Abstract
Background
Pediatric stem cell transplant (SCT) is a demanding procedure for children and parents. Interventions to promote positive adjustment of parents in this setting are needed.
Method
171 patient/parent dyads from 4 sites received one of 3 interventions to reduce SCT-related distress: a child intervention with massage and humor therapy, an identical child intervention plus a parent intervention with massage and relaxation/imagery, or standard care. Parents completed weekly self-report measures of distress and positive affect during the acute phase of treatment (weeks −1 through +6), and measures of depression, posttraumatic stress (PTSD), and benefit-finding at baseline and week +24.
Results
No significant differences across treatment arms were observed on repeated measures of parental distress. There was a marginally significant effect of the child intervention on parental positive affect. Over time, parental distress decreased significantly and positive affect increased significantly in all groups. Similarly, there were no significant intervention effects on the global adjustment outcomes of depression, PTSD, and benefit finding. However, reports of depression and PTSD decreased significantly and reports of benefit-finding increased significantly from baseline to week +24 for all groups.
Conclusion
Across all study arms, parent adjustment improved over time, suggesting that parents demonstrate a transient period of moderately elevated distress at the time of their child’s admission for transplant, followed by rapid improved to normative levels of adjustment. Similar to results previously reported for their children, these parents appear resilient to the challenges of transplant.
Keywords: pediatric cancer, stem cell transplant, parent adjustment
A diagnosis of childhood cancer presents a significant adjustment challenge for both children and their families.1–4 Fortunately, advances in medical treatment, including stem cell transplantation (SCT), have contributed to the increased survival rate of children with cancer. However, this high-risk procedure can create significant physical and emotional demands for both children and their parents.5–8
Given that parents of children undergoing SCT can experience increased distress, it is important to consider designing and implementing effective interventions to promote positive adjustment of these parents. Furthermore, it appears that the emotional functioning of parents of children undergoing SCT is closely related to the child’s psychological well-being—not only during active treatment, but after completion of SCT.5 Therefore, implementing effective parent interventions are beneficial in that they may also indirectly promote positive psychosocial functioning in pediatric patients. It has been suggested that parent interventions be implemented prior to, or at the time of admission for SCT, given findings that suggest this to be a particularly distressing period for parents.7 To date, limited research has examined interventions for parents of children with cancer, and in particular, those who have children undergoing SCT. Existing findings suggest that interventions have not significantly impacted parent functioning, but in general, parents report lower levels of distress over time.9,10
Given the lack of research in this area, and the less than optimal methodological rigor that has been utilized to implement interventions for parents of children with cancer11, further implementation and evaluation of randomized, methodologically sound parent interventions are warranted. Ideally, such investigations should utilize repeated measures to gain a better understanding of parent adjustment over the course of transplant.12,13 Therefore, the primary objective of this investigation was to examine the effects of both parent- and child-targeted interventions implemented during transplant hospitalization on parental adjustment, using a repeated measures design.
Grounded in positive psychology, the intervention was focused not only on reducing distress but also on increasing the experience of positive emotions during this potentially stressful event. While the primary goal of the intervention was to decrease distress and improve well-being in children undergoing transplant, we also targeted and assessed intervention effects on parental adjustment. The study included three arms: 1) a child targeted intervention involving massage and humor therapy; 2) the child intervention plus a parent-targeted intervention involving massage and relaxation/imagery; and 3) standard care. We sought to determine if there are additional benefits on parent psychological functioning from a parent intervention above and beyond the intervention provided to their children. The effects of the intervention on child outcomes have been previously reported.14,15 This report focuses on parental outcomes. We hypothesized that parents who receive this health-promotion intervention (in addition to their child’s intervention) during the acute phase of their child’s SCT will show decreased emotional distress and increased positive adjustment in comparison to parents in the child-targeted arm of the intervention or those receiving only standard care.
Method
Participants
Participants were recruited from four major pediatric transplant centers: St. Jude Children’s Research Hospital, The Hospital for Sick Children, Toronto, Children’s Hospital of Philadelphia, and Nationwide Children’s Hospital, Columbus. Patient eligibility criteria included: a) undergoing stem cell or bone marrow transplant (allogeneic or autologous); b) expected hospital stay of ≥ 3 weeks; c) between the ages of 6–18 years; and d) able to speak and read English fluently. Parent eligibility included: a) primarily responsible for caring for the child during his/her hospital stay; b) available to participate throughout the duration of the child’s hospitalization for transplant; and c) ability to speak and read English fluently. Of the 278 patient/parent dyads approached for participation in the study, 242 dyads were eligible for study enrollment. A total of 189 (78.1%) patient/parent dyads initially consented to participate in the investigation, and a final total of 171 completed baseline measures, were randomized to one of the three study arms, and were admitted to the hospital for transplant. A detailed Consort diagram has been previously reported.14 Descriptive statistics for demographic and medical variables are presented in Table 1. In summary, no significant differences were found among intervention arms on any of the medical (i.e., site, type of transplant, diagnostic group), or demographic (i.e., child age, child gender, child race/ethnicity, resident parent) variables. For the parental outcomes presented here, there was an evaluable sample of 167 at baseline with gradual attrition to 97 at week +24. A total of 25 patients died, 11 withdrew (3 withdrew immediately after being randomized to the standard care arm, the remaining 8 withdrew after a period of non-compliance indicating they were no longer interested or felt study procedures were too burdensome), 8 were taken off study for medical reasons (relapse, second transplant), and 22 failed the week +24 assessment. Comparison of baseline scores between those who provided a week +24 observation and those who did not, revealed no significant differences on any of the outcomes reported here.
Table 1.
Demographic and Medical Characteristics of Parents and Child Patients
| Child-Targeted Intervention | Child + Parent Intervention | Standard Care | Total (Across all Study Arms) | p | |
|---|---|---|---|---|---|
|
| |||||
| Child Age years, % (M=12.8, SD=3.9) years, % | |||||
| 6–12 years | 46.6 | 48.2 | 52.6 | 49.1 | .79 |
| >12 years | 53.4 | 51.8 | 47.4 | 50.9 | NS |
|
| |||||
| Gender % | |||||
| Male | 67.2 | 55.4 | 52.9 | 59.1 | .24 NS |
|
| |||||
| Race/Ethnicity % | |||||
| White | 70.7 | 72.3 | 70.2 | 70.7 | .61 |
| Black | 16.5 | 14.3 | 12.3 | 14.6 | NS |
| Hispanic | 5.2 | 3.6 | 7.0 | 5.3 | |
| Asian | 3.4 | 7.1 | 1.8 | 4.1 | |
| Other/Unknown | 5.1 | 1.8 | 8.8 | 5.3 | |
|
| |||||
| Socioeconomic Status % | |||||
| I | 17.2 | 17.9 | 14.0 | 16.4 | .78 |
| II | 39.6 | 33.9 | 35.0 | 36.2 | NS |
| III | 20.7 | 25.0 | 14.0 | 19.8 | |
| IV & V | 15.5 | 12.5 | 22.8 | 16.9 | |
| Unknown | 6.9 | 10.7 | 14.0 | 10.5 | |
|
| |||||
| Resident Parent % | |||||
| Mother | 84.7 | 85.7 | 76.7 | 82.4 | .46 |
| Father | 10.2 | 8.9 | 16.1 | 11.7 | NS |
| Other | 5.1 | 5.4 | 7.1 | 5.8 | |
|
| |||||
| Site % | |||||
| St. Jude | 46.6 | 36.8 | 38.3 | 41.5 | .33 |
| HSC-Torontoo | 15.5 | 26.1 | 31.6 | 23.9 | NS |
| CHOP | 24.1 | 19.6 | 19.3 | 20.5 | |
| NCH-Columbus | 13.8 | 17.5 | 10.7 | 14.0 | |
|
| |||||
| Type of Transplant % | |||||
| Autologous | 10.3 | 21.4 | 24.1 | 18.1 | .35 |
| Allogeneic-matched sibling | 27.6 | 26.8 | 22.8 | 25.7 | NS |
| Allogeneic-other | 62.1 | 51.8 | 52.6 | 56.1 | |
|
| |||||
| Diagnostic Group % | |||||
| ALL | 27.1 | 26.8 | 26.3 | 26.9 | .98 |
| AML | 23.7 | 21.4 | 28.6 | 24.6 | NS |
| Other Leukemia | 10.8 | 17.9 | 12.5 | 13.5 | |
| HD/NHL | 13.6 | 8.9 | 8.7 | 10.5 | |
| Solid Tumor | 12.2 | 12.5 | 12.5 | 12.3 | |
| Nonmalignancy | 12.2 | 12.5 | 10.7 | 11.1 | |
Procedures
Patient-parent dyads were recruited prior to admission for transplant. After informed consent/assent was obtained, parents completed baseline paper-and-pencil questionnaires, and were subsequently randomized (stratified by child age group, site, and type of transplant) to one of the three study arms: a) a child-targeted intervention; b) a child + parent intervention; and c) standard care. The intervention was implemented beginning at admission through week +3 of transplant.
Intervention
Child-Targeted Intervention
Patients in this treatment group were provided with psychoeducation about the benefits of both massage and humor therapy, including ways in which they can increase their experience of positive affect during the SCT process. Patients were scheduled for three massage sessions per week over the course of four weeks (i.e., admission through week +3). Humor therapy consisted of providing a “humor cart” that contained enjoyable items such as videos, books, and games. Scheduled humor sessions involving an interventionist and the patient occurred once per week. In addition, the humor cart was made available to families at least three times per week over the course of four weeks (i.e.,. admission through week +3).
Child + Parent Intervention
This intervention consisted of the child-targeted intervention described above, plus an additional parent intervention. Parents were provided with psychoeducation about how promoting their own well-being (i.e., engaging in massage and relaxation training) may also positively benefit their children. Parents were scheduled for a massage session three times per week for four weeks (i.e., admission through week +3). In addition, parents participated in weekly relaxation training sessions (i.e., admission through week +3) with a member of the research team that promoted strategies such as muscle relaxation, breathing exercises, and guided imagery. Parents were provided with a relaxation tape and player, and were encouraged to engage in relaxation exercises 15–20 minutes daily.
Standard Care
Patient-parent dyads in the standard care arm of the study did not receive any additional intervention beyond the routine, comprehensive services that are provided for families during the SCT process at these major pediatric SCT centers.
Intervention Adherence
As previously described, completion of intervention components was examined as an indicator of intervention adherence.14 A goal of completing 12 massage sessions (i.e., 3 massages over the course of 4 weeks) was established. Results indicated that patients completed an average of 8.8 massage sessions (SD=3.1), and parents completed an average of 7.6 massages (SD=3.2). In summary, the majority of intervention components were successfully completed by patient/parent dyads. The primary reasons for not completing intervention activities included passive refusal or logistical issues that made implementation of an intervention activity difficult.
Measures
Repeated Measures of Acute Adjustment
Several measures were gathered weekly from parents to obtain a longitudinal perspective of parent adjustment during the transplant process. These measures were obtained at the following timepoints: baseline (i.e., time of admission for transplant), Week −1, Week 0, and Week +1 though Week +6.
Profile of Mood States Scale (POMS, Short Form)16
The POMS is an assessment of one’s present mood. Internal consistency for the subscales of the POMS Short Form have been reported as commensurate with those obtained in the original version. In addition, the relationship between the total Mood Disturbance score and the individual subscales on the original and short versions of the POMS have been reported as being greater than .95.17 A 15-item short version utilized in previous SCT studies was administered.7
Perceived Stress Scale (PSS)18
The 14-item PSS is a well-recognized instrument for assessing one’s experience of stress, including the degree to which individuals perceive their lives as uncontrollable, unpredictable, and overwhelming. This instrument has adequate validity and reliability.
Caregiver Burden Scale (CBS19
The CBS contains 14 items that measure the perceived burden of an individual who is providing care to a loved one with a chronic medical illness. Excellent reliability and validity have been reported for this measure.
Positive and Negative Affect Schedule (PANAS)20
The PANAS is a 20-item instrument that measures self-reported positive and negative affect within a specified timeframe. The two subscales have been reported as being uncorrelated, with alpha coefficients ranging from 0.86 to 0.90 for the positive affect scale.20. For this study, only the positive affect subscale was examined.
Global Adjustment Measures Completed at Baseline and Week +24
In addition to the repeated measures of acute adjustment, three measures were administered to assess parent functioning upon admission for the child’s transplant, and 24 weeks following the procedure (Week +24), to assess for symptoms of posttraumatic stress, depression, and benefit finding.
Impact of Events Scale, Revised (IES-R)21
This 22-item measure is used to assess for symptoms of posttraumatic stress disorder (PTSD) and is comprised of three subscales: Intrusion, Avoidance, and Hyperarousal. Adequate internal consistency, concurrent validity, and discriminant validity have been reported for the IES-R among a number of adult populations experiencing various stressors.
Center for Epidemiological Studies Depression Scale (CES-D)22
The CES-D is a commonly used screening measure containing 20 items that assess depressive symptoms in adults during the past week. A score of 16 or higher on this measure is typically used as a cut-off indicative of clinically significant depressive symptomatology.22 Good internal consistency, as well as adequate test-retest reliability, have been reported in community samples of adults.23.
Benefit Finding Scale (BFS)24
The 17-item BFS examines potential positive outcomes that are experienced as a result of enduring a difficult experience. It has been used primarily with adults facing cancer, but can be adapted to any significant stressor.
Data Analyses
The three repeated measures of parental acute distress, POMS, PSS, and CBS were summed into an overall “parental distress” composite score. This decision was made due to the high degree of inter-correlation between the measures and to reduce experiment-wise error. The parental distress score was calculated by computing a simple sum of the scores for each of the three measures as has been done in previous studies.7 Parent reports of positive affect obtained on the PANAS were examined separately. To examine parental distress and positive affect over time, we utilized Generalized Linear Mixed-Effect Models (GLMM) to estimate longitudinal trends across the three study arms: a) Child-only intervention (HPIC); b) child + parent intervention (HPICP); and c) standard care (SC). Parental distress and positive affect were modeled as binomially distributed variables, and therefore a logistic link was employed in the GLMM regressions.25
For the global adjustment outcomes, three mixed between-within effects analyses of variance (ANOVAs) were conducted to determine intervention effects across the study arms on the three measures, IES-R, CES-D, and BFS obtained at baseline and week + 24.
Results
Repeated Parent Adjustment Measures
Acute Parental Distress
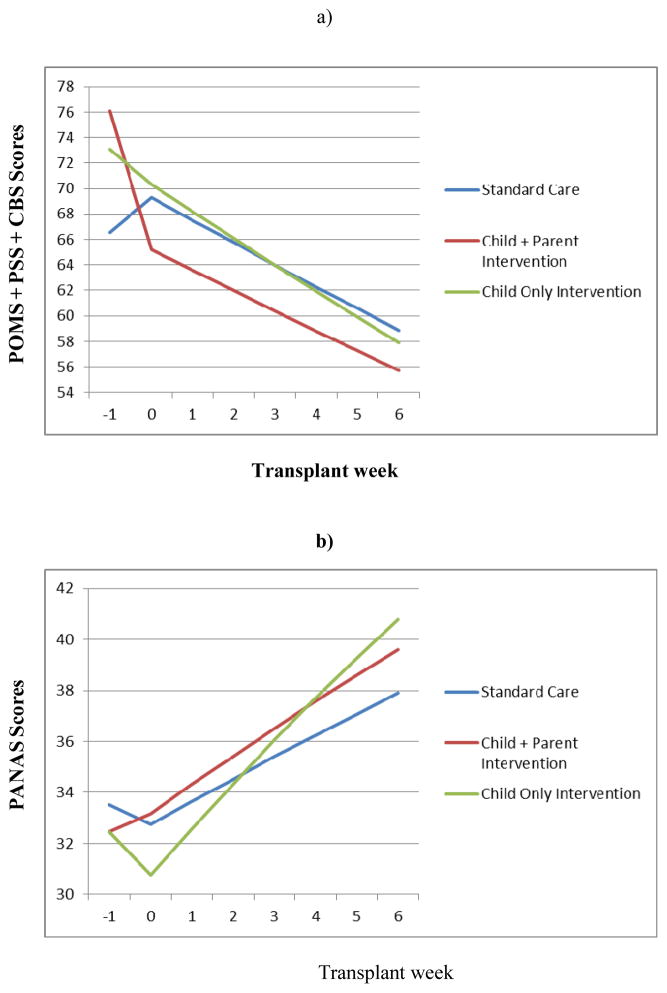
To compare reports of global parental distress (POMS + PSS + CBS) across the three study arms, GLMM with a logistic link was fitted using the SAS 9.2 procedure NLMIXED.25,26 There were no significant differences observed across study arms for the composite measure of global parental distress. The longitudinal trends of parental acute distress were also examined by fitting piecewise-slope GLMM27 with a knot at time 0. Parental distress showed a significant decrease from week 0 to week +6 (p <.01), with a rate of approximately 1.7/week (Figure 1a).
Figure 1.
a) Changes in parent-reported symptoms of distress across the acute phase of transplant from week −1 through week +6, by intervention arm.
b) Changes in parent-reported positive affect across the acute phase of transplant from week −1 through week + 6, by intervention arm.
Positive Affect
Intervention effects on reports of positive affect as measured by the PANAS were also examined using the same analytic approach. No significant differences were observed across study groups at baseline. However, all three groups showed significant increases on the PANAS from week 0 to week +6. The estimated rates are 0.78/, 1.48/week and 0.98/week for the standard care group, HPIC, and HPICP groups, respectively. The rate of increase of positive affect for the HPIC group was significantly greater than that of the control group ( p=0.03), but . not statistically different from that of the HPICP group (p=0.54, Figure 1b).
Parent Adjustment at Baseline and Week +24 Across Study Arms
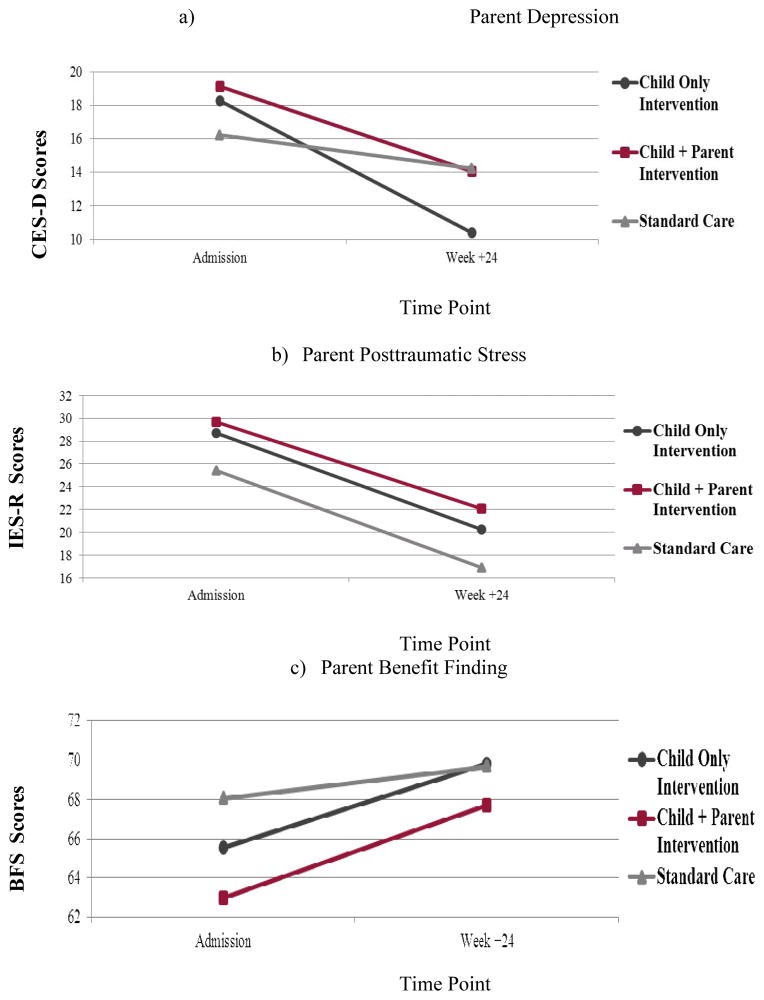
Depression
A 3 (study arm) × 2 (time) mixed effects ANOVA was also used to examine differences in parent depression. Across the entire sample, there was a significant change over time (F =18.3, p <.001), with all groups showing a decline in CES-D depression scores from baseline (M=18.2, SD = 10.8) to week + 24 (M=12.8, SD=11.6). However, there were no significant differences between groups (F= .47, p=.63), and no intervention effect the intervention group by time interaction was not significant (F=1.89, p=.16) (Figure 3b). Descriptively, these data suggest that parents evidence a moderately elevated level of depressive symptoms at baseline, followed by a return to normative levels by week +24.22,23
Posttraumatic Stress
A 3 (study arm) × 2 (time) mixed effects ANOVA was used to examine differences in parent PTSD. Again, there was a significant effect of time (F=27.8, p< .001), whereby parents reported significantly higher symptoms of PTSD at baseline (M=28.3, SD=16.1) in comparison to week +24 (M=20.2, SD=15.0). There was no significant difference between intervention groups (F=.81, p=.45), and the intervention group by time interaction was not significant (F=.04, p=.96), indicating no intervention effect (Figure 2b). Descriptively, the mean score at baseline was higher than that of a comparison group of parents of healthy same-age children from a prior study (M=23.9, SD=17.6).28 But following the decline, mean report of parent PTSD at Week +24 was descriptively lower than the mean reported by the comparison group.
Figure 2.
a) Parental depression scores; b) Parental posttraumatic stress symptoms scores; and c) Parental perceived benefit finding at baseline (admission to SCT), and week +24 by intervention arm.
Benefit Finding
A 3 (study arm) × 2 (time) mixed effects ANOVA was used to examine differences in parent benefit finding. Consistent with the parent PTSD and depression findings, parent reports of benefit finding changed significantly over time (F=12.4, p=.001), with parent reports being significantly higher at week +24 (M=68.9, SD=11.7) in comparison to baseline (M=65.0, SD=11.5). Again, there were no significant group differences (F=.90, p=.02), nor a group by time interaction (F=.80, p=.46, Figure 2c).
Discussion
The primary goal of this investigation was to examine an intervention to promote the positive adjustment of pediatric patients undergoing SCT and their parents. The intervention was designed to increase positive emotions and decrease emotional distress. One study arm contained a parent-targeted intervention utilizing massage therapy and relaxation/imagery to promote positive adjustment. In this analysis, we specifically examined the impact of the interventions on parental outcomes, including acute phase distress and positive affect, and global adjustment outcomes of depression, PTSD, and benefit finding. Contrary to our hypothesis, there were no additional benefits of a parent-targeted intervention beyond that of intervention focused on the child patient. Parents in the child + parent intervention did not differ in distress and adjustment in comparison outcomes in comparison to parents in the child-targeted arm of the study or those receiving standard care only. There were marginally significant improvements noted in parent-reported positive affect in the child-only intervention, and similar, but non-significant increases in parent-reported positive affect in the child + parent intervention relative to the standard care group. These results suggest marginal benefit of intervention on parent adjustment.
Despite the minimal intervention effects on acute adjustment, these results consistently indicated significant improvement across all study arms in parent distress and positive affect over time (from Week 0 to Week +6). Findings were similar for parent reports of more global adjustment outcomes, depression, PTSD, and benefit-finding extending out to week +24. There were no intervention effects, but there was a significant effect of time on each outcome. From baseline to Week +24, parents in all three arms of the study reported statistically significant decreases in depression and PTSD, and increases in benefit finding.
The generally null findings of the intervention are consistent with prior intervention studies, suggesting that parents with children undergoing SCT tend to experience moderate elevations in distress around the time of their child’s admission for SCT, but this distress decreases over time following admission and across the acute phase of SCT.9,10 These findings are also commensurate with investigations that have examined the functioning of parents of children with cancer over time, and suggest that most parents demonstrate heightened psychosocial distress during the early phase of their child’s diagnosis/treatment followed by a return to normative levels of functioning over time.12,29–31
The current findings suggest an adaptive rather than a pathological pattern of parent adjustment, and parallel the results found in the psychosocial functioning of the child patients in this same investigation.14,15 No intervention effect was found for the patients, but similarly, measures of child functioning across all study arms showed significant improvement in psychosocial adjustment over time per both patient and parent report. These findings in both parents and children represent a normative trajectory of adjustment, and serve as an example of the resiliency not only in children undergoing SCT but also their parents. The positive adjustment seen here is striking, since SCT is widely considered the most stressful of treatments in pediatric oncology, and the SCT procedure itself often viewed as a potentially traumatic event.5 The parental findings add to the results of this multisite trial, to suggest that with current levels of supportive care, SCT need not involve significant trauma, lingering distress, or disruption in normal adjustment trajectories for patients or their parents.
There are some potential study limitations that must be considered when interpreting these findings.. The significant attrition during the course of the study decreased the number of parents who completed all self-report measures at all time points, reducing study power to detect smaller effects. Fortunately, there were no differences at baseline between those who completed the study and those who did not, as previously reported.14,15 Another important consideration is the impact that standard care alone has on parents and children undergoing SCT. It appears that all patients in this study benefitted from effective and comprehensive supportive care services. While this is a positive development, it may serve to make detecting benefit above and beyond standard care difficult to document. It should be noted that the participating sites were comprised of large and experienced transplant centers, and may not be representative of all transplant centers, particularly smaller sites that may have fewer resources. Future research can identify what aspects of standard care are most beneficial for promoting the psychosocial functioning of parents of children undergoing SCT. Finally, given the lack of intervention effect, it is worth considering the impact of the intervention longitudinally. While we gathered data from parents through Week +24, it would be helpful to examine the functioning of these parents further out from SCT to determine if intervention effects emerge.
While much of the research in our field focuses on pathological outcomes and risk of maladjustment in children with cancer (including those undergoing SCT) and their parents, these findings highlight that the majority of these patients and parents adjust well when faced with the challenge of significant illness and treatment such as SCT. There has been growing interest in the construct of resilience, and the human capacity to adjust, and even thrive, when faced with adverse or challenging life events.32–34 Given the challenges of SCT, the positive adjustment of parents observed here provide another example of resilience in the face of challenge. Application of resiliency models are also needed to inform our clinical practice with SCT patients and parents, and additional research is necessary that aims to better understand the factors that foster this resiliency.
Acknowledgments
Supported by grant R01 CA60616 from the National Institutes of Health, and by the American Lebanese Syrian Associated Charities (ALSAC)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pai ALH, Greenley RN, Lewandowski A, Drota D, Youngstrom E, Peterson CC. A meta-analytic review of the influence of pediatric cancer on parent and family functioning. J Fam Psychol. 2007;21:407–415. doi: 10.1037/0893-3200.21.3.407. [DOI] [PubMed] [Google Scholar]
- 2.Goldbeck L. Parental coping with the diagnosis of childhood cancer: Gender effects, dissimilarity within couples, and quality of life. Psycho-Oncology. 2001;10:325–335. doi: 10.1002/pon.530. [DOI] [PubMed] [Google Scholar]
- 3.Hildenbrand AK, Clawson KJ, Alderfer MA, Marsac ML. Coping with pediatric cancer: Strategies employed by children and their parents to manage cancer-related stressors during treatment. J Ped Oncol Nurs. 2011;28:344–354. doi: 10.1177/1043454211430823. [DOI] [PubMed] [Google Scholar]
- 4.Manne SL, Hamel KD, Gallell K, Sorgen K, Redd WH. Posttraumatic stress disorder among mothers of pediatric cancer survivors: Diagnosis, comorbidity, and utility of the PTSD checklist as a screening instrument. J Ped Psychol. 1998;23:357–366. doi: 10.1093/jpepsy/23.6.357. [DOI] [PubMed] [Google Scholar]
- 5.Packman W, Weber S, Wallace J, Bugescu N. Psychological effects of hematopoietic SCT on pediatric patients, siblings, and parents: A review. Bone Marrow Transplantation. 2010;45:1134–1146. doi: 10.1038/bmt.2010.74. [DOI] [PubMed] [Google Scholar]
- 6.Barrera M, Atenafu E, Doyle J, Berlin-Romalis D, Hancock K. Differences in mothers’ and fathers’ psychological distress after pediatric SCT: A longitudinal study. Bone Marrow Transplantation. 2011;47:934–939. doi: 10.1038/bmt.2011.206. [DOI] [PubMed] [Google Scholar]
- 7.Phipps S, Dunavant M, Lensing S, Rai SN. Patterns of distress in parents of children undergoing stem cell transplantation. Ped Blood Cancer. 2004;43:267–274. doi: 10.1002/pbc.20101. [DOI] [PubMed] [Google Scholar]
- 8.Phipps S, Dunavant M, Garvie P, Lensing S, Rai SN. Acute health-related quality of life in children undergoing stem cell transplant: I. Descriptive outcomes. Bone Marrow Transplantation. 2002;29:425–434. doi: 10.1038/sj.bmt.1703377. [DOI] [PubMed] [Google Scholar]
- 9.Streisand R, Rodrigue JR, Houch C, Graham-Pole J, Berlant N. Brief report: Parents of children undergoing bone marrow transplantation: Documenting stress and piloting a psychological intervention program. J Ped Psychol. 25:331–337. doi: 10.1093/jpepsy/25.5.331. 200. [DOI] [PubMed] [Google Scholar]
- 10.Hoekstra-Weebers JEHM, Heuvel F, Jaspers JPC, Kamps WA, Klip EC. Brief report: An intervention program for parents of pediatric cancer patients: A randomized controlled trial. J Ped Psychol. 1998;23:207–214. doi: 10.1093/jpepsy/23.3.207. [DOI] [PubMed] [Google Scholar]
- 11.Bougea A, Darviri C, Alexopoulos EC. A systematic review of randomized controlled interventions for parents’ distress in pediatric leukemia. ISRN Oncol. 2011;2011:959247. doi: 10.5402/2011/959247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vrijmoet-Wiersma CM, van Klink JM, Kolk AM, Koopman HM, Ball LM, Maarten ER. Assessment of parental psychological stress in pediatric cancer: A review. J Ped Psychol. 2008;33:694–706. doi: 10.1093/jpepsy/jsn007. [DOI] [PubMed] [Google Scholar]
- 13.Patenaude AF, Kupst MJ. Psychosocial functioning in pediatric cancer. J Ped Psychol. 2005;30:9–27. doi: 10.1093/jpepsy/jsi012. [DOI] [PubMed] [Google Scholar]
- 14.Phipps S, Barrera M, Vannatta K, Xiong X, Doyle JJ, Alderfer MA. Complementary therapies for children undergoing stem cell transplantation. Cancer. 2010;116:3924–3933. doi: 10.1002/cncr.25415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phipps S, Peasant C, Barrera M, Alderfer MA, Huang Q, Vannata K. Resilience in children undergoing stem cell transplantation: Results of a complementary intervention trial. Pediatrics. 2012:e762–770. doi: 10.1542/peds.2011-1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McNair DM, Lorr M, Droppleman LF. Manual, Profile of Mood States. San Diego: Educational and Industrial Testing Services; 1971. [Google Scholar]
- 17.Curran SL, Andrykowski MA, Studts JL. Short form of the Profile of Mood States (POMS-SF). Psychometric information. Psychol Assess. 1995;7:80–83. [Google Scholar]
- 18.Cohen S, Kamarck T, Meermelstein R. A global measure of perceived stress. J Health Soc Beh. 1983;24:385–396. [PubMed] [Google Scholar]
- 19.Poulshock S, Deimling G. Families caring for elders in residence: Issues in the measurement of burden. J Gerontol. 1984;39:230–239. doi: 10.1093/geronj/39.2.230. [DOI] [PubMed] [Google Scholar]
- 20.Watson D, Clark LA, Tellegen A. Development and validation of brief measuresof positive and negative affect: The PANAS scales. J Personal Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 21.Weiss DS, Marmar CR. The Impact of Event Scale-Revised. In: Wilson JP, Keane TM, editors. Assessing Psychological Trauma and PTSD: A Practitioner’s Handbook. New York: Guilford Press; 1997. pp. 399–411. [Google Scholar]
- 22.Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychol Measurem. 1977;1:385–401. [Google Scholar]
- 23.Lesman-Leegte I, Jaarsma T, Coyne JC, Hillege HL, Van Veldhuisen DJ, Sanderman R. Quality of life and depressive symptoms in the elderly: a comparison between patients with heart failure and age- and gender-matched community controls. J Cardiac Fail. 2009;15:17–23. doi: 10.1016/j.cardfail.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 24.Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, Yount SE, McGregor BA, Arena PL, Harris SD, Price AA, Carver CS. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001;20:20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 25.Zhang H, Lu N, Feng C, Thurston SW, Xia Y, Tu XM. On fitting generalized linear mixed-effects models for binary Responses using Different Statistical Packages. Statistics Med. 2011;30:2562–2572. doi: 10.1002/sim.4265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang H, Xia Y, Chen R, Lu N, Tang W, Tu XM. On modeling longitudinal binomial responses: Implications from two dueling paradigms. J Appl Stat. 2011;38:2373–2390. [Google Scholar]
- 27.Cudeck R, Klebe K. Multiphase mixed-effects models for repeated measures data. Psychol Meth. 2002;7:41–63. doi: 10.1037/1082-989x.7.1.41. [DOI] [PubMed] [Google Scholar]
- 28.Jurbergs N, Long A, Ticona L, Phipps S. Symptoms of post-traumatic stress in parents of children with cancer: are they elevated relative to parents of healthy children? J Ped Psychol. 2009;34:4–13. doi: 10.1093/jpepsy/jsm119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dahlquist LM, Czyzewski DI, Jones CL. Parents of children with cancer: A longitudinal study of emotional distress, coping style, and marital adjustment two and twenty months after diagnosis. J Ped Psychol. 1996;21:541–554. doi: 10.1093/jpepsy/21.4.541. [DOI] [PubMed] [Google Scholar]
- 30.Dolgin MJ, Phipps S, Fairclough DL, Sahler OJZ, Askins M, Noll RB, Butler R, Varni JW, Katz ER. Trajectories of adjustment in mothers of children with newly diagnosed cancer: A natural history study. J Ped Psychol. 2007;32:771–782. doi: 10.1093/jpepsy/jsm013. [DOI] [PubMed] [Google Scholar]
- 31.Steele RG, Dreyer ML, Phipps S. Patterns of maternal distress among children with cancer and their association with child emotional and somatic distress. J Ped Psychol. 2004;29:507–518. doi: 10.1093/jpepsy/jsh053. [DOI] [PubMed] [Google Scholar]
- 32.Bonnano GA, Mancini AD. The human capacity to thrive in the face of potential trauma. Pediatrics. 2008;121:369–375. doi: 10.1542/peds.2007-1648. [DOI] [PubMed] [Google Scholar]
- 33.Masten AS. Ordinary magic: resilience processes in development. Am Psychol. 2001;53:227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 34.Bonnano GA, Diminich ED. Annual research review: Positive adjustment to adversity – trajectories of minimal-impact resilience and emergent resilience. J Child Psychol Psychiatr. 2013;54:378–401. doi: 10.1111/jcpp.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]