Abstract
Importance
Fiscal food policies (e.g., taxation) are increasingly proposed to improve population-level health, but their impact on health disparities is unknown.
Objective
We estimated subgroup-specific effects of fast food price changes on fast food consumption and cardio-metabolic outcomes, hypothesizing inverse associations between fast food price with fast food consumption, BMI, and insulin resistance and stronger associations among blacks (vs. whites) and participants with relatively lower education or income.
Design
20-year follow-up (5 exams) in a biracial U.S. prospective cohort: Coronary Artery Risk Development in Young Adults (CARDIA) (1985/86–2005/06, baseline n=5,115).
Participants
Aged 18–30 at baseline; designed for equal recruitment by race (black/white), educational attainment, age, and gender.
Exposures
Community-level price data from the Council for Community and Economic Research (C2ER) temporally- and geographically-linked to study participants’ home address at each exam.
Main outcome and measures
Participant-reported number of fast food eating occasions per week; BMI (kg/m2) from clinical assessment of weight and height; homeostatic model assessment insulin resistance (HOMA-IR) from fasting glucose and insulin. Covariates included individual- and community-level social and demographic factors.
Results
In repeated measures regression, multivariable-adjusted associations between fast food price and consumption were non-linear (quadratic, p<0.001), with significant inverse estimated effects on consumption at higher prices; estimates varied according to race (interaction term p=0.04), income (p=0.07), and education (p=0.03). For example, at the 10th percentile of price ($1.25/serving), blacks and whites had mean fast food consumption (times/week) of 2.2 (95% CI: 2.1–2.3) and 1.6 (1.5–1.7), respectively, while at the 90th percentile of price ($1.53/serving), respective mean consumption estimates were 1.9 (1.8–2.0) and 1.5 (1.4–1.6). We observed differential price effects on HOMA-IR (inverse for lower educational status and at middle income) and BMI (inverse for blacks, lower education, and middle income; positive for whites, high education, and high income).
Conclusions
We found greater fast food price sensitivity on fast food consumption and insulin resistance among sociodemographic groups that have a disproportionate burden of chronic disease. Our findings have implications for fiscal policy approaches related to diet, particularly with respect to possible effects of fast food taxes among populations with diet-related health disparities.
INTRODUCTION
Fiscal policies, such as targeted taxes or subsidies, to motivate healthy diet choices, have received increased consideration as obesity prevention strategies1,2. Research shows a role for food price on dietary consumption3–7 and diet-related health outcomes, such as obesity4,8. Economic theory suggests lower income individuals are more sensitive to price changes9,10. Recent findings support greater response to food prices among sociodemographic subpopulations at higher risk for diet-related health outcomes, such as racial minorities or low income11,12. However, most prior work on food price effects has been small experiments and cross-sectional studies, and has yielded inconsistent results3,8,13,14.
The fast food sector is frequently the target of policy discussion related to the literature linking fast food intake with super-sized portion sizes, poor nutrient intake patterns, excessive caloric intake, and obesity15–19. These studies have found distinctly different patterns of fast food access and intake among low-socioeconomic status (SES) subpopulations20, leading cities (e.g., Los Angeles), to ban the building of new fast food restaurants in selected low SES areas21 or to suggest beverage portion size limitations (e.g., New York City).
We quantified the associations between community-level fast food prices and individual-level fast food consumption, insulin resistance, and body weight within sociodemographic subgroups over 20 years of follow-up in a biracial cohort of young and middle-aged adults. We hypothesized greater price effects among blacks, as compared to whites, and among participants with relatively lower educational attainment or income. These questions are relevant to fiscal policy considerations1,2, and particularly to pricing strategies for eliminating disparities in dietary behaviors and health outcomes.
METHODS
Study sample
CARDIA is a multicenter, longitudinal study of cardiometabolic risk factors in adulthood22. Black and white adults (aged 18–30, n=5,115) were recruited from four metropolitan areas (Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA). Participants were recruited for balance with respect to age, gender, race, and education. Of the surviving cohort, 81% were examined at a year 7 follow-up, 79% at year 10, 74% at year 15, and 72% at year 20. The study protocol was approved by institutional review boards of each participating institution; each study participant provided informed written consent.
Study data
Dietary assessment
Frequency of fast food consumption was assessed with the question: “How many times in a week or month do you eat breakfast, lunch, or dinner in a place such as McDonald’s, Burger King, Wendy’s, Arby’s, Pizza Hut, or Kentucky Fried Chicken?” At years 7 and 10, the frequency of eating at restaurants or cafeterias, which may serve as a substitution venue to fast food establishments, was also queried: “How many times in a week or month do you eat breakfast, lunch or dinner at a restaurant or cafeteria (eat-in or take-out)?” We note that participant responses to these two questions may not reflect mutually exclusive venue choices.
Clinical measures
At each exam, weight (to 0.1 kg) and height (to 0.5 cm) were measured by trained clinical staff; body mass index (BMI) was calculated as kg/m2. Fasting insulin and glucose concentrations were obtained from venous blood draws. Glucose was measured using hexokinase coupled to glucose-6-phosphate dehydrogenase. The homeostasis model assessment of insulin resistance (HOMA-IR) score was calculated as: [fasting glucose (in millimoles per liter) x fasting insulin (in microunits per liter)]/22.5. Higher scores indicated increased insulin resistance23.
Food prices
Consumer price data were from the Council for Community and Economic Research (C2ER)24. Each quarter, the C2ER ascertained prices of more than 60 consumer goods and services to estimate cost of living for approximately 300 US cities.
The C2ER collected price data for 3 fast food items: a 12-inch thin crust cheese pizza from Pizza Hut/Pizza Inn, a ¼ pound burger with cheese from McDonald’s, and 2 pieces of fried chicken from Kentucky Fried Chicken/Church’s Fried Chicken. We rescaled the price of pizza by dividing by 4 for serving-size comparability (on a calorie basis) with the burger and fried chicken, and created a fast food index as the equal-weighted average of the 3 fast food items. Our rescaling insured that the price index was not dominated by pizza ($4.92 at baseline vs. $1.66 for burger and $1.66 chicken).
We adjusted prices for inflation by dividing prices by the Bureau of Labor Statistics’s consumer price index (CPI)25, which has an index base period of 1982–84 (CPI=100). This adjustment removed effects of national-level secular price changes from those unique to each food item.
We linked C2ER data to participants based on the quarter and year of their exams and their geocoded residence at the time of each exam. Each CARDIA one-year examination period covered four quarters. In addition to quarterly variability in local prices, variability in participant residence locations contributed to the distribution of food prices. We assigned price data to participants at the smallest geographic unit for which a match was available. At baseline, 24% of participants were assigned county-level price data, 49% Core-Based Statistical Area (CBSA)26-level data, and 27% population-weighted state-level data. We note that although participants were recruited from four metropolitan areas, there was appreciable C2ER variability within those areas.
Individual-level covariates
Participants provided demographic and socioeconomic information on standardized questionnaires. At baseline, participants reported their age, gender, and race, at all examinations participants reported their current educational attainment (years), and from year 5 onwards their family income (within categories).
Community-level covariates
We linked Census data to each participant at the tract level, based on participant residence at the time of the examination (using 1980 Census for year 0, 1990 for years 7 and 10, and 2000 for years 15 and 20). Tract-level data improved distinction of social differences that may influence dietary behaviors, as compared to county-level data, and were more statistically reliable than block group-level data. We derived an index of neighborhood socioeconomic deprivation from a principal components analysis of four indicators: 1) % of population less than 150% federal poverty level, 2) median family income, 3) % of population with <high school education, and 4) the % of population with ≥ college degree27.
We estimated population density within a 3-km Euclidian buffer around participant residence as a weighted average population count for block groups within the buffer, weighted by the proportion of total buffer area covered by each block group. The cost of living index was from the C2ER.
Statistical analysis
We used repeated measures negative binomial regression to model longitudinal associations between fast food price and weekly frequency of fast food consumption, and linear regression to model BMI and HOMA-IR. In secondary analysis, we quantified negative binomial associations between community-level fast food price and the individual-level frequency of eating at restaurants/cafeterias. Food price and outcome data were concurrently assessed at each exam year.
The negative binomial is a generalization of the Poisson model for count dependent variables. The negative binomial introduces heterogeneity into the model that allows the mean and variance of the outcome to differ, thereby loosening the equidispersion assumption of the Poisson model. Dispersion parameters were significant in our models, indicating that the negative binomial was appropriate. The estimation method was maximum likelihood using Stata –xtnbreg- (negative binomial) and –xtreg- (linear) commands. We tested for heterogeneity in the relationship between fast food price and outcomes over study periods by including an interaction term for time. We log-transformed (ln) HOMA-IR scores and BMI to improve normality of the data and reduce the influence of right-skewed observations.
As we considered price and all control variables exogenous, we used random effects to account for within-individual correlation of serial measures (called “random effects model”). The random effects specification allows for a two component error structure with time-invariant and time-varying individual specific errors. We adjusted for participant gender (male/female), race (black/white), baseline study center (4 cities), maximum reported income over follow-up (units of $10,000 from the midpoint of categorical responses) and maximum educational attainment (years) (both continuous); and time-varying age (6 categories: 18–24, 25–29, 30–34, 35–39, 40–44, 45–50 years), year of examination (5 categories: year 0, 7, 10, 15, 20), and geographic variables (all continuous, assigned to the individual), including neighborhood deprivation, cost of living index, and population density.
In a second modeling strategy, designed to account for possible correlation between the observed covariates such as price and time-invariant unobservables, we decomposed within- and between-person variability. For fast food price and all time-varying covariates, this model (“within-person”) included both a) the within-person average across all five waves as an estimate of between-person effects, and b) the difference from the average for each wave (i.e., the time-varying part) as an estimate of within-person effects28,29. We also adjusted for exam year and time-invariant covariates.
We tested for differences among sample subpopulations in their sensitivity to the price of fast food by including cross-product terms for fast food price and race, education, or income in the regression model. We ran separate interaction models for the following individual-level characteristics: race (2 levels: black/white), highest attained education (2 levels: <16, ≥16 years), and highest reported income (3 levels: <$40,000; $40–75,000; >$75,000), adjusting for the other two variables in the regression model (e.g., in the price*race interaction model, we adjusted for education and income).
We used the -margins- postestimation command in Stata to estimate multivariable-adjusted means and average marginal effects (slopes) of price on study outcomes. Where there was evidence for non-linear price effects, we estimated effects at decile cut-points along the fast food price distribution (10th through 90th percentiles). To insure that our estimates reflected the range of observed prices, we transformed fast food price to reflect a 2 standard deviation (SD) unit increase in price.
We excluded observations (each participant had up to 5 observations) from analysis if the participant was pregnant at the time of exam (n=120) or had missing data (n=1,446 fast food consumption, 10 fast food price, 12 neighborhood deprivation, 3 population density, 242 BMI, and 659 HOMA-IR). Two participants were missing data on gender and 407 never reported their income. Analytic datasets include 18,300 observations for fast food consumption (from 4,690 in year 0 to 2,642 in year 20); 19,580 for BMI; and 19,094 for HOMA-IR.
RESULTS
Over the 20-year follow-up, the prevalence and frequency of fast food consumption declined, as did the fast food price index; BMI and HOMA-IR increased (Table 1). Migration of the study sample and heterogeneity of food prices was such that 19% of the sample faced at least one between-survey price increase of at least $0.10 (1 SD of overall mean). The number of unique fast food prices varied by year, ranging from n=60 at year 0 [with mean(SD): 1.48(0.07)] to 483 at year 20 [mean(SD): 1.35(0.10)].
Table 1.
Individual- and community-level sample characteristics according to study year: CARDIA 1985/86–2005/06.
| Year 0 | Year 7 | Year 10 | Year 15 | Year 20 | p-valuea | |
|---|---|---|---|---|---|---|
| N | 4,696 | 3,938 | 3, 910 | 3,643 | 3,537 | |
| Individual-level variables | ||||||
| Percent: | ||||||
| White | 49.7 | 51.2 | 51.1 | 52.8 | 53.5 | 0.006 |
| Male | 45.2 | 45.5 | 44.7 | 44.4 | 43.3 | 0.35 |
| Fast food consumption, any | 90.2 | 81.1 | 82.0 | 87.4 | 80.1 | <0.001 |
| Educational attainment | ||||||
| ≤ 12 years | 38.6 | 29.6 | 29.6 | 23.0 | 24.2 | |
| 13–15 years | 33.3 | 30.7 | 28.4 | 31.2 | 27.2 | |
| ≥ 16 years | 28.1 | 49.7 | 42.1 | 45.8 | 48.6 | <0.001 |
| Mean (SD): b | ||||||
| Income, $10,000. c | - | 4.07 (2.7)A | 4.62 (2.9)A | 6.59 (3.9)A | 7.25 (4.1)A | <0.001 |
| Fast food consumption, times/week | 1.89 (2.3)10,15,20 | 1.88 (2.5)10,15,20 | 1.70 (2.1)0,7 | 1.76 (2.4)0,7 | 1.66 (2.5)0,7 | <0.001 |
| Among consumers | 2.18 (2.3)7 | 2.37 (2.6)A | 2.14 (2.1)7 | 2.09 (2.4)7 | 2.16 (2.5)7 | <0.001 |
| Body mass index (BMI, kg/m2) | 24.5 (5.0)A | 26.8 (6.2)A | 27.5 (6.5)A | 28.8 (6.8)A | 29.5 (7.2)A | <0.001 |
| HOMA-IR | 2.25 (2.0)A | 3.48 (5.7)0,10,20 | 3.29 (3.3)A | 3.54 (3.5)0,10,20 | 3.88 (3.8)A | <0.001 |
| Community-level variables | ||||||
| Mean (SD) | ||||||
| Real fast food price index, $ d | 1.52 (0.05)A | 1.40 (0.09)A | 1.32 (0.08)A | 1.35 (0.06)A | 1.37 (0.08)A | <0.001 |
| Real price 1/4 pound burger with cheese, $ | 1.23 (0.09)A | 1.30 (0.13)A | 1.21 (0.10)A | 1.27 (0.07)A | 1.32 (0.11)A | <0.001 |
| Real price 2 pieces fried chicken, $ | 1.66 (0.14)A | 1.42 (0.13)A | 1.38 (0.11)A | 1.43 (0.15)A | 1.45 (0.14)A | <0.001 |
| Real price 1/4 12-in cheese pizza, $ | 1.66 (0.10)A | 1.48 (0.15)A | 1.36 (0.12)A | 1.35 (0.08)A | 1.33 (0.11)A | <0.001 |
| Cost of living index, relative to standard of 1.0 | 1.05 (0.06)A | 1.12 (0.13)A | 1.14 (0.24)0,7,15 | 1.18 (0.29)A | 1.15 (0.22)0,7,15 | <0.001 |
| Population density (pop/sq km) e | 3446 (2176)A | 3095 (2438)A | 2301 (2208)0,7,20 | 2282 (2310)0,7,20 | 2073 (2226)A | <0.001 |
| Less than high school educational attainment (%)f | 30.3 (15.5)A | 22.2 (14.7)A | 20.7 (13.9)A | 16.7 (12.3)A | 16.1 (12.1)A | <0.001 |
| College degree (or higher attainment) (%)f | 21.7 (17.0)A | 27.3 (20.3)0,15,20 | 26.8 (18.4)0,15,20 | 32.1 (21.0)0,7,10 | 32.5 (20.7)0,7,10 | <0.001 |
| Less than 150% federal poverty level (%)f | 29.4 (17.2)A | 25.3 (18.0)A | 21.6 (17.2)A | 20.6 (15.9)A | 19.1 (15.5)A | <0.001 |
P-value tests of difference across study years were from: χ2 test for categorical variables and analysis of variance (ANOVA) for continuous variables.
Superscripted numbers indicate the exam years that differ significantly (p<0.05), based on pairwise comparisons of least-square means. If a year differed from all other years, we used a superscripted ‘A.’
Participants were not queried about their income at year 0.
Fast food prices were deflated to a 1982–1984 standard.
Population was per square kilometer of livable land area within a 3-km Euclidean (equal radius) buffer around participant residence.
Mean (SD) of Census tract data. Indicators reflect the percent of population within the tract.
For comparability with published literature, we quantified the price elasticity on consumption (where elasticity is the % change in outcome per 1% change price) at the combined-year mean fast food price ($1.39/serving). The multivariable-adjusted estimate from this analysis was −0.30 (95% CI: −0.56, −0.04) indicating a 0.30 percent decline in fast food consumption (times per week) for every 1% increase in fast food price.
Because fast food price was non-linearly associated with consumption (p for quadratic price term<0.001), we estimated effects at each decile cutpoint (10th through 90th percentiles) along the 20-year fast food price distribution. In age- and multivariable-adjusted models, mean fast food consumption was higher among blacks, as compared to whites, and was also generally higher among participants who lower educational attainment (<16 vs. ≥16 year) (Table 2).
Table 2.
Age- and multivariable-adjusteda subgroup-specific mean (95% CI) fast food consumption frequency (times/week) according to decile cutpointsb on the fast food price distribution.
| Decile cut-points of fast food price index | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| $1.25 | $1.30 | $1.32 | $1.36 | $1.38 | $1.40 | $1.47 | $1.49 | $1.53 | |
| Race | |||||||||
| Age-adjusted | |||||||||
| Black | 2.49 (2.34, 2.63) | 2.42 (2.30, 2.54) | 2.37 (2.26, 2.48) | 2.29 (2.19, 2.40) | 2.23 (2.13, 2.32) | 2.17 (2.07, 2.26) | 1.94 (1.85, 2.03) | 1.85 (1.76, 1.94) | 1.71 (1.62, 1.81) |
| White | 1.76 (1.65, 1.86) | 1.70 (1.61, 1.78) | 1.66 (1.58, 1.74) | 1.61 (1.54, 1.69) | 1.58 (1.50, 1.65) | 1.55 (1.48, 1.62) | 1.45 (1.38, 1.52) | 1.41 (1.34, 1.48) | 1.36 (1.28, 1.44) |
| Multivariable-adjusteda | |||||||||
| Black | 2.20 (2.07, 2.33) | 2.23 (2.12, 2.34) | 2.23 (2.13, 2.34) | 2.22 (2.12, 2.32) | 2.19 (2.10, 2.29) | 2.17 (2.07, 2.27) | 2.03 (1.94, 2.13) | 1.97 (1.87, 2.06) | 1.86 (1.75, 1.97) |
| White | 1.55 (1.45, 1.65) | 1.56 (1.48, 1.64) | 1.56 (1.49, 1.64) | 1.56 (1.49, 1.64) | 1.56 (1.49, 1.63) | 1.56 (1.48, 1.63) | 1.53 (1.46, 1.61) | 1.52 (1.45, 1.60) | 1.50 (1.41, 1.59) |
| Incomec | |||||||||
| Age-adjusted | |||||||||
| <$40,000. | 2.19 (2.00, 2.37) | 2.13 (1.98, 2.29) | 2.09 (1.94, 2.24) | 2.01 (1.87, 2.15) | 1.95 (1.81, 2.08) | 1.89 (1.76, 2.02) | 1.64 (1.53, 1.76) | 1.55 (1.43, 1.66) | 1.40 (1.28, 1.52) |
| $40–75,000. | 2.29 (2.14, 2.44) | 2.25 (2.12, 2.38) | 2.22 (2.10, 2.34) | 2.17 (2.05, 2.28) | 2.12 (2.01, 2.23) | 2.08 (1.97, 2.19) | 1.91 (1.81, 2.01) | 1.84 (1.73, 1.94) | 1.73 (1.62, 1.84) |
| >$75,000. | 1.95 (1.82, 2.08) | 1.88 (1.77, 1.98) | 1.83 (1.74, 1.93) | 1.78 (1.69, 1.87) | 1.74 (1.65, 1.82) | 1.70 (1.62, 1.79) | 1.59 (1.51, 1.67) | 1.55 (1.47, 1.63) | 1.49 (1.40, 1.58) |
| Multivariable-adjusted | |||||||||
| <$40,000. | 1.66 (1.52, 1.80) | 1.68 (1.56, 1.81) | 1.68 (1.56, 1.80) | 1.67 (1.55, 1.78) | 1.64 (1.53, 1.76) | 1.62 (1.50, 1.73) | 1.48 (1.38, 1.59) | 1.42 (1.32, 1.52) | 1.33 (1.21, 1.44) |
| $40–75,000. | 1.97 (1.84, 2.09) | 2.00 (1.90, 2.11) | 2.01 (1.91, 2.12) | 2.02 (1.91, 2.12) | 2.01 (1.91, 2.11) | 1.99 (1.90, 2.09) | 1.92 (1.82, 2.01) | 1.87 (1.77, 1.97) | 1.80 (1.69, 1.92) |
| >$75,000. | 1.92 (1.79, 2.04) | 1.92 (1.81, 2.02) | 1.91 (1.81, 2.01) | 1.90 (1.81, 2.00) | 1.89 (1.80, 1.99) | 1.89 (1.79, 1.98) | 1.84 (1.75, 1.93) | 1.82 (1.72, 1.92) | 1.79 (1.68, 1.90) |
| Educational attainmentd | |||||||||
| Age-adjusted | |||||||||
| <16 years | 2.35 (2.22, 2.49) | 2.31 (2.20, 2.42) | 2.28 (2.17, 2.38) | 2.22 (2.12, 2.32) | 2.17 (2.07, 2.26) | 2.12 (2.03, 2.21) | 1.92 (1.84, 2.01) | 1.84 (1.76, 1.93) | 1.72 (1.63, 1.82) |
| ≥16 years | 1.83 (1.71, 1.94) | 1.75 (1.66, 1.85) | 1.71 (1.63, 1.80) | 1.66 (1.58, 1.74) | 1.61 (1.54, 1.69) | 1.58 (1.51, 1.66) | 1.46 (1.39, 1.53) | 1.42 (1.35, 1.49) | 1.36 (1.28, 1.44) |
| Multivariable-adjusted | |||||||||
| <16 years | 2.05 (1.94, 2.17) | 2.10 (2.00, 2.20) | 2.11 (2.01, 2.20) | 2.11 (2.01, 2.20) | 2.09 (2.00, 2.18) | 2.08 (1.99, 2.17) | 1.97 (1.89, 2.06) | 1.92 (1.83, 2.01) | 1.83 (1.73, 1.94) |
| ≥16 years | 1.67 (1.56, 1.77) | 1.66 (1.57, 1.75) | 1.66 (1.57, 1.74) | 1.64 (1.57, 1.72) | 1.63 (1.56, 1.71) | 1.62 (1.55, 1.70) | 1.58 (1.50, 1.65) | 1.56 (1.48, 1.64) | 1.53 (1.43, 1.62) |
Age-adjusted models also include study year. Multivariable-adjusted models included: age, study center, exam year, sex, maximum educational attainment, highest reported income, population density, neighborhood deprivation score, and cost of living.
Real (deflated to 1982–84 prices) decile cutpoints for the 10th through 90th percentiles of fast food price were: $1.25, 1.30, 1.32, 1.36, 1.38, 1.40, 1.47, 1.49, 1.53. The number of observations within each decile: 1777, 1879, 1894, 1540, 1731, 1853, 1482, 1860, 2151, 2203.
Highest income reported over study.
Maximum educational attainment reported over study.
In general, results from random effects and within-person effects models did not differ substantively. Thus, we present estimates from the random effects models for ease of interpretability. Within- and between-person estimates are provided in supplemental material (eTables 2, 4, and 6). We note model differences in our presentation of results.
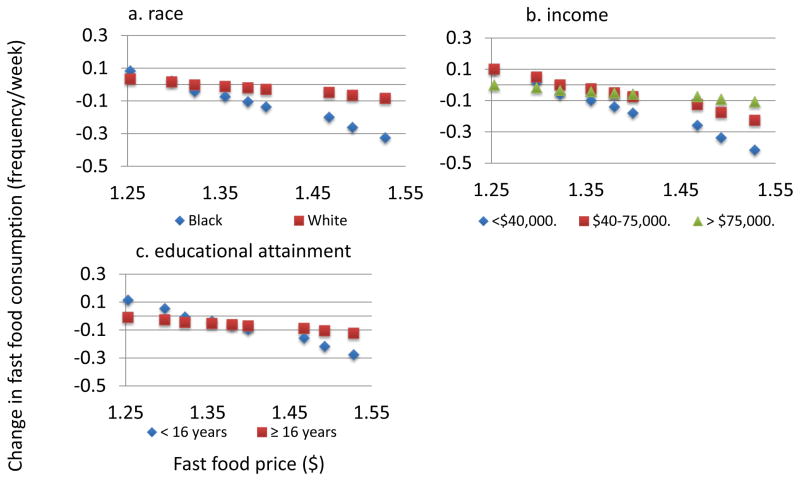
We estimated subgroup-specific changes (shown as average marginal effects) in fast food consumption for a 2 standard deviation (SD) increase in fast food price ($0.20) (Figure 1; eTable 1). Associations between fast food price and consumption varied by subgroup, with larger negative changes in consumption per unit change in price across decile cut-points of the fast food price distribution for blacks (vs. whites) (interaction term p-value =0.04) and for those with relatively less education (p =0.03). In the random effects (but not the within-person) model, participants with lower income were more sensitive to fast food price.
Figure 1.
Slopes1 (95% CI) for the estimated effect of fast food price2 (2 SD units3) on fast food consumption (frequency/week)4 according to sociodemographic subgroups: CARDIA 1985/86–2005/06.
1. Slopes (marginal effects) from repeated measures negative binomial regression models adjusted for: exam year, study center, age, race, sex, maximum educational attainment, highest reported income, population density, cost of living, and neighborhood deprivation. Random effects were used to account for within-person clustering over exam periods. Interaction term p-values: race=0.04, income=0.07, education=0.03. P-values for trend (by group): <0.01 (black), 0.42 (whites), <0.01 (income<$40,000), 0.04 (income $40–75,000), 0.09 (income>$75,000), 0.01 (<16 years education), and 0.50 (≥16 years education). 2.Fast food prices deflated to 1982–1984. Prices shown at decile cutpoints (10th to 90th percentiles: $1.25, 1.30, 1.32, 1.36, 1.38, 1.40, 1.47, 1.49, 1.53). 3.2 SD units = $0.20. 4.Fast food consumption mean (SD): 1.80 (2.34).
We also evaluated the association between fast food price and weekly frequency of eating in restaurants (eTable 3). Fast food price was inversely associated with restaurant visits among participants in the lowest income category.
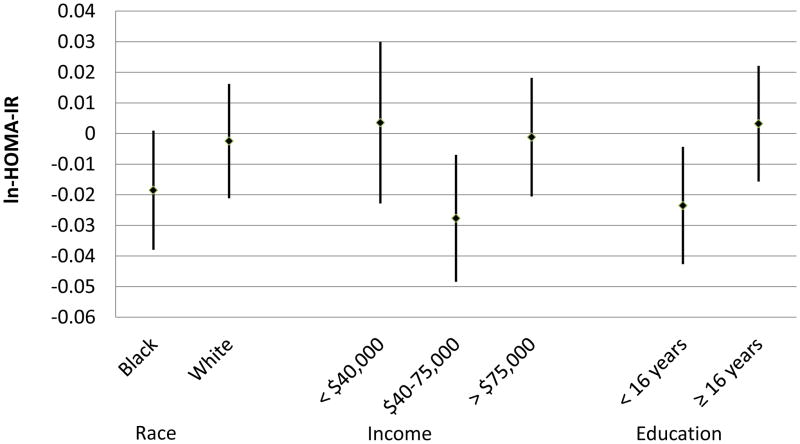
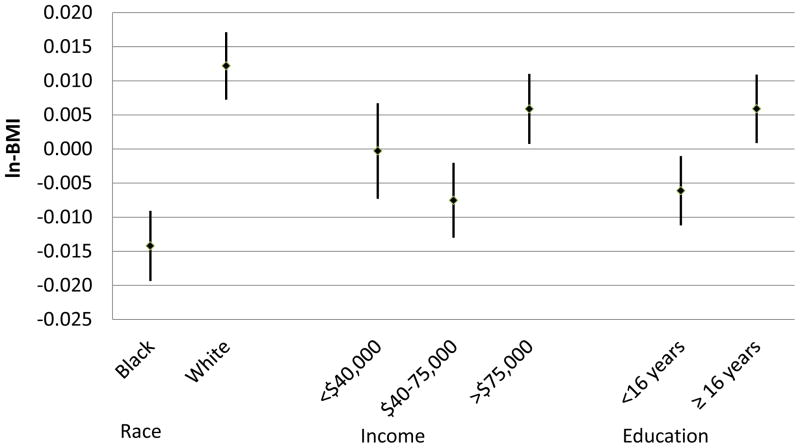
Fast food price was inversely associated with ln-HOMA-IR, with stronger estimated effects among those with lower income (p=0.02) and lower educational attainment (p=0.005) (Figure 2; eTable 5). Fast food price was also differentially associated with BMI among sociodemographic groups (Figure 3; eTable 5), with positive associations between fast food price and BMI among whites, as compared to blacks (p<0.001), and among participants with higher educational attainment, as compared to those with lower educational attainment (p<0.001). Fast food price was positively associated with BMI at the highest income level and inversely associated with BMI at the middle income level (p<0.001).
Figure 2.
Slopes1 (95% CI) for the estimated effect of fast food price2 (2 SD units3) on ln-HOMA-IR4 according to sociodemographic subgroups: CARDIA 1985/86–2005/06.
1. Slopes (marginal effects) from repeated measures linear regression models adjusted for: exam year, study center, age, race, sex, maximum educational attainment, highest reported income, population density, cost of living, and neighborhood deprivation. Random effects were used to account for within-person clustering over exam periods. Interaction term p-values: race=0.10, income=0.02, education<0.01. P-values for trend (by group): 0.06 (black), 0.86 (whites), 0.27 (income<$40,000), <0.01 (income $40–75,000), 0.95 (income>$75,000), 0.02 (<16 years education), and 0.69 (≥16 years education). 2.Fast food prices deflated to 1982–1984. Prices shown at decile cutpoints (10th to 90th percentiles: $1.25, 1.30, 1.32, 1.36, 1.38, 1.40, 1.47, 1.49, 1.53). 3.2 SD units = $0.20. 4. Ln-HOMA-IR mean (SD): 1.31 (0.47).
Figure 3.
Slopes1 (95% CI) for the estimated effect of fast food price2 (2 SD units3) on ln-BMI4 according to sociodemographic subgroups: CARDIA 1985/86–2005/06.
1.Slopes (marginal effects) from repeated measures linear regression models adjusted for: exam year, study center, age, race, sex, maximum educational attainment, highest reported income, population density, cost of living, and neighborhood deprivation. Random effects were used to account for within-person clustering over exam periods. Interaction term p-values: race<0.01, income<0.01, education<0.01. P-values for trend (by group): <0.01 (blacks), <0.01 (whites), 0.98 (income<$40,000), <0.01 (income $40–75,000), 0.02 (income>$75,000), 0.05 (<16 years education), and 0.08 (≥16 years education). 2.Fast food prices deflated to 1982–1984. Prices shown at decile cutpoints (10th to 90th percentiles: $1.25, 1.30, 1.32, 1.36, 1.38, 1.40, 1.47, 1.49, 1.53). 3.2 SD units = $0.20. 4. Ln-BMI mean (SD): 3.27 (0.22).
Our findings did not materially change when we restricted the analysis to participants with county- or CBSA-level food price data. We did not find statistical evidence of 3-way interactions among fast food price and joint sociodemographic combinations (such as race and income). The global F test for time-by-price-by-race (or income, education) variables was not statistically significant.
DISCUSSION
Over 20 years of follow-up in the CARDIA cohort, fast food price was inversely associated with fast food consumption, with greater price sensitivity among blacks, as compared to whites, and among those with relatively lower educational attainment. We observed stronger inverse associations between fast food price and insulin resistance among those with lower educational attainment and among those at the middle income level. Fast food price was inversely associated with BMI in blacks and among those with lower educational attainment or at the middle income level, but was positively associated with BMI among whites and among participants with higher educational attainment or at the highest income level. These findings have implications for fiscal policy considerations, particularly as they relate to sociodemographic disparities in fast food consumption and subsequent health outcomes. These findings are particularly important as blacks and lower SES populations consume greater proportions of their energy from fast food than do other race-ethnic and SES groups30.
In prior CARDIA analysis, Duffey et al. documented significant inverse associations between soda and pizza prices and diet-related outcomes, including total energy consumption, BMI, and insulin resistance17, but did not study sociodemographic differences in price sensitivity. Understanding differential price sensitivity is essential to anticipating the impact of fiscal policies on population subgroups. According to economic theory, population subgroups with less disposable income would be expected to be more sensitive to price9,10. Recent econometric research supports this expectation11,12. A global ecologic meta-analysis of country-level food prices and consumption documented greater sensitivity among lower income countries and households11. Similarly, findings from New Zealand indicate that food pricing policies would have greater impact on the diets of low income and racial minority (Maori) groups, with the potential to decrease health disparities in these groups12. However, documentation of differential price effects on food consumption and biologic outcomes has been a gap in the epidemiologic literature noted by several researchers5,31–33 that we address in this analysis.
Corroborating our findings, in a study of C2ER food prices and fast food consumption over 5-years of follow-up in the National Longitudinal Study of Adolescent Health, Gordon-Larsen and colleagues found that blacks were more sensitive to the price of soda, while whites were more sensitive to the price of burgers3. In contrast, a 4-year study of children found that fast food consumption among whites, but not blacks, was sensitive to the price of fast food34. Study results also vary with respect to the influence of income on the effect of food price on dietary behavior, with some showing stronger inverse associations among low-income participants6,8,35, while others show no difference across income categories34,36,37. Similar to some of our findings, which showed a strongest price effects among those in the middle income group, Finkelstein et al. found that those in a middle (rather than lowest) income group, were most sensitivity to the price of sugar-sweetened beverages38.
The positive associations between fast food price and BMI among whites and those with higher educational attainment and income were unexpected. These findings may reflect chance, though such unanticipated findings are not uncommon in the food price literature. For example, in an experimental study, subsidies on fruits and vegetables led to increased caloric consumption, from both fruits and vegetables and less healthy options39. Similarly, simulation studies, using published estimates of elasticities and other inputs, have found that taxes on food away from home40 or saturated fats41 may adversely affect dietary behaviors and weight-related outcomes. These studies point to complicated food behavior dynamics, and underscore the importance of increased specificity in evaluations of proposed fiscal policies.
It is possible that differential substitution patterns help explain our BMI findings, which could be considered a type of confounding bias. For example, if those with greater financial resources substitute other high-energy-dense foods for fast food meals. In our data, increases in fast food price were associated with decreases in visits to both fast food and non-fast food establishments among blacks and those with lower educational attainment, which may yield overall greater improvements in insulin resistance within those population subgroups. We lack price data for eating at non-fast food restaurants and thus could not further evaluate these pricing dynamics. Accounting for cross-price elasticities (the impact of a specific food price on the consumption of other foods) is a pervasive challenge in food price-demand studies42. Limitations of our data did not allow us to better delineate price-consumption dynamics.
Several other limitations of our study merit discussion. The C2ER provide the lowest-level geographic price data available, but even with the variability captured in our study (range of 60 unique price data points at year 0 to 483 at year 20), it is possible that price estimates may miss important regional variability. Price data may be measured with error or the C2ER, which attempts to reflect consumption patterns of a professional household, may not represent purchases of the CARDIA sample. Furthermore, our models assume a temporal relation whereby price influences consumption, but prices may themselves be confounded by demand or other individual- or community-level characteristics, though we controlled for many participant and contextual variables, including family and employment status, and the neighborhood deprivation and regional cost of living index.
The CARDIA diet history asked about frequency of fast food consumption, but did not assess what people ate at fast food establishments, and the C2ER price data may not align well with participants’ consumption of specific foods. We were also limited in our ability to control for residential selectivity. We adjusted for baseline study center and for several neighborhood attributes of each participant’s current residence, but, to the extent that people’s choices about where to live correlate differentially with both fast food price and consumption, residual bias may exist. Another limitation, not limited to our study, was the lack of variability in fast food prices over the study period, which hindered our ability to estimate outcome changes across a broad range of fast food prices.
Despite these limitations, our study also has significant strengths. As compared to previous studies, CARDIA has substantial power for detecting subgroup associations, due to the large sample size, the racial and socioeconomic diversity of the sample, and temporal variability in food prices over 20 years of follow-up. The longitudinal and observational nature of our study is important in the field of food price studies, many of which have been either cross-sectional or small experimental studies. Furthermore, CARDIA followed people through important life cycle stages, and provided temporal and geographic variability in food price and dietary habits. The lack of effects observed in some cross-sectional studies may reflect limited price variability. In contrast, experimental studies have been able to show effects by differentiating on price30, but may lack external variability and it is often unclear whether interventions will play out as expected in observed populations.
The success of fiscal food policies requires understanding of how different populations will respond to changes in food prices, and whether policies will have the desired impact on those in most need. While many low income and minority populations fight price increases because they note they unduly affect the poor, it is equally important for us to remember that these reduced unhealthy behaviors can ameliorate health disparities and call out for strong support for the inclusion of subgroup-specific elasticity estimates in model-based evaluations of policy approaches, as proposed by others36. The major results of this study, the impact of higher fast food prices in reducing consumption of fast food and risk of diabetes among blacks and lower SES subpopulations, speak to this issue directly. Counter-intuitive findings in this study and others lead us to need additional studies on these and related potentially unhealthy eating behaviors so comprehensive food pricing policies will best achieve desired outcomes.
Supplementary Material
Acknowledgments
The authors would like to acknowledge CARDIA Chief Reviewer Janne Boone-Heinonen, PhD, whose thoughtful suggestions improved the paper. This work was funded by NHLBI grant R01 HL104580 and R24 HD050924. The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute (NHLBI), the Intramural Research Program of the National Institute on Aging (NIA), and an intra-agency agreement between NIA and NHLBI (AG0005).
Footnotes
The authors have no disclosures to report.
The authors have no financial or other conflicts of interest to disclose.
KAM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis.
Authors’ contributions:
KAM: conceptualized the study, statistical analysis, wrote the manuscript. KJD: conceptualized the study, statistical analysis, manuscript review. DKG: secured funding, conceptualized the study, oversaw the statistical analysis, manuscript review. BMP: secured funding, conceptualized the study, manuscript review. SWN: statistical analysis and manuscript review. CIK: secured funding, analysis and manuscript review. LMS: chairs CARDIA diet committee, manuscript review. JMS: CARDIA data coordination and management, manuscript review. PGL secured funding, conceptualized the study, oversaw the statistical analysis, wrote and reviewed the manuscript.
References
- 1.Brownell KD, Farley T, Willett WC, et al. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med. 2009;361:1599–1605. doi: 10.1056/NEJMhpr0905723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Popkin B. The World is Fat--the Fads, Trends, Policies, and Products that are Fattening the Human Race. New York: Avery-Penguin Group; 2008. [Google Scholar]
- 3.Gordon-Larsen P, Guilkey DK, Popkin BM. An economic analysis of community-level fast food prices and individual-level fast food intake: a longitudinal study. Health Place. 2011;17:1235–1241. doi: 10.1016/j.healthplace.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duffey KJ, Gordon-Larsen P, Shikany JM, Guilkey D, Jacobs DR, Jr, Popkin BM. Food price and diet and health outcomes: 20 years of the CARDIA Study. Arch Intern Med. 2010;170:420–426. doi: 10.1001/archinternmed.2009.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andreyeva T, Long MW, Brownell KD. The impact of food prices on consumption: a systematic review of research on the price elasticity of demand for food. Am J Public Health. 2010;100:216–222. doi: 10.2105/AJPH.2008.151415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powell LM, Zhao Z, Wang Y. Food prices and fruit and vegetable consumption among young American adults. Health Place. 2009;15:1064–1070. doi: 10.1016/j.healthplace.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Powell LM, Han E. The costs of food at home and away from home and consumption patterns among U.S. adolescents. J Adolesc Health. 2011;48:20–26. doi: 10.1016/j.jadohealth.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Powell LM. Fast food costs and adolescent body mass index: evidence from panel data. J Health Econ. 2009;28:963–970. doi: 10.1016/j.jhealeco.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Timmer CP, Falcon WP, Pearson SR. Food policy analysis. Baltimore: The Johns Hopkins University Press for the World Bank; 1984. [Google Scholar]
- 10.Timmer CP, Alderman H. Estimating Consumption Parameters for Food Policy Analysis. American Journal of Agricultural Economics. 1979;61:982–987. [Google Scholar]
- 11.Green R, Cornelsen L, Dangour AD, Turner R, Shankar B, Mazzocchi M, Smith RD. The effect of rising food prices on food consumption: systematic review with meta-regression. BMJ. 2013;346:f3703. doi: 10.1136/bmj.f3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ni Mhurchu C, Eyles H, Schilling C, Yang Q, Kaye-Blake W, Genc M, Blakely T. Food prices and consumer demand: Differences across income levels and ethnic groups. PLoS ONE. 2013;8:e75934. doi: 10.1371/journal.pone.0075934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blakely T, Ni Mhurchu C, Jiang Y, et al. Do effects of price discounts and nutrition education on food purchases vary by ethnicity, income and education? Results from a randomised, controlled trial. J Epidemiol Community Health. 2011;65:902–908. doi: 10.1136/jech.2010.118588. [DOI] [PubMed] [Google Scholar]
- 14.Epstein LH, Handley EA, Dearing KK, et al. Purchases of food in youth. Influence of price and income. Psychol Sci. 2006;17:82–89. doi: 10.1111/j.1467-9280.2005.01668.x. [DOI] [PubMed] [Google Scholar]
- 15.Prentice AM, Jebb SA. Fast foods, energy density and obesity: a possible mechanistic link. Obes Rev. 2003;4:187–194. doi: 10.1046/j.1467-789x.2003.00117.x. [DOI] [PubMed] [Google Scholar]
- 16.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365:36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 17.Duffey KJ, Gordon-Larsen P, Jacobs DR, Jr, Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. Am J Clin Nutr. 2007;85:201–208. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- 18.Bauer KW, Hearst MO, Earnest AA, French SA, Oakes JM, Harnack LJ. Energy content of U.S. fast-food restaurant offerings: 14-year trends. Am J Prev Med. 2012;43:490–497. doi: 10.1016/j.amepre.2012.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Currie J, DellaVigna S, Moretti E, Pathania V. The effect of fast food restaurants on obesity and weight gain. w14721. National Bureau of Economic Research; 2009. [Google Scholar]
- 20.Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health. 2012;102:1644–1654. doi: 10.2105/AJPH.2012.300865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Medina J. South Los Angeles, New Fast-Food Spots Get a ‘No, Thanks’. The New York Times. 2011 Jan 15; [Google Scholar]
- 22.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 23.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 24.The Council for Community and Economic Research (C2ER) [accessed 2 June 2013];Cost of Living Index. www.coli.org.
- 25.Bureau of Labor Statistics, United States Department of Labor. [accessed 2 June 2013];Consumer Price Index. http://www.bls.gov/cpi.
- 26.Office of Management and Budget. [accessed 8 July 2013];Federal Register: 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas. http://www.whitehouse.gov/sites/default/files/omb/assets/fedreg_2010/06282010_metro_standards-Complete.pdf.
- 27.Boone-Heinonen J, Diez Roux AV, Kiefe CI, Lewis CE, Guilkey DK, Gordon-Larsen P. Neighborhood socioeconomic status predictors of physical activity through young to middle adulthood: the CARDIA study. Soc Sci Med. 2011;72:641–649. doi: 10.1016/j.socscimed.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allison PD. Fixed Effects Regression Methods for Longitudinal Data Using SAS. Cary, NC: SAS Institute Inc; 2005. [Google Scholar]
- 29.Neuhaus JM, Kalbfleisch JD. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics. 1998;54:638–645. [PubMed] [Google Scholar]
- 30.Ng SW, Slinging Meghan, Popkin Barry M. A turning point for US diets? Recessionary effects or behavioral shifts in foods purchased and consumed. University of North Carolina; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Powell LM, Chriqui JF, Khan T, Wada R, Chaloupka FJ. Assessing the potential effectiveness of food and beverage taxes and subsidies for improving public health: a systematic review of prices, demand and body weight outcomes. Obesity Reviews. 2013;14:110–128. doi: 10.1111/obr.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Epstein LH, Jankowiak N, Nederkoorn C, Raynor HA, French SA, Finkelstein E. Experimental research on the relation between food price changes and food-purchasing patterns: a targeted review. Am J Clin Nutr. 2012;95:789–809. doi: 10.3945/ajcn.111.024380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 34.Khan T, Powell LM, Wada R. Fast food consumption and food prices: evidence from panel data on 5th and 8th grade children. J Obes. 2012;2012:857697. doi: 10.1155/2012/857697. Epub 2012 Jan 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Raper KC, Wanzala MN, Nayga R. Food expenditures and household demographic composition in the US: a demand systems approach. Applied Economics. 2002;34:981–992. [Google Scholar]
- 36.Beydoun MA, Powell LM, Chen X, Wang Y. Food prices are associated with dietary quality, fast food consumption, and body mass index among U.S. children and adolescents. J Nutr. 2011;141:304–311. doi: 10.3945/jn.110.132613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beydoun MA, Powell LM, Wang Y. The association of fast food, fruit and vegetable prices with dietary intakes among US adults: is there modification by family income? Soc Sci Med. 2008;66:2218–2229. doi: 10.1016/j.socscimed.2008.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Finkelstein EA, Zhen C, Nonnemaker J, Todd JE. Impact of targeted beverage taxes on higher- and lower-income households. Arch Intern Med. 2010;170:2028–2034. doi: 10.1001/archinternmed.2010.449. [DOI] [PubMed] [Google Scholar]
- 39.Epstein LH, Dearing KK, Roba LG, Finkelstein E. The influence of taxes and subsidies on energy purchased in an experimental purchasing study. Psychol Sci. 2010;21:406–414. doi: 10.1177/0956797610361446. [DOI] [PubMed] [Google Scholar]
- 40.Schroeter C, Lusk J, Tyner W. Determining the impact of food price and income changes on body weight. Journal of Health Economics. 2008;27:45–68. doi: 10.1016/j.jhealeco.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 41.Nnoaham KE, Sacks G, Rayner M, Mytton O, Gray A. Modelling income group differences in the health and economic impacts of targeted food taxes and subsidies. Int J Epidemiol. 2009;38:1324–1333. doi: 10.1093/ije/dyp214. [DOI] [PubMed] [Google Scholar]
- 42.Nghiem N, Wilson N, Genc M, Blakely T. Understanding price elasticities to inform public health research and intervention studies: Key issues. Am J Public Health. 2013;103:1954–1961. doi: 10.2105/AJPH.2013.301337. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.