Structure Summary
Objective
Although not previously reported, experience suggests that dentoalveolar injury (DAI) is common among patients with maxillofacial (MF) fractures. The objective of this study was to evaluate and describe the prevalence and nature of DAIs in patients identified with MF fractures.
Methods
Medical records of 43 dogs and cats diagnosed with MF fractures between 2005–2012 were reviewed to identify patients with concurrent DAI. Medical records of patients with DAI were abstracted for the following information: signalment (including sex, age, and skull type), mechanism of MF trauma, location and number of MF fractures, DAI type and location and the number of DAI per patient. Statistical evaluation was performed to determine associations between signalment; mechanism of trauma; location and number of MF fractures; and the prevalence and nature of concurrent DAI.
Results
Dentoalveolar injuries are common among patients with MF trauma. Age and mechanism of trauma are significant predictors of the presence of DAI in patients with MF trauma.
Conclusions and Clinical Relevance
The findings of this study serve to encourage veterinarians to fully assess the oral cavity in patients with MF fractures as DAI are common and can be predicted by age and mechanism of trauma.
Introduction
The pet owning public increasingly values the canine and feline dentition from a functional and cosmetic point of view, a perspective that is not loosely held. When faced with considering treatment options for maxillofacial (MF) trauma, owners not only focus on life-saving treatment and effective and timely treatment of MF fractures, but also other body systems and the overall long-term quality of life for their pet after treatment. Unaddressed dentoalveolar injury (DAI) may cause years of pain and chronic inflammation in dogs and cats. In addition, many DAI require timely recognition in order to render the most appropriate treatment. For this reason, proper appreciation for, and evaluation of, the health status of the entire patient, including the dentition, should be a priority.
Presently, it is unclear how common DAI are in MF trauma patients but experience suggests it is common. The purpose of this study was to: 1) Identify and report the incidence and nature of DAI in patients treated for MF fractures and 2) Investigate any associations between the nature of the MF fractures and the nature of concurrent DAI. It was hypothesized that DAI would be common among patients with MF fractures and that there would be significant associations between the nature of MF fractures (mechanism of trauma, region of the MF apparatus fractured, etc.) and the nature of DAI.
Materials and Methods
Patients diagnosed with MF fractures between 2005 and 2012 within the Dentistry and Oral Surgery Section, University of Wisconsin-Madison Veterinary Medical Teaching Hospital were identified from the section database. Patients diagnosed with fractures of the MF region were included in the study. Exclusion criteria included: 1) patients who had sustained DAI without concurrent MF fractures; and 2) patients diagnosed with MF fractures sustained from causes other than trauma (i.e. pathologic fractures secondary to periodontal disease, severe osteomyelitis, neoplasia).
Medical records were abstracted for the following information: signalment (including sex, age, and skull type); mechanism of trauma; region and number of MF fractures; and type, location and number of DAI per patient.
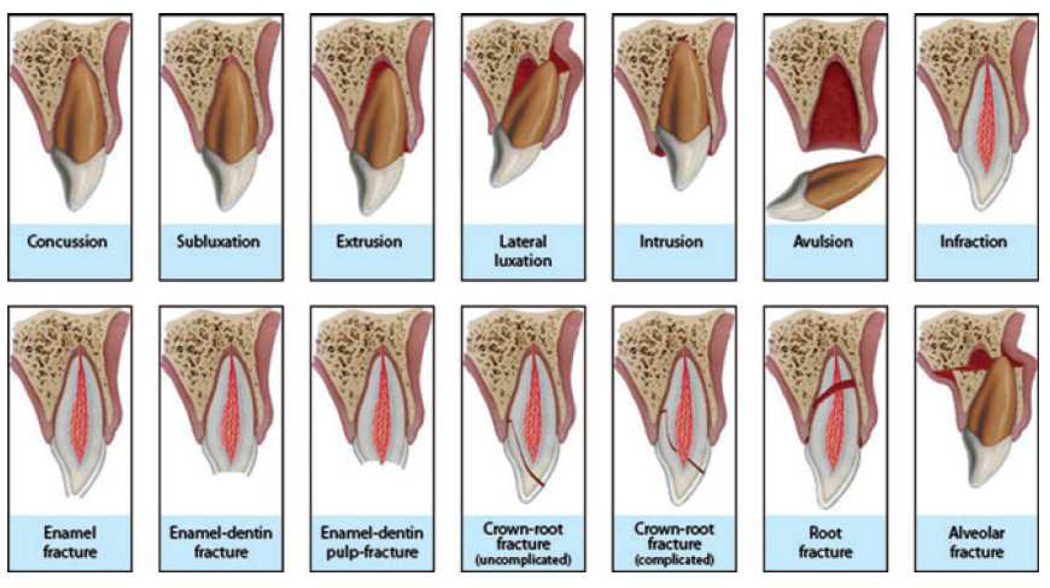
The type of DAI sustained was classified as: 1) dental concussive injury (clinical or radiographic evidence of tooth non-vitality in the region of trauma at the time of initial treatment or at the time of follow-up treatment up to one year after the injury); 2) crown fracture (+/− pulp exposure); 3) root fracture (+/− crown fracture); 4) displacement (subluxation, luxation, intrusion, extrusion); 5) avulsion; and 6) trauma to un-erupted permanent tooth bud. (Figure 1) The DAI were also classified as either severe or non-severe. For the purposes of this study root fracture, displacement and avulsion injuries were considered severe and dental concussion, crown fracture and trauma to the permanent tooth bud were considered non-severe.
Figure 1.
Classification of dentoalveolar injuries adopted by the International Association of Dental Traumatology and used as the basis for the classification within this study. (Reprinted with permission from Andreasen JO, Lauridsen E, Gerds AT, et al. Dental Trauma Guide: A source of evidence-based treatment guidelines for dental trauma. Dent Traumatol 2012;28:142–147.)
The location of DAI was classified as either mandibular or maxillary and further classified as either incisor, canine, premolar or molar.
Patients were classified according to age at the time of the injury. Patients were classified as paediatric/juvenile (< 3 yrs) or adult (> 3 yrs). Adults were further classified into age groups 3–6 yrs, 7–10 yrs, and >10 yrs.
The mechanism of trauma was classified as: 1) unknown; 2) play accident; 3) altercation with another animal; 4) miscellaneous accident; 5) motor vehicle accident; 6) hit by object; and 7) fall from height.
The region of MF fracture sustained was categorized as either: 1) Upper third (cranial unit including the frontal bone, temporal bone and bones of the skull base); 2) Middle third (mid-face unit including nasal, maxillary palatoalveolar, zygomatic and orbitoethmoidal fractures); 3) Lower third (mandibular unit including the mandibular body/symphysis and mandibular angle/ramus/condylar process); and 4) Combination [any combination of the above fracture types, including pan-facial (when all MF thirds were fractured)].
Patients with MF fractures were separated into two groups based on the presence or absence of DAI and compared. In addition, patients identified with DAI were separated into two groups according to the severity of the injury (severe and not severe). Patient characteristics were summarized with frequencies and percentages. Associations between characteristics and DAI group and between characteristics and DAI severity were assessed with Fisher's exact tests. All tests were conducted at a 0.05 significance level.
Results
Forty-four patients were identified with traumatic MF fractures within the study period. One patient was removed from the study due to incomplete medical records. Descriptive statistics for the remaining 43 patients are shown in Table 1. Male patients were overrepresented (55.8%) compared to female patients (44.2%). Most patients (76.7%) were neutered. The age of the patients ranged from 2 months to 15 years (mean and median = 1 year). The largest age group, patients < 3 years of age, comprised 62.8 % of the patients. The most common skull type was mesaticephalic at 67.4%. Only 4.7% of the population was dolichocephalic. Altercation with another animal was the most common mechanism of trauma (34.9%). In 23.3% of the patients, the mechanism of trauma was unknown. Motor vehicle accident was the second most common mechanism at 16.3%. The most common region of MF fracture was the lower third (72%). No patients suffered exclusively upper third injuries. A total of 62 DAI were diagnosed in 31 patients (72.1%) providing a mean of two DAI per patient. One DAI was diagnosed in 17 patients (54.8%). Seven patients (22.6%) sustained two DAI. Only two patients (6.5%) had three DAI. Five patients (16.1%) had four or more DAI.
Table I.
Descriptive statistics of the study population.
| Totals | |
|---|---|
| Sample Size | 43 |
| Sex | |
| Male (n = 24) | |
| Intact | 7 |
| Neutered | 17 |
| Female (n = 19) | |
| Intact | 3 |
| Spayed | 16 |
| Age (years) | |
| Range | 0.16 – 15 |
| Mean | 1 |
| Median | 1 |
| < 3 | 27 |
| 3 – 6 | 5 |
| 7 – 10 | 6 |
| >10 | 5 |
| Skull Type | |
| Brachycephalic | 12 |
| Mesaticephalic | 29 |
| Dolicocephalic | 2 |
| Mechanism of Trauma | |
| Unknown | 10 |
| Play | 2 |
| Altercation with Animal | 15 |
| Miscellaneous Accident | 2 |
| Motor Vehicle Accident | 7 |
| Hit by Object | 6 |
| Fall from Height | 1 |
| Region of MF Fracture | |
| Exclusively Upper Third | 0 |
| Exclusively Middle Third | 4 |
| Exclusively Lower Third | 31 |
| Combination | 8 |
| Number of MF Regions Fractured | |
| 1 | 28 |
| 2 | 11 |
| 3 | 2 |
| 4 | 2 |
Table 2 reviews the types of DAI seen and their locations. The most common types of DAI were root (30.6%) and crown (29%) fractures. Mandibular teeth represented the more commonly affected jaw (34 teeth; 54.8%). While most crown fractures (66.6%), and avulsions (80%) occurred in the maxilla, most root fractures (63.2%), displacements (87.5%) and concussions (80%) occurred in the mandible. Most injuries (37%) occurred in the incisor region, which was the most affected region in the maxilla. The most commonly affected region in the mandible was the molar region (35.3%).
Table 2.
Type and location of DAI diagnosed in patients with MF fracture. PTB = permanent tooth bud
| Type of DAI | ||||||||
|---|---|---|---|---|---|---|---|---|
| Location | Crown Fracture |
Root Fracture |
Displacement | Avulsion | Concussion | PTB Trauma |
Total | |
| Mandible | (n = 6) | (n = 12) | (n = 7) | (n = 1) | (n = 4) | (n = 4) | (n = 34) | |
| Incisor | 0 | 7 | 2 | 1 | 1 | 0 | 11 | |
| Canine | 2 | 1 | 1 | 0 | 3 | 1 | 8 | |
| Premolar | 2 | 0 | 1 | 0 | 0 | 0 | 3 | |
| Molar | 2 | 4 | 3 | 0 | 0 | 3 | 12 | |
| Maxilla | (n = 12) | (n = 7) | (n = 1) | (n = 4) | (n = 1) | (n = 3) | (n = 28) | |
| Incisor | 4 | 2 | 0 | 4 | 1 | 1 | 12 | |
| Canine | 6 | 0 | 1 | 0 | 0 | 1 | 8 | |
| Premolar | 2 | 5 | 0 | 0 | 0 | 1 | 8 | |
| Molar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total | (n = 18) | (n = 19) | (n = 8) | (n = 5) | (n = 5) | (n = 7) | (n = 62) | |
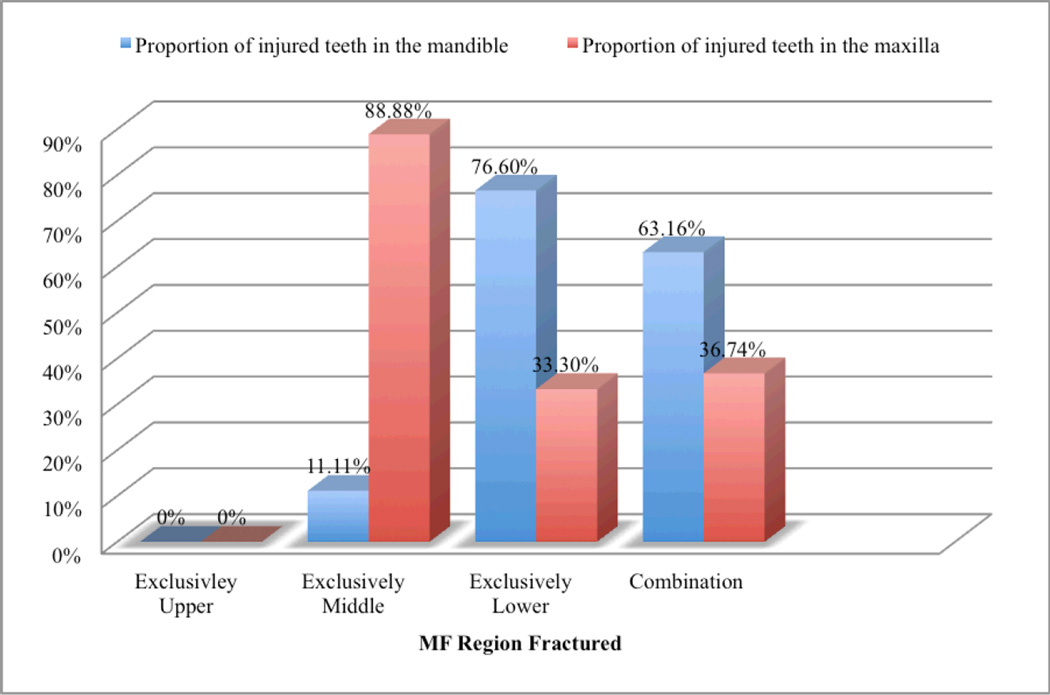
Figure 2 depicts the relative proportion of injured teeth in the maxilla and mandible as they relate to the MF region fractured. When the fractures exclusively involved the middle third, most DAI (88.88%) were maxillary. On the contrary, when the fractures exclusively involved the lower third, most DAI (76.6%) were located in the mandible. Overall, there was a disparity between maxillary (36.74%) and mandibular (63.16%) DAI.
Figure 2.
Proportion of mandibular versus maxillary DAI per MF region fractured.
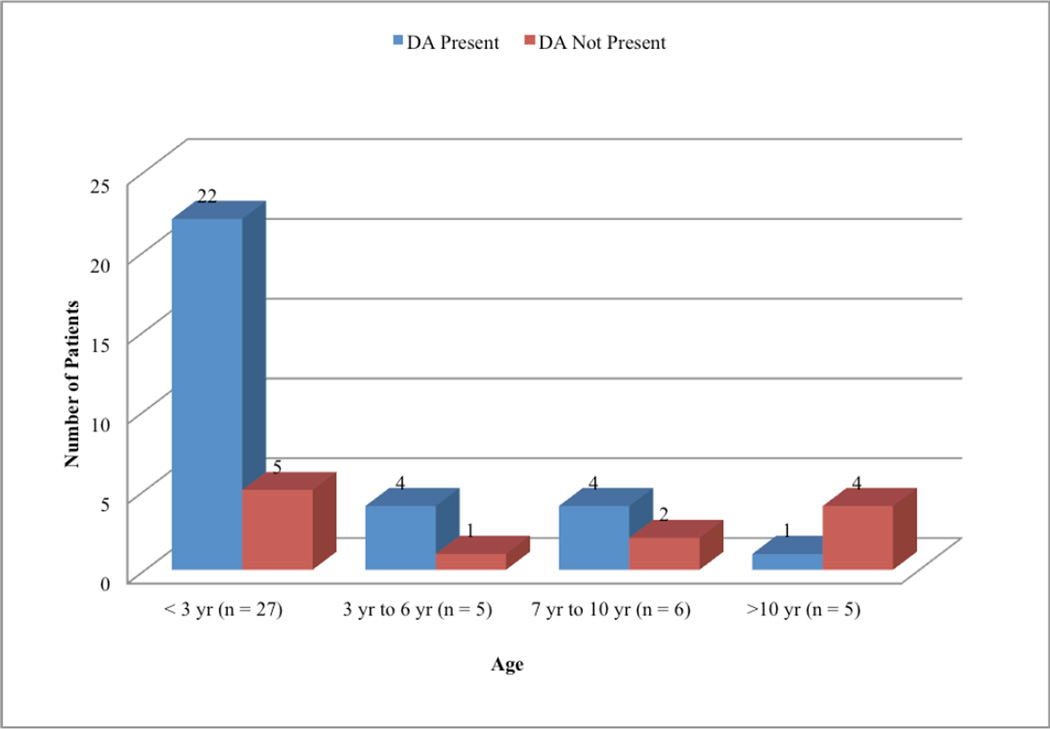
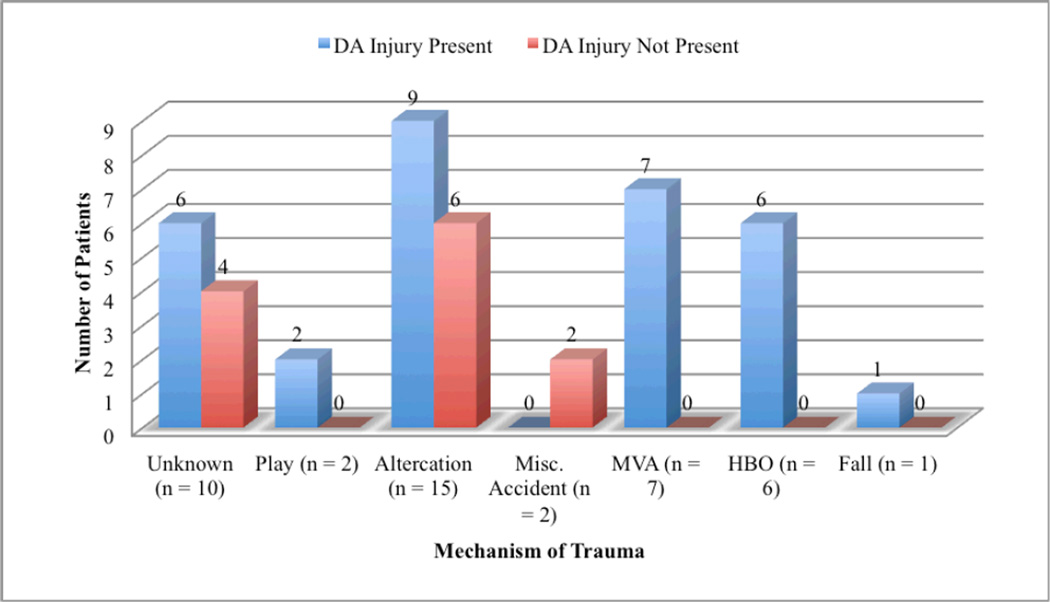
The relationship between the prevalence of DAI and sex, age, skull type, mechanism of trauma, region of MF fracture and number of MF fractures per patient is summarized in table 3. Those patients with a DAI (mean – 1 year) were significantly younger than those patients without a DAI (mean – 6 years). A statistically significant difference in the occurrence of DAI was also observed between age groups (p = 0.04). (Figure 3). The older a patient was, the less likely it was to suffer a DAI in conjunction with a MF fracture. The relationship between DAI and mechanism of trauma was also observed to be statistically significant (p = 0.04). (Table 3) Patients were more likely to sustain a DAI when the mechanism of MF fracture was motor vehicle accident (7/7; 100%) or hit by object (6/6; 100%) compared to patients who sustained a MF fracture from an altercation with another animal (9/15; 60%).
Table 3.
Association between patient/MF fracture characteristics and the incidence of DAI.
| DAI Present (%) | DAI Not Present (%) | |
|---|---|---|
| Sex | ||
| M (n = 7) | 5 (71.4) | 2 (28.6) |
| N (n = 17) | 11 (64.7) | 6 (32.6) |
| F (n = 3) | 3 (100) | 0 (0) |
| S (n = 16) | 12 (75) | 4 (25) |
| p = 0.37 | ||
| Age (years) | ||
| Range | 0.16 – 12 | 0.41 – 15 |
| Mean | 1 | 6 |
| Median | 1 | 4 |
| < 3 yr (n = 27) | 22 (81.5) | 5 (18.5) |
| 3 yr to 6 yr (n = 5) | 4 (80) | 1 (20) |
| 7 yr to 10 yr (n = 6) | 4 (66.6) | 2 (33.3) |
| >10 yr (n = 5) | 1 (20) | 4 (80) |
| p = 0.04* | ||
| Skull Type | ||
| Brachycephalic (n = 12) | 10 (83.3) | 2 (16.6) |
| Mesaticephalic (n = 29) | 20 (69) | 9 (31) |
| Dolicocephalic (n = 2) | 1 (50) | 1 (50) |
| p = 0.5 | ||
| Mechanism of Trauma | ||
| Unknown (n = 10) | 6 (60) | 4 (40) |
| Play (n = 2) | 2 (100) | 0 (0) |
| Altercation (n = 15) | 9 (60) | 6 (40) |
| Miscellaneous Accident (n = 2) | 0 (0) | 2 (100) |
| Motor Vehicle Accident (n = 7) | 7 (100) | 0 (0) |
| Hit by Object (n = 6) | 6 (100) | 0 (0) |
| Fall from Height (n = 1) | 1 (100) | 0 (0) |
| p = 0.04* | ||
| Region of MF Fracture | ||
| Exclusively Upper (n = 0) | 0 (0) | 0 (0) |
| Exclusively Middle (n = 4) | 4 (100) | 0 (0) |
| Exclusively Lower (n = 31) | 20 (64.5) | 11 (35.5) |
| Combination (n = 8) | 7 (87.5) | 1 (12.5) |
| Number of MF Fractures | ||
| 1 (n = 28) | 21 (75) | 7 (25) |
| 2 (n = 11) | 6 (54.5) | 5 (45.5) |
| 3 (n = 2) | 2 (100) | 0 (0) |
| 4 (n = 2) | 2 (100) | 0 (0) |
| p = 0.34 |
= statistically significant (p<0.05)
Figure 3.
Incidence of DAI as it relates to patient age.
Thirty-two (51.6%) teeth were severely injured. In those patients with a DAI, the relationship between the severity of the DAI and sex, age, skull type, mechanism of trauma, region of MF fracture and number of MF fractures per patient was not statistically significant.
Discussion
A DAI is any injury related to the tooth or tooth supporting structures (gingiva, periodontal ligament, and alveolar bone). There have been numerous attempts to classify the variety of injuries that can affect the dentoalveolar structures. The American Veterinary Dental College has proposed a classification system that classifies increasing degrees of trauma to the tooth (AVDC 2010). However, the AVDC system does not address conditions in which the tooth has been displaced from its supporting alveolus (socket). Nor does it address fractures to the supporting alveolar bone. The most up-to-date and inclusive classification of DAI for humans (Figure 1) fulfills the need to clearly define tooth displacement injuries and alveolar bone fractures (Andreason and others 2012). For the purposes of this study a modified version of the human classification system was used. Several types of injuries were combined in an attempt to improve the information garnered from comparisons between injury type and patient characteristics. For example, all types of crown fracture (infraction, enamel fracture, enamel-dentin-pulp fracture, etc.) were combined into one group and all displacement injures (subluxation, extrusion, intrusion, lateral luxation and alveolar fracture) were combined into another group. In addition, a class to describe damage to the developing (but not yet erupted) permanent tooth bud in juvenile patients was added.
It is difficult to acquire an accurate impression of the prevalence of DAI in dogs from the literature. This area of veterinary traumatology has historically been overlooked and poorly studied. Previous studies have focused on the nature of MF trauma (Whitney 1987, Umphlet 1990, Lopes and others 2005) or on the incidence of oral disease (Golden and others 1982) within the general population rather than on DAI. Within the general population, the prevalence of dental fractures in dogs and cats has been reported to be between 14–27% (Golden and others 1982). Fractures with pulp exposure have been reported in 10% of dogs (Golden and others 1982). A study evaluating high-rise syndrome in cats reported dental fractures in 17% of the study population (Whitney 1987). However, a more recent study of high-rise syndrome in cats reported a drastically higher incidence of dental trauma (Bonner and others 2012). An interesting and important finding within the more recent high-rise syndrome study was a disparity between the incidence of reported dental trauma when the oral examination was performed by either a specialist or resident in dentistry and oral surgery (71.4%) and when the oral examination was performed by other clinicians (i.e. emergency and critical care) (6.0%).
To the authors’ knowledge this is the first study of its kind in veterinary medicine. The goal was to look specifically at those patients with MF fractures and evaluate the prevalence of, and the factors that contribute to, concurrent DAI. It was hypothesized that the prevalence of DAI in this subset of patients would be high. Within the study population, 72.1% of patients with MF fractures had at least one DAI. This is consistent with the aforementioned report on high-rise syndrome in cats (Bonner and others 2012) and higher than that which has been reported in humans (16%–48.25%) (Ignatius and others 1992, Gassner and others 1999, Thorén and others 2010). The mean number of teeth injured per patient was two, which is consistent with previous human reports Thorén and others 2010).
Male patients were overrepresented in this study and most were neutered, consistent with the general population. Previous veterinary studies evaluating MF fractures in dogs revealed similar findings (Umphlet 1990, Lopes and others 2005). Human studies reveal a similar propensity for males to sustain more MF fractures and DA injuries compared to females (Ignatius and others 1992, Gassner and others 1999, Thorén and others 2010). It is suggested that this is consistent with the activities that young men tend to engage in (assault, work, sport, hit by object, etc.) (Gassner and others 1999).
Within the scope of this study, age was found to be a significant predictor of DAI. Older patients were less likely to suffer DAI when MF fractures were present compared to younger animals. In humans, the same association with age is present (Gassner and others 1999, Thorén and others 2010). There are two potential explanations for this. Dentinogenesis (natural deposition of dentin within the tooth) continues throughout the life of the tooth resulting in thicker dentin and ultimately makes a tooth stronger. It is possible that older teeth are better equipped to withstand the forces associated with trauma to the MF region without being injured. On the other hand, this may relate more to the nature of the behavior of older versus younger patients. Younger patients may be more likely to engage in activities that put them at risk of sustaining MF, and thus, DAI.
The forces required to cause MF fractures and DAI are dictated more by the buttressing forces of the skull than the breed of the dog (Boudrieau 2004). Therefore, in an attempt to more accurately delineate any association between those forces and the DAI they may cause, skull type (brachycephalic, mesaticephalic, dolichocephalic) was compared with the incidence of DAI, rather than evaluating breed. The most common skull type within this study was mesaticephalic (29/43; 67.4%). This finding may reflect a propensity for breeds with this skull type to sustain DAI or, more likely, reflect the popularity of those breeds with a mesaticephalic skull type within the general population. No significant associations were present between skull types and DAI.
The most common type of DAI observed within the study population was root (30.6%) and crown (29%) fractures, the most commonly affected teeth being the incisors and canines. This is comparable with previous reports of dental fractures in dogs where most occurred in incisor teeth (57%) and canine teeth (24%) (Golden and others 1982). This is also true in humans where it is hypothesized that the incisors and canines are the most vulnerable due to anatomy (Gassner and others 1999, Thorén and others 2010). It is reasonable to draw the same conclusion as to why the incisor and canines are injured more often than premolars and molars in dogs and cats. The present results are also consistent with the findings of a population of cats suffering from high-rise syndrome (Bonner and others 2012). Dentoalveolar injuries have the potential to occur in either jaw regardless of the location of the MF fracture. However, this study revealed a tendency for the location of the DAI to be consistent with the location of the MF fractures.
There is no standard classification system for describing the mechanism of MF fractures in humans or animals. The category “play accident” was used to describe any injury that occurred while playing as long as it did not involve impact with a moving object (golf club, baseball bat, horse kick, etc.) For example, one patient sustained a mandibular fracture when it collided with a parked trailer while running through the yard. Collisions with a swinging object (golf club, etc.) were categorized as “hit by object” and grouped together according to a general sense of the type and degree of force applied to the MF region.
The frequency of the mechanism of trauma was remarkably consistent with a report of MF fractures in Brazilian dogs (Lopes and others 2005). Unknown trauma was the second most common mechanism (23.3%) behind altercation with another animal (34.9%). Motor vehicle accident was the third most common mechanism of trauma. In addition, if one were to exclude activities that animals cannot engage in (work, sports, etc.) from human studies and the unknown cases in our study, our results are very consistent with the relative proportions of MF fracture mechanisms reported in humans (Gassner and others 1999, Thorén and others 2010).
It was also hypothesized that the mechanism of MF fracture would be associated with the DAI. Although the force of impact for different mechanisms cannot be reported accurately, it stands to reason that some mechanisms (i.e. motor vehicle accident) would likely be associated with higher forces and, therefore, would be associated with more DAI. This hypothesis held true within the confines of the present study. Cases that sustained MF trauma secondary to a motor vehicle accident or when hit by an object were 40% more likely to sustain a DAI when compared to other mechanisms of trauma, such as an altercation with another animal. (Figure 4) It also stands to reason that mechanisms of trauma with presumed higher impact forces would lead to a more severe DAI. Within the limits of this study no statistically significant relationship was seen between mechanism of trauma and severity of DAI.
Figure 4.
Incidence of DAI as it relates to mechanism of trauma. MVA = motor vehicle accident; HBO = Hit by Object
In order to evaluate possible associations between the location of MF fractures and the occurrence and nature of DAI, the skull was divided into three units (cranial/upper third; mid-face/middle third; and mandible/lower third). Most MF fractures in the present study involved the mandible, which is consistent with previous reports. In general the location of the MF fracture predicted the location but not the nature of the concurrent DAI.
Just over 50% of the DAI within this study were considered severe injuries. This is consistent with human studies (Gassner and others 1999, Thorén and others 2010). The justification for making the distinction of severe versus non-severe injuries lies in the timeliness of treatment required to maintain the affected tooth. Severe injuries generally require emergency treatment (within 1–4 hours), if possible, if the dentition is to be maintained. In light of the increasing importance of the dentition to veterinary clients, this distinction is important.
The most significant limitation of the present study was the retrospective nature of the design. However, given that all patients within the study were evaluated and treated by specialists in dentistry and oral surgery, it is unlikely that a prospective design would have had any significant impact on the findings that DAI are commonly associated with MF fractures.
It is clear from the results of this study that concurrent DAI are common in patients with MF fractures. Dentoalveolar injuries should be expected in patients who have sustained maxillofacial fractures. The findings of this study serve to encourage veterinarians to fully assess the oral cavity in patients with MF fractures as DAI are common and, if left undiagnosed and untreated, often lead to chronic pain, and inflammation. The most appropriate treatment for some DAI is best rendered on an emergency basis, when possible. Therefore, an appreciation for and timely recognition of DAI may be crucial for treatment success and meeting the clients’ expectations.
Acknowledgements
The authors of this manuscript would like to thank Scott Hetzel, M.S., Research Assistant of the Department of Biostatistics and Medical Informatics, University of Wisconsin-Madison for his assistance in the statistical analysis of the data
Contributor Information
Jason W. Soukup, Diplomate American Veterinary Dental College, Department of Surgical Sciences, School of Veterinary Medicine, University of Wisconsin-Madison, 2015 Linden Drive, Madison, WI 53706, 608-263-7600, soukupj@svm.vetmed.wisc.edu.
Brenda L. Mulherin, Department of Surgical Sciences, School of Veterinary Medicine, University of Wisconsin-Madison, 2015 Linden Drive, Madison, WI 53706, 608-263-7600.
Christopher J. Snyder, Diplomate American Veterinary Dental College, Department of Surgical Sciences, School of Veterinary Medicine, University of Wisconsin-Madison, 2015 Linden Drive, Madison, WI 53706, 608-263-7600.
References
- 1.American Veterinary Dental College. [accessed 15 April 2012];2010 www.avdc.org/nomenclature.html#toothfracture. [Google Scholar]
- 2.Andreasen JO, Lauridsen E, Gerds AT, Ahrensburg SS. Dental Trauma Guide: A source of evidence-based treatment guidelines for dental trauma. Dent Traumatol. 2012;28:142–147. doi: 10.1111/j.1600-9657.2011.01059.x. [DOI] [PubMed] [Google Scholar]
- 3.Bonner SE, Reiter AM, Lewis JR. Orofacial manifestations of high-rise syndrome in cats: A retrospective study of 84 cases. J Vet Dent. 2012;29:10–18. doi: 10.1177/089875641202900103. [DOI] [PubMed] [Google Scholar]
- 4.Boudrieau RJ. Miniplate reconstruction of severely comminuted maxillary fractures in two dogs. Vet Surg. 2004;33:154–163. doi: 10.1111/j.1532-950x.2004.04023.x. [DOI] [PubMed] [Google Scholar]
- 5.Gassner R, Bösch R, Tuli T, Rüdiger E. Prevalence of dental trauma in 6000 patients with facial injuries. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:27–33. doi: 10.1016/s1079-2104(99)70290-8. [DOI] [PubMed] [Google Scholar]
- 6.Golden AL, Stoller N, Harvey CE. A survey of oral and dental diseases in dogs anesthetized at a veterinary hospital. J Am Anim Hosp Assoc. 1982;18:891–899. [Google Scholar]
- 7.Ignatius ET, Olkarinen KS, Silvennoinen U. Frequency and type of dental traumas in mandibular body and condyle fractures. Endod Dent Traumatol. 1992;8:235–240. doi: 10.1111/j.1600-9657.1992.tb00250.x. [DOI] [PubMed] [Google Scholar]
- 8.Lopes FM, Gioso MA, Ferro DG, Leon-Roman MA, Venturini MAFA, Correa HL. Oral fractures in dogs in Brazil: A retrospective study. J Vet Dent. 2005;22:86–90. doi: 10.1177/089875640502200202. [DOI] [PubMed] [Google Scholar]
- 9.Thorén H, Numminen L, Snäll J, Lindqvist T, Iizuka T, Törnwall J. Occurrence and types of dental injuries among patients with maxillofacial fractures. Int J Oral Maxillofac Surg. 2010;39:774–778. doi: 10.1016/j.ijom.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 10.Umphlet RC, Johnson AL. Mandibular fractures in the dog. Vet Surg. 1990;19:272–275. doi: 10.1111/j.1532-950x.1990.tb01184.x. [DOI] [PubMed] [Google Scholar]
- 11.Whitney WO, Mehlhaff CJ. High-rise syndrome in cats. J Am Vet Med Assoc. 1987;191:1399–1402. [PubMed] [Google Scholar]