Abstract
Objectives:
While the short-term impact of atrial fibrillation–related stroke has been well studied, surprisingly little is known about its long-term effect on survival.
Methods:
We followed 13,559 patients with atrial fibrillation for a median of 6 years, identifying ischemic strokes through computerized databases and validating 1,025 events. Stroke severity was determined from hospital records. We compared survival of stroke patients with comparator nonstroke patients (matched for age, sex, race, comorbid conditions, and time of entry into the cohort) using proportional hazard models controlling for warfarin use and compared survival by degree of discharge deficit.
Results:
Median survival after stroke was 1.8 years compared with 5.7 years for matched nonstroke comparators (hazard ratio [HR] 2.8, 95% confidence interval [CI] 2.5–3.2). This increased risk of all-cause death persisted even after restricting the analysis to the 576 stroke patients who survived 6 months after the initial stroke event (HR 2.0, 95% CI 1.7–2.5, adjusting for warfarin use). Risk of death was strongly associated with stroke severity: HR 2.9 (95% CI 2.3–3.5) for strokes resulting in major deficits and HR 8.3 (95% CI 5.2–13.2) for strokes resulting in severe deficits compared with matched comparators without stroke.
Conclusions:
Ischemic stroke approximately triples the mortality rate in patients with atrial fibrillation. This effect persists well beyond the immediate period poststroke and is strongly associated with disability after stroke. Stroke prevention by anticoagulation has even greater beneficial effects on survival than usually considered when focusing solely on 30-day mortality rates.
Atrial fibrillation is an increasingly common medical condition, with an estimated prevalence of at least 2.5 million people in the United States,1,2 and contributes to significant morbidity and mortality largely by raising the risk of ischemic stroke.3 Stroke is the fourth leading cause of death in the United States and median survival after stroke has been reported to be approximately 5 to 10 years, depending on stroke severity and patient factors.2,4–6 Strokes occurring in the setting of atrial fibrillation result in worse neurologic deficits and higher 30-day mortality than strokes occurring in people without atrial fibrillation.7,8 As a result, we would anticipate that long-term survival after atrial fibrillation–related stroke would also be particularly poor. However, information on long-term outcomes after atrial fibrillation–related stroke is relatively scarce. The objective of this analysis was to provide precise estimates of the impact of atrial fibrillation–associated ischemic stroke on long-term survival. Such information is needed to fully inform the decision to use anticoagulants or other risky interventions to prevent stroke in patients with atrial fibrillation.9,10
METHODS
The AnTicoagulation and Risk factors In Atrial fibrillation (ATRIA) Study is a cohort of 13,559 adults aged 18 years or older with diagnosed atrial fibrillation enrolled in Kaiser Permanente Northern California.11 As described previously, cohort members were identified between July 1, 1996 and December 31, 1997 by searching automated inpatient, outpatient, and ECG databases for ICD-9 diagnoses of atrial fibrillation (427.31) and followed until death, cohort disenrollment, or the study end date of September 30, 2003.12 Patients with diagnosed mitral stenosis, valvular repair or replacement, transient postoperative atrial fibrillation, or concurrent hyperthyroidism were excluded so as to focus on “nonvalvular,” nontransient atrial fibrillation.
Identification of ischemic stroke and outcomes.
To identify stroke events, computerized hospitalization and billing databases were searched for primary discharge diagnosis of ischemic stroke. Patients who presented to other institutions with stroke were also identifiable using health plan databases because Kaiser Permanente was financially responsible for those hospitalizations. The medical records of potential events were abstracted and the events adjudicated by an outcomes committee using a formal study protocol, with 2 physicians reviewing the medical records for each potential event and a third physician reviewing cases in which the initial reviewers disagreed. If there was no consensus on the validity of an event, an expert neurologist adjudicated the event. We considered events as valid ischemic strokes if they resulted in sudden-onset neurologic deficits that persisted for at least 24 hours that were not explained by other etiologies (such as tumor, infection, or vasculitis). The primary outcome of the analysis, all-cause mortality, was determined using medical chart review, health plan databases, and the comprehensive California State death certificate registry.
Clinical risk factors.
Patient age and sex were obtained from administrative databases. Clinical risk factors were identified by searching for specific ICD-9–coded diagnoses based on previously validated algorithms.11 The diagnosis of diabetes mellitus was determined through a health plan registry.13 Clinical factors were used to calculate a CHADS2 (Congestive heart failure, Hypertension, Age >75 years, Diabetes mellitus, and Stroke) and a CHA2DS2-VASc (Congestive heart failure, Hypertension, Age, Diabetes mellitus, Stroke, Vascular disease, and Sex) stroke risk score for patients at the index date.14 Warfarin exposure at the time of stroke was obtained through review of the admission medical records, and longitudinal warfarin use was determined using a validated algorithm that incorporated pharmacy dispensing of warfarin and serial outpatient international normalized ratio tests.11 Data on functional disability at the time of hospital discharge were collected by reviewing physician, nursing, physical/occupational therapy, and social work notes available in the medical record. Severity of functional deficits was categorized using a modified Rankin Scale15 with the following scores: fatal inpatient event = 6; severe disability (i.e., deficits that resulted in total dependence) = 5; major disability (i.e., deficits that prevented independent living) = 3 or 4; minor disability (i.e., residual deficit that did not interfere with independent living) = 1 or 2; and no disability = 0.
Statistical analysis.
The primary outcome was all-cause mortality occurring during the cohort follow-up period through September 2003. For each patient who developed a stroke, we randomly selected a single matched comparator from among patients in the cohort who had not developed a stroke. Stroke patients and their comparators were matched on age (within 5 years), sex, whether they had a stroke before entry into the cohort, and time since entering the cohort. We also attempted to match on the following risk factors that could contribute to differences in mortality: hypertension, diabetes mellitus, congestive heart failure, coronary artery disease, and history of cancer (excluding nonmelanoma skin cancers). Ninety-eight percent of patients sustaining an ischemic stroke were paired with nonstroke comparators who matched on all 5 of these latter clinical features. The median survival was determined from Kaplan-Meier curves, with the index date being the date of stroke presentation for stroke patients. Log-rank tests were used to compare the survival of all stroke patients and their comparators, as well as stratify by modified Rankin Scale score at discharge. Unadjusted hazard ratios (HRs) were calculated using proportional hazards models, containing an indicator for patients with stroke. We generated adjusted HRs using proportional hazards models controlling for time-varying warfarin use during follow-up. The analysis of subsequent survival for stroke patients who were alive at 6 months poststroke was limited to stroke patient/nonstroke comparator pairs who were both alive at 6 months. This excluded 7% of stroke patients who were alive at 6 months but whose matched nonstroke comparator had died by 6 months. All analyses were performed using SAS software, version 9.3 (SAS Institute Inc., Cary, NC).
Standard protocol approvals, registrations, and patient consents.
The study was approved by institutional review boards of participating institutions. Waiver of informed consent was obtained because of the nature of the study.
RESULTS
The cohort consisted of 13,559 subjects with atrial fibrillation followed for a median of 6 years, accumulating a total of 66,754 person-years of follow-up. There were 1,025 patients presenting with incident ischemic stroke during follow-up. Stroke patients and their nonstroke comparators were well matched for age, sex, race, hypertension, diabetes mellitus, congestive heart failure, coronary artery disease status, history of cancer, CHADS2 stroke risk score, and time from cohort entry to index date (table). Among the 1,025 stroke patients, 382 (37%) were receiving warfarin therapy at the time of their stroke, 286 (28%) were taking aspirin therapy alone, 329 (32%) were not receiving antithrombotic therapy, and 3% were not receiving warfarin and had unknown aspirin status. A total of 64% of stroke cases and 65% of nonstroke comparators were treated with warfarin for at least some part of follow-up.
Table.
Characteristics of 1,025 patients presenting with ischemic stroke and 1,025 matched comparator patientsa without stroke in the ATRIA atrial fibrillation cohort
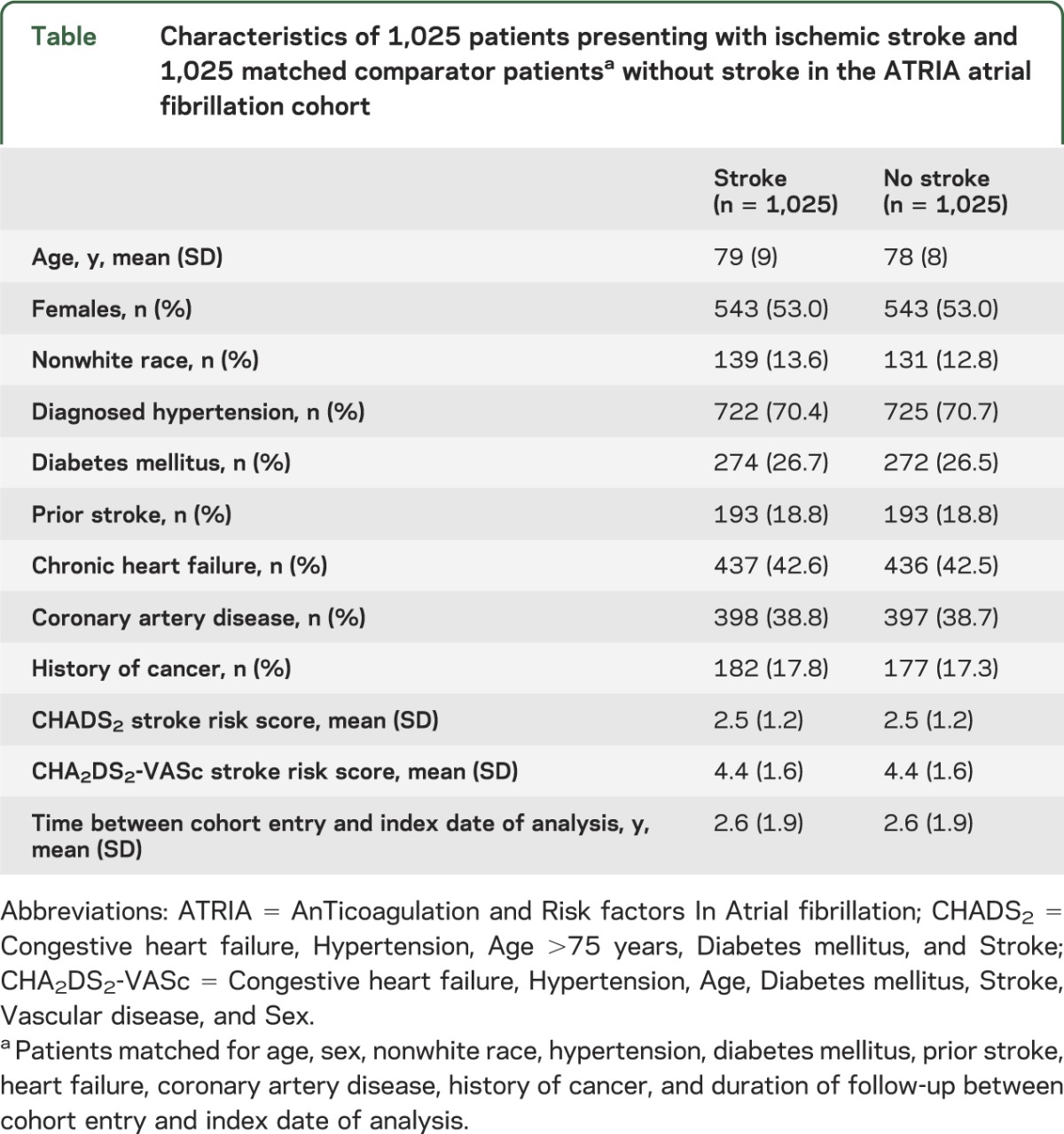
Thirty-day mortality after ischemic stroke was 24.7%. By 1 year, 40.3% (95% confidence interval [CI] 37.3%–43.5%) of stroke patients had died, 51.9% (95% CI 48.7%–55.1%) by 2 years, and 72.8% (95% CI 69.4%–76.1%) by 5 years (figure 1A). Median survival was 1.8 years (95% CI 1.6–2.1 years) after stroke. For matched nonstroke comparators, the median survival was 5.7 years (95% CI 5.1–6.2 years).
Figure 1. Survival of patients with ischemic stroke compared with matched controls.
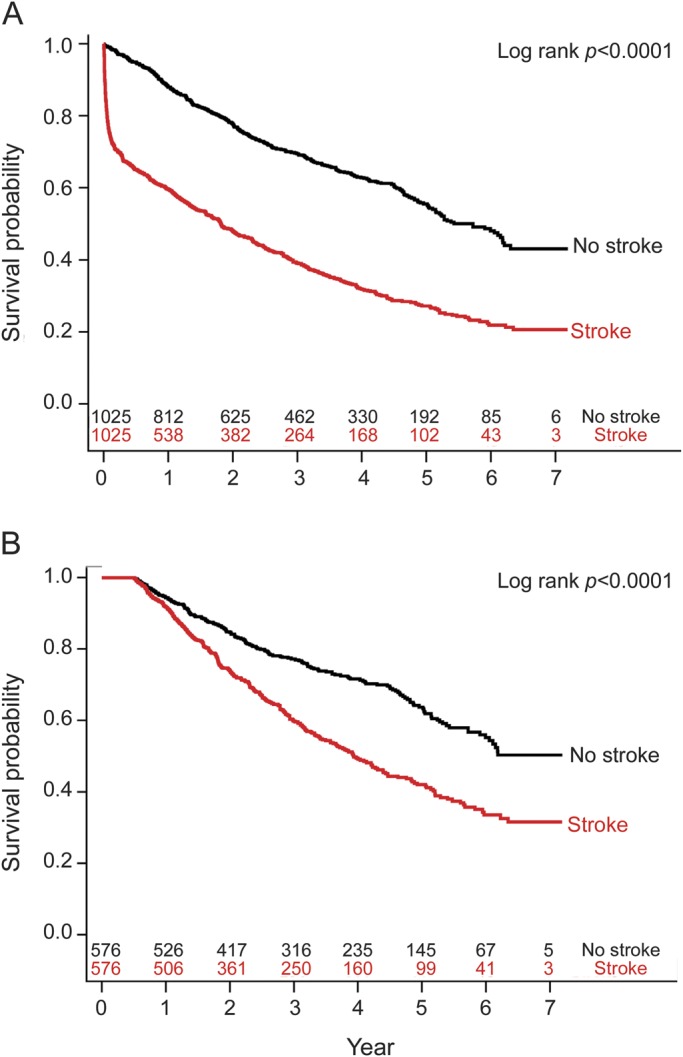
(A) Survival of 1,025 atrial fibrillation patients with ischemic stroke compared to 1,025 matched comparators without stroke. (B) Survival of 576 patients with ischemic stroke who survived ≥6 months after stroke presentation compared to 576 matched comparators.
The HR for death comparing patients sustaining an ischemic stroke with matched nonstroke comparators was 2.6 (95% CI 2.3–3.0). After controlling for warfarin exposure during follow-up, the HR for death associated with stroke was largely unchanged at 2.8 (95% CI 2.5–3.2). This increased risk of all-cause death associated with stroke persisted even after we restricted the analysis to the 576 stroke patients and their matched controls who survived 6 months after the initial stroke event (figure 1B) (HR 2.0, 95% CI 1.7–2.5, adjusting for warfarin use).
Of the 1,002 subjects who had documented functional status at discharge, 13% died in hospital, 9% had severe deficits at the time of discharge, 37% had major deficits, 38% had minor deficits, and 4% had no deficits. Severity of stroke was strongly associated with subsequent survival. Subjects with minor or no deficits after stroke had only slightly worse survival compared with patients without stroke (HR 1.7, 95% CI 1.3–2.1; figure 2A). In contrast, survival was dramatically worse with more severe strokes: compared with subjects without stroke, stroke patients with major deficits had an HR of death of 2.9 (95% CI 2.3–3.5) and those with severe deficits had an HR of 8.3 (95% CI 5.2–13.2) (figure 2, B and C). These HRs were all adjusted for warfarin use during follow-up.
Figure 2. Survival after ischemic stroke resulting in no/minor, major, or severe deficits compared with matched controls.
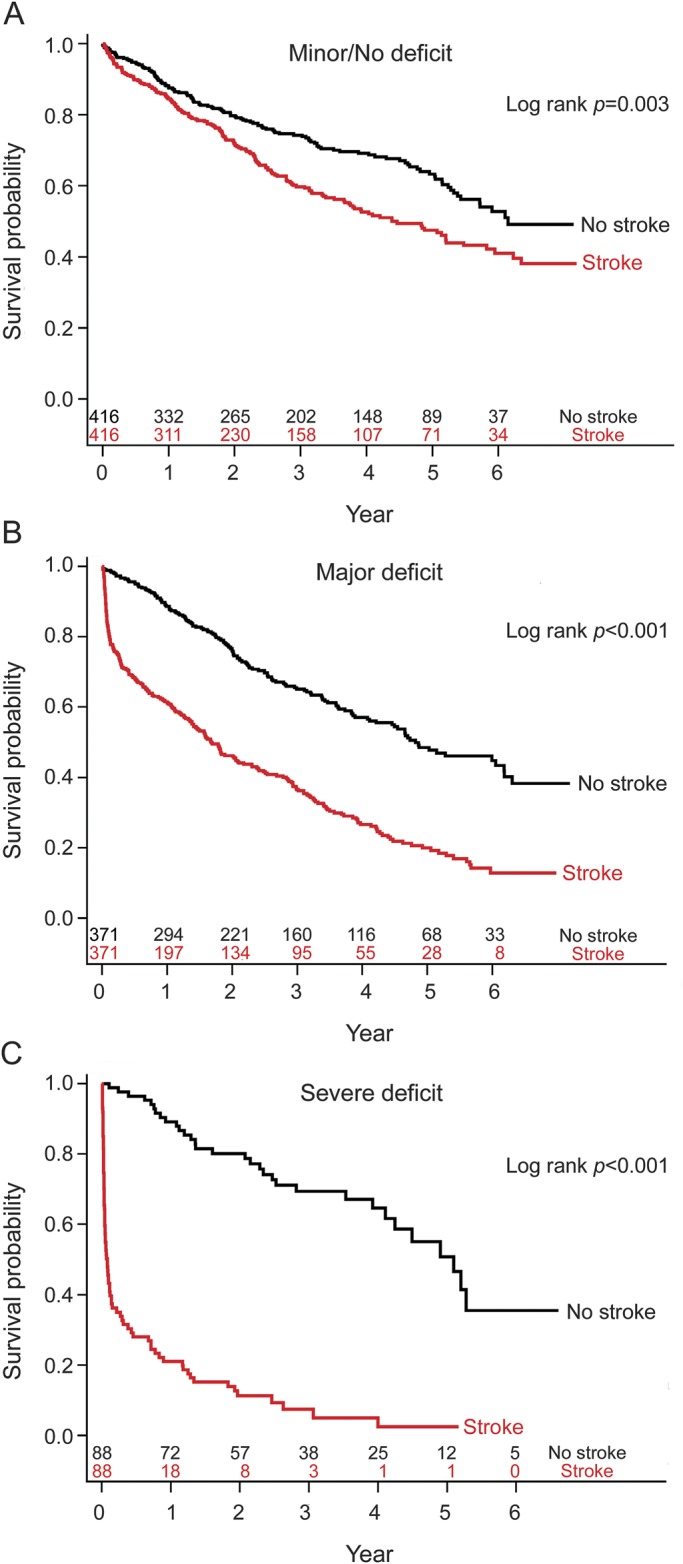
(A) Survival comparison of 416 stroke patients with no or minor deficits at discharge to 416 matched comparator patients without stroke. (B) Survival comparison of 371 stroke patients with major deficits at discharge to 371 matched comparator patients without stroke. (C) Survival comparison of 88 stroke patients with severe deficits at discharge to 88 matched comparator patients without stroke.
DISCUSSION
Numerous studies have documented the heightened risk of ischemic stroke in patients with atrial fibrillation and the augmented severity of atrial fibrillation–associated strokes, including increased 30-day mortality.7,8,16,17 However, relatively few studies have focused on the impact of such events on longer-term survival. Precise estimates of longer-term survival are needed to fully inform decisions to use risky therapies, such as anticoagulants, to prevent stroke.9 Our study finds that ischemic stroke nearly triples the risk of death in patients with atrial fibrillation, even after controlling for multiple other factors that might contribute to mortality by tight matching on covariates supplemented by regression modeling. Our analysis of the longer-term outcomes after stroke demonstrates that the negative consequences of stroke on survival persist far beyond the immediate event. Specifically, the median survival of ATRIA cohort members sustaining an ischemic stroke was less than 2 years. In comparison, the median survival of cohort members who had not sustained an ischemic stroke but were otherwise matched for age, sex, and multiple comorbid conditions was 5.7 years. Adjusting for warfarin use poststroke had little effect on our findings. There was a clear negative impact of stroke on survival even among patients who had survived 6 months after the stroke.
The poor survival that we observed after atrial fibrillation–related ischemic stroke is considerably worse than the survival reported for patients after stroke from all causes.18–20 In a general, predominantly non–atrial fibrillation population, 1-year mortality after ischemic stroke ranged from approximately 2% to 29% depending on patient factors.4,18,20–22 In contrast, among ATRIA atrial fibrillation cohort members sustaining an ischemic stroke, 40% had died within 1 year after their stroke event.
In our study, long-term survival after an ischemic stroke was strongly correlated with the severity of the stroke. For those with no or minor deficits poststroke, survival was only modestly worse than that for nonstroke matched comparators. However, as the functional deficits increased, the mortality rates increased markedly. Such findings have been observed in other studies of stroke in the general population.5,6 This association between long-term survival and stroke severity provides strong evidence that later deaths poststroke are, at least in part, attributable to the stroke events themselves. In many studies, “fatal” stroke is limited to deaths within 30 days of the stroke event.23,24 Our results make clear that the impact of stroke on survival extends far beyond the initial 30-day period.16,25,26
There are several limitations to our analysis. Although we successfully matched for multiple clinical factors related to mortality risk, we did not have measures of the severity of these comorbid conditions. We included warfarin use as a poststroke variable but did not assess anticoagulation control. Also, other unmeasured confounders may have affected our estimates of mortality risk and we lacked measures of initial stroke severity, such as the NIH Stroke Scale. We did not have clinical information on the cause of death after hospital discharge. As a result, we could not directly link later deaths to the functional deficits resulting from stroke. However, the strong association between discharge deficit and subsequent risk of death supports such a relationship across the entire ATRIA population sustaining an ischemic stroke.
Ischemic stroke nearly triples the risk of death in patients with atrial fibrillation, with more than half of patients dying within 2 years after the event. Importantly, the negative effect of stroke on survival persists far beyond the initial event, demonstrating that 30-day case fatality rates are a conservative estimate of the effect of stroke on survival. Our findings quantify additional negative health effects of stroke among patients with atrial fibrillation and further highlight the importance of preventing stroke in the first place and reducing the severity of strokes that do occur, primarily through the judicious use of anticoagulant therapy.16,26
GLOSSARY
- ATRIA
AnTicoagulation and Risk factors In Atrial fibrillation
- CHADS2
Congestive heart failure, Hypertension, Age >75 years, Diabetes mellitus, and Stroke
- CI
confidence interval
- HR
hazard ratio
- ICD-9
International Classification of Diseases, Ninth revision
AUTHOR CONTRIBUTIONS
M.C. Fang and A.S. Go: contributed to drafting/revising the manuscript for content, study concept and design, and analysis and interpretation of the data. Y. Chang: contributed to drafting/revising the manuscript for content, study concept and design, and statistical analysis. L.H. Borowsky: contributed to drafting/revising the manuscript for content, and study supervision and coordination. N.K. Pomernacki: contributed to drafting/revising the manuscript for content, study supervision and coordination, and data acquisition. N. Udaltsova: contributed to drafting/revising the manuscript for content and data acquisition. D.E. Singer: contributed to drafting/revising the manuscript for content, study concept and design, and analysis and interpretation of the data.
STUDY FUNDING
Supported by the National Institute on Aging (R01 AG15478 and K23 AG028978), the National Heart, Lung, and Blood Institute (U19 HL91179 and RC2HL101589), and the Eliot B. and Edith C. Shoolman fund of the Massachusetts General Hospital (Boston). The funding sources had no role in study design, data collection, data analysis, data interpretation, or preparation of the manuscript. Dr. Fang had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
DISCLOSURE
M.C. Fang, A.S. Go, Y. Chang, L.H. Borowsky, N.K. Pomernacki, and N. Udaltsova report no disclosures relevant to the manuscript. D.E. Singer reports consulting for Bayer Healthcare, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, Inc., Johnson & Johnson, Inc., and Pfizer, Inc. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors In Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370–2375 [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 2013;127:e6–e245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Arch Intern Med 1987;147:1561–1564 [PubMed] [Google Scholar]
- 4.Towfighi A, Saver JL. Stroke declines from third to fourth leading cause of death in the United States. Stroke 2011;42:2351–2355 [DOI] [PubMed] [Google Scholar]
- 5.Slot KB, Berge E, Dorman P, Lewis S, Dennis M, Sandercock P. Impact of functional status at six months on long term survival in patients with ischaemic stroke: prospective cohort studies. BMJ 2008;336:376–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eriksson M, Norrving B, Terént A, Stegmayr B. Functional outcome 3 months after stroke predicts long-term survival. Cerebrovasc Dis 2008;25:423–429 [DOI] [PubMed] [Google Scholar]
- 7.Lin HJ, Wolf PA, Kelly-Hayes M, et al. Stroke severity in atrial fibrillation: the Framingham Study. Stroke 1996;27:1760–1764 [DOI] [PubMed] [Google Scholar]
- 8.Lopes RD, Shah BR, Olson DM, et al. Antithrombotic therapy use at discharge and 1 year in patients with atrial fibrillation and acute stroke: results from the AVAIL registry. Stroke 2011;42:3477–3483 [DOI] [PubMed] [Google Scholar]
- 9.Eckman MH, Singer DE, Rosand J, Greenberg SM. Moving the tipping point. Circ Cardiovasc Qual Outcomes 2011;4:14–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casciano JP, Singer DE, Kwong WJ, Fox ES, Martin BC. Anticoagulation therapy for patients with non-valvular atrial fibrillation. Am J Cardiovasc Drugs 2012;12:313–323 [DOI] [PubMed] [Google Scholar]
- 11.Go AS, Hylek EM, Borowsky LH, Phillips KA, Selby JV, Singer DE. Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: the AnTicoagulation and Risk Factors In Atrial Fibrillation (ATRIA) Study. Ann Intern Med 1999;131:927–934 [DOI] [PubMed] [Google Scholar]
- 12.Go AS, Hylek EM, Chang Y, et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA 2003;290:2685–2692 [DOI] [PubMed] [Google Scholar]
- 13.Selby JV, Ray GT, Zhang D, Colby CJ. Excess costs of medical care for patients with diabetes in a managed care population. Diabetes Care 1997;20:1396–1402 [DOI] [PubMed] [Google Scholar]
- 14.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 2001;285:2864–2870 [DOI] [PubMed] [Google Scholar]
- 15.Farrell B, Godwin J, Richards S, Warlow C. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry 1991;54:1044–1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fang MC, Go AS, Chang Y, et al. Thirty-day mortality after ischemic stroke and intracranial hemorrhage in patients with atrial fibrillation on and off anticoagulants. Stroke 2012;43:1795–1799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lamassa M, Di Carlo A, Pracucci G, et al. Characteristics, outcome, and care of stroke associated with atrial fibrillation in Europe: data from a multicenter multinational hospital-based registry (the European Community Stroke Project). Stroke 2001;32:392–398 [DOI] [PubMed] [Google Scholar]
- 18.Dennis MS, Burn JP, Sandercock PA, Bamford JM, Wade DT, Warlow CP. Long-term survival after first-ever stroke: the Oxfordshire Community Stroke Project. Stroke 1993;24:796–800 [DOI] [PubMed] [Google Scholar]
- 19.Boysen G, Marott JL, Grønbæk M, Hassanpour H, Truelsen T. Long-term survival after stroke: 30 years of follow-up in a cohort, the Copenhagen City Heart Study. Neuroepidemiology 2009;33:254–260 [DOI] [PubMed] [Google Scholar]
- 20.Hartmann A, Rundek T, Mast H, et al. Mortality and causes of death after first ischemic stroke: the Northern Manhattan Stroke Study. Neurology 2001;57:2000–2005 [DOI] [PubMed] [Google Scholar]
- 21.Vernino S, Brown RD, Jr, Sejvar JJ, Sicks JD, Petty GW, O'Fallon WM. Cause-specific mortality after first cerebral infarction: a population-based study. Stroke 2003;34:1828–1832 [DOI] [PubMed] [Google Scholar]
- 22.Rutten-Jacobs LA, Arntz RM, Maaijwee NM, et al. Long-term mortality after stroke among adults aged 18 to 50 years. JAMA 2013;309:1136–1144 [DOI] [PubMed] [Google Scholar]
- 23.Ezekowitz MD, Connolly S, Parekh A, et al. Rationale and design of RE-LY: randomized evaluation of long-term anticoagulant therapy, warfarin, compared with dabigatran. Am Heart J 2009;157:805–810.e2 [DOI] [PubMed] [Google Scholar]
- 24.ROCKET AF Study Investigators Rivaroxaban-once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation: rationale and design of the ROCKET AF Study. Am Heart J 2010;159:340–347.e1 [DOI] [PubMed] [Google Scholar]
- 25.Hart R, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 2007;146:857–867 [DOI] [PubMed] [Google Scholar]
- 26.Hylek EM, Go AS, Chang Y, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med 2003;349:1019–1026 [DOI] [PubMed] [Google Scholar]


