Abstract
In the absence of trauma, perforated jejunal diverticulum (JD) is a rare entity. Perforated isolated JD is rarer. We report a case of perforated isolated JD in a 55-year-old woman who presented with features of peritonitis and had no history of trauma. Resection and anastomosis of the involved jejunal segment was performed.
Background
Isolated jejunal diverticulum is rare and usually asymptomatic. However, it may lead to chronic non-specific abdominal symptoms or rarely an acute complication like perforation. Intraoperative identification of the perforated diverticulum, often hidden in between the mesenteric leaves, requires a high index of suspicion for the condition in patients with acute abdomen.
Case presentation
A 55-year-old woman presented to the emergency room with a history of generalised abdominal pain for 2 days and absolute constipation for 1 day. On examination, her vitals were stable but she was febrile. Abdominal examination revealed features of peritonitis.
Investigations
A straight X-ray of the abdomen in erect posture revealed dilated loops of small bowel and free gas under the domes of the diaphragm. Haematological investigations showed neutrophilic leucocytosis (20 000/mm3;90% neutrophils), hypokalaemia (2.7 mEq/L) and raised serum creatinine (2.1 mg/dL).
Differential diagnosis
Differential diagnoses included perforative peritonitis due to enteric or peptic perforation.
Treatment
Exploratory laparotomy was performed after proper resuscitation. Intraoperatively, a solitary jejunal diverticulum was found at about 50 cm from the duodenojejunal flexure. The diverticulum was encroaching into the mesentery and had a perforation about 1 cm in diameter on the mesenteric side (figure 1). Gross intraperitoneal contamination was also present. Resection of the segment containing the perforated diverticulum and a single layer end-to-end anastomosis was performed along with a thorough peritoneal lavage. An examination of the entire length of small and large bowel did not reveal presence of any other diverticulum.
Figure 1.
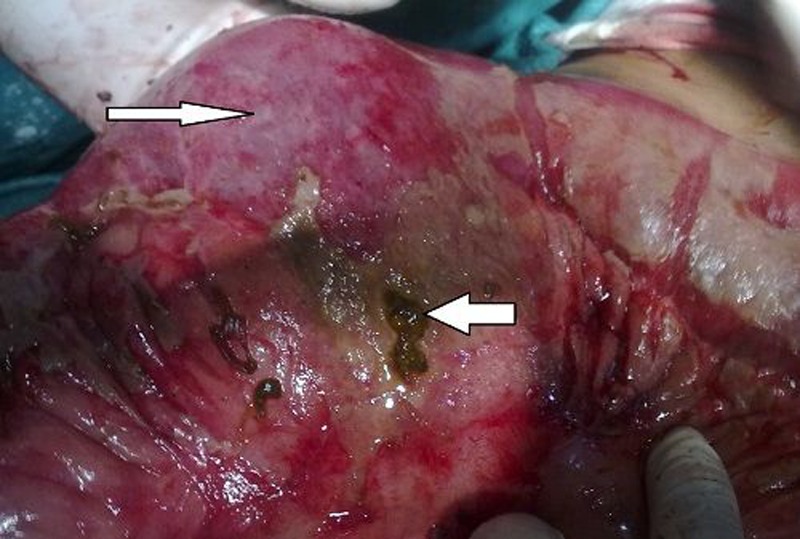
(Narrow arrow) Jejunal diverticulum; (wide arrow) site of perforation with intestinal contents coming out through it.
Outcome and follow-up
The postoperative period was uneventful. The patient was discharged on postoperative day 10. Histopathological examination of the resected specimen revealed evidence of diverticulitis. A full-length colonoscopy and a small bowel barium meal follow through, performed 1 month postoperatively, confirmed the absence of any other intestinal diverticulum.
Discussion
JD, a rare entity, accounts for less than 0.5% of all small gut diverticula.1 It is rarely solitary.2–5 Motor dysfunction of the alimentary smooth muscle or myenteric plexus and the resultant increased intraluminal pressure may have a role in its formation. JD is usually found on the mesenteric border of small bowel, as in our case. The average age of presentation is 62 years, close to that of our patient. Men and women are affected nearly equally. Diverticula of other parts of the gut commonly coexist, with the colon being involved in 35% of cases.6 In the case we report, there were no such diverticula in the rest of the small or large bowel.
JD is usually clinically silent in the absence of complications. Perforation is an infrequent acute complication, with only a few reports in the literature on perforated isolated JD.2 3 Diverticulitis (82%), blunt trauma (12%) and foreign body impaction (6%)6 are reported to predispose to perforation. Cocaine sniffing2 and prolonged use of non-steroidal anti-inflammatory drugs or steroid7 also increase the chances of perforation. Other precipitating factors include distal obstruction due to band adhesion or stricture.8 A mesenteric abscess may result when perforation occurs into the jejunal mesentery.9 This may cause a diagnostic delay because the classical findings of generalised perforative peritonitis may be absent. Other acute complications include bleeding, diverticulitis and intestinal obstruction by enteroliths.10 Chronic complications such as malabsorption, pseudoobstruction and chronic haemorrhage may occur. Surgical intervention is required in 8–30% of patients.1 Mortality rate of complicated JD ranges from 21% to 30%.4
Preoperative diagnosis of perforated JD is difficult. Abdominal and chest X-rays may show free gas under the diaphragm, as in our case. CT scan may demonstrate jejunal thickening, inflammation or localised abscess formation. Diagnostic laparoscopy may be performed in uncertain cases.1 Presentation with perforative peritonitis or obstruction warrants surgical exploration. Laparoscopic management of perforated JD has been reported in the literature.11 The diverticulum is often hidden between the mesenteric leaves, as in our case, and may be difficult to find intraoperatively. In such cases, air insufflation into the jejunum using manual compression or intraoperative enteroscopy may help.12 Knowledge of the typical location of the perforation hidden in between mesenteric leaves is necessary to correctly identify it during exploration. Surgery is also justified in patients with chronic symptoms, in view of associated life-threatening complications.11 Conservative management with intravenous antibiotics and CT-guided aspiration in stable patients with localised collection has also been reported.1
Learning points.
Isolated jejunal diverticulum is a rare entity and usually asymptomatic.
However, it may lead to chronic non-specific abdominal symptoms or rarely an acute complication like perforation.
A high index of suspicion is necessary for prompt diagnosis and treatment.
During exploration, identification of the perforation may be difficult, as it is usually hidden in the mesenteric leaves.
Footnotes
Contributors: AB, SG, SK and UR have contributed equally towards preparation of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Butler JS, Collins CG, McEntee GP. Perforated jejunal diverticula: a case report. J Med Case Rep 2010;4:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albu E, Parikh V, Alankar S, et al. Perforated solitary jejunal diverticulum. South Med J 1995;88:575–6 [DOI] [PubMed] [Google Scholar]
- 3.Dasarathi Murmur Perforated solitary jejunal diverticulum: a rare case report. Int J Biol Med Res 2012;3:1845–7 [Google Scholar]
- 4.Chendrasekhar A, Timberlake GA. Perforated jejunal diverticula: an analysis of reported cases. Am Surg 1995;61:984–8 [PubMed] [Google Scholar]
- 5.Fass G, Colonval P. Perforation and abscess formation of a solitary jejunal diverticulum. Acta Chir Belg. 2007;107:222–4 [PubMed] [Google Scholar]
- 6.Patel VA, Jefferis H, Spiegelberg B, et al. Diverticulosis is not always a silent spectator: a report of 4 cases and review of the literature. World J Gastroenterol 2008;14:5916–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palanivelu C, Rangarajan M, Rajapandian S, et al. Perforation of jejunal diverticula in steroid and non-steroidal anti-inflammatory drug abusers: a case series. World J Surg 2008;32:1420–4 [DOI] [PubMed] [Google Scholar]
- 8.Durai R, Sinha A, Khan M, et al. Ruptured jejunal diverticulum due to a single-band small bowel obstruction. Sci World J 2008;8:934–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gotian A, Katz S. Jejunal diverticulitis with localized perforation and intramesenteric abscess. Am J Gastroenterol 1998;93:1173–5 [DOI] [PubMed] [Google Scholar]
- 10.Woods K, Williams E, Melvin W, et al. Acquired jejunoileal diverticulosis and its complications: a review of the literature. Am Surg 2008;74:849–54 [PubMed] [Google Scholar]
- 11.Garg N, Khullar R, Sharma A, et al. Total laparoscopic management of large complicated jejunal diverticulum. J Min Access Surg 2009;5:115–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goshtasby P, Vasudevan T, Nicholson T. Perforated jejunal diverticulitis. http://www.hcplive.com/publications/surgical-rounds/2006/2006-08/2006-08_06


