Abstract
Stroke is the fourth leading cause of death and the leading cause of long-term disability in the United States. Stroke incidence and prevalence is not uniform. It occurs more frequently in some geographical areas of the United States and the rates are higher in minority groups.1,2 Some proposed causes for these disparities include increased rate of vascular risk factors that disproportionally affect some minority groups, differential effect of hypertension on stroke risk across racial groups, lack of access to health care and other social determinants of health, suboptimal control of risk factors, and although lacking substantive data to date, an inherited predisposition to stroke associated with genetic differences. The Reasons for Geographic and Racial Differences in Stroke (REGARDS) investigators found that the rate of suboptimal control of vascular risk factors and unhealthy lifestyles were significantly greater in African Americans compared to non-Hispanic whites (NHW).2 Moreover, regarding high blood pressure (BP), a triple threat has been described: blacks are not only more likely to have high BP, they are less likely, once diagnosed, to have their high BP controlled, and this suboptimal control has been shown to confer a stroke risk that is 3 times higher among blacks compared to whites for every 10-mm Hg increase in systolic BP (SBP).3
Stroke is the fourth leading cause of death and the leading cause of long-term disability in the United States. Stroke incidence and prevalence is not uniform. It occurs more frequently in some geographical areas of the United States and the rates are higher in minority groups.1,2 Some proposed causes for these disparities include increased rate of vascular risk factors that disproportionally affect some minority groups, differential effect of hypertension on stroke risk across racial groups, lack of access to health care and other social determinants of health, suboptimal control of risk factors, and, although lacking substantive data to date, an inherited predisposition to stroke associated with genetic differences. The Reasons for Geographic and Racial Differences in Stroke (REGARDS) investigators found that the rate of suboptimal control of vascular risk factors and unhealthy lifestyles was significantly greater in African Americans compared to non-Hispanic whites (NHW).2 Moreover, regarding high blood pressure (BP), a triple threat has been described: blacks are not only more likely to have high BP, they are less likely, once diagnosed, to have their high BP controlled, and this suboptimal control has been shown to confer a stroke risk that is 3 times higher among blacks compared to whites for every 10-mm Hg increase in systolic BP (SBP).3
To investigate whether racial and ethnic disparities in stroke prevalence in the United States are explained by the suboptimal control of cardiovascular risk factors, we used data from the National Health and Nutrition Examination Survey (NHANES) from 2000 to 2009 that represent the noninstitutionalized US population. We included in the analysis adults 20 years or older who had complete information on the variables studied. Age, sex, and racial/ethnic identification were obtained by self-report. Only NHW, non-Hispanic blacks (NHB), and Mexican Americans (MA) were included in the analysis because sampling from other Hispanics and other races was not enough to obtain accurate estimates. Family poverty income ratio was used for income input. Education was categorized into <9th grade, 9th–11th grade, high school graduate, some college, and college graduate or above. Physical inactivity was defined as the lack of moderate or vigorous activity in the last 30 days prior to the interview. Participants with a lifetime history of smoking more than 100 cigarettes and who were smoking at the time of the interview were considered current smokers. Hypertension was defined by self-report, antihypertensive use, or SBP >140 mm Hg or diastolic BP (DBP) >90 mm Hg (for diabetic subjects, SBP >130 mm Hg or DBP >80 mm Hg); diabetes mellitus (DM) by self-report, hypoglycemic use, or glycosylated hemoglobin >7%; and hypercholesterolemia by self-report, hypocholesterolemic drug use, or total cholesterol >240 mg/dL (>200 mg/dL for diabetic subjects). An alternative definition of vascular risk factors was used to assess the degree of control. Hypertension, DM, and hypercholesterolemia were defined as suboptimally controlled if they were undiagnosed, untreated, or if the cutoffs for diagnosis in BP, total cholesterol, and glycosylated hemoglobin remained elevated despite treatment. Logistic regression models were created to obtain the odds ratios (ORs) and their 95% confidence intervals (CIs) between stroke and ethnic/racial groups after adjusting for survey design factors and appropriate weights. The validity and relevance of each logistic regression was evaluated with the maximum likelihood test. A p of ≤0.05 was considered statistically significant.
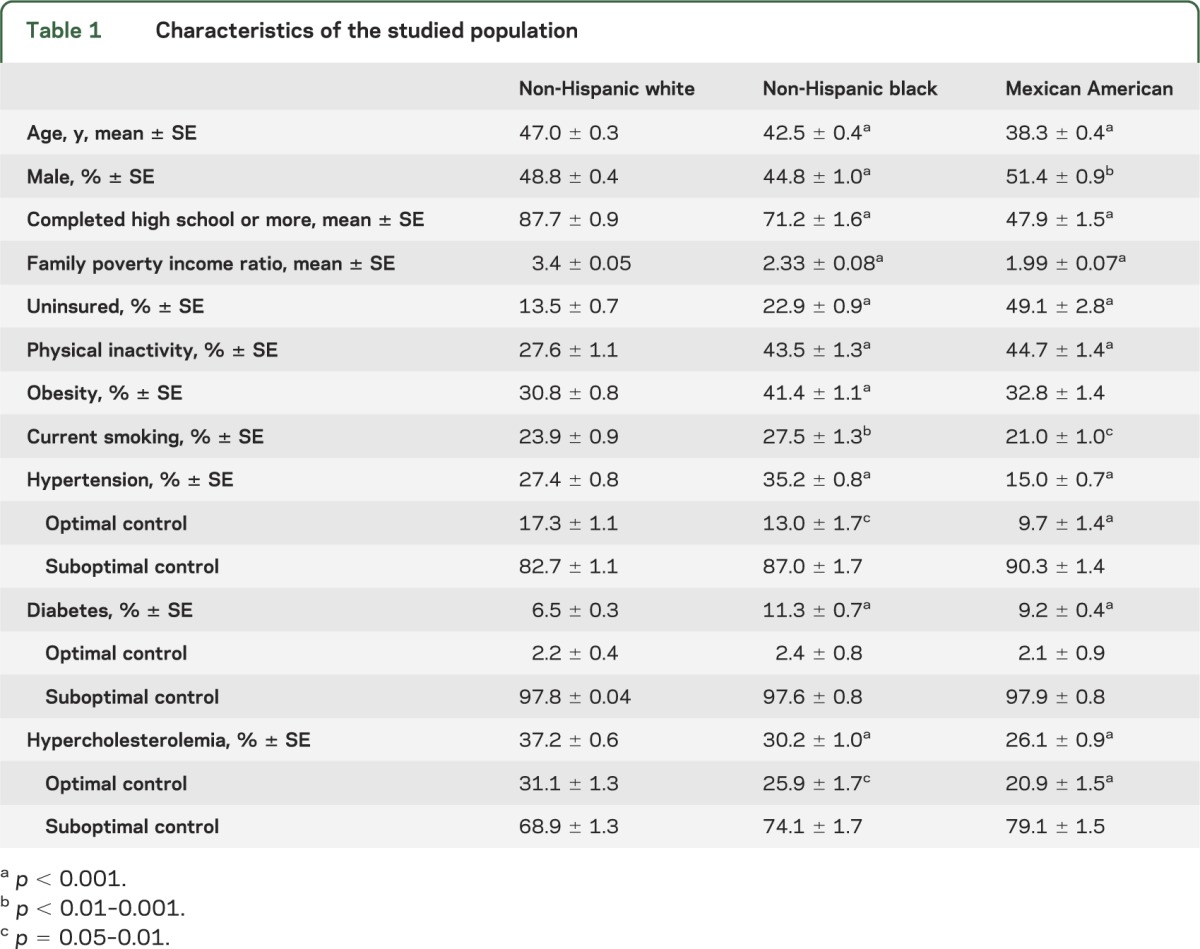
The sample included 37,847 participants with complete information, mean age 48.7 years (range 20–85); 49% were men, 79% were NHW, 12% were NHB, and 9% were MA. The characteristics of the cohort varied by racial and ethnic group (table 1). NHB had significantly higher prevalence of physical inactivity, obesity, smoking, hypertension, and DM compared to NHW. For MA, physical inactivity and DM were higher compared to NHW, while hypertension, smoking, and hypercholesterolemia were lower. Compared to NHW, NHB not only had a higher prevalence of hypertension, but among those with hypertension, NHB more frequently had suboptimal control compared to NHW (87% vs 83%, p = 0.03). The same disparity was noted for in hypertension control for MA compared to NHW (90% vs 83%, p < 0.001). Although hypercholesterolemia was more prevalent among NHW, hypercholesterolemia was more frequently uncontrolled in NHB (74%, p = 0.04) and MA (79%, p < 0.001) compared to NHW (69%). There was no significant difference in the rate of diabetes control among ethnic and racial groups.
Table 1.
Characteristics of the studied population
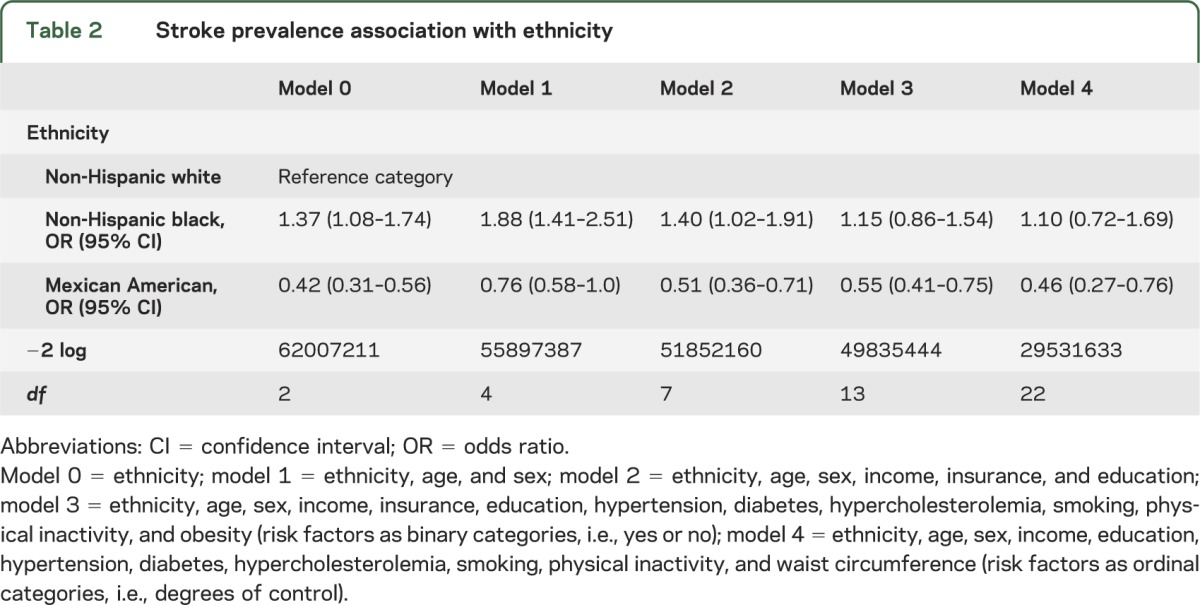
The overall stroke prevalence was 2.1% ± 0.1%. Compared to NHW, stroke was more frequent in NHB (OR 1.37, 95% CI 1.08–1.74) but less common in MA (OR 0.42, 95% CI 0.31–0.56). As evidenced in table 2, the higher prevalence of stroke in NHB was confounded by the covariates used in this analysis. Despite an initial increase in OR in the sex- and age-adjusted model, the strength of association decreased progressively after adjusting for sociodemographic variables and vascular risk factors. Using hypertension, DM, and hypercholesterolemia as ordinal instead of categorical variables yielded the lowest possible OR (1.10, 0.72–1.69) between NHB and stroke and it was the best fitting model (>50% fitness improvement, p < 0.001). Despite the more unfavorable social and vascular profile observed in MA, the prevalence of stroke remained lower than that observed in NHW. In addition to the ethnic and racial disparities described in model 4, stroke was more frequent with increasing age (OR 1.04, 95% CI 1.03–1.05), physical inactivity (OR 1.46, 95% CI 1.07–1.975), smoking (OR 1.88, 95% CI 1.32–2.66), suboptimal hypertension control (OR 2.41, 1.67–3.45), suboptimal DM control (1.62, 1.24–2.13), and optimal hypercholesterolemia control (1.62, 1.22–2.15). There was no statistically significant difference in the rate of stroke between participants with optimally controlled hypertension (OR 1.59, 0.81–3.15) and DM (OR 1.08, 0.36–3.26) compared to those without these conditions.
Table 2.
Stroke prevalence association with ethnicity
This analysis underscores the challenges facing health care providers in the United States; more than half of the studied US population with diabetes, hypertension, or hypercholesterolemia has suboptimal vascular risk control because participants do not take medications, are not aware of their diagnosis, or remain uncontrolled despite medications. Stroke prevalence is greater in those with uncontrolled hypertension and DM compared to participants who have these risks under control or those who do not have these risk factors. These results also add evidence to the current literature that ethnic and racial stroke disparities in the United States are mainly explained by the disproportionate increased prevalence of vascular risk factors and the degree of risk factor control among the most affected groups, particularly NHB. We also replicate what others have called the Hispanic paradox, where Hispanics, in this case, MA, have decreased morbidity and mortality compared to NHW, despite the more unfavorable social and vascular profile, although it is more true for those born outside the United States.4 There is a discrepancy between the lower rate of stroke prevalence in MA nationwide and regional cohorts of MA or other Hispanic groups.1,5 Some potential explanations of this discrepancy involve differences in the subpopulation of Hispanics enrolled in these cohorts, environmental or geographic factors related to stroke, and potential underdiagnoses of stroke in MA in the NHANES survey, as stroke is determined by self-report.
Addressing racial and ethnic disparities in stroke requires more robust and systematic approaches to vascular risk factor control, as suggested by this study. The success of stroke disparities interventions that are focused on prevention, such as the National Institute of Neurological Disorders and Stroke Stroke Prevention/Intervention Research Program, depends on their ability to effectively address vascular risk factor control.
AUTHOR CONTRIBUTIONS
Jose Gutierrez: design and conceptualization of the data, analysis and interpretation of the data, drafting of the manuscript. Olajide A. Williams: analysis and interpretation of the data.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
J. Gutierrez reports no disclosures. O. Williams reports support from NIH/NINDS 1 R01 NS067443-01A 1, NIH/NINDS 1U54NS081765-01, NYCDOH 11AC074301R0X00, and NYS HEALD C024255. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Morgenstern LB, Smith MA, Lisabeth LD, et al. Excess stroke in Mexican Americans compared with non-Hispanic whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol 2004;160:376–383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kulshrestha A, Judd S, Vaccarino V, et al. Life's Simple 7 and risk of incident stroke in black and white Americans: Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke 2013;44:1909–1914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howard G, Lackland DT, Kleindorfer DO, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med 2013;173:46–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moon JR, Capistrant BD, Kawachi I, et al. Stroke incidence in older US Hispanics: is foreign birth protective? Stroke 2012;43:1224–1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sacco RL, Boden-Albala B, Abel G, et al. Race-ethnic disparities in the impact of stroke risk factors: the Northern Manhattan Stroke Study. Stroke 2001;32:1725–1731 [DOI] [PubMed] [Google Scholar]


