Abstract
Background
Adjacent segment disease has become a common topic in spine surgery circles because of the significant increase in fusion surgery in recent years and the development of motion preservation technologies that theoretically should lead to a decrease in this pathology. The purpose of this review is to organize the evidence available in the current literature on this subject.
Methods
For this literature review, a search was conducted in PubMed with the following keywords: adjacent segment degeneration and disease. Selection, review, and analysis of the literature were completed according to level of evidence.
Results
The PubMed search identified 850 articles, from which 41 articles were selected and reviewed. The incidence of adjacent segment disease in the cervical spine is close to 3% without a significant statistical difference between surgical techniques (fusion vs arthroplasty). Authors report the incidence of adjacent segment disease in the lumbar spine to range from 2% to 14%. Damage to the posterior ligamentous complex and sagittal imbalances are important risk factors for both degeneration and disease.
Conclusion
Insufficient evidence exists at this point to support the idea that total disc arthroplasty is superior to fusion procedures in minimizing the incidence of adjacent segment disease. The etiology is most likely multifactorial but it is becoming abundantly clear that adjacent segment disease is not caused by motion segment fusion alone. Fusion plus the presence of abnormal end-fusion alignment appears to be a major factor in creating end-fusion stresses that result in adjacent segment degeneration and subsequent disease. The data presented cast further doubt on previously established rationales for total disc arthroplasty, at least with regard to the effect of total disc arthroplasty on adjacent segment degeneration pathology.
Keywords: Arthrodesis, arthroplasty, cervical vertebrae, intervertebral disc degeneration, lumbar vertebrae, spinal diseases, spinal fusion, total disc replacement
INTRODUCTION
Adjacent segment disease (ASDis) has become a common topic in spine surgery circles because of the significant increase in fusion surgery in recent years and the development of motion preservation technologies that theoretically should lead to a decrease in this pathology.1-4 ASDis is defined as new degenerative changes at a spinal level adjacent to a surgically treated level or levels in the spine, accompanied by related symptoms (radiculopathy, myelopathy, or instability). Adjacent segment degeneration (ASDeg) represents the radiographic changes without the symptomatology.5 An important question remains unanswered: are adjacent disc degeneration and disease the result of the natural history of age-related degeneration or are they the result of adjacent segment fusion that has led to the adjacent segment changes?
ETIOLOGY
The etiology of ASDis is most likely multifactorial; no study to date has proven that a single risk factor directly correlates with this pathology. The natural history of degeneration, changes in intradiscal pressure, anatomy disruption, and sagittal malalignment have been proposed as etiologic factors for this pathology.1-3
NATURAL HISTORY
As the cervical spine ages, degenerative changes tend to occur naturally, a progression that complicates attempts to determine whether ASDis results from surgical fusion, natural history, or other causes.
Boden et al6 studied asymptomatic subjects using magnetic resonance imaging (MRI) of the cervical spine. Imaging abnormalities were found in 14% of the individuals aged <40 years and 28% of the individuals aged >40 years, clearly indicating an age-related degeneration.
In a study of cervical noninstrumented arthrodesis patients who had undergone single or multilevel anterior cervical discectomy and fusions (ACDF), Hilibrand et al7 observed that age, abnormal segmental motion, and preexisting disease were risk factors for the development of ASDis. The incidence of ASDis was less in patients with multilevel fusions than in patients with single-level fusions. This finding is in conflict with the belief that fusion increases biomechanical stress at the adjacent level. A multilevel fusion, in which the exerted bending moment is greater than that of a single-level fusion, is intuitively expected to lead to an increased incidence of ASDis. Observations such as the one made by Hilibrand et al likely result from the fact that most ACDFs are performed at the most degeneration-prone levels, leaving the remaining degeneration-resistant levels unfused. In such cases, the incidence of ASDis is diminished.
Matsumoto et al8 compared patients who had undergone ACDF to healthy control patients at 10-year follow-up. After performing MRI studies, the authors concluded that ACDF increases the incidence of adjacent level degeneration. A major drawback of this study is that the groups did not represent matched cohorts and the patients in the ACDF group were older (approximately 6.2 years) than the patients in the control group. Additionally, the fact that this group had already undergone ACDFs suggests that these patients were more susceptible to the development of disc degeneration than the patients in the control group.
Although no conclusive etiology exists for ASDis, natural history seems to be an important factor.
ANATOMY DISRUPTION ADJACENT TO PRIOR SURGICAL LEVEL
Soft tissue disruption adjacent to the surgical level is considered a potential cause of ASDeg and subsequent ASDis. Nassr et al found a threefold increase in degeneration at the level where a needle was placed for radiographic localization purposes.9 The authors alleged that the puncture of the annulus caused the subsequent degeneration. Other studies have demonstrated the association between adjacent level ossification and the positioning of the ACDF plate within 5 mm of the adjacent level, highlighting the importance of preserving the soft tissue anatomy of the adjacent level to avoid further adjacent segment degeneration.10,11
INTRADISCAL PRESSURE ADJACENT TO THE SURGICAL LEVEL
Biomechanical studies have shown increased intradiscal pressure (mechanical stress) on the adjacent discs after a single-level fusion model.12 This pressure is particularly high in flexion-extension when fusion is compared to total disc arthroplasty (TDA) and baseline. In theory, the increase of mechanical stresses may lead to an increase in ASDeg and ultimately to ASDis. Even though this theory was the rationale for the development of TDA, current clinical studies have failed to demonstrate this direct correlation, and so far the difference in ASDis incidence among the fusion vs TDA groups is not statistically significant.13
SAGITTAL ALIGNMENT AND POSTURE
Postoperative spinal malalignment is a major stressor of intradiscal mechanics and a contributor to a motion segment and ASDeg in the cervical and lumbar spines.14-21 Several studies have shown that postoperative spinal pelvic parameters, most notably a large pelvic incidence angle and small lumbar lordotic angle, are associated with greater risk of adjacent segment stresses and degenerative changes.15,17-22 Specifically regarding lumbar lordotic angle, the maintenance of lumbar lordosis following fusion results in a diminished incidence of adjacent segment stresses and instability compared to a kyphotic spine.17,22 Sagittal alignment is strongly related to segmental mobility and disc degeneration.14-21,23,24
THE EVIDENCE: FUSION VS TDA AND ADJACENT SEGMENT DISEASE
Cervical Literature
Many randomized controlled trials (RCTs) have been published on TDA of the cervical spine vs fusion (Table 1). Even though the results favor TDA over fusion, none of the RCTs has demonstrated a statistically significant difference regarding the incidence of ASDis.25-31 The reported annual incidence of ASDis in fusion patients is approximately 3%.4 Nunley et al25 reexamined current evidence on ASDis in patients who underwent TDA and found an annual incidence of 3.1% regardless of the patient's age, sex, smoking habits, and design of the disc replacement device.
Table 1.
Summary of Relevant Studies on Cervical Adjacent Segment Degeneration and Disease
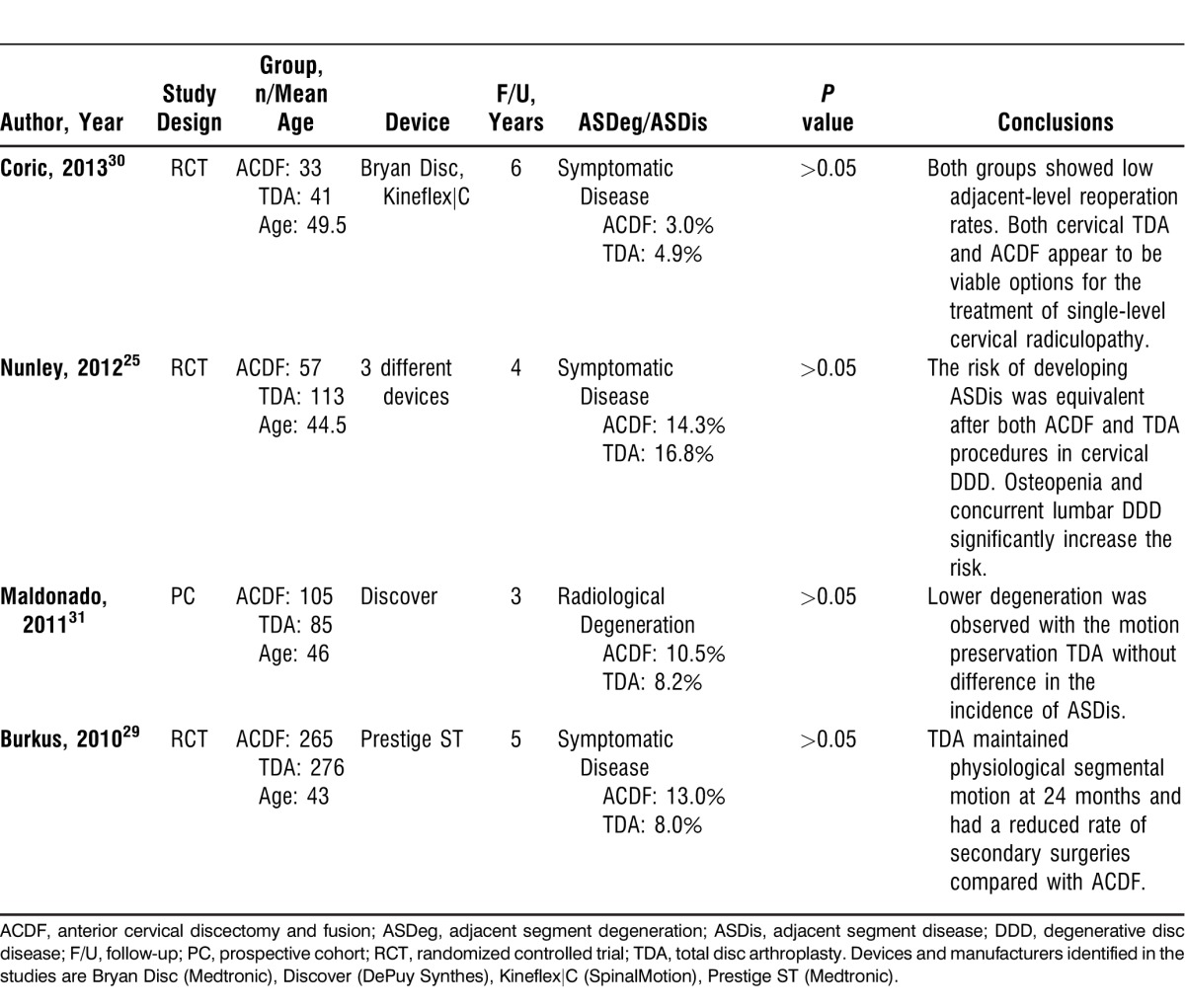
Burkus et al29 have shown that TDA using a Prestige ST ball-in-socket device (Medtronic) is a motion-preserving procedure that at 24-month follow-up maintained a greater range of motion compared to ACDF. The incidence of ASDis was lower in the TDA group than the ACDF group; however, the difference was not statistically significant.
Maldonado et al31 compared radiographic degeneration in patients who had undergone either ACDF or TDA; they found a lower rate of ASDeg in the TDA group but no correlation with a lower incidence of symptomatic disease.
Nunley et al25 studied more than 200 patients randomized between ACDF and TDA using 3 different disc replacement devices. The incidence of ASDis was equivalent in both groups. However, they observed that the presence of lumbar degenerative disease and osteopenia increases the risk of developing symptomatic cervical ASDis.
Coric et al30 reported a surprisingly low rate of ASDis following surgery and concluded that both ACDF and TDA are viable options for the treatment of single-level cervical radiculopathy.
A series of published meta-analyses on the same subject has shown minimal clinically relevant differences between TDA and ACDF; most importantly, no significant difference was demonstrated in terms of ASDis.26-28,32-34
Lumbar Literature
The reported incidence of lumbar spine ASDeg and ASDis ranges widely (Table 2); this range can be attributed to the variety of techniques used to address the lumbar spine pathology.35
Table 2.
Summary of Relevant Studies on Lumbar Adjacent Segment Degeneration and Disease
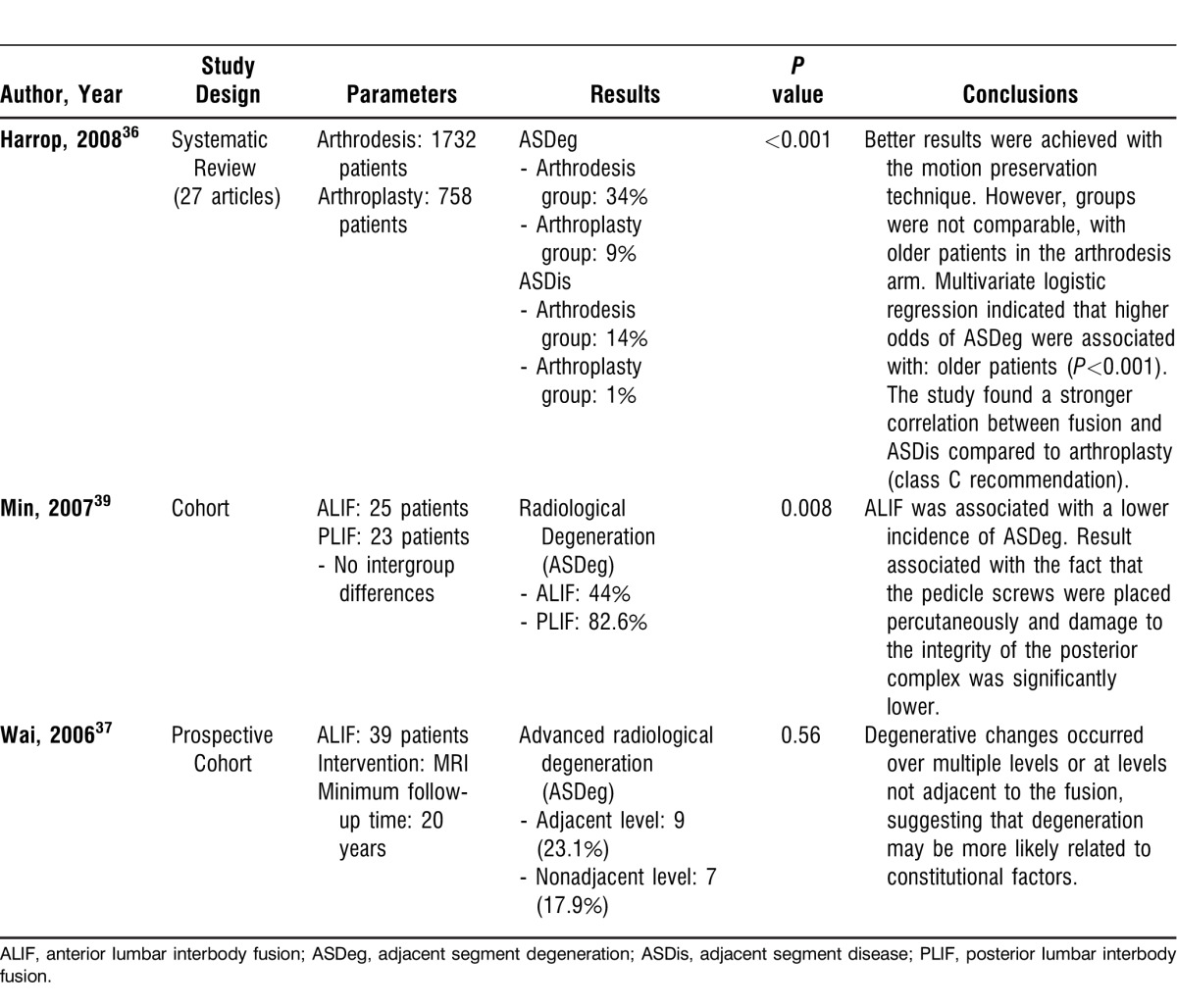
In a systematic review, Harrop et al compared arthrodesis vs arthroplasty in the lumbar spine.36 In the fusion group, the incidence of ASDeg was 34% and the incidence of ASDis was 14%. In the TDA group, the incidence was significantly lower—9% ASDeg and 1% ASDis. A limitation of the study was that the patients in the arthrodesis arm were significantly older and likely more susceptible to degeneration.
For more than 20 years, Wai et al followed patients who had undergone anterior lumbar interbody fusion (ALIF) with MRI.37 They found that 6% of the patients required surgery at the adjacent level and noted a similar incidence of adjacent level degeneration compared with nonadjacent levels (23.1% and 17.9%, respectively). The authors concluded that the ASDis was more likely related to the natural history of disc degeneration rather than altered biomechanics at the adjacent level.37
Ishihara et al38 found the incidence of ASDeg to be 52% at the rostral adjacent level and 70% at the caudal adjacent level after ALIF for isthmic spondylolisthesis, but they did not correlate these findings with symptomatic disease.
Min et al39 compared ALIFs vs posterior lumbar interbody fusions (PLIFs) for lumbar spondylolisthesis. They found the incidence of ASDeg to be 44% with ALIF and 82.6% with PLIF. In the ALIF group, posterior instrumentation with pedicle screws was performed percutaneously. This result suggests that ALIF may reduce damage to the integrity of the posterior complex, which is known to be an important risk factor for ASDis.
Radcliff et al found an annual ASDis incidence of 2% to 3% after decompression and stabilization procedures.40 Factors consistently associated with ASDis included laminectomy adjacent to a fusion and a sagittal imbalance.
CONCLUSION
The incidence of ASDis in the cervical spine is close to 3% per year and no statistical difference is observed when TDA is compared to fusion.1-4,25,29-31 In the lumbar spine the incidence ranges from 2% to 14%.35-40 Damage to the posterior ligamentous complex and sagittal imbalances are important risk factors.
Insufficient evidence exists at this point to support the idea that TDA is superior to ACDF regarding minimizing the incidence of ASDis.
The literature clearly suggests that ASDis is not caused by motion segment fusion alone.4,14,16,24,41 Fusion plus the presence of abnormal end-fusion alignment (usually kyphosis) appears to be a major factor in creating end-fusion stresses that result in ASDeg and ASDis. The data presented cast further doubt on previously established rationales for TDA, at least with regard to the effect of TDA on ASDeg pathology.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J. Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg Spine. 2007 Jul;7(1):33–39. doi: 10.3171/SPI-07/07/033. [DOI] [PubMed] [Google Scholar]
- 2.Finn MA, Brodke DS, Daubs M, Patel A, Bachus KN. Local and global subaxial cervical spine biomechanics after single-level fusion or cervical arthroplasty. Eur Spine J. 2009 Oct;18(10):1520–1527. doi: 10.1007/s00586-009-1085-7. Epub 2009 Jul 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anakwenze OA, Auerbach JD, Milby AH, Lonner BS, Balderston RA. Sagittal cervical alignment after cervical disc arthroplasty and anterior cervical discectomy and fusion: results of a prospective, randomized, controlled trial. Spine (Phila Pa 1976) 2009 Sep 1;34(19):2001–2007. doi: 10.1097/BRS.0b013e3181b03fe6. [DOI] [PubMed] [Google Scholar]
- 4.Cho SK, Riew KD. Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg. 2013 Jan;21(1):3–11. doi: 10.5435/JAAOS-21-01-3. [DOI] [PubMed] [Google Scholar]
- 5.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004 Nov-Dec;4((6 Suppl)):190S–194S. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990 Sep;72(8):1178–1184. [PubMed] [Google Scholar]
- 7.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999 Apr;81(4):519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Matsumoto M, Okada E, Ichihara D, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010 Jan 1;35(1):36–43. doi: 10.1097/BRS.0b013e3181b8a80d. [DOI] [PubMed] [Google Scholar]
- 9.Nassr A, Lee JY, Bashir RS, et al. Does incorrect level needle localization during anterior cervical discectomy and fusion lead to accelerated disc degeneration? Spine (Phila Pa 1976) 2009 Jan 15;34(2):189–192. doi: 10.1097/BRS.0b013e3181913872. [DOI] [PubMed] [Google Scholar]
- 10.Kim HJ, Kelly MP, Ely CG, Dettori JR, Riew KD. The risk of adjacent-level ossification development after surgery in the cervical spine: are there factors that affect the risk? A systematic review. Spine (Phila Pa 1976) 2012 Oct 15;37((22 Suppl)):S65–S74. doi: 10.1097/BRS.0b013e31826cb8f5. Erratum in: Spine (Phila Pa 1976). 2013 Jan 1;38(1):E49. [DOI] [PubMed] [Google Scholar]
- 11.Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am. 2005 Mar;87(3):558–563. doi: 10.2106/JBJS.C.01555. [DOI] [PubMed] [Google Scholar]
- 12.Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine (Phila Pa 1976) 2005 May 15;30(10):1165–1172. doi: 10.1097/01.brs.0000162441.23824.95. [DOI] [PubMed] [Google Scholar]
- 13.Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002 Nov 15;27(22):2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 14.Levin DA, Hale JJ, Bendo JA. Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bull NYU Hosp Jt Dis. 2007;65(1):29–36. [PubMed] [Google Scholar]
- 15.Park JY, Cho YE, Kuh SU, et al. New prognostic factors for adjacent-segment degeneration after one-stage 360 degrees fixation for spondylolytic spondylolisthesis: special reference to the usefulness of pelvic incidence angle. J Neurosurg Spine. 2007 Aug;7(2):139–144. doi: 10.3171/SPI-07/08/139. [DOI] [PubMed] [Google Scholar]
- 16.Hwang SH, Kayanja M, Milks RA, Benzel EC. Biomechanical comparison of adjacent segmental motion after ventral cervical fixation with varying angles of lordosis. Spine J. 2007 Mar-Apr;7(2):216–221. doi: 10.1016/j.spinee.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 17.Hioki A, Miyamoto K, Kodama H, et al. Two-level posterior lumbar interbody fusion for degenerative disc disease: improved clinical outcome with restoration of lumbar lordosis. Spine J. 2005 Nov-Dec;5(6):600–607. doi: 10.1016/j.spinee.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Sudo H, Oda I, Abumi K, Ito M, Kotani Y, Minami A. Biomechanical study on the effect of five different lumbar reconstruction techniques on adjacent-level intradiscal pressure and lamina strain. J Neurosurg Spine. 2006 Aug;5(2):150–155. doi: 10.3171/spi.2006.5.2.150. [DOI] [PubMed] [Google Scholar]
- 19.Vialle R, Ilharreborde B, Dauzac C, Lenoir T, Rillardon L, Guigui P. Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study. Eur Spine J. 2007 Oct;16(10):1641–1649. doi: 10.1007/s00586-007-0348-4. Epub 2007 Apr 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007 Sep;16(9):1459–1467. doi: 10.1007/s00586-006-0294-6. Epub 2007 Jan 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hresko MT, Labelle H, Roussouly P, Berthonnaud E. Classification of high-grade spondylolistheses based on pelvic version and spine balance: possible rationale for reduction. Spine (Phila Pa 1976) 2007 Sep 15;32(20):2208–2213. doi: 10.1097/BRS.0b013e31814b2cee. [DOI] [PubMed] [Google Scholar]
- 22.Chen WJ, Lai PL, Tai CL, Chen LH, Niu CC. The effect of sagittal alignment on adjacent joint mobility after lumbar instrumentation—a biomechanical study of lumbar vertebrae in a porcine model. Clin Biomech (Bristol, Avon) 2004 Oct;19(8):763–768. doi: 10.1016/j.clinbiomech.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 23.Keorochana G, Taghavi CE, Lee KB, et al. Effect of sagittal alignment on kinematic changes and degree of disc degeneration in the lumbar spine: an analysis using positional MRI. Spine (Phila Pa 1976) 2011 May 15;36(11):893–898. doi: 10.1097/BRS.0b013e3181f4d212. [DOI] [PubMed] [Google Scholar]
- 24.Ozer E, Yücesoy K, Yurtsever C, Seçil M. Kyphosis one level above the cervical disc disease: is the kyphosis cause or effect? J Spinal Disord Tech. 2007 Feb;20(1):14–19. doi: 10.1097/01.bsd.0000211274.74238.c0. [DOI] [PubMed] [Google Scholar]
- 25.Nunley PD, Jawahar A, Kerr EJ. 3rd, et al. Factors affecting the incidence of symptomatic adjacent-level disease in cervical spine after total disc arthroplasty: 2- to 4-year follow-up of 3 prospective randomized trials. Spine (Phila Pa 1976) 2012 Mar 15;37(6):445–451. doi: 10.1097/BRS.0b013e31822174b3. [DOI] [PubMed] [Google Scholar]
- 26.Bartels RH, Donk R, Verbeek AL. No justification for cervical disk prostheses in clinical practice: a meta-analysis of randomized controlled trials. Neurosurgery. 2010 Jun;66(6):1153–1160. doi: 10.1227/01.NEU.0000369189.09182.5F. discussion 1160. [DOI] [PubMed] [Google Scholar]
- 27.Gao Y, Liu M, Li T, Huang F, Tang T, Xiang Z. A meta-analysis comparing the results of cervical disc arthroplasty with anterior cervical discectomy and fusion (ACDF) for the treatment of symptomatic cervical disc disease. J Bone Joint Surg Am. 2013 Mar 20;95(6):555–561. doi: 10.2106/JBJS.K.00599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McAfee PC, Reah C, Gilder K, Eisermann L, Cunningham B. A meta-analysis of comparative outcomes following cervical arthroplasty or anterior cervical fusion: results from 4 prospective multicenter randomized clinical trials and up to 1226 patients. Spine (Phila Pa 1976) 2012 May 15;37(11):943–952. doi: 10.1097/BRS.0b013e31823da169. [DOI] [PubMed] [Google Scholar]
- 29.Burkus JK, Haid RW, Traynelis VC, Mummaneni PV. Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine. 2010 Sep;13(3):308–318. doi: 10.3171/2010.3.SPINE09513. [DOI] [PubMed] [Google Scholar]
- 30.Coric D, Kim PK, Clemente JD, Boltes MO, Nussbaum M, James S. Prospective randomized study of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up: results in 74 patients from a single site. J Neurosurg Spine. 2013 Jan;18(1):36–42. doi: 10.3171/2012.9.SPINE12555. [DOI] [PubMed] [Google Scholar]
- 31.Maldonado CV, Paz RD, Martin CB. Adjacent-level degeneration after cervical disc arthroplasty versus fusion. Eur Spine J. 2011 Aug;20(Suppl 3):403–407. doi: 10.1007/s00586-011-1916-1. Epub 2011 Jul 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heller JG, Sasso RC, Papadopoulos SM, et al. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 2009 Jan 15;34(2):101–107. doi: 10.1097/BRS.0b013e31818ee263. [DOI] [PubMed] [Google Scholar]
- 33.Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007 Mar;6(3):198–209. doi: 10.3171/spi.2007.6.3.198. [DOI] [PubMed] [Google Scholar]
- 34.Murrey D, Janssen M, Delamarter R, et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009 Apr;9(4):275–286. doi: 10.1016/j.spinee.2008.05.006. Epub 2008 Sep 6. [DOI] [PubMed] [Google Scholar]
- 35.Helgeson MD, Bevevino AJ, Hilibrand AS. Update on the evidence for adjacent segment degeneration and disease. Spine J. 2013 Mar;13(3):342–351. doi: 10.1016/j.spinee.2012.12.009. Epub 2013 Feb 15. [DOI] [PubMed] [Google Scholar]
- 36.Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976) 2008 Jul 1;33(15):1701–1707. doi: 10.1097/BRS.0b013e31817bb956. [DOI] [PubMed] [Google Scholar]
- 37.Wai EK, Santos ER, Morcom RA, Fraser RD. Magnetic resonance imaging 20 years after anterior lumbar interbody fusion. Spine (Phila Pa 1976) 2006 Aug 1;31(17):1952–1956. doi: 10.1097/01.brs.0000228849.37321.a8. [DOI] [PubMed] [Google Scholar]
- 38.Ishihara H, Osada R, Kanamori M, et al. Minimum 10-year follow-up study of anterior lumbar interbody fusion for isthmic spondylolisthesis. J Spinal Disord. 2001 Apr;14(2):91–99. doi: 10.1097/00002517-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 39.Min JH, Jang JS, Lee SH. Comparison of anterior- and posterior-approach instrumented lumbar interbody fusion for spondylolisthesis. J Neurosurg Spine. 2007 Jul;7(1):21–26. doi: 10.3171/SPI-07/07/021. [DOI] [PubMed] [Google Scholar]
- 40.Radcliff KE, Kepler CK, Jakoi A, et al. Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J. 2013. Jun 14, [Epub ahead of print] [DOI] [PubMed]
- 41.Kolstad F, Nygaard ØP, Leivseth G. Segmental motion adjacent to anterior cervical arthrodesis: a prospective study. Spine (Phila Pa 1976) 2007 Mar 1;32(5):512–517. doi: 10.1097/01.brs.0000256448.04035.bb. [DOI] [PubMed] [Google Scholar]


