Summary
The demographic and clinical characteristics of adults and children with lower extremity deep-vein thrombosis and/or pulmonary embolism (LE DVT/PE) may differ from those with abdominal vein thrombosis (abdominal VT). Abdominal VT can be a presenting sign of an underlying prothrombotic state, and its presence in the setting of known disease might have prognostic implications different from LE DVT/PE. This study describes clinical presentations of abdominal VT compared to LE DVT/PE in adults and children. We analysed prospectively-collected data from consecutive consenting patients enrolled in one of seven Centers for Disease Control and Prevention (CDC) funded Thrombosis and Hemostasis Network Centers from August 2003 to April 2011 to compare the demographic and clinical characteristics of adults and children with abdominal VT. Both adults and children with abdominal VT tended to be younger and have a lower body mass index (BMI) than those with LE DVT/PE. Of patients with abdominal VT, children were more likely to have inferior vena cava (IVC) thrombosis than adults. For adults with venous thromboembolism (VTE), relatively more women had abdominal VT than LE DVT/PE, while the proportions with LE DVT/PE and abdominal VT by sex were similar in children. Children with abdominal VT were more likely to have diagnosed inherited thrombophilia, while trauma was more common in children with LE DVT/PE. In conclusion, both children and adults with abdominal VT were younger with a lower BMI than those with LE DVT/PE. Significant differences exist between children and adults in respect to abdominal VT compared to LE DVT/PE.
Keywords: Venous thromboembolism, deep venous thrombosis, paediatrics, abdominal vein thrombosis
Introduction
With more children living with chronic disease and with an increase in vascular procedures and indwelling catheters, the incidence of venous thromboembolism (VTE) in paediatric patients is increasing (1–4). In adults, VTE continues to be a major cause of morbidity, and its incidence in older women might be increasing (5). As with adults, the most common types of VTE in children are lower extremity deep-vein thrombosis (LE DVT) and pulmonary embolism (PE).
While less common than LE DVT/PE, abdominal vein thrombosis (abdominal VT) is a significant cause of morbidity in children and adults. Furthermore, abdominal VT can be a presenting sign of an underlying prothrombotic state, and its presence in the setting of known disease might have prognostic implications different from LE DVT/PE (6). Compared with LE DVT/PE, abdominal VT is not described well in the literature, particularly in children, where (the incidence is comparatively low. Paediatric providers and researchers often rely on data from adults to inform management decisions. Especially in the setting of abdominal VT, this approach is inadequate and could be improved through characterisation of adult and paediatric VTE as distinct clinical entities.
Children have different risk factors and locations of VTE compared with adults. Overall, 90% of paediatric patients who develop a VTE have an acquired or congenital risk factor for thrombosis, compared to about 60% for adults (3, 7). A common acquired risk factor for VTE in children is an indwelling central venous line (CVL), which has previously been reported in 33–59% of all paediatric cases and 80–97% of neonates with VTE (8, 9). In addition to CVLs, sepsis, antiphospholipid antibodies, malignancy, and trauma are also common acquired VTE risk factors in children.
Using data compiled from the Centers for Disease Control and Prevention (CDC)-funded U.S. Thrombosis and Hemostasis Centres Program from 2003–2011, we compared the demographic and clinical characteristics of adults and children with common VTE presentations, namely LE DVT or PE (LE DVT/PE), to those with abdominal vein thrombosis (abdominal VT) (i.e. thrombosis of hepatic, portal, splenic, mesenteric or renal veins, or inferior vena cava [IVC]). Our aim was to assess how abdominal VT differs from LE DVT/PE overall and among adults and children separately. Understanding differences in risk factors for less common presentations of VTE, including children and patients with abdominal VT, is important for developing age-specific prevention and management strategies. Patients with abdominal VT seem to present differently than those with LE DVT/PE, and the presenting characteristics, mechanisms of disease, and prognostic implications for children with VTE differ from those of adults. Ultimately, an overall lack of data on paediatric VTE, specifically abdominal VT, motivated this study. This report presents an analysis of VTE patients participating in this multi-site registry.
Materials and methods
Study setting, population, and design
We conducted this cross-sectional study across seven centres within the CDC-funded thrombosis and Hemostasis Centers Research and Prevention Network (the University of Michigan Hemophilia and Coagulation Disorders Program, Ann Arbor, MI, USA; the Thrombophilia Program, UNC, Chapel Hill, NC, USA; the Michigan State University Comprehensive Centre for Bleeding Disorders, East Lansing, MI, USA; the Wayne State University, Detroit, MI, USA; the Mountain States Regional Hemophilia and Thrombosis Centre, Aurora, CO, USA; the Duke Hemostasis and Thrombosis Program, Durham, NC, USA; UMDNJ-Robert Wood Johnson Medical School, New Brunswick, NJ, USA). The Thrombosis and Hemostasis Network Centers have been described previously (10).
Demographic and clinical characteristics were prospectively collected from consecutive consenting thrombosis and thrombophilia patients enrolled within one of seven Thrombosis and Haemostasis Centres over the nine-year period, from August 2003 to April 2011 using a standardised data-collection form. Many patients were referred to one of the seven centres by local providers for further evaluation and management of thrombotic disease, and most were seen as outpatients. This report presents an analysis of VTE patients participating in this multi-site registry.
Patients and/or their families attending one of the seven centres for medical care, or seen as an inpatient consult or referral, were approached by local centre staff for participation in a multi-site patient registry, regardless of age, gender, or race. For paediatric patients, consent was obtained from the parent or legal guardian as well as an assent for children older than seven years of age.
For consenting patients, data were collected at the initial and all subsequent visits and entered into a web-based registry maintained on a secure server within the Division of Blood Disorders at the CDC. Patient identifying information, including name, address, physician, and insurance carrier, remained within a locally housed secure database at each centre. For purposes of confidentiality, only the study identification number and registry information were sent to the registry at the CDC. The registry, study protocol, and other study materials are approved annually by the Institutional Review Hoards at each of the participating sites and at the CDC.
Inclusion and exclusion criteria
Utilising the Network’s patient registry, we identified patients with a history of abdominal VT and LE DVT/PE enrolled as of April 2011. Patients with a history of thrombosis Involving any of the hepatic, portal, mesenteric, renal, splenic, ovarian, and penile veins, or in the IVC were defined to have abdominal VT. Patients with a history of diagnosed VTE occurring only as lower extremity DVT and/or PE, i.e. no VTE in any other location at any time, comprised the comparison LE DVT/PE group. Lower extremity DVT and abdominal VT were considered objectively diagnosed when symptoms or signs of acute thrombus were present, and the diagnosis was confirmed by venography, compression venous duplex ultrasonography, impedance plethysmography, computed tomographic (CT) venography, or magnetic resonance imaging (MRI). Symptoms included pain, swelling, or sometimes evidence of organ dysfunction, as with renal vein thrombosis. A PE was considered objectively diagnosed when symptoms and/or signs of acute PE were present, and the diagnosis was confirmed by pulmonary angiography, a ventilation/perfusion lung scan interpreted as high probability for PE, CT pulmonary angiography, or MRI. Patients enrolled in the registry who did not meet the abdominal VT or LE DVT/PE definitions were excluded.
Measurements
Data collected for the registry included patient demographic and clinical characteristics, referral patterns, reasons for and details of the visit including providers seen, laboratory and radiological tests ordered, educational materials received, comorbidities, and treatments prescribed. To assess age-specific characteristics, the two age groups were further stratified by age at enrollment into paediatric (age <21 years) and adult (age ≥21 years) subgroups.
Definition of variables
The presence of medical comorbidities was defined as the patient having the condition within the three months prior to the VTE event. The presence of thrombophilia was defined by diagnosis of an inherited or acquired thrombophilia (factor V Leiden, prothrombin 20210A mutation, antiphospholipid syndrome, anti-thrombin, protein C or protein S deficiency) at enrollment or after subsequent evaluation by a CDC Thrombosis and Haemostasis Research and Prevention Network Centre. For patients with antiphospholipid antibodies and for many with an inherited thrombophilia, the presence of thrombophilia was confirmed by laboratory testing performed at the participating Centre, and the decision to test was at the discretion of the Network provider. The updated Sapporo criteria (11) were used for diagnosis of antiphospholipid syndrome. When assessing the prevalence of VTE complications, we restricted our analyses to those patients with sufficient time after their initial event for the complication to occur. Thus, we defined patients with multiple VTE as patients with more than one VTE occurring at least one month apart, and post-thrombotic syndrome (PTS) was assessed in patients at least 12 months after their initial presentation.
Analyses
The prevalence of a priori identified patient demographic and clinical characteristics for abdominal VT and LE DVT/PE were compared overall and separately among children and adults. For categorical variables, univariate frequencies were generated and compared using Pearson’s chi-square and two-tailed p-values, and in the case of small cell sizes (<5), two-tailed Fisher’s exact p-values are reported. For the continuous variables of age at first VTE and body mass index (BMI), the mean and median values were computed, and differences were tested for statistical significance using Student’s t-test and the Wilcoxon sign rank test, respectively. To assess the risk for abdominal VT compared to LE DVT/PE, unadjusted odds ratios (OR) and 95% confidence intervals (CI) were computed for those demographic and clinical characteristics that met the p=0.05 significance level among the paediatric and adult subgroups. Multiple logistic regression analysis was used lo generate adjusted OR and associated 95% CI and Wald p-values. To compare the prevalence of VTE complications between the two VTE groups, the proportion of patients who developed multiple VTE (VTE at least one month apart) and post-thrombotic syndrome (PTS) were calculated and compared overall and by age strata using Pearson’s chi-square and two-tailed p-values.
The distance from patient residence to Network centre was compared between patients with abdominal VT and LE DVT/PE to better characterise the patient population. Distances represent miles from the centroid of the home residence zip code to the centroid of the Centre’s zip code. Mean distance was calculated and then compared between the groups using Student’s t-test. All analyses were performed using SAS 9.2 (SAS Institute Cary, NC, USA).
Results
As of April 2011, the patient registry contained a total of 3,466 patients with VTE, of whom 466 were children. Among these, 55 children (11.8%) and 240 adults (8.0%) had abdominal VT, while 236 children (50.6%) and 2,308 adults (76.9%) met the criteria for the LE DVT/PE comparison group.
Presenting characteristics for patients with abdominal VT differed between paediatric and adult patients. Paediatric patients with abdominal VT were more likely to have IVC thrombus (25 of 55; 45.5%) than adults (40 of 240; 16.7%; p<0.0001). Conversely, paediatric patients were less likely to have hepatic, portal, and mesenteric thrombosis (n=35; 63.6%) than adults (n=205; 85.4%, p<0.0002). Five patients in each age group had abdominal VT involving the IVC and another abdominal vein.
There was no relationship between sex and location of VTE overall and among children, with equal proportions of boys and girls having abdominal VT and LE DVT/PE (Table 1). However, among adults, the abdominal VT group had more females than the LE DVT/PE group (67% vs. 60%; p=0.03; Table 1).
Table 1.
Comparison of patients with abdominal VT vs. LE DVT/PE by gender, race, ethnicity, age, and BMI.
| Overall | Age ≥ 21 | Age < 21 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Abd VT (n=295) N (%) | LE DVT/PE (n=2544) N (%) | p-value | Abd VT (n=240) N (%) | LE DVT/PE (n=2308) N (%) | p-value | Abd VT (n=55) N (%) | LE DVT/PE (n=236) N (%) | p-value | |
| Female | 189 (64.1) | 1520 (59.8) | 0.15 | 161 (67.1) | 1382 (59.9) | 0.03 | 28 (50.9) | 138 (58.5) | 0.31 |
| White race | 221 (77.8) | 1976 (78.7) | 0.74 | 189 (80.1) | 1813 (79.2) | 0.75 | 32 (66.7) | 163 (73.1) | 0.81 |
| Black race | 38 (13.4) | 414 (16.5) | 0.18 | 31 (13.1) | 377 (16.5) | 0.19 | 7 (14.6) | 37 (16.6) | 0.12 |
| Hispanic ethnicity | 24 (8.1) | 76 (3.0) | <0.0001 | 10 (4.2) | 52 (2.3) | 0.07 | 14 (25.5) | 24 (10.2) | 0.002 |
| Mean age at first VTE [year (SD)]* | 33.4 (17.6) | 41.3 (17.6) | <0.0001 | 38.8 (14.7) | 44.1 (16.0) | <0.0001 | 9.9 (7.2) | 14.2 (5.8) | 0.0001 |
| Median age at first VTE [year (SD)]* | 31.9 (0.01, 83.5) | 40.5 (0.01, 92.3) | <0.0001 | 36.3 (10.0, 83.5) | 43.2 (1.8, 92.3) | <0.0001 | 11.7 (0.01, 20.1) | 16.4 (0.01, 20.8) | <0.0001 |
| Mean BMI at enrollment [kg/m2 (SD)]** | 27.2 (7.8) | 30.4 (8.1) | <0.0001 | 28.5 (7.2) | 30.9 (7.9) | <0.0001 | 21.6 (7.6) | 25.1 (8.0) | 0.005 |
| Median BMI at enrollment [kg/m2 (range)]** | 26.4 (10.4, 60.9) | 29.10 (10.3, 72.6) | <0.0001 | 27.5 (15.7, 60.9) | 29.6 (15.0, 72.6) | <0.0001 | 20.2 (10.4, 51.9) | 23.3 (10.3, 58.9) | 0.0006 |
Median=Wilcoxon rank sum test p-value; Mean p-value- t test;
Age at first VTE missing in 2 with abdominal VT and 50 with LE DVT/PE.
BMI missing in 22 with abdominal VT and 272 with LE DVT/PE.
Abd VT, abdominal venous thrombosis; BMI, body mass index; LE DVT, lower extremity deep-vein thrombosis; PE, pulmonary embolism; N, number; VTE, venous thromboembolism.
The demographics of patients experiencing abdominal VT differed from those experiencing LE DVT/PE overall and by age. Overall, patients who develop abdominal VT tend to develop their first VTE earlier than those who developed LE DVT/PE (p<0.0001; ▶Figure 1). Most children with VTE were 13 years or older; however, among both adult and paediatric patients, the mean age at first VTE for patients having abdominal VT was lower than that of patients having LE DVT/PE (▶Table 1). Of the six neonates (<28 days) identified for the analysis, five had abdominal VT.
Figure 1.
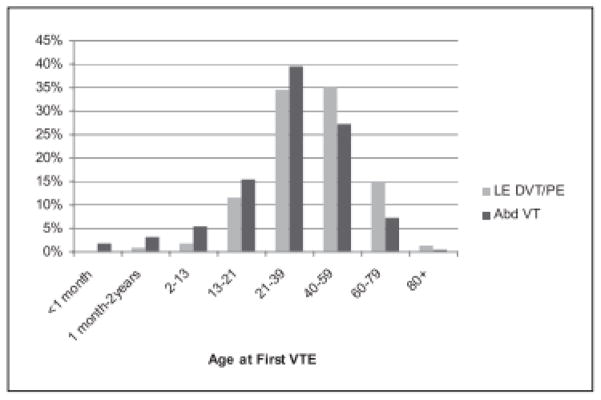
Distribution of age at first VTE occurrence among patients with abdominal VT and LE DVT/PE. Chi-square. p<0.0001; p for trend= <0.0001; Data not collected an 52 patients.
Similar to age, the mean and median body mass index (at enrollment) was lower for patients having abdominal VT than for patients having LE DVT/PE for both children and adults (Table 1). There was no difference by race between the two VTE groups overall. However, paediatric patients with abdominal VT were more likely to be of Hispanic ethnicity compared to paediatric patients with LE DVT/PE (25.5% vs. 10.2%; p=0.002). This relationship was not found in adults (▶Table 1).
Clinical characteristics also differed between the two VTE groups by age. Adults with abdominal VT had a higher prevalence of recent surgery, recent catheter, chronic renal and liver disease, and autoimmune conditions compared to the adult LE DVT/PE group (▶Table 2). Some reported autoimmune conditions included lupus, multiple sclerosis, rheumatoid arthritis, hypothyroidism, Bechet’s disease, Addison’s disease, sarcoidosis, and inflammatory bowel disease. Only two paediatric patients (3.6%) and eight adult patients (3.3%) with abdominal VT had a CVL. Only the relationship with autoimmune conditions was seen in the paediatric patients, but trauma was more frequently seen in paediatric patients with LE DVT/PE than abdominal VT (11% vs. 2%, p=0.03; ▶Table 2).
Table 2.
Frequency of clinical characteristics in patients with abdominal VT compared to patients with common VTE overall and by age.
| Overall | Age ≥ 21 | Age < 21 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Abd VT (n=295) N (%) | LE DVT/PE (n=2544) N (%) | p-value | Abd VT (n=240) N (%) | LE DVT/PE (n=2308) N (%) | p-value | Abd VT (n=55) N (%) | LE DVT/PE (n=236) N (%) | p-value | |
| Cancer | 20 (6.8) | 232 (9.1) | 0.18 | 20 (8.3) | 223 (9.7%) | 0.50 | 0 | 9 (3.8) | 0.22 |
| Surgery | 41 (13.9) | 240 (9.4) | 0.02 | 34 (14.2) | 204 (8.8) | 0.007 | 7 (12.7) | 36 (15.3) | 0.63 |
| Trauma/Injury | 9 (3.1) | 131 (5.2) | 0.12 | 8 (3.3) | 105 (4.6) | 0.38 | 1 (1.8) | 26 (11.0) | 0.03 |
| CVL related | 10 (3.4) | 35 (1.4) | 0.02 | 8 (3.3) | 10 (0.4) | <0.0001 | 2 (3.6) | 25 (10.6) | 0.11 |
| History of myocardial infarction | 9 (3.1) | 107 (4.2) | 0.34 | 9 (3.8) | 106 (4.6) | 0.55 | 0 | 1 (0.4) | 1.0 |
| History of stroke | 13 (4.4) | 111 (4.4) | 0.97 | 10 (4.2) | 107 (4.6) | 0.74 | 3 (5.5) | 4 (1.7) | 0.13 |
| Diabetes | 20 (6.8) | 182 (7.2) | 0.81 | 18 (7.5) | 176 (7.6) | 0.94 | 2 (3.6) | 6 (2.5) | 0.65 |
| Hypertension | 51 (17.3) | 517 (20.3) | 0.22 | 48 (20.0) | 512 (22.2) | 0.44 | 3 (5.4) | 5 (2.1) | 0.18 |
| Chronic renal disease | 13 (4.4) | 20 (0.8) | <0.0001 | 11 (4.6) | 19 (0.8) | <0.0001 | 2 (3.7) | 1 (0.4) | 0.09 |
| Chronic liver disease | 17 (5.8) | 79 (3.1) | 0.02 | 16 (6.7) | 76 (3.3) | 0.007 | 1 (1.8) | 3 (1.3) | 0.57 |
| Sickle cell disease/trait | 2 (0.7) | 12 (0.5) | 0.63 | 1 (0.4) | 9 (0.4) | 1.0 | 1 (1.8) | 3 (1.3) | 0.57 |
| Autoimmune conditions | 55 (18.6) | 307 (12.1) | 0.001 | 48 (20.0) | 296 (12.8) | 0.002 | 7 (12.7) | 11 (4.7) | 0.05 |
| Thrombophilic conditions* | |||||||||
| Factor V Leiden | 31 (10.5) | 318 (12.5) | 0.32 | 23 (9.6%) | 285 (12.3%) | 0.21 | 8 (14.6%) | 33 (14.0%) | 0.91 |
| Prothrombin G20210A | 12 (4.1) | 80 (3.1) | 0.40 | 7 (2.9%) | 73 (3.2%) | 0.84 | 5 (9.1%) | 7 (3.0%) | 0.05 |
| Protein C deficiency | 8 (2.7) | 31 (1.2) | 0.06 | 3 (1.3%) | 29 (1.3%) | 1.0 | 5 (9.1%) | 2 (0.9%) | 0.003 |
| Protein S deficiency | 6 (2.0) | 77 (3.0) | 0.34 | 4 (1.7%) | 72 (3.1%) | 0.21 | 2 (3.6%) | 5 (2.1%) | 0.62 |
| Antithrombin deficiency | 3 (1.0) | 14 (0.6) | 0.41 | 3 (1.3%) | 13 (0.6%) | 0.19 | 0 | 1 (0.4%) | 1 |
| APS | 28 (9.5) | 186 (7.3) | 0.18 | 19 (7.9%) | 156 (6.8%) | 0.5 | 9 (16.4%) | 30 (12.7%) | 0.47 |
| Any of the above thrombophilic conditions | 75 (25.4%) | 631 (24.8%) | 0.82 | 52 (21.7%) | 564 (24.4%) | 0.34 | 23 (41.8%) | 67 (28.4%) | 0.05 |
APS=antiphospholipid antibody syndrome. CVL=central venous line.
Reports percent of patients with known thrombophilia; not all patients were tested.
Abd VT, abdominal venous thrombosis; LE DVT, lower extremity deep-vein thrombosis; PE, pulmonary embolism; N, number; VTE, venous thromboembolism.
The prevalence of inherited thrombophilia or antibody syndrome (APS) did not differ between adults with abdominal VT compared to those with LE DVT/PE. However, children with abdominal VT were more likely to have a diagnosed thrombophilia (p=0.05) compared with children with lower extremity LE DVT/PE (▶Table 2). In particular, protein C deficiency and prothrombin 20210A were more commonly identified in children with abdominal VT than LE DVT/PE (p=0.003 and p=0.05, respectively). Adjusted OR for these risk factors are calculated and given in ▶Table 3.
Table 3.
Unadjusted and adjusted OR for risk factors for abdominal VT in adults (age ≥ 21) and paediatric patients (age < 21).
| Age ≥ 21 | Unadjusted OR (95% CI) | Adjusted* OR (95%CI) | Wald p-value |
|---|---|---|---|
| Female sex | 1.37 (1.03, 1.81) | 1.36 (0.99, 1.86) | 0.06 |
| Hispanic | 1.89 (0.95, 3.76) | 1.65 (0.79, 3.47) | 0.18 |
| Age first VTE | 0.98 (0.9, 0.99) | 0.98 (0.97, 0.99) | <0.0001 |
| BMI | 0.96 (0.94, 0.98) | 0.96 (0.94, 0.98) | <0.0001 |
| Surgery | 1.70 (1.15, 2.51) | 1.55 (1.02, 2.37) | 0.04 |
| Chronic renal disease | 5.79 (2.7, 12.3) | 4.04 (1.69, 9.70) | 0.002 |
| Chronic liver disease | 2.07 (1.2, 3.7) | 2.02 (1.09, 3.75) | 0.03 |
| Central venous line | 2.07 (3.10, 20.3) | 4.39 (1.60, 12.11) | 0.004 |
| Autoimmune conditions | 1.70 (1.21, 2.39) | 1.42 (0.98, 2.05) | 0.07 |
| Age < 21 | Unadjusted OR (95% % CI) | Adjusted* OR (95%CI) | Wald p-value |
|---|---|---|---|
| Hispanic ethnicity | 3.02 (1.44, 6.32) | 2.30 (0.97, 5.41) | 0.06 |
| Age at first VTE | 0.91 (0.87, 0.95) | 0.92 (0.87, 0.97) | 0.003 |
| BMI | 0.93 (0.88, 0.98) | 0.97 (0.92, 1.03) | 0.30 |
| Trauma/Injury | 0.15 (0.02, 1.13) | 0.17 (0.02, 1.38) | 0.10 |
| Autoimmune conditions | 2.98 (1.10, 8.90) | 4.45 (1.47, 13.51) | 0.008 |
| Prothrombin 20210A | 3.27 (1.0, 10.7) | 2.45 (0.62, 9.67) | 0.20 |
| Protein C deficiency | 11.70 (2.2, 62.0) | 13.4 (2.29, 78.7) | 0.004 |
Adjusted for all other listed variables.
BMI, body mass index CI, confidence interval; OR, odds ratio; VTE, venous thromboembolism.
Among adults, recent surgery, chronic renal disease, chronic liver disease, and recent catheter, were all found to be independent risk factors for abdominal VT compared to LE DVT/PE (▶Table 3). While older age and higher BMI were associated with LE DVT/PE. Similar to adults, older age was a risk for LE DVT/PE among the paediatric group, but other associations differed. Presence of autoimmune conditions and protein C deficiency were the only independent risk factors for abdominal VT in those under age 21 (▶Table 3).
Among females at least 13 years old, we did not find any difference in the use of oral contraceptives (OCs), hormone replacement therapies (HRTs), history of adverse pregnancy outcomes, or pregnancy-related VTE between those who had abdominal VT compared those with LE DVT/PE overall or by age.
The prevalence of additional VTE did not differ by VTE type or age (data not shown). Seventy-two adult (30.0%) and eight paediatric patients (15.4%) with abdominal VT had another VTE, among whom 41 developed a LE DVT/PE after their abdominal VT (34 DVT and 7 PE). The prevalence of post-thrombotic syndrome (PTS) did not differ between the adults or children with abdominal VT compared to those with LE DVT/PE. However, children with abdominal VT had a higher prevalence of PTS compared to adults with abdominal VT (17.7% vs. 7.8%; p=0.02). Conversely, children with LE DVT/PE were less likely to develop PTS than adults with LE DVT/PE (6.4% vs. 9.7%; p=0.05).
The mean distance to a referral centre was greater for adults with abdominal VT compared to LE DVT/PE (83.7 miles vs. 46.9 miles; p=0.04), but this relationship was not seen in children (50.9 miles vs. 56.1 miles; p=0.66).
Discussion
The study found several significant differences in patient characteristics and outcomes between abdominal VT and LE DVT/PE in children and adults: Both adult and paediatric patients with abdominal VT tended to be younger and have a lower BMI than patients with LE DVT/PE. Only six neonates (<1 month old) were included in the study, of whom five had abdominal VT. However, even outside of the neonatal period, children with abdominal VT were younger than those with LE DVT/PE. In our study, adult females with VTE were more likely to have abdominal involvement than males, and adults with abdominal VT were more likely to have hepatic, portal and/or mesenteric vein thrombosis, and common co-morbid conditions included recent surgery and autoimmune disorders. While, paediatric patients with abdominal VT in our study were more evenly divided between male and female, more commonly had IVC thrombosis, and co-morbid conditions, they were less likely to include recent trauma, in addition, children with abdominal VT were more likely to have an inherited thrombophilia, specifically protein C deficiency, compared to children with LE DVT/PE. Beth adult and paediatric patients with abdominal VT exhibited a high prevalence of multiple VTE events.
In a previous report, neonatal and pre-adolescent males and females have had similar incidences of VTE, while teenage girls were twice as likely as boys to develop VTE (12). In our study population, there was no gender predominance in paediatric patients, and there were relatively few patients <21 years old with pregnancy-related VTE. There were no pregnancy-related episodes of abdominal VT in children, and only eleven of 236 cases of LE DVT/PE in children were pregnancy-related. Our age cut-off of 21 years old reflects a general separation between paediatric and adult providers, but it is possible that pregnant adolescents are also managed by obstetricians, who could have different referral patterns compared to other paediatric providers.
Although the presence of a CVL is a common modifiable risk factor for VTE, only a small minority of the children and adults in our study had a CVL. This is almost certainly due to referral bias. Patients with modifiable risk factors, such as a CVL, or those with a disease commonly complicated by VTE (perhaps including pregnancy) may be less likely to be referred to one of the centres. Conversely, the registry contained a large proportion of VTE in patients with non-modifiable risk factors, such as antiphospholipid antibodies or inherited thrombophilia.
By comparing the distances travelled by patients seen at one of the seven CDC centres, we sought to explore referral patterns and perhaps gauge local providers’ level of comfort in managing common VTE compared to more unusual presentations of VTE. While there was no difference in distance to referral centre for children with abdominal VT vs. LE DVT/PE, adults with abdominal VT tended to come from greater distances than adults with LE DVT/PE. This discrepancy could stem from adult providers managing LE DVT/PE locally, whereas paediatric patients with any VTE could be more likely to be referred.
We found that children with abdominal VT were much more likely to have an inherited thrombophilia or antiphospholipid syndrome compared to children with LE DVT/PE, although not all patients were tested for thrombophilia which limits the interpretation of these data. Overall, the absolute risk for VTE in children heterozygous for a thrombophilia mutation is small; one large prospective study in patients with heterozygous protein C, protein S, antithrombin, and prothrombin gene defects found negligible rates of VTE in children <15 years of age (13). However, a large meta-analysis of observational studies showed a significant link between inherited thrombophilia mutations and first onset of VTE, with highest OR in patients with multiple thrombophilic traits or who had antithrombin, protein C, or protein S deficiencies (14). Again, we suspect that patients with non-modifiable risk factors were more likely to be referred to one of the centres.
We also found a large frequency of children had multiple VTE with both abdominal VT (15.4%) and LE DVT/PE (11.6%). Young et al. reported that 95% at children without a known acquired risk factor who developed recurrent VTE had at least one inherited risk factor, and 47% had two genetic risk factors (14). The overall recurrence risk for DVT in children has been estimated at 4–13% (2, 8, 14–17), and the higher frequency of multiple events in our population might stem from an increased proportion of patients with non-modifiable risk factors.
Adult data have shown that the cumulative incidence of VTE recurrence increases with follow-up duration (18), and this is almost certainly true for children as well. In a large German registry, the risk of recurrence in children who had no acquired risk factor on initial presentation at a median seven years of follow-up was reported to be about 21% (19).
Children with abdominal VT or LE DVT/PE were also more likely to have antiphospholipid antibodies when tested than adults with abdominal VT or LE DVT/PE, respectively. Previous studies have reported a positive lupus anticoagulant in about 25% of children with VTE (4); approximately 16% of paediatric patients in our study met diagnostic criteria for antiphospholipid syndrome.
Post-thrombotic syndrome (PTS) is a common cause of morbidity after DVT and consists of venous insufficiency, swelling, and pain occurring after VTE. Reports of PTS in children vary widely, with incidences reported between 9% (20) and 70% (3) of children with VTE outside the neonatal period. We found that children were more likely than adults to develop PTS following abdominal VT. The prevalence of PTS in children with abdominal VT in our study was 14.6% compared to 4.2% of children with lower extremity DVT/PE. Data from the Canadian registry at a median follow-up of 2 years showed 9% of children had developed PTS (20). Therefore it is important for providers to be cognisant of the high risk for PTS in children with abdominal VT since prompt initiation of anticoagulation therapy seems to reduce the risk for developing PTS in children (21) as well as adults (22).
Limitations
Although this study contains a large number of children and adults with a history of abdominal VT, the population studied may not be representative of all children and adults with VTE because of the potential for referral bias. Most patients were seen as outpatients, and a larger proportion of patients in the registry had a non-modifiable risk factor compared with VTE patients in the general population. We expect that the common presentations of VTE, especially those in the setting of modifiable risk factors, would be less likely to be referred to one of the Haemostasis and Thrombosis Centres. We chose 21 years of age for a cut-off between paediatric and adult patients but recognise variability exists on this topic in the literature. A central aim of our study was to compare presenting characteristics of abdominal VT vs. LE DVT/PE in children and adults to help inform patient care and management. VTE is a complex disease in which maturity of the coagulation system, presence of underlying disease or other risk factors, and medical environment of the patient interact. While our study contained a large proportion of patients with non-modifiable risk factors, the increasing incidence of paediatric VTE is likely driven by children with underlying medical disease living longer. These patients are often followed by paediatric specialists and have modifiable risk factors different from those in older adults.
Conclusions
The multi-site design of the CDC Thrombosis and Haemostasis Centres Network registry provides a means to compile robust data on both paediatric and adult VTE. Particularly, the Network’s enrollment of a large number of children with abdominal VT in the multi-site patient registry make it useful for comparing risk factors and characteristics in children with these variables to adults with similar clinical events. However, since the Centres are all large referral centres, the data collected in the registry may not be representative of all VTE patients.
Abdominal VT is a significant cause of morbidity and may be a harbinger of disease or have prognostic implications. Presenting characteristics differ between patients with abdominal VT compared to those with LE DVT/PE. The presence of abdominal VT, particularly in children, should trigger clinicians to investigate for thrombophilia, and following these patients prospectively, especially in the setting of non-modifiable risk factors for VTE, is important for elucidating prognostic information. Continued reports on the presentations and subsequent courses of abdominal VT and LE DVT/PE in children are needed to develop screening and treatment guidelines.
What is known about this topic?
Compared with lower extremity deep-vein thrombosis (DVT)/pulmonary embolism (PE), abdominal vein thrombosis (abdominal VT) is less common in children and adults.
Characteristics of children with venous thromboembolism (VTE) differ from those of adults.
Characteristics between patients with lower extremity DVT/PE likely differ from those with abdominal VT
What does this paper add?
We report data compiled from a large number of children and adults with VTE in a well-powered study investigating characteristics of patients with abdominal VT.
We report significant differences in clinical and demographic characteristics between children and adults with abdominal VT compared to those with lower extremity DVT/PE.
Acknowledgments
This work was supported by grants from the Centers for Disease Control and Prevention (DD000014 to T.L.O, DD000015 to P.B., R.K., and J.C.A;, DD000016 to M.M.J.; DD000017 to C.S.P.; DD07-004 to T.L.O, C.S.P., and M.M.J.; and DD07-005 to J.A.H and S.M.) and the National Institutes of Health (K12 HL 087097 to N.R.S).
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Conflicts of interest
None declared.
References
- 1.Raffini L, Huang YS, Witmer C, et al. Dramatic increase in venous thromboembolism in children’s hospitals in the United States from 2001 to 2007. Paediatrics. 2009;124:1001–1008. doi: 10.1542/peds.2009-0768. [DOI] [PubMed] [Google Scholar]
- 2.Chan AK, Deveber G, Monagle P, et al. Venous thrombosis in children. J Thromb Haemost. 2003;1:1443–1455. doi: 10.1046/j.1538-7836.2003.00308.x. [DOI] [PubMed] [Google Scholar]
- 3.Goldenberg NA. Long-term outcomes of venous thrombosis in children. Curr Opin Hematol. 2005;12:370–376. doi: 10.1097/01.moh.0000160754.55131.14. [DOI] [PubMed] [Google Scholar]
- 4.Journeycake JM, Manco-Johnson MJ. Thrombosis during infancy and childhood: what we know and what we do not Know. Hematol Oncol Clin North Am. 2004;18:1315–1338. viii–ix. doi: 10.1016/j.hoc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Silverstein MD, Heit JA, Mohr DN, et al. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158:585–593. doi: 10.1001/archinte.158.6.585. [DOI] [PubMed] [Google Scholar]
- 6.Gangat N, Wolanskyj AP, Tefferi A. Abdominal vein thrombosis in essential thrombocythemia: prevalence, clinical correlates, and prognostic implications. Eur J Haematol. 2006;77:327–333. doi: 10.1111/j.1600-0609.2006.00715.x. [DOI] [PubMed] [Google Scholar]
- 7.Goldenberg NA, Bernard TJ. Venous thromboembolism in children. Hematol Oncol Clin North Am. 2010;24:151–166. doi: 10.1016/j.hoc.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Monagle P, Adams M, Mahoney M, et al. Outcome of paediatric thromboembolic disease: a report from the Canadian Childhood Thrombophilia Registry. Paediatr Res. 2000;47:763–766. doi: 10.1203/00006450-200006000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt B, Andrew M. Neonatal thrombosis, report of a prospective Canadian and international registry. Paediatrics. 1995;96:939–943. [PubMed] [Google Scholar]
- 10.Dowling NF, Beckman MG, Manco-Johnson M, et al. The U.S. Thrombosis and Haemostasis Centres pilot sites program. J Thromb Thrombolysis. 2007;23:1–7. doi: 10.1007/s11239-006-9002-y. [DOI] [PubMed] [Google Scholar]
- 11.Miyakis S, Lockshin MD, Atsumi T, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS) J Thromb Haemost. 2006;4:295–306. doi: 10.1111/j.1538-7836.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 12.Stein PD, Kayali F, Olson RE. Incidence of venous thromboembolism in infants and children: data from the National Hospital Discharge Survey. J Paediatr. 2004;145:563–565. doi: 10.1016/j.jpeds.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 13.Tormene D, Simioni P, Prandoni P, et al. The incidence of venous thromboembolism in thrombophilic children: a prospective cohort study. Blood. 2002;100:2403–2405. doi: 10.1182/blood-2002-04-1186. [DOI] [PubMed] [Google Scholar]
- 14.Young G, Albisetti M, Bonduel M, et al. Impact of inherited thrombophilia on venous thromboembolism in children: a systematic review and meta-analysis of observational studies. Circulation. 2008;118:1373–1382. doi: 10.1161/CIRCULATIONAHA.108.789008. [DOI] [PubMed] [Google Scholar]
- 15.Babyn PS, Gahunia HK, Massicotte P. Pulmonary thromboembolism in children. Paediatr Radiol. 2005;35:258–274. doi: 10.1007/s00247-004-1353-y. [DOI] [PubMed] [Google Scholar]
- 16.Massicotte P, Julian JA, Gent M, et al. An open-label randomized controlled trial of low molecular weight heparin for the prevention of central venous line-related thrombotic complications in children: the PROTEKT trial. Thromb Res. 2003;109:101–108. doi: 10.1016/s0049-3848(03)00099-9. [DOI] [PubMed] [Google Scholar]
- 17.Kosch A, Kuwertz-Broking E, Heller C, et al. Renal venous thrombosis in neonates: prothrombotic risk factors and long-term follow-up. Blood. 2004;104:1356–1360. doi: 10.1182/blood-2004-01-0229. [DOI] [PubMed] [Google Scholar]
- 18.Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute-deep venous thrombosis. Ann Intern Med. 1996;125:1–7. doi: 10.7326/0003-4819-125-1-199607010-00001. [DOI] [PubMed] [Google Scholar]
- 19.Nowak-Gottl U, Junker R, Kreuz W, et al. Risk of recurrent venous thrombosis in children with combined prothrombotic risk factors. Blood. 2001;97:858–862. doi: 10.1182/blood.v97.4.858. [DOI] [PubMed] [Google Scholar]
- 20.Massicotte MP, Dix D, Monagle P, et al. Central venous catheter related thrombosis in children: analysis of the Canadian Registry of Venous Thromboembolic Complications. J Paediatr. 1998;133:770–776. doi: 10.1016/s0022-3476(98)70149-0. [DOI] [PubMed] [Google Scholar]
- 21.Sharathkumar AA, Pipe SW. Post-thrombotic syndrome in children: a single centre experience. J Paediatr Hematol Oncol. 2008;30:261–266. doi: 10.1097/MPH.0b013e318162bcf5. [DOI] [PubMed] [Google Scholar]
- 22.Segal JB, Streiff MB, Hofmann LV, et al. Management of venous thromboembolism: a systematic review for a practice guideline. Ann Intern Med. 2007;146:211–222. doi: 10.7326/0003-4819-146-3-200702060-00150. [DOI] [PubMed] [Google Scholar]


