: incidence, patterns of clinical presentation, and etiology in a bariatric patient population. JAMA Surg 2013;148:340–6 [DOI] [PubMed] [Google Scholar]


