Abstract
Hemiconvulsion-hemiplegia-epilepsy (HHE) syndrome involves initial sudden and prolonged unilateral convulsive seizures, followed by transient or permanent hemiplegia and epilepsy during infancy or early childhood. Seizures are prolonged, difficult to control and sometimes may require surgery. Hemiplegia varies in intensity, differs from Todd paralysis and disappears in about 20% of cases. Neuroimaging characteristically shows brain atrophy more pronounced on the hemisphere contralateral to the side of hemiplegia with dilation of the ventricular system. A 20-month-old girl presented with left hemiconvulsions and left hemiplegia lasting for a prolonged period. Seizures failed to resolve with various anticonvulsants even after many physician contacts. Characteristic neuroimaging findings, seizure control with carbamazepine and valproate, subsequent recovery of hemiplegia and attainment of developmental milestones observed on follow-up confirmed HHE syndrome. The case highlights the need for good seizure control in this syndrome.
Background
Hemiconvulsion-hemiplegia-epilepsy (HHE) syndrome is defined by a prolonged unilateral seizure followed by the development of a hemiplegia ipsilateral to the side of the convulsion. The condition occurs in children younger than 4 years of age.1–3 The most common age of onset is between 5 months and 2 years but the youngest age of 1.5 months has been reported.4 Seizures may be simple partial seizures (33%), partial seizures with secondary generalisation (20%) and repeated episodes of status epilepticus (10%). Hemiplegia is initially flaccid and fairly massive, but tends to become spastic over a period of time. Although hemiplegia is usually permanent, it may disappear in about 20% of cases. HHE syndrome associated with certain underlying conditions and idiopathic forms has been described. The authors report the syndrome and its course in a 20-month-old girl.
Case presentation
A 20-month-old girl was referred to us with a history of recurrent episodes of left-sided hemiconvulsions since 1 month of age followed by ipsilateral weakness of limbs and failure of routine anticonvulsant medications. Convulsions involved left-sided limbs and face, lasted for 10–30 min with a frequency of 10–15/day. Her symptoms worsened and limb weakness deteriorated in the past 1 month with no relief from various physician and neurologist contacts. Her history revealed usage of phenobarbitone, clobazam, sodium valproate, levetiracetam and complimentary medicines with transient partial relief or no relief. Her birth history was normal and she weighed 2750 g at birth. She received immunisation as per schedule. There was no family history of seizure. Attainment of developmental milestones was delayed particularly in the gross motor domain. On examination, her growth was normal and head circumference was 46 cm. Developmental quotient was <50% in gross motor, 60% in fine motor, >70% in language and >75% in personal social domain. There were no dysmorphic features or neurocutaneous markers. Vital sings including blood pressure was normal. Cardiovascular, respiratory and abdomen examinations were normal. Central nervous system examination revealed conscious child with normal cranial nerves and fundus, left hemiplegia with hypertonia, grade 0 power, hypereflexia and extensor plantar reflex.
Investigations
Laboratory tests revealed normal complete blood counts, blood lactate, ammonia and arterial blood gas analysis. Antinuclear antibodies and urine metabolic screen for homocystinuria were negative. Vision and hearing assessments were normal. EEG showed generalised sharp waves and mild slow waves with low-voltage background activity. A CT of the brain showed prominence of ventricles and cisternal spaces, suggesting diffuse cerebral atrophy (figure 1A). Asymmetric prominence of the right temporal horn (figure 1B), prominent extra-axial space in the right frontal region and asymmetrically dilated right lateral ventricle (figure 1C) suggested predominant right hemicerebral atrophy.
Figure 1.
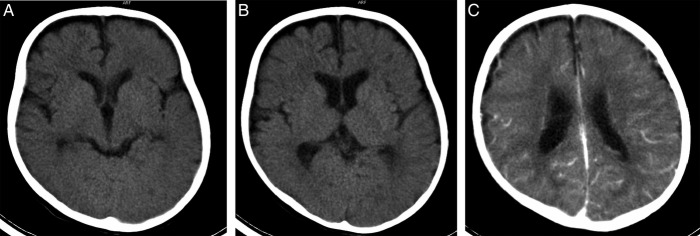
CT of the brain showing the prominence of ventricles and cisternal spaces, suggestive of diffuse cerebral atrophy (A), asymmetric prominence of the right temporal horn (B), prominent extra-axial space in the right frontal region and asymmetrically dilated right lateral ventricle (C) suggesting predominant right hemisphere atrophy.
Treatment
The patient was put on carbamazepine 10 mg/kg/day and valproate 20 mg/kg/day. Physiotherapy for affected limbs was continued. Seizures were decreased in frequency by day 4 and she remained seizure free on day 6 and was hence discharged.
Outcome and follow-up
On follow-ups, 5 months later she was seizure free and able to stand with support; after 11 months, tone normalised on the left side, could walk normally and after 2 years, she had normal gait and age-appropriate developmental milestones.
Discussion
HHE syndrome is characterised by clonic epileptic seizures of long duration affecting one side of the body in children under 4 years of age. Subsequently, a hemiplegia of varying intensity develops on the same side.1–4 In the present case, seizures involved the left side of the body and persisted until 20 months.
Several aetiologies for the initial seizures in HHE syndrome have been proposed. They include meningitis, subdural effusions, perinatal or prenatal onset hemispheric small lesions, trauma, protein S deficiency and L2 hydroxyglutaric aciduria.2–5 The ischaemic theory, however, was not generally agreed on as it fails to explain the general atrophy of the hemisphere in the absence of ischaemic lesions. In many patients, no obvious cause was found. In the present case, no aetiology could be identified.
In the beginning of the disease course, seizures may be associated with a febrile illness. However, repeated febrile and afebrile seizures since infancy have been reported.1 Seizures may be simple partial, partial with secondary generalisation or status epilepticus in nature.4 Generalised tonic–clonic seizures have also been explained with this condition.5 EEG shows ipsilateral slowing and low voltage of background activity. The present case had partial seizures with similar EEG findings. The associated hemiplegia may vary in intensity. Hemiplegia may clear in about 20% of patients but subtle pyramidal signs may remain.5 The present case had initial dense hemiplegia which recovered following seizure control.
The pathological features of HHE syndrome identified with neuroimaging include acute oedema of the affected hemisphere often followed by the development of volume loss.3 Cerebral hemiatrophy is a consistent finding in all patients by cranial CT and/or MRI.2–6 Furthermore, vasospasms of cerebral vascular smooth muscle has been proposed as the mechanism of seizure by Yamazaki et al.2 Potential risk of HHE with severe myoclonic epilepsy in infancy has been proposed by Sakakibara et al.1
The standard treatment of HHE syndrome involves medical treatment as there is no curative treatment. Medical therapy aims at satisfactory control of seizures. Carbamazepine and/or phenobarbitone have been used with good control of seizures.4–6 We found good seizure control with carbamazepine and valproate. Surgical treatment with hemispherectomy and corpus callosotomy has been found successful in refractory cases.3 7
In conclusion, in young children with hemiconvulsion and hemiplegia, EEG and characteristic neuroimaging abnormalities further help in diagnosis of HHE syndrome. A seizure control can help in the recovery of hemiplegia and achievement of developmental milestones in young children.
Learning points.
In hemiconvulsion-hemiplegia-epilepsy syndrome, prolonged hemiconvulsions lead to hemiplegia of varied intensity and substantial morbidity.
Clinical course, EEG and characteristic neuroimaging features aid in proper diagnosis.
Adequate seizure control with appropriate anticonvulsants leads to recovery of hemiplegia and facilitates attainment of further developmental milestones in a growing young child.
Footnotes
Contributors: RYB and SK involved in treatment of the case. RBY wrote the manuscript. KP provided expert radiological inputs. All authors approved the final manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sakakibara T, Nakagawa E, Saito Y, et al. Hemiconvulsion hemiplegia syndrome in a patient with severe myoclonic epilepsy in infancy. Epilepsia 2009;50:2158–62 [DOI] [PubMed] [Google Scholar]
- 2.Yamazaki S, Ikeno K, Abe T, et al. Hemiconvulsion-hemiplegia-epilepsy syndrome associated with CACNA1A S218L mutation. Pediatr Neurol 2011;45:193–6 [DOI] [PubMed] [Google Scholar]
- 3.Holland KD, Buchhalter J. Hemiconvulsion-hemiplegia-epilepsy syndrome: another case for epilepsy surgery. Neurology 2008;70:2097–8 [DOI] [PubMed] [Google Scholar]
- 4.Ashrafi MR, Tafarroji J. Hemiconvulsion-hemiplegia-epilepsy syndrome. Iran J Child Neurology 2008;3:55–8 [Google Scholar]
- 5.Salih MA, Kabiraj M, Al-Jarallah AS, et al. Hemiconvulsion-hemiplegia-epilepsy syndrome: a clinical, electroencephalographic and neuroradiological study. Childs Nerv Syst 1997;13:257–63 [DOI] [PubMed] [Google Scholar]
- 6.Toldo I, Calderone M, Boniver C, et al. Syndrome: early MRI findings, Brain Dev 2007;29:109–11 [DOI] [PubMed] [Google Scholar]
- 7.Devlin AM, Cross JH, Harkness W, et al. Clinical outcomes of hemispherectomy for epilepsy in childhood and adolescence. Brain 2003;126:556–66 [DOI] [PubMed] [Google Scholar]


