Abstract
Objective
Research on the effects of weight cycling on health is mixed, strife with inconsistent definitions and the exclusion of African Americans. This study examined weight cycling prevalence among African American women prior to enrolling in a weight management program. Associations of weight cycling with physical and psychological health were conducted.
Design
Cross-sectional analysis.
Setting
Community-based weight-management program.
Participants
167 overweight or obese treatment-seeking African American women.
Main Outcome Measures
Weight cycling was examined in relation to physiological factors, including eating pathology, mood, self esteem, and physical health, specifically current weight, ideal weight, peak weight, and blood pressure.
Results
Weight cycling was prevalent (63%). Cyclers had higher current and peak weights (P<.01). Blood pressure did not differ between groups. Cyclers had higher drive for thinness, less body satisfaction, and less self-esteem for appearance (P<.05).
Conclusion
African American women are at risk for weight cycling and it may be associated with greater weight and poorer measures of psychological health. (Ethn Dis
Keywords: Weight Loss, African American Women, Blood Pressure, Weight Cycling
Introduction
Obesity and Weight Cycling
Nearly 80% of African American (AA) women are overweight or obese and obesity-related health disparities significantly affect their lives.1,2 Dieting, once considered as a nearly exclusive Caucasian enterprise,3 is quite common among AA women. A survey of 1,150 AAs conducted in 2002 revealed that nearly 14% reported dieting4 and in a study of weight-control practices among AAs, 61% reported trying to lose weight.5 In a recent study of low-income post-partum AA women, 75% reported dissatisfaction with current body size and 55.9% wanted to lose weight.6 However, a historically-biased view that body image disturbance and self-esteem effects of dieting are more common among Caucasian women7 may partially explain the limited research among ethnic minority groups.
The number of weight-loss studies targeting AA women, however, has increased.8,9 Unfortunately, data suggest that AA women may be at greater risk of weight regain after loss than their Caucasian counterparts.10 Therefore, as more AA women attempt to lose weight, they may be more likely to weight cycle (WC), or to have repeated loss and regain of body weight. Weight cycling has been reported in up to 80% of weight-loss treatment-seeking women of unreported ethnicity.11
As more AA women attempt to lose weight, they may be more likely to weight cycle (WC), or to have repeated loss and regain of body weight.
Weight Cycling and Physical Health
Links between WC and increased weight, hypertension, and eating-disordered cognitions have been proposed, however, studies on the physical and/or psychological health risks associated with WC have produced mixed results. Some studies report no relation between WC and physical health,12 while others suggest that cycling increases health risks. Specifically, WC has been associated with increased weight and central adiposity,13,14 hypertension,14,15 and type 2 diabetes.16 None of these studies, however, have examined an entirely AA sample or did not include information on participant ethnicity, limiting their generalizability. Consequently, the physical health risks associated with WC among AA women are unknown.
Weight Cycling and Psychological Health
Links between WC and psychological health are inconclusive. Studies have reported WC is associated with binge eating,17–19 anxiety, depression, and lower overall well-being18,20 in undefined or primarily Caucasian samples. Yet, other studies suggest no association with psychological health,21,22 and again, there is no information on these outcomes within different ethnic groups. Since dieting has been linked to increased eating disorder symptoms23 among Caucasian women, it is worth investigating whether similar links exist among AA women who diet. Although past research suggests AA women may accept and appreciate larger body sizes and are less likely to view themselves as overweight than other cultural groups,24 this finding may not apply to all AA.25 Given the increased rates of obesity among AA women, subsequent increased rates of dieting may mitigate this buffering effect26 on body image and the gap between Caucasian and AA women in body image disturbance is reportedly narrowing.27 As such, further investigation of the psychological impact of WC among AA women is warranted, rather than assuming that ethnic minority women are protected from low body esteem and drive for thinness.
Purpose of Present Study
Inconclusive results on the physical and psychological health problems associated with WC may be due, in part, to factors such as sex, age, and current weight of participants. And limited data among ethnic minority groups prevent adequate understanding of WC's effects on much of the population. The prevalence of obesity and related health disparities among AA women require a thoughtful examination of weight control efforts, including WC. As a fundamental step, the current study aimed to identify the prevalence of WC among overweight or obese AA women seeking weight-loss treatment. Further, we examined the association between WC and physical and psychological variables known to influence health. The amount of weight lost (20+ lbs) required to meet definition of WC in this study is the same amount as was used in the Nurses' Health Study II,28 a large trial that investigated the influence of WC on physical health factors. While the Nurses' Health Study II required this amount lost at least three times to be classified as a severe cycler, we were interested in capturing the full range of self-induced weight losses of 20+ lbs among AA women, a population for which this behavior has yet to be studied. Based on previous research, cyclers were expected to have higher current weight, peak weight, and blood pressure. We further aimed to expand upon gaps in previous literature among AA women by hypothesizing that AA women who had cycled would experience poorer self-esteem, poorer psychological health (eg, symptoms of depression and anxiety) and greater body image disturbance than non-cyclers, as has been reported among Caucasian women or among women of unreported race, but not yet studied in AA women.
Method
Participants
Participants were 167 overweight or obese AA women enrolled in a community-based weight-loss program. Participants gave written consent to participate and completed 13 weeks of weight-loss treatment, however the present data are from baseline assessments completed prior to the program. This study was approved by the university's human subjects review board.
Procedure
The current investigation is part of a larger ongoing study that recruited only AA women by newspaper advertisements and church bulletins. Inclusion criteria required participants to be overweight/ obese (BMI: 27–40 kg/m2), female nonsmokers aged 18–60 years. Exclusion criteria included medical problems affecting metabolism or exercise participation including heart disease, recent weight loss (ie, more than 9.1kg in the past 6 months or 4.5kg in the past month), thyroid disease, renal failure, diabetes, current tobacco use, pregnancy, antidepressant use, or uncontrolled high blood pressure defined by physician evaluation. Physician approval was required. Height, weight, and blood pressure were measured at baseline and participants completed self-report measures related to psychological health and history of eating behavior.
Measures
Demographic Information
Demographic information was assessed using a self-report questionnaire created for the ongoing treatment outcome study. The questions were formatted as either check-the-box or fill-in-the-blank, and included the following questions: for race participants checked one or more boxes (African American, White, African, Hispanic, West Indies/Caribbean, American Indian or Alaska, Native Hawaiian or Pacific Islander, Other, or no response); age; employment status (part-time, fulltime, retired, disabled, homemaker, or unemployed); level of education (some high school, GED, graduated high school, attended/graduated college, or attended/graduated graduate school); and marital status (single, cohabitating, married, separated, divorced, or widowed).
Blood Pressure
Blood pressure (BP) measurements were taken by a registered nurse or trained research assistant using a random zero sphygmomanometer and appropriately-sized cuffs. Readings were classified according to the Joint National Committee (JNC) V Guidelines for Blood Pressure (Table 1).29 Participants' blood pressure readings were measured after the orientation session, which allowed participants to rest in the seated position for approximately 40 minutes prior to measurements. Pressures were measured one time unless a high reading (>120/80 mm Hg) resulted. In these cases, pressures were measured a second time and the first reading was excluded from the present analysis.
Table 1. Demographic information*.
| Weight Cyclers (n=105) | Non-Cyclers (n=62) | |
|---|---|---|
| Age | 41.57 (9.41) | 41 (8.95) |
| Education, ≥16 years | 54 (52%) | 31 (50%) |
| Full-time employment | 94 (90%) | 59 (95%) |
| Individual income, >$40,000 | 70 (67%) | 40 (65%) |
| Married | 49 (47%) | 37 (60%) |
| Hypertension classification†, mm Hg | ||
| Normal, <120/<80 | 29 (28%) | 20 (32%) |
| Pre-HTN, 120–139/80–89 | 46 (44%) | 28 (46%) |
| Stage 1 HTN, 140–159/90–99 | 22 (21%) | 12 (19%) |
| Stage 2 HTN, >160/>100 | 6 (6%) | 2 (4%) |
Results are given as mean (SD) for age or n (%).
Joint National Committee 7 Guidelines for Blood Pressure.27
HTN, hypertension.
Height and Weight
Participants' height (centimeters) and weight (kilograms) were assessed using a standard balance beam scale. Body mass index (BMI) in kg/m2 was calculated from these measurements.
Self-esteem
The State Self-esteem Scale (SSES) was used to assess global and appearance-specific self-esteem.30 The measure requires respondents to use a 5-point scale to rate their current feelings (1=Not at all and 5=Extremely) such as body image, public regard, and confidence. Intercorrelations with the Rosenberg Self Esteem scale (RSE)31 revealed high convergent validity (r=.72) in a sample of unreported ethnicity.32
Mood
Mood was assessed with the Beck Depression Inventory-II (BDI-II), a 21-item questionnaire designed to measure the extent and severity of depressive symptomology33 which is validated for use among AA.34 Anxiety was measured with the Beck Anxiety Inventory (BAI).35 A confirmatory factor analysis of the BAI among AA college students revealed differences on the factor loadings of scale among this racial group; however, the authors support its use as an anxiety screening tool,36 which is how it was used in the present study.
Weight Cycling, Eating Pathology, and Body Image Disturbance
Weight cycling was assessed by the answer to question 9 on the Questionnaire on Eating and Weight Patterns Revised (QEWP-R)37, which asks “How many times (approximately) have you lost 20 lbs (9.1kg) or more when you weren't sick and then gained it back?” Participants were categorized as cyclers if their response was “once” to “five times or more.”
The Binge Questionnaire, a 9-item self-report questionnaire, was used to assess likelihood to binge eat.38 The reported one-month test-retest reliability of the scale was good (r=.88), and the only cross-cultural work on this scale reports an alpha coefficient of .70 among a sample of Arab women suggesting decent internal validity.39 The Eating Disorders Inventory (EDI-2) assesses behavioral and attitudinal characteristics observed in eating disor-ders.40 The body dissatisfaction and drive for thinness subscales were used in the present study. While the EDI has not been normed among AA samples, body image disturbance among ethnic and racial minority groups has been assessed.27
Results
Demographics
Analyses are based on 167 AA women with a mean age of 42 years (SD=9.11) and BMI of 36.08 kg/m2 (SD=5.81). Cyclers and non-cyclers did not differ on demographic information including age, education, employment status, income, marriage, or medication use (all P>.05). See Table 1 for a list of all demographic information.
Sixty-three percent of participants (n=105) were defined as cyclers. See Table 2 for a description of reported WC history. Interestingly, more than half of cyclers had cycled more than three times. Analysis of variance tests were used to assess differences in physical health, psychological health and eating pathology between cyclers (n=105) and non-cyclers (n=62).
Table 2. Psychological variables and blood pressure by weight cycling history, mean (standard deviation).
| Self Esteem for Appearance |
Total Self Esteem |
BDI | BAI | Binge Likelihood |
Drive for Thinness |
Body Dissatisfaction |
Systolic BP (mm Hg) |
Diastolic BP (mm Hg) |
||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of weight cycles as defined on QEWP-R | ||||||||||
| 0 (n=62) | 18.47 (3.52) | 79.83 (11.72) | 4.89 (5.42) | 3.46 (4.42) | 15.84 (7.86) | 3.02 (3.85) | 14.43 (6.43) | 125.74 (16.76) | 79.91 (9.95) | |
| 1–2 (n=50) | 16.42 (3.11) | 77.25 (9.74) | 6.11 (5.13) | 4.70 (5.00) | 17.45 (8.58) | 5.01 (4.43) | 18.10 (6.43) | 128.21 (17.68) | 80.24 (12.30) | |
| 3–4 (n=46) | 18.37 (3.94) | 81.07 (12.03) | 7.91 (6.88) | 5.29 (9.19) | 20.00 (6.92) | 3.86 (3.77) | 15.81 (5.82) | 132.50 (18.08) | 82.87 (11.85) | |
| ≥5 (n=9) | 14.00 (3.38) | 73.92 (6.90) | 6.50 (5.47) | 5.42 (6.08) | 22.08 (8.85) | 5.91 (4.34) | 22.33 (4.58) | 125.65 (11.14) | 80.71 (8.75) | |
QEWP-R, Questionnaire on Eating and Weight Patterns Revised; BDI, Beck Depression Inventory; BAI, Beck Anxiety Inventory; BP, Blood Pressure.
Physical Outcomes
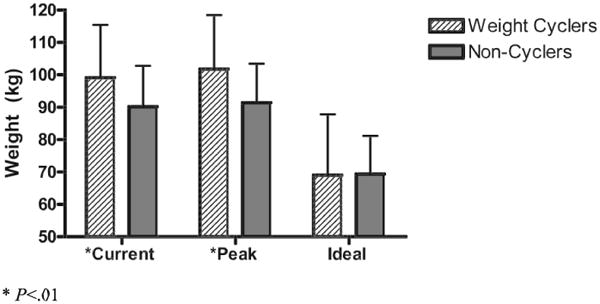
Cyclers weighed more, had a higher BMI, and reported a higher peak weight compared to non-cyclers, despite reporting no differences in ideal weight. Figure 1 depicts cyclers' and non-cyclers' current weight, peak weight, and ideal weight. Cyclers reported being at their highest weight ever while non-cyclers were slightly below.
Fig 1. Weight differences between weight cyclers and non-cyclers.
Due to the known association of body weight and BP and the 9.1kg difference in body weight between cyclers and non-cyclers, weight was controlled in BP analyses. As displayed in Table 3, there were no differences in systolic or diastolic BP between cyclers and non-cyclers. Despite participants' physician approval to participate in the study and confirmation that all participants had normal BP prior to enrollment, 21% of cyclers and 21% of non-cyclers reported a history of hypertension. Additionally, the groups did not differ in JNC Stage Classification, as depicted in Table 1.
Table 3. Analysis of variance results for blood pressure and psychological measure scores controlling for baseline weight, mean (SD).
| Weight Cyclers (n=105) |
Non-Cyclers (n=62) |
ANOVA F | ||
|---|---|---|---|---|
| Blood Pressure, mm Hg | ||||
| Systolic | 128.64 (16.97) | 125.74 (16.77) | 1.62 | |
| Diastolic | 80.81 (11.70) | 79.91 (9.96) | 1.69 | |
| Self-esteem, SSES | ||||
| Self-esteem for appearance* | 16.59 (3.64) | 18.31 (3.52) | 3.56 | |
| Global self-esteem | 77.70 (10.37) | 79.35 (11.82) | 1.07 | |
| Mood | ||||
| Depressive symptoms, BDI total score | 6.53 (5.70) | 4.98 (5.50) | 1.39 | |
| Anxiety, BAI total score | 4.84 (8.42) | 3.56 (4.49) | 2.04 | |
| Eating Pathology | ||||
| Binge Questionnaire | 18.48 (8.42) | 15.87 (7.92) | 1.75 | |
| Drive for Thinness, EDI-2 subscale* | 4.94 (4.33) | 3.02 (3.89) | 3.86 | |
| Body Dissatisfaction, EDI-2 subscale* | 18.06 (6.36) | 14.43 (6.07) | 5.58 | |
SSES, State Self-esteem Scale; BDI, Beck Depression Inventory; BAI, Beck Anxiety Inventory; EDI, Eating Disorders Inventory.
P<.05.
Psychological Outcomes
Since the relationships between body weight and psychological variables remained to be elucidated, all analyses were completed both when controlling for body weight and when not controlling for body weight. When body weight was not controlled, the WC groups differed in depressive symptoms, F (2,141)=4.92, P<.05, and the likelihood to binge eat, F (2,139)=8.62, P<.05. Binge scores were in the clinical range, suggesting that participants endorsed some level of disordered eating behaviors.
When controlling for baseline weight, cyclers reported significantly lower self-esteem for their appearance and greater body dissatisfaction and drive for thinness compared to non-cyclers, however, all scores were within clinically normal limits. Average total self-esteem scores, symptoms of anxiety, and symptoms of depression were all clinically nonsignificant and did not differ between cyclers and non-cyclers. Mean and standard deviations for psychological measures are presented in Table 3.
Post-hoc Analyses
The number of cyclers with five or more cycles was very low; analyses to detect differences in psychological measures among individuals who had weight cycled “one or two times, three or four times, or five or more times” were underpowered. Therefore, Pearson's correlations were calculated to assess the association between number of cycles as a continuous variable and psychological factors. WC was negatively correlated with global self-esteem (P<.05) and positively correlated with likelihood of bingeing (P<.01), drive for thinness (P<.05), and body dissatisfaction (P<.01) (See Table 4).
Table 4. Intercorrelations for psychological variables, blood pressure, and continuous measure of weight cycling.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1.Number of weight cycles | – | |||||||||
| 2.Self-esteem for appearance | −.082 | – | ||||||||
| 3.Global self-esteem | −.235* | .672† | – | |||||||
| 4.Depressive symptomology | .153 | −.470† | −.447 | – | ||||||
| 5.Anxiety | .124 | −.435† | −.439† | .598† | – | |||||
| 6.Binge questionnaire | .233 | −.021 | −.062 | .169* | .087 | – | ||||
| 7.Drive for thinness | .172* | −.537† | −.379† | .443* | .260† | .186* | – | |||
| 8.Body dissatisfaction | .267† | −.096 | −.494† | .297† | .123 | .106 | .134 | – | ||
| 9.Systolic blood pressure | .058 | .081 | .109 | −.028 | .059 | –.039 | –.110 | –.061 | – | |
| 10.Diastolic blood pressure | .056 | .041 | .114 | −.034 | .075 | –.007 | –.049 | –.035 | .625† | – |
P<.05.
P<.01.
Discussion
To our knowledge, this is the first study to report on the prevalence of WC among a community sample of AA women presenting for weight-loss treatment. Our findings suggest that this phenomenon is quite common; two thirds of participants in our sample reported losing and regaining 9.1 kg not due to illness at least once. One-third reported experiencing this type of WC three or more times. These data are similar to a previous report that 80% of treatment-seeking women of unreported race had weight cycled.11 This replication of findings in our sample lends support to the notion that intentional weight loss, followed by regain, may be quite common among overweight AA women. Given the increasing prevalence of overweight and obesity among AA women, it is likely that this number will continue to rise as more women attempt weight loss.
With regards to physical health and WC, cyclers weighed more upon entry into treatment and reported higher peak weights compared to non-cyclers. However, reported ideal weight did not differ by group. Surprisingly, almost 70% of the sample's BP measured in the prehypertensive or hypertensive range, despite being screened for uncontrolled hypertension prior to enrollment. These findings are of concern and may reflect poor BP control among a significant number of individuals.41 Although research suggests that AA women do not differ from Caucasians on reasons for seeking weight-loss treatment,42,43 the finding that many AA women seeking treatment had elevated BP highlights the importance of educating women about the risk factors associated with obesity.
Our findings suggest that this phenomenon [weight cycling] is quite common; two thirds of participants in our sample reported losing and regaining 9.1 kg not due to illness at least once.
Psychological health also varied by cycling history. African American cyclers were more likely to binge eat and reported greater body image disturbance and drive for thinness compared to their non-cycling counterparts. However, the groups did not differ in depressive or anxious symptomatology, suggesting that the relationship between psychological health and WC may be limited to the domain of body image and eating. These results are similar to existing literature, although such results had previously only been reported among Caucasian samples.17,18
Although cyclers reported poorer self-esteem for their appearance, scores were within clinically normal limits. However, it is important to consider that clinical norms have been established in primarily Caucasian samples. Thus, lower self-esteem among AA women cyclers, in combination with our findings that both cyclers and non-cyclers scored above published norms for overweight women on binge eating38 and body dissatisfaction40 warrants further research. Future studies should attempt to develop norms on measures of binge eating, body dissatisfaction, and body-related self-esteem among AA women. Without relevant norms, it is difficult to draw appropriate conclusions and determine which scores are clinically significant. Our results do, however, lend support to the notion that AA women experience minimal non-eating related psychological distress related to being overweight25 as indicated by the low levels of anxiety and depression in both groups.
Limitations of this work should be addressed. Our sample comprised treatment-seeking women enrolling in a weight-management study with several exclusion criteria, therefore the generalizability of our findings may be restricted. For example, recent cyclers may have been excluded from this study due to the exclusion criteria of a loss of 9.1kg or more over the past six months. Additionally, we attempted to exclude hypertensive patients. While some patients with blood pressure readings in the hypertensive range were enrolled, our exclusion criteria may have increased the likelihood of rejecting a true hypothesis linking weight cycling to higher blood pressure. In addition, due to inconsistency in nonresponse across measures, the subsequent small sample size of nonresponders for each measure does not allow for adequately powered comparisons between responders and nonresponders. However, because this study is the first of its kind, our findings are an important step in expanding the literature in WC to an understudied group.
Also, there is no single agreed upon definition of the WC construct.44 The National Institutes of Health suggest that small weight cycles range from loss and regain of 2.3–4.5kg, whereas a large cycle may be characterized by 23kg or more. Assessment methods also vary, from open-ended questions such as, “Have you lost and gained weight in the past?”45 to measuring a specific number of kilograms lost and regained a particular number of times.46 The definition chosen for this study might not have captured women who cycle more frequently or cycle through smaller losses and gains (eg, 4.5kg). Yet another assessment issue is that many of the measures we included in this study have yet to be validated among AA samples.
AA women are at increased risk for obesity and obesity-related morbidities and mortality. Yet data rarely include analysis of obesity from a cultural perspective for AA and effective assessment tools and treatment approaches are lacking. Our study used a previously supported definition of WC and found interesting and meaningful differences between cyclers and non-cyclers, which could be useful in expanding on the somewhat confusing extant literature on WC. Our findings support the notion that the buffer proposed to protect AA women's body image47 may not uniformly apply.25 Rather, some of the same pressures traditionally faced by Caucasian women regarding appearance, such as pressure to achieve a lower body weight, may be important to assess among AA treatment seekers as well. In fact, very recent data suggest that emphasizing physical appearance in treatment groups resulted in great weight loss at 6 and 12-month follow up among a group of AA and Caucasian treatment-seeking women.43 Although AA women's body size and shape ideals may still differ from Caucasians', understanding the unique physical and psychological impact of weight loss attempts for AA women is important.
Replication of our results in additional AA samples will be important, particularly using measures that have been validated with AA samples. The prevalence of WC in our sample underscores the importance of further exploration of clinically meaningful outcomes which may be related to cycling, such as waist circumference and eating patterns. While AA women have often been considered buffered from body image ideals common among Caucasian women, our findings that WC was associated with poorer self esteem and body image among AAs highlight the need for further analysis.
Acknowledgments
Funding for this project was made possible (in part) by P20MD000505 from the National Center on Minority Health and Health Disparities. The views expressed here do not necessarily reflect the official policies of the Department of Health and Human Services nor does mention by trade names, commercial practices, or organizations imply endorsement by the US Government.
Footnotes
Author Contributions: Design concept of study: Osborn, Forys, Sbrocco
Acquisition of data: Osborn, Forys, Sbrocco
Data analysis and interpretation: Osborn, Forys, Psota, Sbrocco
Manuscript draft: Osborn, Forys, Psota, Sbrocco
Statistical expertise: Osborn, Forys, Psota, Sbrocco
Acquisition of funding: Osborn, Sbrocco
Administrative: Osborn, Forys, Psota, Sbrocco
Supervision: Osborn, Sbrocco
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Singh V, Deedwania P. Dyslipidemia in special populations: Asian Indians, African Americans, and Hispanics. Curr Atheroscler Rep. 2006;8(1):32–40. doi: 10.1007/s11883-006-0062-4. [DOI] [PubMed] [Google Scholar]
- 3.Root MPP. Disordered eating in women of color. Sex Roles. 1990;22:525–535. [Google Scholar]
- 4.Paeratakul S, YorkCrowe EE, Williamson DA, Ryan DH, Bray GA. Americans on diet: results from the 1994–1996 Continuing Survey of Food Intakes by Individuals. J Am Diet Assoc. 2002;102(9):1247–1251. doi: 10.1016/s0002-8223(02)90276-2. [DOI] [PubMed] [Google Scholar]
- 5.Clark JM, Bone LR, Stallings R. Obesity and approaches to weight in an urban African-American community. Ethn Dis. 2001;11(4):676–686. [PubMed] [Google Scholar]
- 6.Boyington J, Johnson A, CarterEdwards L. Dissatisfaction with body size among low-income, postpartum Black women. J Obstet Gynecol Neonatal Nurs. 2006;36:144–151. doi: 10.1111/j.1552-6909.2007.00127.x. [DOI] [PubMed] [Google Scholar]
- 7.Caldwell MB, Brownell KD, Wilfley DE. Relationship of weight, body dissatisfaction, and self-esteem in African American and white female dieters. Int J Eat Disord. 1997;22(2):127–130. doi: 10.1002/(sici)1098-108x(199709)22:2<127::aid-eat2>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 8.Bronner Y, Boyington JE. Developing weight loss interventions for African-American women: elements of successful models. J Natl Med Assoc. 2002;94(4):224–235. [PMC free article] [PubMed] [Google Scholar]
- 9.Kumanyika SK, WhittGlover MC, Gary TL, et al. Expanding the obesity research paradigm to reach African American communities. Prev Chronic Dis. 2007;4(4):A112. [PMC free article] [PubMed] [Google Scholar]
- 10.Weinsier RL, Hunter GR, Zuckerman PA, et al. Energy expenditure and free-living physical activity in black and white women: comparison before and after weight loss. Am J Clin Nutr. 2000;71(5):1138–1146. doi: 10.1093/ajcn/71.5.1138. [DOI] [PubMed] [Google Scholar]
- 11.Strychar I, Lavoie ME, Messier L, et al. Anthropometric, metabolic, psychosocial, and dietary characteristics of overweight/obese postmenopausal women with a history of weight cycling: a MONET (Montreal Ottawa New Emerging Team) study. J Am Diet Assoc. 2009;109(4):718–724. doi: 10.1016/j.jada.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 12.Field AE, Byers T, Hunter DJ, et al. Weight cycling, weight gain, and risk of hypertension in women. Am J Epidemiol. 1999;150(6):573–579. doi: 10.1093/oxfordjournals.aje.a010055. [DOI] [PubMed] [Google Scholar]
- 13.Wallner SJ, Luschnigg N, Schnedl WJ, et al. Body fat distribution of overweight females with a history of weight cycling. Int J Obes Relat Metab Disord. 2004;28(9):1143–1148. doi: 10.1038/sj.ijo.0802736. [DOI] [PubMed] [Google Scholar]
- 14.Guagnano MT, Ballone E, PacePalitti V, et al. Risk factors for hypertension in obese women. The role of weight cycling. Eur J Clin Nutr. 2000;54(4):356–360. doi: 10.1038/sj.ejcn.1600963. [DOI] [PubMed] [Google Scholar]
- 15.Guagnano MT, PacePalitti V, Carrabs C, Merlitti D, Sensi S. Weight fluctuations could increase blood pressure in android obese women. Clin Sci (Lond) 1999;96(6):677–680. doi: 10.1042/cs0960677. [DOI] [PubMed] [Google Scholar]
- 16.Holbrook TL, BarrettConnor E, Wingard DL. The association of lifetime weight and weight control patterns with diabetes among men and women in an adult community. Int J Obes. 1989;13(5):723–729. [PubMed] [Google Scholar]
- 17.Venditti EM, Wing RR, Jakicic JM, Butler BA, Marcus MD. Weight cycling, psychological health, and binge eating in obese women. J Consult Clin Psychol. 1996;64(2):400–405. doi: 10.1037//0022-006x.64.2.400. [DOI] [PubMed] [Google Scholar]
- 18.Marchesini G, Cuzzolaro M, Mannucci E, et al. Weight cycling in treatment-seeking obese persons: data from the QUOVADIS study. Int J Obes Relat Metab Disord. 2004;28(11):1456–1462. doi: 10.1038/sj.ijo.0802741. [DOI] [PubMed] [Google Scholar]
- 19.Spitzer RL, Yanovski S, Wadden T, et al. Binge eating disorder: its further validation in a multisite study. Int J Eat Disord. 1993;13(2):137–153. [PubMed] [Google Scholar]
- 20.Fontaine KR, Barofsky I, Bartlett SJ, Frankowiac SC, Andersen RE. Weight loss and health related quality of life: Results at 1-year follow-up. Eating Behavior. 2004;5:85–88. doi: 10.1016/S1471-0153(03)00059-X. [DOI] [PubMed] [Google Scholar]
- 21.SimkinSilverman LR, Wing RR, Plantinga P, Matthews KA, Kuller LH. Lifetime weight cycling and psychological health in normal-weight and overweight women. Int J Eat Disord. 1998;24(2):175–183. doi: 10.1002/(sici)1098-108x(199809)24:2<175::aid-eat7>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 22.Clark MM, King TK. Eating self-efficacy and weight cycling: a prospective clinical study. Eat Behav. 2000;1(1):47–52. doi: 10.1016/s1471-0153(00)00009-x. [DOI] [PubMed] [Google Scholar]
- 23.Stice E. A prospective test of the dual-pathway model of bulimic pathology: Mediating effects of dieting and negative affect. J Abnorm Psychol. 2001;110(1):124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- 24.Kumanyika S, Wilson J, GuilfordDavenport M. Weight-related attitudes and behaviors in Black women. J Am Diet Assoc. 1993;93:416–422. doi: 10.1016/0002-8223(93)92287-8. [DOI] [PubMed] [Google Scholar]
- 25.Sabik NJ, Cole ER, Ward LM. Are all minority women equally buffered from negative body image? Intra-ethnic moderators of the buffering hypothesis. Psychol Women Qtrly. 2010;34(2):139–151. [Google Scholar]
- 26.Grabe S, Hyde JS. Ethnicity and body dissatisfaction among women in the United States: A meta-analysis. Psychol Bull. 2006;132:622–640. doi: 10.1037/0033-2909.132.4.622. [DOI] [PubMed] [Google Scholar]
- 27.Roberts A, Cash T, Feingold A, Blair J. Are Black–White differences in females' body dissatisfaction decreasing? A meta-analytic review. J Consult Clin Psychol. 2006;74(6):1121–1131. doi: 10.1037/0022-006X.74.6.1121. [DOI] [PubMed] [Google Scholar]
- 28.Field AE, Manson JE, Taylor CB, Willett WC, Colditz GA. Association of weight change, weight control practices, and weight cycling among women in the Nurses' Health Study II. Int J Obes Relat Metab Disord. 2004 Sep;28(9):1134–1142. doi: 10.1038/sj.ijo.0802728. [DOI] [PubMed] [Google Scholar]
- 29.The fifth report of the Joint National Committee on Detection Evaluation Treatment of High Blood Pressure. Arch Intern Med. 1993;153:154–183. [PubMed] [Google Scholar]
- 30.Heatherton TF, Polivy J. Development and validation of a scale for measuring state self-esteem. J Pers Soc Psyc. 1991;60:895–910. [Google Scholar]
- 31.Rosenberg M. Society and the Adolescent Self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 32.Heatherton TF, Polivy J. Development and validation of a scale for measuring state self-esteem. J Pers Soc Pscyhol. 1991;60(6):895–910. [Google Scholar]
- 33.Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory II (BDI-II) San Antonio, Tx: Psychology Corporation; 1996. [Google Scholar]
- 34.Grothe KB, Dutton G, Jones GN, Bodenlos J, Anconaa M, Brantley PJ. Validation of the Beck Depression Inventory—II in a low-income African American sample of medical outpatients. Psychol Assess. 2005;17(1):110–114. doi: 10.1037/1040-3590.17.1.110. [DOI] [PubMed] [Google Scholar]
- 35.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 36.Chapman LK, Williams SR, Mast BT, WoodruffBorden J. A confirmatory factor analysis of the Beck Anxiety Inventory in African American and European American young adults. J Anxiety Disord. 2009;23:387–392. doi: 10.1016/j.janxdis.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 37.Spitzer RL, Yanovski SZ, Marcus M. The Questionnaire on Eating and Weight Patterns-Revised (QEWP-R) New York: New York State Psychiatric Institute; 1993. [Google Scholar]
- 38.Hawkins RC, Clement PF. Development and construct validation of a self-report measure of binge eating tendencies. Addict Behav. 1980;5:219–226. doi: 10.1016/0306-4603(80)90042-8. [DOI] [PubMed] [Google Scholar]
- 39.Dolan B, Ford K. Binge eating and dietary restraint: A cross-cultural analysis. Int J Eat Disord. 1991;10(3):345–353. [Google Scholar]
- 40.Garner DM. The Eating Disorder Inventory-2 Professional Manual. Odessa, Fla: Psychological Assessment Resources; 1991. [Google Scholar]
- 41.Nieto FJ, Alonso J, Chambless LE, et al. Population awareness and control of hyper-tension and hypercholesterolemia. The Atherosclerosis Risk in Communities study. Arch Intern Med. 1995;155(7):677–684. [PubMed] [Google Scholar]
- 42.StriegelMoore RH, Wilfley DE, Caldwell MB, Needham ML, Brownell KD. Weight-related attitudes and behaviors of women who diet to lose weight: a comparison of Black dieters and White dieters. Obes Res. 1996;4:109–116. doi: 10.1002/j.1550-8528.1996.tb00522.x. [DOI] [PubMed] [Google Scholar]
- 43.Kalarchian MA, Levine MD, Klem MD, Burke LE, Soulakova JN, Marcus MD. Impact of addressing reasons for weight loss on behavioral weight-control outcome. Am J Prev Med. 2011;40(1):18–24. doi: 10.1016/j.amepre.2010.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Strohacker K, Carpenter KC, McFarlin BK. Consequences of weight cycling: an increase in disease risk? Int J Exerc Sci. 2009;2(3):191–201. doi: 10.70252/ASAQ8961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Foreyt JP, Brunner RL, Goodrick GK, Cutter G, Brownell KD, Jeor ST., St Psychological correlates of weight fluctuation. Int J Eat Disord. 1995 Apr;17(3):263–275. doi: 10.1002/1098-108x(199504)17:3<263::aid-eat2260170307>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 46.Blackburn GL, Wilson GT, Kanders BS, et al. Weight cycling: the experience of human dieters. Am J Clin Nutr May. 1989;49(5 Suppl):1105–1109. doi: 10.1093/ajcn/49.5.1105. [DOI] [PubMed] [Google Scholar]
- 47.Grabe S, Hyde JS. Ethnicity and body dissatisfaction among women in the United States: A meta-analysis. Psychol Bull. 2006;132:722–640. doi: 10.1037/0033-2909.132.4.622. [DOI] [PubMed] [Google Scholar]


