Abstract
Two patients with cancer requiring removal of specific impalpable lymph nodes for full pathological analysis underwent ultrasound-guided lesion localisation and marking with a low-activity I-125 seed. A gamma probe was used in theatre to localise the signal from the seed and guide excision. Successful removal of the lesions was confirmed with the probe and by specimen radiography. Radioguided Occult Lesion Localisation using I-125 Seeds (“ROLLIS”) provides a method of precisely marking impalpable lesions for surgical excision.
Background
Breast screening programmes worldwide have emphasised the need to accurately localise and surgically remove breast lesions. However, occasionally, it becomes necessary, for diagnostic and/or therapeutic purposes, to accurately localise other impalpable lesions for surgical removal.
Many methods have been developed for impalpable breast lesion localisation, including hookwires, carbon injection, radioactive colloid injection and Iodine 125 (I-125) radioactive seed localisation.
The technical and logistic advantages of radioactive seed localisation offered over the alternative methods of impalpable breast lesion localisation can be exploited for other anatomical sites. In this report, it has been used to accurately and successfully localise and remove specific lymph nodes of interest.
Case presentation
Co-incidentally, two cases presented simultaneously to our institutions with a similar challenge: how to target, localise and remove a specific impalpable axillary lymph node.
Case 1
A 46-year-old woman who had a history of two malignancies presented to us. She had an endometrial cancer 11 years ago treated with hysterectomy and a transitional cell carcinoma (TCC) of the bladder approximately 2.5 years ago treated with neoadjuvant chemotherapy and total cystectomy.
Within the past 12 months, two isolated transitional cell carcinoma metastatic lesions had been identified in the spleen and colon; these had been surgically removed with splenectomy and partial colectomy. As part of her ongoing surveillance, a Flourine-18 fluorodeoxyglucose (F-18 FDG) positron emission tomography CT (PET/CT) scan identified increased uptake in an isolated right axillary lymph node (figure 1). This was clinically impalpable.
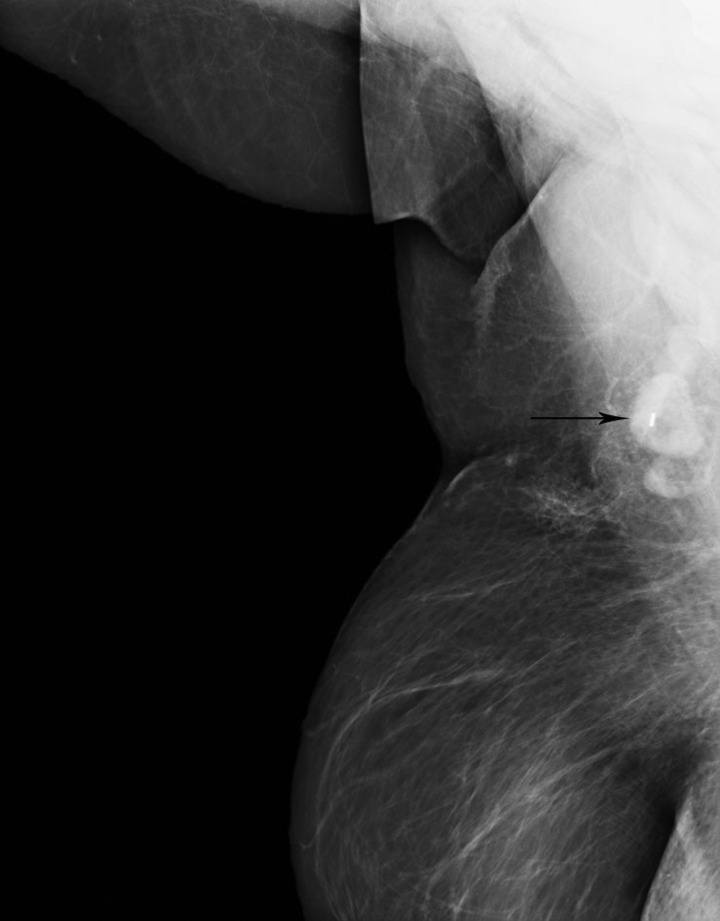
Figure 1.
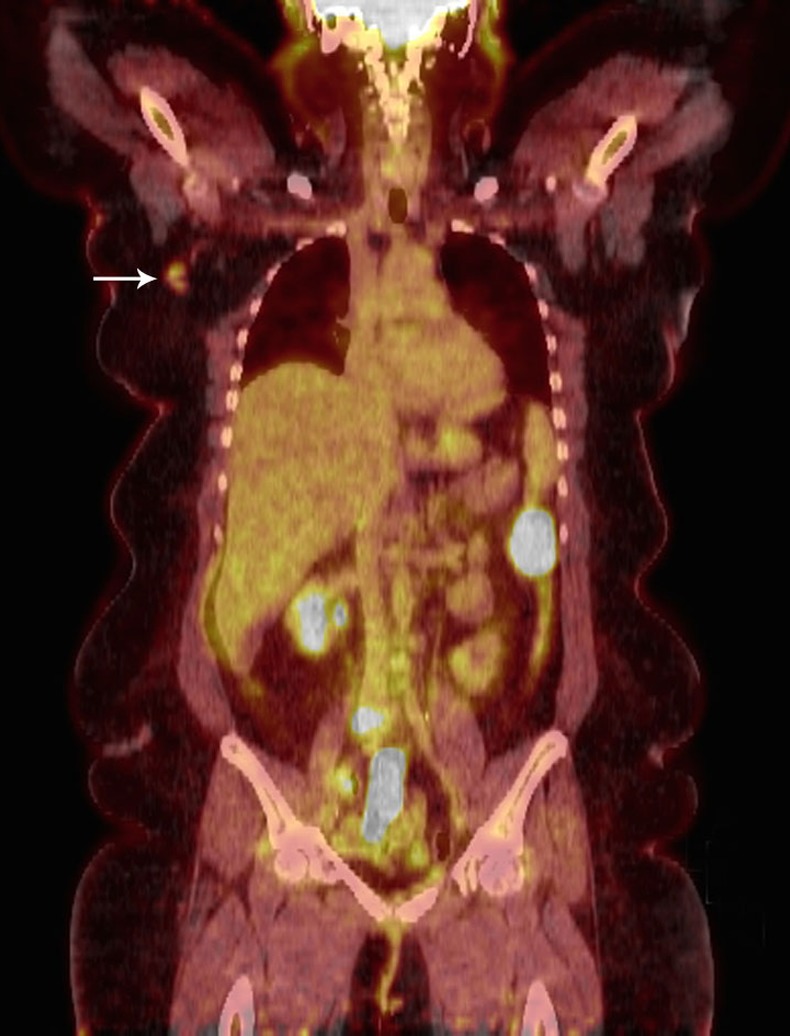
F-18 FDG PET/CT case 1, coronal image. Tracer uptake (arrow) is noted in an abnormal axillary lymph node.
This suspicious right axillary lymph node persisted on follow-up PET scanning, with no other suspicious sites and no other evidence of TCC metastasis. Right axillary ultrasound identified a lymph node with a focally thickened cortex (figure 2A,B) which corresponded with the FDG avid node seen on the PET scan. Ultrasound-guided fine needle aspirate (FNA) of this node was benign; suspicion remained high and she was referred for localisation and retrieval of this node for full histological analysis.
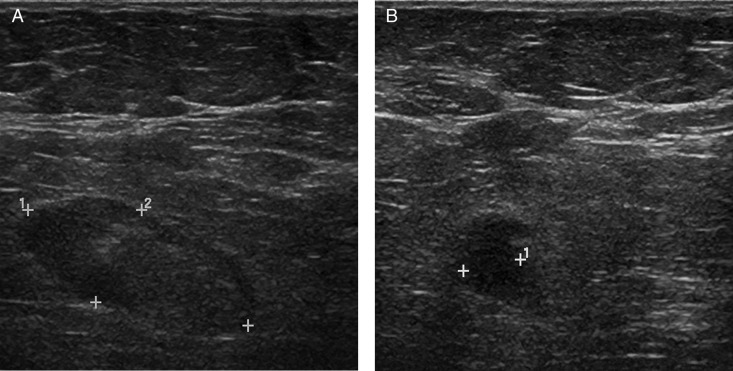
Figure 2.
Ultrasound of lymph node, case 1: (A) long axis view and (B) short axis view. The cortex is focally thickened and hypoechoic.
Case 2
A 65-year-old woman was referred with a palpable right lower outer quadrant (8 o’clock position) breast mass to SCGH Breast Centre. Mammography demonstrated a 25 mm poorly defined non-calcified mass with spiculated margins (figure 3A,B). A core biopsy diagnosis of breast malignancy was made. Ultrasound-guided FNA of a morphologically abnormal lymph node in the axillary tail of the breast (figure 4A,B) was also malignant.
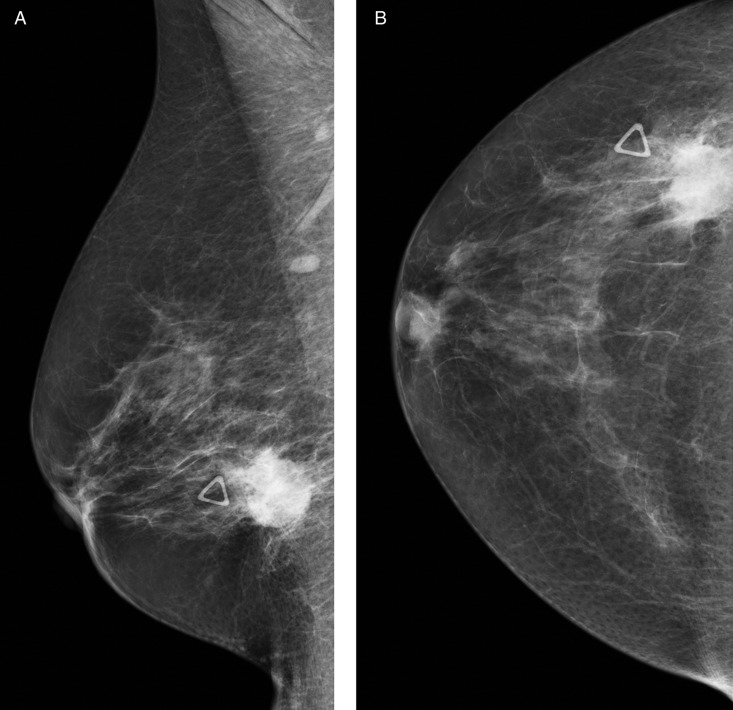
Figure 3.
Right mammogram, case 2: (A) oblique view and (B) craniocaudal view. Marker denotes palpable mass.
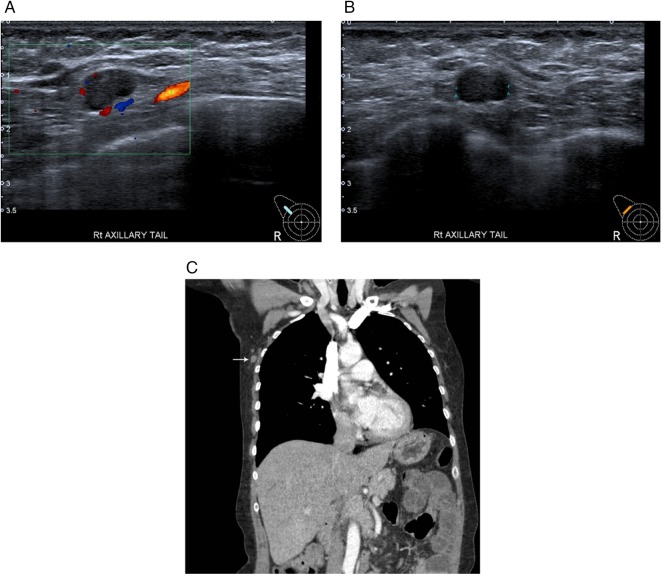
Figure 4.
(A–C) Lymph node imaging case 2. (A) Ultrasound long axis view. (B) Ultrasound short axis view. Focal and generalised cortical thickening is present. (C) Thoracic CT coronal image. Note that the node (arrow) lies 12 cm from the nipple in the axillary tail of the breast.
Wide local excision and axillary clearance found a 24 mm grade III invasive duct carcinoma, ER+/PR+/HER2+. However, axillary clearance of 15 nodes was negative for carcinoma.
A postoperative ultrasound again identified the node previously sampled surrounded by breast tissue in the axillary tail of the breast. The location of this involved (sentinel) node is shown in the coronal image from the preoperative staging CT (figure 4C).
Treatment
In both cases, accurate retrieval of impalpable axillary nodes was required; one was diagnostic and the other was therapeutic. Both institutions had developed skill in the use of I-125 seeds for localisation of impalpable breast lesions during a pilot study in 2011; however, neither site had used seeds to localise non-breast lesions.
In each of the cases, a single low-activity (approximately 0.06 mCi) I-125 seed was inserted into the target node using ultrasound guidance (figure 5A,B), with preoperative mammographic confirmation in case 2 (figure 6). Intraoperative gamma probes (Navigator GPS, Dynasil Products, Massachusetts, USA; Neo-Probe neo2000 GDS, Devicor Medical Products, Inc.) were used to successfully identify and remove the localised nodes, with specimen X-ray proof of successful seed-localised node retrieval (figure 7A,B). Localisation and surgery were carried out as same day procedures, and there were no complications.
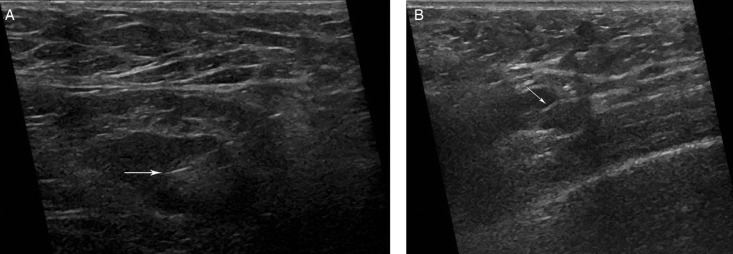
Figure 5.
Insertion of I-125 seeds using ultrasound guidance. (A) Case 1 long axis during seed insertion. (B) Case 1 short axis seed in situ.
Figure 6.
Oblique mammographic view of right axilla in case 1. Accurate seed placement within the hilum of the abnormal lymph node is confirmed.
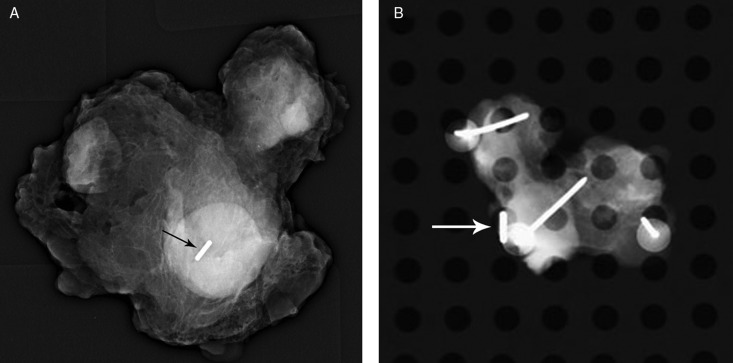
Figure 7.
Specimen radiographs of tissue removed from axillae. Note the presence of a radio-opaque I-125 seed (arrow) within a mass corresponding to the abnormal lymph node in each case: (A) case 1 and (B) case 2.
Outcome and follow-up
In case 1, pathology of the node showed inflammatory changes only, with no evidence of malignancy. A follow-up PET scan showed resolution of the previously identified right axillary node (figure 8), providing confirmation of successful localisation and retrieval of the node of interest.
Figure 8.
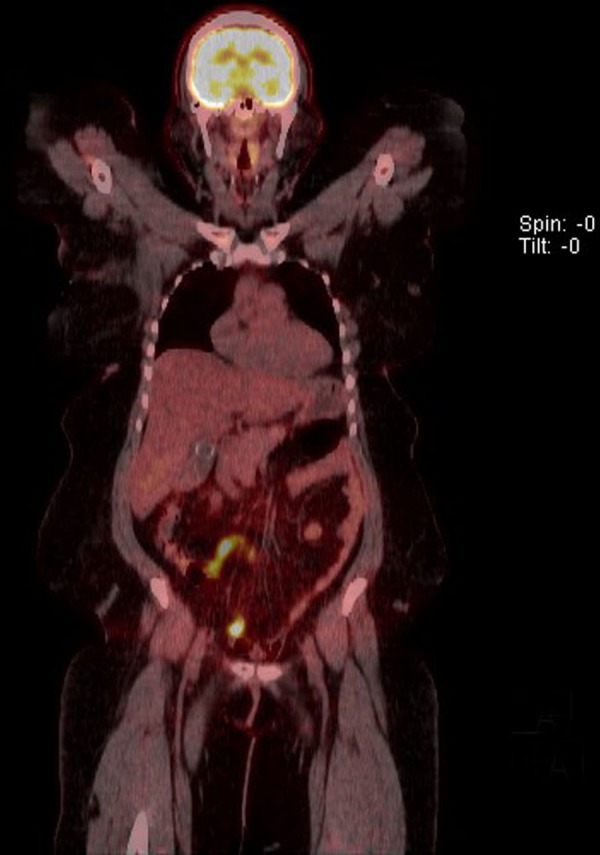
Coronal view postoperative F-18 FDG PET-CT scan, case 1. No residual tracer uptake is seen in the right axilla. Minor postoperative fat stranding is noted.
In case 2, final histology revealed 8 mm tumour deposit in the node with no extranodal spread. Postoperative management included chemotherapy, radiotherapy and endocrine therapy.
No significant postoperative complications were experienced by either patient.
Discussion
Radioguided occult lesion localisation of impalpable breast lesions using low-activity I-125 seeds (“ROLLIS”) has been described by many authors1–4 and is the technique of choice in some centres in the USA and the Netherlands. The ROLLIS technique uses the same hand-held gamma probe commonly used to guide sentinel lymph node biopsy and most probes have the ability to selectively detect signals from either Tc99m (used for the sentinel node) or I-125 (within the seed).
While the insertion of I-125 seeds into many other body organs has been described for tumour brachytherapy, there are a few reports describing the use of seeds for lesion localisation, other than in the breast.
Recently, Straver et al5 inserted a single low-activity seed into a pathologically proven metastatic axillary lymph node prior to the commencement of neoadjuvant chemotherapy in 15 patients to mark the node for later removal. All the marked nodes were successfully removed and the radiologists and surgeons reported no difficulty with the technique.
The ROLLIS technique offers many advantages over other localisation methods. As I-125 has a 59-day half-life, the insertion procedure can be performed several days in advance of surgery, enabling flexible use of theatre bookings and improved patient convenience. Unlike hook-wires, seeds rarely move after insertion,6 7 making surgical failure less likely. The localised source of emissions provided by the seed allows precise localisation of the lesion. This provides continuous three-dimensional feedback as to the location of the centre of the lesion during removal.
The use of an I-125 seed for lesion localisation helps to minimise the dissection required to find the lesion and the risk of damage to adjacent vital structures. Reducing the amount of surrounding normal tissue that needs to be removed also reduces the chance of obtaining poor cosmetic results. Liquid colloid labelled with Tc99m can also be used for radioguided lesion localisation. However, these compounds can diffuse from the injection site, thereby reducing the precision of localisation. They are not radiopaque, making confirmation of correct labelling of the target lesion and its removal within the excised tissue more difficult.
Immediate confirmation of successful removal of a seed localised lesion can be obtained by noting the absence of counts in the surgical bed and high counts within the excised tissue. The radiopaque nature of the seed facilitates X-ray confirmation of the initial correct seed placement and presence of the seed within the excised tissue.
As the I-125 seeds used are of low activity, the radiation dose received by the patient, family and staff during the ROLLIS procedure is very low, even if the seed is left in place for several days. Special precautions are not usually needed. It is important to note, however, that as the seed is a sealed source of radioactivity, it must by law be accounted for at all times, meaning that a strict seed handling protocol and tracking system are required.
The I-125 seeds used for ROLLIS are commercially available as single preloaded seed-needle kits.
Learning points.
I-125 radioactive seed localisation can be used to precisely mark specific lymph nodes of interest and guide their removal.
Radioactive seed localisation can be used to target, localise and remove non-breast lesions using the current readily available technology.
Radioguided occult lesion localisation using low-activity I-125 seeds is a safe procedure, with minimal radiation dose to the patient and no significant radiation doses received by staff.
A seed handling protocol is necessary to ensure that all seeds are tracked from insertion to removal and returned to the physics department for safe storage and decay.
Footnotes
Contributors: LJ, DT and AGB contributed to the study concept and design, DT, LJ, AGB, FAA contributed to the acquisition, analysis and interpretation of data, and critically reviewed the manuscript, and LJ, DT and AGB were involved in the drafting of manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gray RJ, Salud C, Nguyen K, et al. Randomized prospective evaluation of a novel technique for biopsy or lumpectomy of nonpalpable breast lesions: radioactive seed versus wire localization. Ann Surg Oncol 2001;8:711–15 [DOI] [PubMed] [Google Scholar]
- 2.Lovrics PJ, Goldsmith CH, Hodgson N, et al. A multicentered, randomized, controlled trial comparing radioguided seed localization to standard wire localization for nonpalpable, invasive and in situ breast carcinomas. Ann Surg Oncol 2011;18:3407–14 [DOI] [PubMed] [Google Scholar]
- 3.Sung JS, King V, Thornton CM, et al. Safety and efficacy of radioactive seed localization with I-125 prior to lumpectomy and/or excisional biopsy. Eur J Radiol 2013;82:1453–7 [DOI] [PubMed] [Google Scholar]
- 4.van Riet YE, Jansen FH, van Beek M, et al. Localization of non-palpable breast cancer using a radiolabelled titanium seed. Br J Surg 2010;97:1240–5 [DOI] [PubMed] [Google Scholar]
- 5.Straver ME, Loo CE, Alderliesten T, et al. Marking the axilla with radioactive iodine seeds (MARI procedure) may reduce the need for axillary dissection after neoadjuvant chemotherapy for breast cancer. Br J Surg 2009;97:1226–31 [DOI] [PubMed] [Google Scholar]
- 6.Alderliesten T, Loo CE, Pengel KE, et al. Radioactive seed localization of breast lesions: an adequate localization method without seed migration. Breast J 2011;17:594–601 [DOI] [PubMed] [Google Scholar]
- 7.Jackson LR, Taylor DB. Superior non-migration of radioactive seed for impalpable breast lesion localization. ANZ J Surg 2012;82:187–8 [DOI] [PubMed] [Google Scholar]