Abstract
Adefovir/tenofovir are commonly used antiviral agents in the treatment of chronic hepatitis B infection (CHB). We report a case of CHB-related cirrhosis presenting with sequential femoral neck fractures. Operative reduction and fixation was performed. Laboratory result and imaging was consistent with hypophosphataemic osteomalacia. He had bilateral femoral neck non-union and presented with a new left side subtrochanteric femoral fracture. Corrective osteotomy and cephalomedullary fixation was performed. The fractures healed in 6 months after correction of the hypophosphataemia.
Background
Approximately 350 million people are carriers of the hepatitis B virus (HBV).1 Prevalent in cities like Hong Kong, antiviral therapy is commonly prescribed for disease control and decrease of risk of complications namely, cirrhosis and heptatocellular carcinoma. Adefovir/tenofovir, nucleotide analog reverse transcriptase inhibitors, are commonly used in chronic hepatitis B (CHB). Hypophosphataemic osteomalacia associated with the use of these drugs was reported recently2–4 but there was no case report of management of fracture associated with this situation.
Case presentation
A 60-year-old Chinese man presented to us with a displaced left femoral neck fracture (figure 1) after a fall in January 2011. He did not have any significant bone pain before this injury. He had CHB infection and was prescribed adefovir 10 mg daily since March 2008. Blood test before the injury showed elevated alkaline phosphate of 244 (normal 40–100 IU/L) and a low serum phosphate level of 0.65 (normal 0.82–1.4 mmol/L). Operation of closed reduction and screw fixation (Synthes 7.3 mm short thread titanium cannulated screws) was preformed 6 h after the admission. The fracture reduction and screw purchase was satisfactory. He had persistent left hip pain and radiographs taken 3 months after the operation showed that the fracture did not heal and there was back out of the screws (figure 2).
Figure 1.
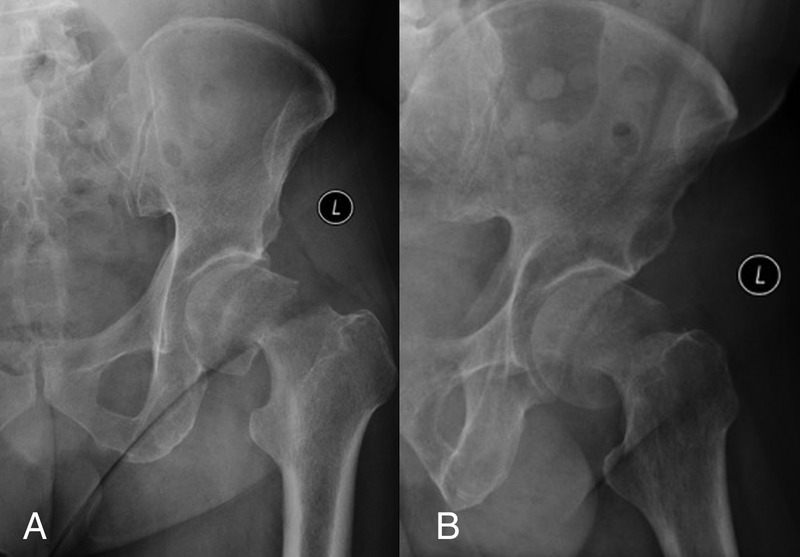
Anteroposterior (A) and lateral (B) radiographs of the left hip showed displaced fracture of the neck of the left femur.
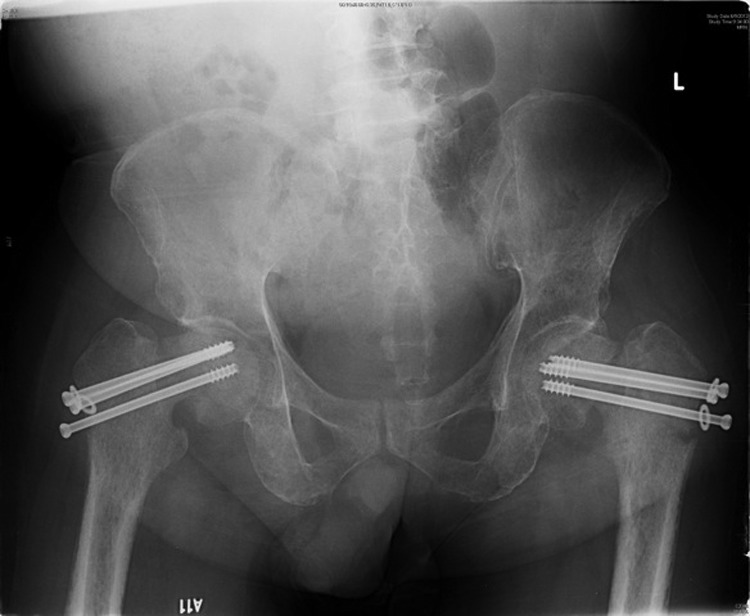
Figure 2.

Radiograph showed back out of the left hip screws and displaced fracture of the neck of the right femur.
He complained of right hip pain 4 months after the operation without any preceding injury. Radiographs showed a displaced fracture of his right femoral neck. Closed reduction and screw fixation (Synthes 7.3 mm short thread titanium cannulated screws) of the fracture was performed.
During subsequent follow-up, radiographs showed bilateral femoral neck non-union with back out of the screws. There was no collapse of the femoral heads (figure 3). He also complained of generalised fatigue and bone pain. Work up for infection was negative. Adefovir was switched to tenofovir 300 mg daily since November 2011 by the physician. He was newly diagnosed to have hepatocellular carcinoma with decompensating cirrhosis in July 2012, so he preferred conservative treatment for his hip condition at that time. Tc-99 MDP bone scan showed metabolic superscan with multiple insufficiency fractures in ribs, spine, articular bones of weight bearing joints, consistent with osteomalacia.
Figure 3.

Screw back out of both hips without radiological evidence of avascular necrosis of the femoral heads.
He complained of increased left hip pain and generalised bone pain. He did not have any preceding history of injury or increase in activity level. Radiograph showed a new subtrochanteric fracture of his left femur. No obvious osteolytic lesion or avascular necrosis of the femur was noticed. There was non-union of the previous fracture of the femoral neck with neck shaft angle of 95° and Pauwel angle of 68° (figure 4). Corrective osteotomy of the left proximal femur was performed. Under general anaesthesia, the previous hip screws were removed. A valgus closing wedge osteotomy was performed at the subtrochanteric fracture site. The femoral neck shaft angle was improved to 125° (figure 5). Cephalomedullary fixation was performed with Stryker Gamma 3 nail. The excised bone wedge was morselised and packed into femoral neck non-union site through the lag screw tract. Non-weight bearing walking was started after the operation. Hypophosphataemia was corrected with oral phosphate supplement. Progressive weight bearing walking was started 3 months after the osteotomy and the patient resumed full weight bearing walking 6 months after the operation.
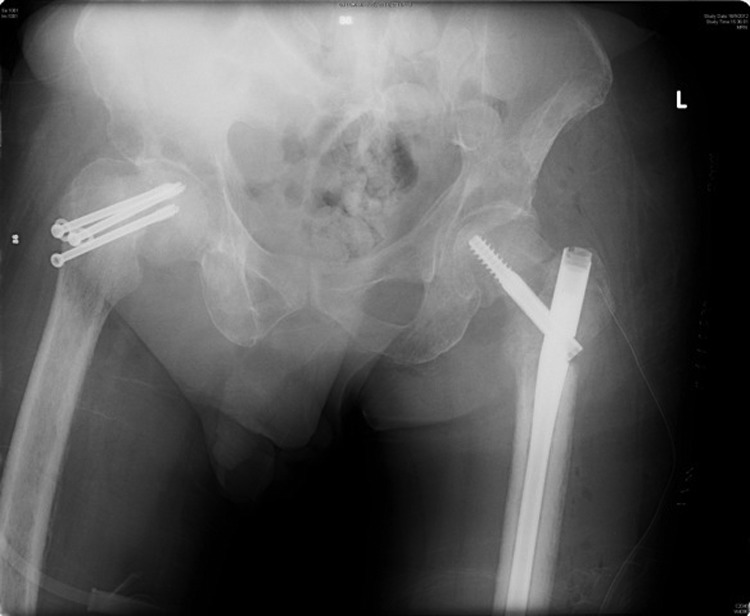
Figure 4.
Radiograph showed left femoral neck non-union with neck shaft angle 95° and Pauwel angle 68°. There was a left subtrochanteric fracture.
Figure 5.
Post osteotomy radiograph showed that the neck shaft angle of the left hip was corrected to 125°.
Investigations
The blood phosphate level was 0.28 mmol/L. The alkaline phosphate level was elevated to 632 (U/L). Calcium, parathyroid hormone and Vitamin D levels were normal. Urine phosphate level was elevated with decreased TMP/GRF ratio to 0.24 mmol/L. Tc-99 MDP bone scan showed metabolic superscan with multiple insufficiency fractures in ribs, spine, articular bones of weight bearing joints, consistency with osteomalacia. Intraoperative bone biopsy was negative for malignancy and infection.
Differential diagnosis
Differential diagnosis of oncogenic osteomalacia was ruled out by bone scan and bone biopsy.
Treatment
For the treatment of osteomalacia, he was put on sandaz phosphate one tab three times a day after the last operation. Tenofovir was kept by the hepatologist.
For the femoral non-union, corrective osteotomy with internal fixation was performed.
Outcome and follow-up
The latest serum phosphate level was normalised and the bone pain was much improved. Radiographs showed fracture union at 6 months time (figure 6).
Figure 6.
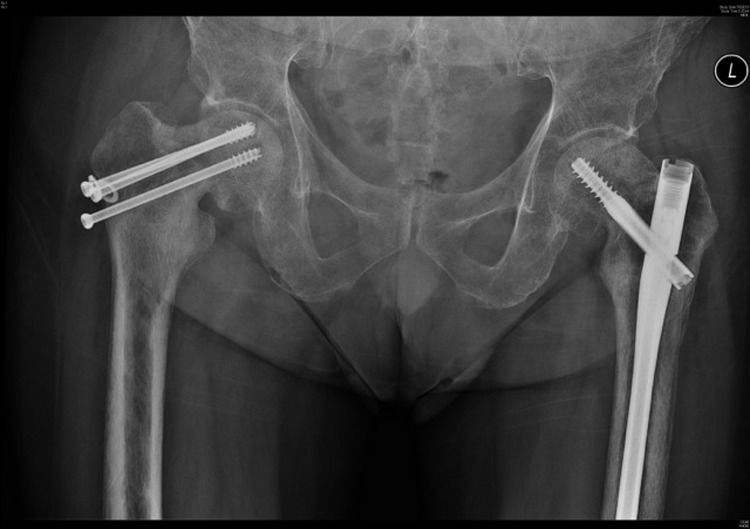
Radiograph taken 6 months after the osteotomy showed both the osteotomy site and femoral neck fracture healed.
Discussion
CHB is common among Chinese and so is the antiviral treatment. Adefovir/tenofovir is demonstrated to have association with impaired reabsorption and urine wasting of phosphate, calcium, magnesium, potassium, sodium, urate, amino acids, glucose and bicarbonate, resulting in hypophosphataemic osteomalacia or progression to complete proximal tubular damage (De Toni-Debré-Fanconi syndrome).
Adult onset hypophosphataemia osteomalacia is rarely encountered in orthopaedic practice.5 6 To the best of our knowledge, there was no publication about fracture management in the presence of hypophosphataemia osteomalacia in the English literature. We believe that the management should include correction of the underlying osteomalacia in addition to fracture reduction and fixation. In our case, since the patient had decompensated cirrhosis and hepatocellular carcinoma, tenofovir was kept by physician as there was no good antiviral alternative. Therefore, the underlying cause of osteomalacia was not reversed. The initial fracture reduction was acceptable but the fixation may not be stable enough in the presence of weak bone. It resulted in progressive varus deformity of the femoral neck and resulted in vertical shearing force across the fracture site. This formed a vicious cycle leading to non-union.
Since there was no avascular necrosis of the femoral head or gross bone resorption at the non-union site, hip joint preservation operation was planned for this patient. Valgus osteotomy was performed to reduce the shear force and to provide compression force at the non-union site.
Hypophosphataemia was found in this patient on initial presentation and a bone scan showed multiple insufficiency fractures pointing to a generalised bone quality deficiency. However, the necessary treatment of phosphate replacement was withheld until the final operation. We believed that this is one of the reasons leading to non-union.
Phosphate supplement corrected the osteomalacia as evident by the improvement of generalised bone pain. The valgus osteotomy together with correction of the underlying osteomalacia provided a good condition for osteogenesis at the non-union site and we believe this is the treatment of choice in this case.
Learning points.
It will be difficult for bone to heal without full nutritional support.
Adefovir/tenofovir may result in hypophosphataemic osteomalacia and so orthopaedic surgeon should be aware of this in chronic hepatitis B (CHB) pandemic region.
Valgus osteotomy can reduce the shear force and provide compression force at the non-union site. This can provide a favourable mechanical environment for the non-union to heal.
Patients with osteomalacia are more prone to have fracture and subsequent bone deformity. This may then give rise to stress fracture in the adjacent site. Treating the underlying cause is the key to success.
Footnotes
Contributors: YKS was responsible for collection of data and completion of the manuscript. THL was responsible for the initiation of the idea and editing of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Yuen MF, Lai CL. Treatment of chronic hepatitis B. Lancet Infect Dis 2001;1:232–41 [DOI] [PubMed] [Google Scholar]
- 2.De Socio GV, Fabbriciani G. Hypophosphatemic osteomalacia associated with tenofovir: a multidisciplinary approach is required. Mediterr J Hematol Infect Dis 2012;4:e2012025–1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong T, Girgis CM. Hypophosphatemic osteomalacia after low-dose adefovir dipivoxil therapy for hepatitis B. J Clin Endocrinol Metab 2010;95:479–80 [DOI] [PubMed] [Google Scholar]
- 4.Wu C, Zhang H. Hypophosphatemic osteomalacia and renal Fanconi syndrome induced by low-dose adefovir dipivoxil: a case report and literature review suggesting ethnic predisposition. J Clin Pharm Ther 2013;38:321–6 [DOI] [PubMed] [Google Scholar]
- 5.Kim S, Park CH, Chung YS. Hypophosphatemic osteomalacia demonstrated by Tc-99 m MDP bone scan: a case report. Clin Nucl Med 2000;25:337–40 [DOI] [PubMed] [Google Scholar]
- 6.Milgram JW, Compere CL. Hypophosphatemic vitamin D refractory osteomalacia with bilateral femoral pseudofractures. Clin Orthop Relat Res 1981;160:78–85 [PubMed] [Google Scholar]


