Abstract
A 47-year-old ex-nurse presented to the emergency department having consumed an unknown quantity of antifreeze. She was found to have a high level of ethylene glycol (the toxic component of antifreeze) in her bloodstream. Treatment is with either fomepizole or ethanol. She was treated with a loading dose of 2.5 mL/kg followed by 0.58 mL/kg/h of oral ethanol, equating to a maintenance dose of 35 mL of whisky every hour. She was placed on the gastroenterology ward next to two alcoholics recovering from acute withdrawal. It is important to appreciate the potential difficulties posed by scenarios of this type in order to provide optimum care both for the patient and those situated on the ward in the immediate vicinity. There is a requirement to compare the efficacies of fomepizole and ethanol therapy in the UK in order for a decision to be made on the most cost-effective first-line treatment.
Background
Antifreeze exposure most commonly occurs either as a result of deliberate ingestion with suicidal intent, or as a more affordable replacement for alcohol.1 Ethylene glycol is the active ingredient in antifreeze that causes most health effects because the metabolites glycoaldehyde, glycolic acid, glyoxylic acid and oxalic acid can cause central nervous system (CNS) depression, cardiopulmonary and renal failure.2 These toxic metabolites are generated after metabolism with alcohol dehydrogenase, and so the principle of treatment is to inhibit the enzyme to prevent the build-up of the aforementioned toxins.3 Alcohol dehydrogenase has a higher affinity for ethanol than for ethylene glycol, allowing alcohol to be exploited therapeutically as a competitive inhibitor.4 In this article, we present a case of substantial ethylene glycol ingestion and consider the ethical considerations relating to the treatment of a patient with alcohol in an environment containing recovering users.
Case presentation
A 47-year-old nurse presented to accident and emergency department following the deliberate ingestion of an estimated 200 mLs of antifreeze (in addition to a handful of rat poison and 0.5 L of vodka). Having fallen unconscious for the majority of the night, the patient was found wandering the streets searching for water and was subsequently brought into hospital. This was the second (the first being 6 days earlier of paracetamol overdose) and the most determined attempt to take her own life. Her desire for a successful suicide was such that she travelled for several hours to the area in order to carry out the attempt: in proximity to a hospital that she believed did not stock the antidote fomepizole. The patient has a 5-year history of depression managed by her general practitioner, treated with mirtazapine and sertraline. She also reported a significant history of alcohol excess.
The patient vomited three times prior to admission, including once immediately following consumption of the rat poison. She reported no haematemesis, malaena, fits or urinary symptoms. On examination, the patient was afebrile, had a Glasgow Coma Scale of 15, a respiratory rate 16, a regular pulse 92 bpm, blood pressure 151/97 mm Hg and glucose 6 mmol/L. On abdominal examination, the patient had mild epigastric tenderness. Cardiovascular, respiratory and neurological examinations were all unremarkable.
Investigations
On admission, the patient's venous blood gas revealed a metabolic acidosis (7.29) and a mildly raised anion gap (18.4). Her full blood count was found to be within normal limits; she was hypernatraemic (153 mmol/L) with the remainder of her electrolytes within normal range. Renal function was normal. She was found to have moderately deranged liver enzymes: raised alanine transaminase (189 IU/L) and alkaline phosphatase (77 IU/L), but synthetic function (demonstrated by normal albumin and clotting profile) was intact.
Following the advice from the National Poison Information Centre (NPIC), blood samples were taken for ethylene glycol (the toxic component of antifreeze) and sent for analysis at the Regional Laboratory for Toxicology in Birmingham. The sample taken on admission was 6510 mg/L.
Treatment
Fomepizole is the preferred treatment for ethylene glycol poisoning but was unavailable in this case. The alternative treatment is ethanol, either oral (40%) or intravenous (10%) via central line. After consultation with NPIC, the patient was given a loading dose of oral ethanol (40%) 2.5 mL/kg followed by maintenance of 0.58 mL/kg/h, with the aim of obtaining a constant blood ethanol level between 100 and 150 mg/L. Ethanol levels were measured four hourly and ethylene glycol daily.
Outcome and follow-up
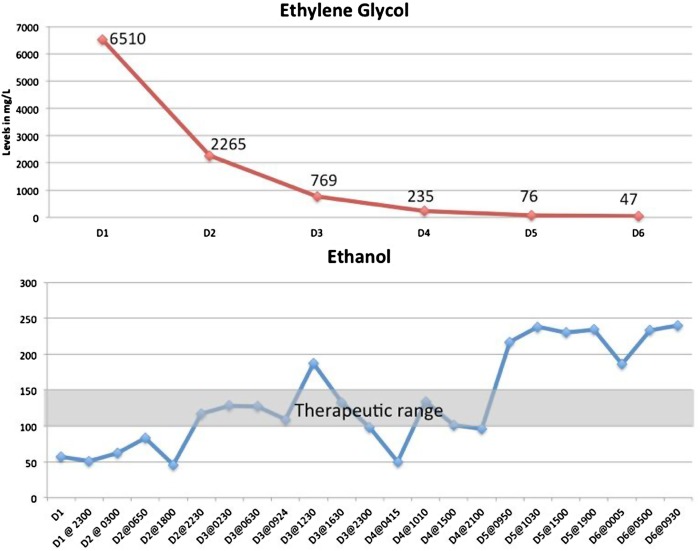
The patient was admitted to the gastroenterology ward where she received close monitoring, four hourly ethanol levels and arterial blood gas, plus daily ethylene glycol levels. In this 60 kg patient, this translated into 35 mL of whisky every hour. The ethylene glycol level was effectively reduced (figure 1) until it reached the safe range of <50 mg/L after 6 days, although the blood ethanol level dropped transiently below the therapeutic range on day 4.
Figure 1.
Ethylene glycol and ethanol levels in the patient over the treatment period.
Discussion
During 2010 and 2012, there were 1070 reported individual exposures involving toxic alcohols and glycols in the UK.5 Ethylene glycol has extremely harmful but treatable properties that, in combination with the incidence of ingestion, makes it an important poison for clinicians to be aware of. The presentation of acute intoxication is similar to that of alcohol, except without the characteristic smell of ethanol consumption.6 Clinicians must have a high index of suspicion in order not to miss this important and potentially life-saving diagnosis.
Ethylene glycol is rapidly absorbed via the gastrointestinal tract and metabolised in the liver where the toxic metabolites are formed.7 Either ethanol or fomepizole can be used as antidotes, both of which act to competitively inhibit the metabolism of ethylene glycol by alcohol dehydrogenase.3 4 This prevents the production and accumulation of the toxic metabolites. Figure 2 provides an explanation of this metabolic breakdown pathway and the location of ethanol and fomepizole action.
Figure 2.
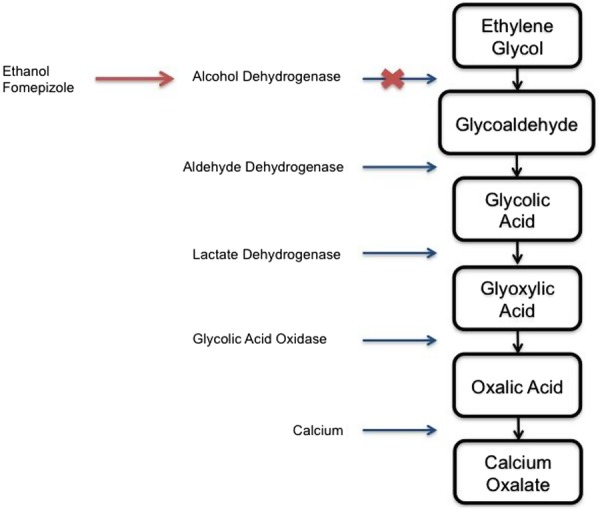
Metabolism of ethylene glycol. Ethanol and fomepizole inhibit alcohol dehydrogenase and so prevent the build-up of downstream toxic metabolites. Adapted from Davis et al.6
Ethylene glycol poisoning results in toxic effects that occur in a three-stage clinical syndrome.1 Over the first 6–12 h, CNS symptoms predominate, thought to be due to high concentrations of aldehydye metabolites.8 Clinically, there is apparent inebriation, nausea, vomiting, dizziness, ocular manifestations, hyporeflexia, coma, convulsions and even death in severe cases.1 At 12–24 h, cardiopulmonary features dominate (dyspnoea, tachycardia, cyanosis, hypertension, pulmonary oedema and congestive heart failure) with death being associated with pulmonary oedema, bronchopneumonia and cardiac dilation.1 9 Finally, at 24–72 h, renal toxicity follows and can result in acute renal failure (ARF).9 ARF is characterised by the accumulation of large birefringent calcium oxalate crystals in the renal tubular cells with proximal tubular necrosis.10 11 Oxalic acid, the terminal metabolite, is implicated as the renal toxicity causative agent.12
The lethal dose of ethylene glycol is estimated at being 1.4 mL/kg; therefore, in the patient (a 60 kg woman), this calculated to approximately 84 mL, significantly less than the 200 mL suspected intake.
Owing to the availabilities in the hospital when the patient presented, she was treated with oral ethanol in the form of whisky. Although this is the appropriate treatment in order to prevent the build-up of toxic metabolites, ethanol therapy is not without its drawbacks. Effects range from impaired reaction times and blurred vision to convulsions and coma, depending on the amount ingested.13 It is therefore of paramount importance to monitor patients treated with ethanol, especially in such high doses. Furthermore, therapy can result in hypoglycaemia and further CNS depression.7 14 Regular oral treatment may result in the development of a degree of alcohol dependence in otherwise non-alcoholic patients, so this risk should be carefully considered and balanced with the requirement to treat the current acute condition.
Successful competitive inhibition of ethylene glycol metabolism requires an ethanol concentration of 100–150 mg/L.15 Ethylene glycol levels should be monitored as a surrogate for ethanol's therapeutic effect and treatment should be terminated once the levels are undetectable.15
The patient's placement on the gastroenterology ward resulted in her being adjacent to two alcohol misusers currently undergoing detoxification. This therefore posed a second potential risk: following the patient's admission, patients suffering from acute withdrawal symptoms were now attempting to recover next to a woman consuming 35 mL of whisky every hour. Notwithstanding the urgency to start treatment, it is important to weigh up the benefits versus the risks of the patient being treated on the ward as opposed to a side room. Ward treatment allowed the patient to have personal contact with other patients (in this case, the patient reported interactions lifting her mood), thereby potentially reducing the risk of a suicide attempt in the immediate future. On the other hand, the neighbouring patients being regularly exposed to whisky could have a detrimental effect on their recovery. Side room treatment of the patient may be in the best interests of a greater number of vulnerable patients and therefore a more just choice given that the care plan would be acting in the collective best interest of more individuals.
With appropriate medical, psychological care and family support, it is possible that the patient will be rehabilitated with no future attempts at suicide, but poor handling of any of these aspects could result in a less favourable outcome. Arguably, the patient should have been placed on a higher dependency unit with more significant monitoring, particularly considering the high-dose ethanol treatment.16 This may have even limited the effect of the patient's treatment on other patients. However, if circumstances prohibit this, then the patients’ carers must be aware of and strive to minimise the potential risks: perhaps patients such as this 47-year-old woman could consume their ethanol outside of the bay.
The final question we pose in this article is: should all hospitals stock fomepizole, when there is a cheap and accessible alternative? Fomepizole has been proved to be the superior therapy for ethylene glycol poisoning: it has a higher potency of enzyme inhibition and therapeutic levels are more easily maintained, resulting in the lower frequency of adverse drug effects and reduced requirement for close monitoring.14 16 17 A comparative study identified that adverse drug events occurred in 57% of ethanol-treated patients compared with 12% for that of fomepizole.18 There is a strong case for the provision of fomepizole in all hospitals when looking at the relative efficacies and risks of the two drugs. According to a study in the USA, fomepizole is a more cost-effective treatment, even though it is considerably more expensive.17 It could be argued that the health service cannot always allocate the funds to the optimum treatment if there is a cheaper alternative. Ethically, given the financial restraints of the National Health Service (NHS), there is a further argument for resource rationing in treatments of self-caused conditions in the interest of net beneficence. NPIS and the College of Emergency Medicine released guidelines in 2008 for antidote stocking in the UK.19 The guideline recommends that either fomepizole or ethanol should be available within 1 h, and therefore present in the hospital.19 A national audit, performed in 2010, identified a suboptimal availability of antidotes for the treatment of toxic ethanol and glycol poisoning with 72% stocking intravenous ethanol, 28% oral ethanol and only 17% stocking fomepizole.20 Further research is required to comprehensively compare the safety and cost-effectiveness of fomepizole and ethanol in the UK before a judgement can be made as to an optimal first-line treatment of ethylene glycol poisoning.
Learning points.
Ethylene glycol, the active ingredient in antifreeze, has dangerous and detrimental health effects that can be treated with ethanol ingestion or the drug fomepizole.
Treat those who need treatment in the most effective environment while not compromising the interests of other patients.
Try where possible to reduce the reliance on problematic medications when there are better alternatives.
There is a requirement for further research into the most appropriate and cost-effective first-line treatment of ethylene glycol poisoning within the National Health Service.
Footnotes
Contributors: TW, JMW, RLV and PK made contributions to the design of the case report, acquisition of the data, analysis and interpretation of the data and the writing of the manuscript. All authors have read and agreed on the submitted version of this paper.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Parry MF, Wallach R. Ethylene glycol poisoning. Am J Med 1974;57:143–50 [DOI] [PubMed] [Google Scholar]
- 2.Leth PM, Gregersen M. Ethylene glycol poisoning. Forensic Sci Int 2005;155:179–84 [DOI] [PubMed] [Google Scholar]
- 3.Brent J. Current management of ethylene glycol poisoning. Drugs 2001;61:979–88 [DOI] [PubMed] [Google Scholar]
- 4.Wacker WE, Haynes H, Druyan R, et al. Treatment of ethylene glycol poisoning with ethyl alcohol. JAMA 1965;194:1231–3 [PubMed] [Google Scholar]
- 5.Public Health England National Poisons Information Service Annual Report 2012/2013. 2013
- 6.Davis DP, Bramwell KJ, Hamilton RS, et al. Ethylene glycol poisoning: case report of a record-high level and a review. J Emerg Med 1997;15:653–67 [DOI] [PubMed] [Google Scholar]
- 7.Brent J. Fomepizole for ethylene glycol and methanol poisoning. N Engl J Med 2009;360:2216–23 [DOI] [PubMed] [Google Scholar]
- 8.Frommer JP, Ayus JC. Acute ethylene glycol intoxication. Am J Nephrol 1982;2:1–5 [DOI] [PubMed] [Google Scholar]
- 9.Hess R, Bartels MJ, Pottenger LH. Ethylene glycol: an estimate of tolerable levels of exposure based on a review of animal and human data. Arch Toxicol 2004;78:671–80 [DOI] [PubMed] [Google Scholar]
- 10.McMartin K. Are calcium oxalate crystals involved in the mechanism of acute renal failure in ethylene glycol poisoning? Clin Toxicol (Phila) 2009;47:859–69 [DOI] [PubMed] [Google Scholar]
- 11.Friedman EA, Greenberg JB, Merrill JP, et al. Consequences of ethylene glycol poisoning: report of four cases and review of the literature. Am J Med 1962;32:891–902 [DOI] [PubMed] [Google Scholar]
- 12.Fraser AD. Clinical toxicologic implications of ethylene glycol and glycolic acid poisoning. Ther Drug Monit 2002;24:232–8 [DOI] [PubMed] [Google Scholar]
- 13.Health Protection Agency. Compendium of chemical hazards. http://www.hpa.org.uk.
- 14.McMartin KE. Antidotes for alcohol and glycol toxicity: translating mechanisms into treatments. Clin Pharmacol Ther 2010;88:400–4 [DOI] [PubMed] [Google Scholar]
- 15.Porter WH. Ethylene glycol poisoning: quintessential clinical toxicology; analytical conundrum. Clin Chim Acta 2012;413:365–77 [DOI] [PubMed] [Google Scholar]
- 16.Brent J, McMartin K, Phillips S, et al. Fomepizole for the treatment of ethylene glycol poisoning. Methylpyrazole for Toxic Alcohols Study Group. N Engl J Med 1999;340:832–8 [DOI] [PubMed] [Google Scholar]
- 17.Maraffa J, Stork C, Medicis J. Cost-effectiveness of fomepizole versus ethanol in the management of acute ethylene glycol exposure. Clin Toxicol 2005;43:691 [Google Scholar]
- 18.Lepik KJ, Levy AR, Sobolev BG, et al. Adverse drug events associated with the antidotes for methanol and ethylene glycol poisoning: a comparison of ethanol and fomepizole. Ann Emerg Med 2009;53:439–50 e10 [DOI] [PubMed] [Google Scholar]
- 19.College of Emergency Medicine Antidote availability and treatment guideline (2008). http://www.collemergencymed.ac.uk/Shop-Floor/Clinical%20Guidelines
- 20.Thanacoody RH, Aldridge G, Laing W, et al. National audit of antidote stocking in acute hospitals in the UK. Emerg Med J 2013;30:393–6 [DOI] [PubMed] [Google Scholar]