Abstract
Background:
Professional burnout has been widely explored in health care. We conducted this study in our hospital intensive care unit (ICU) in United States to explore the burnout among nurses and respiratory therapists (RT).
Materials and Methods:
A survey consisting of two parts was used to assess burnout. Part 1 addressed the demographic information and work hours. Part 2 addressed the Maslach Burnout Inventory-Human Service Survey.
Results:
The analysis included 213 total subjects; Nurses 151 (71%) and RT 62 (29%). On the emotional exhaustion (EE) scale, 54% scored “Moderate” to “High” and 40% scored “Moderate” to “High” on the depersonalization (DP) scale. Notably 40.6% scored “Low” on personal accomplishment (PA) scale.
Conclusion:
High level of EE, DP and lower PAs were seen among two groups of health care providers in the ICUs.
Keywords: Burnout nurses, intensive care unit nurses, sleepy nurses, sleepy therapist
Introduction
Professional burnout is a psychological construct widely explored in the healthcare literature. No standard definition exists for burnout yet researchers refer to burnout as “a syndrome of emotional exhaustion (EE), depersonalization (DP) and reduced personal accomplishments (PAs) that occur among individuals who work with people”.[1,2] The consequences associated with professional burnout affect both the health care professionals and recipients. Increased professional burnout is associated with absenteeism, physical illness, emotional problems, poor job performance and negative attitudes for the health care professionals in general.[3] Health care recipients can experience a decrease in quality of care provided and poor communication from healthcare providers as a result of the healthcare professional's burnout.
Variations in the prevalence and severity of professional burnout have been reported across specialties by both doctors and nurses. Doctors and nurses who work in intensive care units (ICU) are thought to have higher levels of burnout because of their stressful work demands associated with caring for critically ill patients.[4] Guntupalli and Fromm,[5] first studied burnout among ICU physicians who were members of the section of Internal Medicine of the Society of Critical Care Medicine. The authors indicated that ICU physicians experience high levels of EE, DP and decreased personal achievement. They found 29% of respondents scored high in EE, 20.4% scored high in DP and with 59% had low personal achievement scores on the Maslach Burnout Inventory-Human Service Survey (MBI-HSS). Similar findings are reported among French ICU physicians.[2] Gender status, workload and conflict with other employees appear to be significant factors that increase their level of professional burnout. Professionals who have dedicated personality, over-committed personality and authoritarian personality are more susceptible to the effects of burnout.[6] Common causes leading to burnout are overwhelming and hard work with no clear goals, being powerless to change something important and forcing oneself to make the impossible happen. Some of the early warning signs of burnout syndrome is shown in Graph 1.
Graph 1.

Early warning signs for burnout syndrome
Nurses are also influenced by professional burnout but appear to be impacted by different factors. Nurses, who are younger in age, separated or divorced, do not receive days off as requested, experience conflict with patients and co-workers, make the end of life decisions regarding patient care and work full time in ICUs are more prone to severe burnout.[7,8] Nursing burnout has been documented in the literature for critical care, oncology, palliative care, emergency care and other areas.[9,10] In a French study evaluating 2497 nurses working in 165 different ICUs found four groups of nurses to have high burnout syndrome; younger age, participation in ICU work groups, quality of working relationships and end of life related factors.[7]
The determinants and predictors of professional burnout in an ICU setting vary according to professions. Based on earlier studies, it is erroneous to assume that similar factors perpetuate professional burnout in ICU staff. The literature currently places little attention on the prevalence of burnout for respiratory therapists (RT) working in ICU.
Burnout is a term used for a long-term exhaustion with diminished interest usually in the work context. It is used as a slang term to mean exhaustion. Burnout is much more than stress alone. People do experience high stress at work but are not at risk for burnout. Certain professions such as entrepreneurs, teachers and athletes in addition to healthcare professionals are susceptible to work-related burnout. Quiet often these people are highly motivated, committed and accomplished individuals. Burnout syndrome is reported to have three components (1) EE (2) DP and (3) low PA. Some of the early warning signs of burnout syndrome is shown in Graph 1.
The focus of this study was healthcare professionals, specifically Registered Nurses (RN) and RT, involved in the care of ICU patients. The professional staff in the ICU setting are often required to spend considerable periods of intense involvement with other people. RN and RT are frequently involved with patients and families having serious physical, psychological and social problems creating interactions charged with feelings of anxiety, fear, embarrassment, anger and despair. Solutions to most of the problems are not always obvious, straight forward or easily obtained, thus adding to ambiguity and frustrations of the situation. For the helping professionals who work continually under such circumstances, this chronic stress can be emotionally draining and pose the risk of “burnout”. The consequences of burnout are potentially serious to staff, clients and institutions where they interact. Initial research on this syndrome suggests that it can lead to deterioration in the quality of care or services provided by the staff. It is believed to be a factor in job turn over, absenteeism and low morale.
The most well studied measurement of burn out is the MBI-HSS.[11] Maslach and Jackson first identified the construct “burnout” in the 1970's and developed a measure that weighs the effects of EE, DP and reduced sense of personal achievement. This inventory has become the standard tool for measuring burnout in research performed on the syndrome.
Few studies have been done on health care professionals involved in the care of ICU patients. This study was conducted in the United States to explore burnout among nurses and RT in ICU.
Site
This study was conducted in the ICUs of the Harris County Hospital District Houston, a safety net hospital for the 700,000 indigent populations residing in Harris and neighboring counties of Texas. The survey was conducted at Ben Taub General Hospital containing 120 ICU beds and LBJ Hospital using 16 ICU beds.
Approval
Study approval was obtained from the Baylor College of Medicine Institutional Review Board and the Harris County Hospital District.
Study
The survey consisted of a two-part handout placed in an envelope and given to the ICU RNs and RTs. Part 1 addressed demographic information including gender, age, credentials, race, years in practice, employment status, work schedule, hours worked/week and departmental position.
Part 2 of the handout was the MBI-HSS; an inventory consisting of 22 questions to assess three components of burnout, EE, DP and lack of personal achievement. These 22 questions were divided into three subscales to measure the three components separately. These items were written in the form of statement about personal feelings and attitudes and answered on a 7-point scale from 0 as never to 6 as every day.
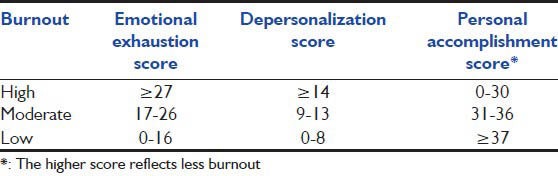
The 9-item EE subscale assesses feelings resulting from depletion of emotional resources. The 5-item DP subscale assesses personal and caring attitudes and the 8-item PA subscale assesses feelings of competence and successful achievement when working with people. For EE and DP subscales, a higher mean score corresponded to a higher degree of burnout. The higher mean scores on the EE and DP subscales and a lower mean score on the PA subscale are consistent with burnout [Table 1].
Table 1.
Burnout scores classification
Statistical analysis
Statistical analysis was performed using Microsoft Excel® and SPSS (IBM; Armonk, New York) statistical package.
Results
Univariate frequencies were performed [Table 2] and included 213 total subjects 151 (71%) RNs and 62 (29%) RTs. Age was evenly distributed, with 20-30 years being the smallest category with 32 (15%) respondents. Years of work in critical care was also distributed as expected with a decline between 21 and 25 years; nearly 25% of the sample had been working in critical care <5 years and 21% >21 years. 38 respondents (18%) reported managerial or charge duties and approximately half of the sample reported working overtime in the past month.
Table 2.
Demographic data and univariate frequencies of the subjects

Results of the EE subscale revealed 54% scored “Moderate” or “High” and 40% scored “Moderate” or “High” on the DP subscale. Notably, 40.6% scored “Low” on the PA subscale [Table 3]. Odds ratios were performed on RNs and RTs for other variables [Table 3]. No difference was found between gender, managerial or non-managerial position, years of experience, overtime worked and rotating shifts. Scatter plots of the raw data showed worsening trends for EE, DP and PA [Figures 1–3] in the subject group.
Table 3.
Frequencies of scores for emotional exhaustion, depersonalization and personal achievement
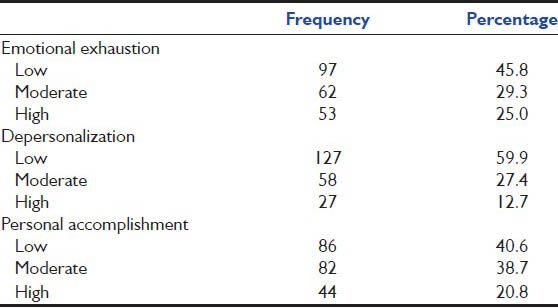
Figure 1.

Emotional exhaustion correlated with depersonalization
Figure 3.

Depersonalization correlated to personal achievement
Figure 2.

Emotional exhaustion correlated to personal achievement
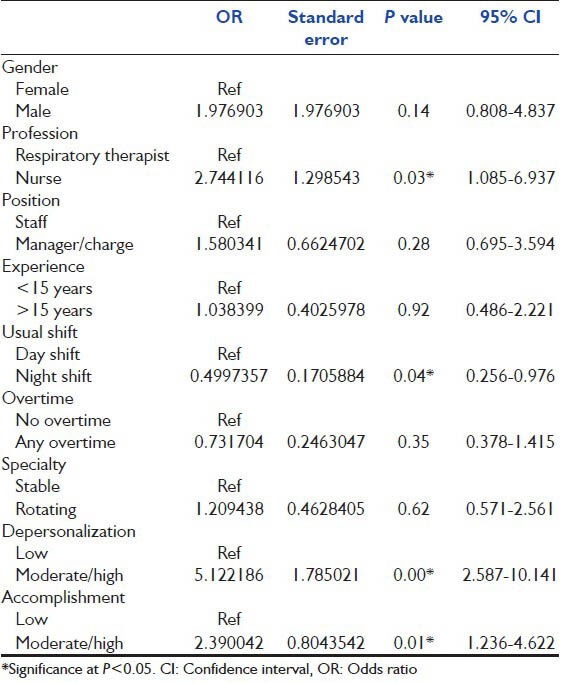
Linear regression revealed surprising trends in the univariate analysis model expecting the night shift to have higher EE and DP scores with lower PA scores when compared to the day shift which was not supported in this study. In the final model, moderate and high categories for EE, DP and accomplishment were collapsed due to the presence of small cells (N < 8) among some variables. Once stratified, overall goodness of fit was achieved [Table 4]. The model was tested for “years of experience” and “age” separately since these variables was not identified as independent for all study participants. These variables were also tested as originally stratified and then collapsed yielding no significance. In the analysis of night shift and day shift, night shift nurses had less degree of burnout when compared with the day shift nurses and regression analysis showed the night shift to have a protective effect although with a wide confidence interval (CI) (P < 0.05; CI: 0.256-0.976). Managerial and non-managerial positions had no significant effect on EE (P = 0.28; CI: 0.695-3.594). Moderate or high DP (P ≤ 0.05; CI: 2.587-10.14) and PA scores (P ≤ 0.5; CI: 1.236-4.622) had a significant effect on moderate or high EE scores RNs had also higher burnout rate when compared with RTs (P < 0.05; CI: 1.085-6.937).
Table 4.
Comparison of experience, profession and other variable among nurses and respiratory therapist
Discussion
In this study, 54% of the staff suffered from moderate to severe EE, 41% suffered from moderate to severe DP and 40% had low personal achievements. Study results showed gender, managerial position and years of experience, had no effect on burnout and no difference was identified based on shift; consistent with the Ilhan et al. study[12] Surprisingly, no difference in burnout was found between staff with or without overtime hours. RNs had higher overall burnout when compared to RTs with DP being higher among the RNs. Night shift may have some protective effect possibly attributed to survival of the initial phase of burnout. Those unable to tolerate night shift have likely changed shifts or possibly even changed professions.
ICU staff (RN/RT) results differed from previous studies on surgical residents, radiologists and Chinese nurses. This study's ICU staff had higher EE scores, lower DP scores yet similar PA scores when compared to surgical residents[13] and a burnout rate when compared to radiologist and Chinese nurses.[14,15] Gender, managerial position and years of experience, had no effect on burnout and no difference in burn out on the basis of shift rotation consistent with the study by Ilhan et al.[12] Surprisingly, no difference in burnout was identified between the staff working over-time and those with no over-time hours. Nursing staff were shown to have higher burnout syndrome and more specifically DP when compared to RT. In the comparison by shift rotation, night shift appeared to have had some protective effect. It may be possible that nurses or therapists working the night shift have already survived the initial phase of burnout and those who were not able to tolerate the night shift have moved to the day shift or changed professions.
This study identified important components of burnout among ICU staff by using the MBI-HSS The limitations of this study was the exclusion of confounding variables such as the nursing shortage, increased patient complexity, pressure to comply with increasing regulations and higher consumer demands. The lower rate of burnout among RT may be explained by their well-defined scope of practice and area of patient care allowing less involvement with a minute-to-minute decisions.
Limitations
This study has several limitations. It was conducted in a single institution and did not account for nurses and therapist who may have dropped out or changed the shifts, or profession.
Conclusion
The syndrome identified as burnout is seen in across healthcare professionals including residents, physicians, surgeons, nurses and RT. Increased demand on healthcare workers due to the shortage of providers, limited resources and increasing consumer load can lead to burnout of these providers and attrition. Further multi-center prospective studies are warranted to assess the effect of burnout on attrition further contributing to the workforce shortage.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Maslach C JS, Leiter MP, editors. Consulting Psychologists Press; 1996. Maslach Burnout Inventory Manual. [Google Scholar]
- 2.Embriaco N, Azoulay E, Barrau K, Kentish N, Pochard F, Loundou A, Papazian L. High level of burnout in intensivists: Prevalence and associated factors. Am J Respir Crit Care Med. 2007;175:686–92. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- 3.Schaufeli W LM, Maslach C. Burnout: Thirty-five years of research and practice. Career Dev Int. 2009;14:204–20. [Google Scholar]
- 4.Bakker AB, Le Blanc PM, Schaufeli WB. Burnout contagion among intensive care nurses. J Adv Nurs. 2005;51:276–87. doi: 10.1111/j.1365-2648.2005.03494.x. [DOI] [PubMed] [Google Scholar]
- 5.Guntupalli KK, Fromm RE., Jr Burnout in the internist-intensivist. Intensive Care Med. 1996;22:625–30. doi: 10.1007/BF01709737. [DOI] [PubMed] [Google Scholar]
- 6.Gillespie M, Melby V. Burnout among nursing staff in accident and emergency and acute medicine: A comparative study. J Clin Nurs. 2003;12:842–51. doi: 10.1046/j.1365-2702.2003.00802.x. [DOI] [PubMed] [Google Scholar]
- 7.Poncet MC, Toullic P, Papazian L, Kentish-Barnes N, Timsit JF, Pochard F, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175:698–704. doi: 10.1164/rccm.200606-806OC. [DOI] [PubMed] [Google Scholar]
- 8.Chen SM, McMurray A. “Burnout” in intensive care nurses. J Nurs Res. 2001;9:152–64. doi: 10.1097/01.jnr.0000347573.45553.e0. [DOI] [PubMed] [Google Scholar]
- 9.Kilfedder CJ, Power KG, Wells TJ. Burnout in psychiatric nursing. J Adv Nurs. 2001;34:383–96. doi: 10.1046/j.1365-2648.2001.01769.x. [DOI] [PubMed] [Google Scholar]
- 10.Escribà-Agüir V, Martín-Baena D, Pérez-Hoyos S. Psychosocial work environment and burnout among emergency medical and nursing staff. Int Arch Occup Environ Health. 2006;80:127–33. doi: 10.1007/s00420-006-0110-y. [DOI] [PubMed] [Google Scholar]
- 11.Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav. 1981;2:99–113. [Google Scholar]
- 12.Ilhan MN, Durukan E, Taner E, Maral I, Bumin MA. Burnout and its correlates among nursing staff: Questionnaire survey. J Adv Nurs. 2008;61:100–6. doi: 10.1111/j.1365-2648.2007.04476.x. [DOI] [PubMed] [Google Scholar]
- 13.Businger A, Stefenelli U, Guller U. Prevalence of burnout among surgical residents and surgeons in Switzerland. Arch Surg. 2010;145:1013–6. doi: 10.1001/archsurg.2010.188. [DOI] [PubMed] [Google Scholar]
- 14.Czekajska-Chehab E, Okła W, Drop A, Skrzypek M. The professional burnout syndrome in radiologists. Ann Univ Mariae Curie Sklodowska Med. 2003;58:254–60. [PubMed] [Google Scholar]
- 15.Lei W, Youn Hee K, Dong W. A review of research and strategies for burnout among Chinese nurses. Br J Nurs. 2010;19:844–50. doi: 10.12968/bjon.2010.19.13.48862. [DOI] [PubMed] [Google Scholar]


