Abstract
Objective:
To determine the causative genetic lesion in 3 adult siblings with a slowly progressive, juvenile-onset phenotype comprising cerebellar atrophy and ataxia, intellectual decline, hearing loss, hypogonadism, hyperreflexia, a demyelinating sensorimotor neuropathy, and (in 2 of 3 probands) supratentorial white matter changes, in whom numerous prior investigations were nondiagnostic.
Methods:
The patients’ initial clinical assessment included history and physical examination, cranial MRI, and nerve conduction studies. We performed whole-exome sequencing of all 3 probands, followed by variant annotation and selection of rare, shared, recessive coding changes to identify the gene responsible. We next performed a panel of peroxisomal investigations in blood and cultured fibroblasts, including assessment of D-bifunctional protein (DBP) stability and activity by immunoblot and enzymologic methods, respectively.
Results:
Exome sequencing identified compound heterozygous mutations in HSD17B4, encoding peroxisomal DBP, in all 3 probands. Both identified mutations alter a conserved residue within the active site of DBP’s enoyl-CoA hydratase domain. Routine peroxisomal screening tests, including very long-chain fatty acids and phytanic acid, were normal. DBP enzymatic activity was markedly reduced.
Conclusion:
Exome sequencing provides a powerful and elegant tool in the specific diagnosis of “mild” or “atypical” neurometabolic disorders. Given the broad differential diagnosis and the absence of detectable biochemical abnormalities in blood, molecular testing of HSD17B4 should be considered as a first-line investigation in patients with compatible features.
Peroxisomal D-bifunctional protein (DBP) deficiency (OMIM 261515) is classically described as a Zellweger-like syndrome comprising neonatal encephalopathy, polyneuropathy, retinopathy, hearing loss, hepatomegaly, and dysmorphic features, and death in infancy. Autosomal recessive mutations of the gene HSD17B4 are responsible.1–3 Patients lack either or both of DBP’s 2 enzymatic activities (enoyl-CoA hydratase and d-3-hydroxyacyl-CoA dehydrogenase), which are essential for the oxidation of a wide range of peroxisomal substrates (very long-chain acyl-CoAs, branched-chain acyl-CoAs including pristanoyl-CoA, and bile acid precursors).4–7 Recently, HSD17B4 mutations have been identified in 4 persons with a relatively indolent, juvenile-onset condition comprising cerebellar ataxia, hearing loss, peripheral neuropathy, and premature ovarian failure; this disorder, termed type IV DBP deficiency, is allelic with some cases of Perrault syndrome (OMIM 233400).8,9
METHODS
Standard protocol approvals, registrations, and patient consents.
This study was approved by the McMaster University Research Ethics Board. Each participant (or legal guardian) signed an informed consent document before enrollment. Written consent to disclose health information was obtained from each individual.
Whole-exome sequencing and variant annotation.
Total leukocyte DNA was enriched using the Agilent SureSelect Human All Exon 50 Mb capture kit (Agilent Technologies, Santa Clara, CA), and subjected to bidirectional 100-bp paired-end sequencing (Illumina Hi-Seq 2000; Illumina, Inc., San Diego, CA). Mean exon coverage was 134–162×, with >98% of target base positions having at least 10× coverage. Sequence reads were aligned to the hg19 reference human genome using Burrows-Wheeler Aligner (http://bio-bwa.sourceforge.net), and duplicate reads were removed with MarkDuplicates (Picard tools version 1.35; http://picard.sourceforge.net). Alignments were refined using local realignment in Short Read Micro re-Aligner version 0.1.15 (http://sourceforge.net/projects/srma). Single nucleotide variants and insertion/deletions were detected using Genome Analysis Toolkit version 1.1.28 (http://www.broadinstitute.org/gatk) with default parameters. Single nucleotide variants and insertion/deletions were annotated with SnpEff (http://snpeff.sourceforge.net/) and filtered to remove common (frequency >0.01) polymorphisms by screening against the following databases: dbSNP (http://www.ncbi.nlm.nih.gov/projects/SNP/); 1000 Genomes (www.1000genomes.org); the NHLBI Exome Variant Server (http://evs.gs.washington.edu/EVS/); and data from 130 local control exomes. Filtered variants were annotated with SIFT (http://sift-dna.org) and PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2/). Mutations were confirmed by Sanger sequencing according to standard protocols.
RESULTS
Clinical description.
The patients were 3 adult siblings (2 women and 1 man) of nonconsanguineous Italian background, presenting with sensorineural hearing loss in middle childhood, followed by ataxia and progressive cognitive decline from adolescence onward. Clinical findings in these 3 individuals are summarized in table 1. Cranial MRI revealed marked cerebellar atrophy (figure 1); this was accompanied by a progressive peripheral neuropathy, with diminished deep tendon reflexes, reduced vibration sensation, and a demyelinating motor polyneuropathy on nerve conduction testing. Neuro-ophthalmic assessment, including dilated fundus examination, was normal. Symptoms were gradually progressive in all cases; however, the course of patient 2 was further complicated by episodes of left-sided weakness with abnormal eye movements and the appearance of multiple, gadolinium-enhancing white-matter lesions. These occurred in both infra- and supratentorial compartments, and in a pericallosal/periventricular distribution, including the presence of Dawson fingers. Oligoclonal bands were present in CSF; pulse steroids were given with a good initial response, and the patient was maintained on immunosuppressive therapy (initially with azathioprine, and later with fingolimod as newer agents became available). On follow-up imaging, the individual lesions exhibited interval evolution and contraction; however, there was a gradual overall progression of the supratentorial lesions toward confluence (figure 1). From a functional standpoint, the patient became wheelchair-bound at age 32 years, and at 38 years is now dependent for all aspects of his care. In comparison, both of his sisters have remained able to volunteer in the community. The eldest sister (patient 1; 39 years) had recently developed nonspecific T2 signal changes in her deep white matter, along with bilateral pallidal mineral deposition. The youngest (patient 3; 35 years) had not been imaged since 2001.
Table 1.
Clinical findings in juvenile DBP deficiency

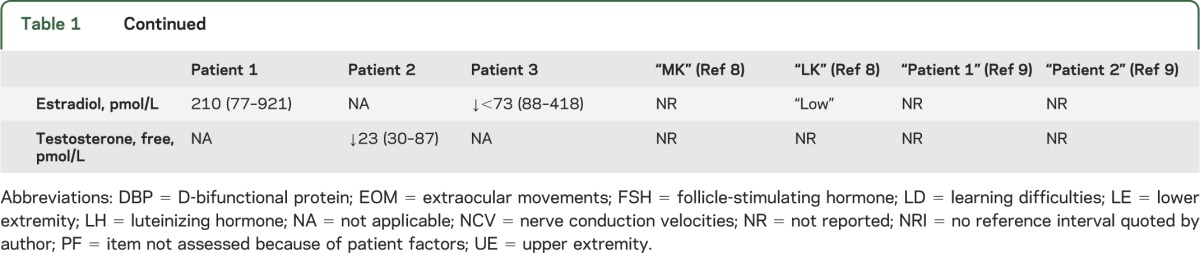
Figure. Cranial MRI findings in D-bifunctional protein deficiency.
(A–C) Cranial MRI of patient 1 shows marked, diffuse cerebellar atrophy without cerebral atrophy. (D–F) MRI of patient 2 (clinically more severe) shows an even greater degree of cerebellar atrophy, with additional cystic white matter lesions, thinned corpus callosum, and diffuse cerebral volume loss.
Before this study, the patients underwent a panoply of diagnostic and laboratory investigations, none of which revealed a specific diagnosis. These included very long-chain fatty acids and phytanic acid in plasma (normal, genomic microarray, muscle biopsy) with full mitochondrial disease workup, and genetic testing for each of the following: spinocerebellar ataxia types 1, 2, 3, 6, 7, 8, and 17, Friedreich ataxia, autosomal recessive hereditary spastic paraplegias (CYP7B1, SPG11, SPG7, SPG15, PNPLA6, SPG20, SPG21, CCT5, and SPG44), and autosomal recessive spastic ataxia of Charlevoix-Saguenay.
Mutation identification.
To identify the causative gene in this family, we conducted whole-exome sequencing at The Centre for Applied Genomics (see methods), revealing the presence of 2 rare, nonsynonymous coding variants in HSD17B4 in all 3 affected individuals. The specific mutations identified were NM_000414.3:c.1537C>A (p.Pro513Thr; maternally inherited) and c.1628G>C (p.Arg543Pro; paternally inherited). Both of these mutations alter a highly conserved residue within the active site of DBP’s enoyl-CoA hydratase domain (figure e-1 on the Neurology® Web site at Neurology.org).
Biochemical features.
In light of the molecular findings, a more detailed assessment of peroxisomal function in both plasma and skin fibroblasts (table 2) was undertaken. Of note, total serum bile acids were increased (approximately 2-fold) in all cases; phytanic and very long-chain fatty acids were normal. DBP enoyl-CoA hydratase activity was markedly reduced, confirming the diagnosis. The normal 45-kDa fragment containing DBP’s (posttranslationally cleaved) hydratase domain was absent by immunoblot in patient fibroblasts (figure e-2).
Table 2.
Peroxisomal investigations in blood and cultured fibroblasts

DISCUSSION
This report increases to 7 the total number of reported individuals with juvenile-onset DBP deficiency; our study participants are the oldest reported patients to date. All reported diagnoses of juvenile DBP deficiency to date have been accomplished by whole-exome sequencing, rather than by conventional clinical means. The difficulty in clinically recognizing this condition stems from (1) its extreme rarity, (2) its poor resemblance to the classic neonatal form, and (3) the presence of many of its key findings in other, relatively common, conditions. For instance, compatible symptoms may be seen in many of the spinocerebellar ataxias and in the complicated hereditary spastic paraplegias SPG7 (OMIM 607259), SPG20 (Troyer syndrome, OMIM 275900), and SPG21 (Mast syndrome, OMIM 248900), and in mitochondrial diseases. Given the low pretest probability for each of these disorders, exome- or panel-based molecular testing may indeed be the most practical initial test in patients with overlapping clinical presentations.
White matter lesions, a variable feature in our patients, are a known sequela of classic DBP deficiency, with periventricular cerebral demyelination and callosal thinning reported to occur in 17% and 55% of cases, respectively.2 As far as we are aware, white matter disease has not previously been reported in later (juvenile)-onset patients. The presence of CSF oligoclonal bands in patient 2 is interesting, especially considering the recent report of severe, chronic cerebral inflammation in knockout mice lacking DBP.10 Whether this represents simple coincidence vs an autoimmune component to the disease process itself is unclear.
No proven treatments exist to address the underlying biochemical defect in this disorder, although dietary phytanic acid restriction and/or bile acid supplementation may warrant further study. Although our probands do not demonstrate phytanic acid accumulation in peripheral blood, concentrations in other tissues (e.g., CSF and brain tissue) are unknown. It is reasonable to suppose that juvenile-onset patients may possess a degree of residual enzyme activity in vivo; enhancing this (e.g., via chaperone therapy) is another possible approach. Although the number of reported patients is currently too few to permit clinical trials, the recognized prevalence of this disorder is likely to increase as exome sequencing enters the clinical mainstream.
Supplementary Material
ACKNOWLEDGMENT
The authors gratefully acknowledge the participation of the patients and family, without whom this work could not be undertaken. This work was selected for study by the FORGE Canada Steering Committee, consisting of K. Boycott (University of Ottawa), A. Mackenzie (University of Ottawa), M. Samuels (University of Montreal), F. Bernier (University of Calgary), and M. Innes (University of Calgary).
GLOSSARY
- CoA
coenzyme A
- DBP
D-bifunctional protein
- OMIM
Online Mendelian Inheritance in Man
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Dr. Lines and Dr. Jobling: analysis and interpretation, drafting and critical revision of the manuscript. L. Brady: acquisition of data, analysis and interpretation, critical revision of the manuscript. Dr. Marshall: acquisition of data, analysis and interpretation, drafting and critical revision of the manuscript. Dr. Scherer: analysis and interpretation, critical revision of the manuscript. Dr. Rodriguez, Dr. Lee, Dr. Mestre, and Dr. Lang: acquisition of data, critical revision of the manuscript. Dr. Wanders: analysis and interpretation, critical revision of the manuscript. Dr. Ferdinandusse: acquisition of data, analysis and interpretation, critical revision of the manuscript. Dr. Tarnopolsky: study concept and design, acquisition of data, analysis and interpretation, critical revision of the manuscript, study supervision.
STUDY FUNDING
Supported by Genome Canada, the Canadian Institutes of Health Research, and the Ontario Genomics Institute (OGI-049), with additional funding from Genome Québec, Genome British Columbia, The University of Toronto McLaughlin Centre, and The Centre for Applied Genomics.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Clayton PT, Lake BD, Hjelm M, et al. Bile acid analyses in “pseudo-Zellweger” syndrome: clues to the defect in peroxisomal beta-oxidation. J Inherit Metab Dis 1988;11:165–168 [DOI] [PubMed] [Google Scholar]
- 2.Ferdinandusse S, Denis S, Mooyer PA, et al. Clinical and biochemical spectrum of D-bifunctional protein deficiency. Ann Neurol 2006;59:92–104 [DOI] [PubMed] [Google Scholar]
- 3.Suzuki Y, Jiang LL, Souri M, et al. D-3-hydroxyacyl-CoA dehydratase/D-3-hydroxyacyl-CoA dehydrogenase bifunctional protein deficiency: a newly identified peroxisomal disorder. Am J Hum Genet 1997;61:1153–1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adamski JF, Normand T, Leenders F, et al. Molecular cloning of a novel widely expressed human 80 kDa 17 beta-hydroxysteroid dehydrogenase IV. Biochem J 1995;311:437–443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Möller G, van Grunsven EG, Wanders RJ, Adamski J. Molecular basis of D-bifunctional protein deficiency. Mol Cell Endocrinol 2001;171:61–70 [DOI] [PubMed] [Google Scholar]
- 6.Adamski JF, Leenders F, Carstensen JF, et al. Steroids, fatty acyl-CoA, and sterols are substrates of 80-kDa multifunctional protein. Steroids 1997;62:159–163 [DOI] [PubMed] [Google Scholar]
- 7.Ferdinandusse S, Ylianttila MS, Gloerich J, et al. Mutational spectrum of D-bifunctional protein deficiency and structure-based genotype-phenotype analysis. Am J Hum Genet 2006;78:112–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pierce SB, Walsh T, Chisholm KM, et al. Mutations in the DBP-deficiency protein HSD17B4 cause ovarian dysgenesis, hearing loss, and ataxia of Perrault syndrome. Am J Hum Genet 2010;87:282–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McMillan HJ, Worthylake T, Schwartzentruber J, et al. Specific combination of compound heterozygous mutations in 17beta-hydroxysteroid dehydrogenase type 4 (HSD17B4) defines a new subtype of D-bifunctional protein deficiency. Orphanet J Rare Dis 2012;7:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verheijden S, Bottelbergs A, Krysko O, et al. Peroxisomal multifunctional protein-2 deficiency causes neuroinflammation and degeneration of Purkinje cells independent of very long chain fatty acid accumulation. Neurobiol Dis 2013;58:258–269 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



