Abstract
AIM:
The aim of the following study is to compare pregnancy rates between the use of non-temperature and temperature controlled centrifugation on semen preparation technique in intrauterine insemination.
MATERIALS AND METHODS:
The retrospective study was conducted on 671 patients of idiopathic infertility who underwent homologous artificial insemination at Fertility Research Center from the period of January 2007 to September 2012. The couples were randomized into two groups namely, Group A-patients (n = 303) being treated with sperm prepared by using non-temperature controlled centrifuge and Group B-Patients (n = 368) being treated with sperm prepared by temperature (37°C) controlled centrifuge.
RESULTS AND CONCLUSION:
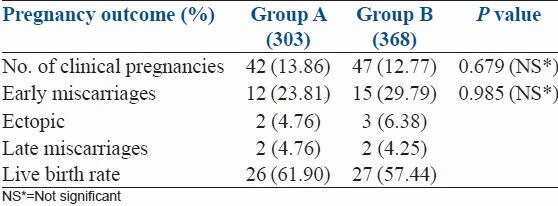
The clinical pregnancy rate Group A was 13.86% and Group B was 12.77%. The clinical pregnancy fetal loss rate between the two groups was 38% and 42% respectively. The delivery rate per transfer was 62% and 58% respectively. No statistically significant difference was found between these two groups.
KEY WORDS: Intrauterine insemination, morphology, pregnancy rate, sperm concentration, sperm motility
INTRODUCTION
Over the last decade there has been a rise in incidence of subfertility among the reproductive age group couples.[1,2] However, modifications in laboratory techniques have helped to improve pregnancy rates in a corresponding manner. Yet new techniques are being continuously evaluated in order to prove their value both in achieving clinical pregnancies as well as being cost-effective for these couples.
Intrauterine insemination (IUI) has been used for the treatment of infertile couples with male factor, ovulatory dysfunction, cervical factor and unexplained infertility often as a first line therapy. The overall success of IUI varies with pregnancy rates ranging from 5% to 20% per cycle. Several prognostic factors for IUI outcome have been proposed, including the age of the women, endometrial thickness, duration of infertility, type of ovarian stimulation, number of inseminations and total number of motile sperm inseminated.[3,4]
Renewed interest in IUI is definitely the result of better washing procedures, enhancing the quality of the initial sperm sample. These washing procedures are necessary to remove prostaglandins, infectious agents, antigenic proteins, non-motile spermatozoa, leukocytes and immature germ cells. Current techniques of sperm preparation for IUI such as swim-up and density gradient require the use of centrifugation to separate the sperm from the seminal plasma. This processing technique provides better sperm quality regarding concentration and motility, which may lead to higher success rates after IUI.[5]
Ever since the advent of sperm processing techniques there has been an ongoing debate pertaining to the maintenance of core temperature considering the natural location of testes. In this regard, came about modification of the conventional centrifuge to include a temperature controlled centrifugation process. The temperature controlled centrifuge has been designed to regulate and subsequently maintain the critical inner chamber temperature at 37°C before, after and during centrifugation. Maintenance of this critical temperature throughout the entire sperm processing procedure helps the sperm to maintain their peak motility and enhanced linearity.
Processing of human spermatozoa during therapeutic procedures usually involves cell exposure to room temperature for different periods of time. Sperm incubation at room temperature regulates cellular mechanisms involved in sperm capacitation and produces a temporary blockage of capacitation related events. Capacitation and acrosome reaction can be achieved in vitro by placing the spermatozoa under defined conditions, which include incubation at body temperature. Previous studies have shown the effect of temperature on cell motility and spontaneous acrosome reaction.[6] Human sperm incubation at room temperature does not allow capacitation, although it does not affect human follicular fluid-induced acrosome reaction in capacitated cells. The blocking effect is overcome when spermatozoa are exposed to 37°C.[7]
The present study has been designed to evaluate the efficacy of non-temperature and temperature controlled centrifugation on semen preparation techniques for IUI and their possible effects on pregnancy outcome in unexplained infertility. The concentration of sperm along with the motility and morphological characteristics of the sperm recovered through the two centrifuges were assessed and compared.
MATERIALS AND METHODS
This retrospective study analyzed data of 671 patients of unexplained infertility, who underwent homologous artificial insemination at our Fertility Research Center from the period of January 2007 to September 2012. All these patients had primary infertility with duration of 2-8 years.
The couples were randomized into two groups namely, Group A – Patients (n = 303) being treated with sperm prepared by using non-temperature controlled centrifuge (Heraeus Biofuge Prima; Thermo Scientific, Germany) and Group B – Patients (n = 368) being treated with sperm prepared by temperature (37°C) controlled centrifuge (Spermfuge SF 800; Shivani Scientific Industries, Mumbai, India).
All the female partners in this study had documented patent fallopian tubes either by hysterosalphingogram and or by laparoscopy. Unexplained infertility was defined as couples who had normal tubal patency, regular ovulation and no cervical factors with regular unprotected intercourse and at least 1 year duration of infertility. The semen parameters were determined by using Makler counting chamber according to World Health organization criteria (2000) of semen analysis. Couples were excluded from the study when the female partner was aged more than 35 years and if there was presence of other known causes of infertility such as male factor, anovulation or immunological factors. The number of cycles is equal to the number of couples.
All patients in both groups underwent ovulation induction by clomiphine citrate with a daily dose of 150 mg administered for 5 days from 5th to 9th days of menstrual cycle. Simultaneously the patients were on Aloes compound (twice a day) from 1st to 21st day of the cycle and T. Progynova (once or twice a day) for 10 days starting from day 5. On the 12th day of the cycle, transvaginal ultrasonography was carried out and 10,000 IU of human chorionic gonadotrophin (human chorionic gonadotropin [hCG]; Life Medicare and Biotech, New Delhi, India) was given when at least 1-3 follicles had reached a diameter of 20 mm.
Semen samples for IUI were collected by masturbation into a sterile wide mouth container after 3 days of sexual abstinence. After liquefaction, semen samples were evaluated using phase contrast microscope (Olympus Medical Systems, Haryana, India). Assessment of semen parameters included sperm concentration per milliliter, percentage of sperm motility and sperm morphology.
The spermatozoa were prepared by the conventional swim-up technique. In both groups, the semen samples after liquefaction were diluted with Whittingham T6 culture media (in-house prepared media supplemented with 10% heat inactivated fetal cord serum) in the ratio of 1:2. The tubes were placed in two centrifuges and then the semen samples were centrifuged for 5 min at 428 × g to separate the seminal plasma from the serum. The supernatant was discarded and the pellet was resuspended in 1 ml of T6 culture media. The sample was again centrifuged for 5 min at 285 × g to remove the cell debris and the supernatant was removed again. The final pellet was gently loosened by resuspension and under-layered in 1 ml of T6 culture media without allowing the sperm pellet and media to mix and incubated at 37°C in 5% CO2 for 30 min. Finally 0.3 ml of the top layer containing highly motile fraction of spermatozoa was aspirated gently in a 1 ml syringe and sperm concentration and motility was ascertained once again.
In both groups, the sperm preparation method was not altered. The sperm parameters before and after preparation were compared. The pre- and post-wash semen characteristics that were reported include sperm concentration, percentage of sperm motility and normal morphology.
The speculum (Cusco's) is gently inserted in the vagina to expose the cervix. The cervix was gently wiped with sterile gauze and Milli Q water. The insemination cannula (Vardhman Medicare, New Delhi, India) was attached to the 1 ml syringe containing the processed sample and the cannula was then gently introduced through the cervical canal. The sperm fraction was then gently expelled and the cannula was gently withdrawn. The patient remained in supine position for 30 min after the insemination. Almost in all the cases, two inseminations were performed on 2 consecutive days in the periovulatory period in order to increase the success rate of IUI. The inseminations were timed 24 h and 48 h post-hCG. A pregnancy test was performed if next mensus was delayed for more than 3 days after the IUI procedure. Clinical pregnancy was confirmed by the presence of an intrauterine gestational sac by transvaginal ultrasonography.
Statistical analysis
All the continuous data's are presented as mean ± standard deviation. Statistical analysis was performed using Independent t-test. Categorical data's were analyzed by Chi-square test, Fisher exact test and was used to determine the predictive power of the sperm parameters (Sperm concentration, motility and sperm morphology) between the temperature and non-temperature controlled centrifuge. The statistical analysis of the data was performed using Statistical Package for the Social Sciences version 14.0 software (Chicago, IL, USA). A P < 0.05 was considered to be statistically significant.
RESULTS
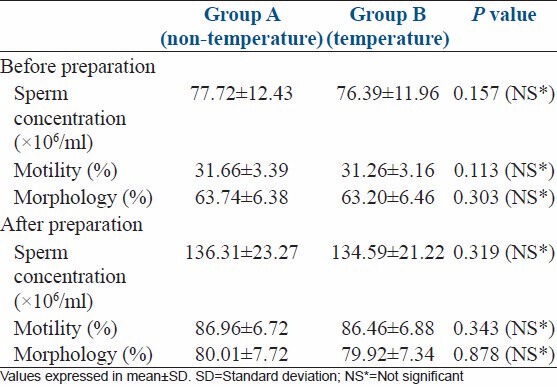
A total of 671 patients of unexplained infertility were assigned to two different groups: Group A (n = 303) had their semen samples prepared by NTC and Group B (n = 368) had their semen samples prepared by TC. The patient's demographic and semen characteristics (pre- and post-washing) of the study population between the two groups are shown in Tables 1 and 2. None of the studied parameters was significantly different between these groups.
Table 1.
Demographic characteristics of the study population between the two groups
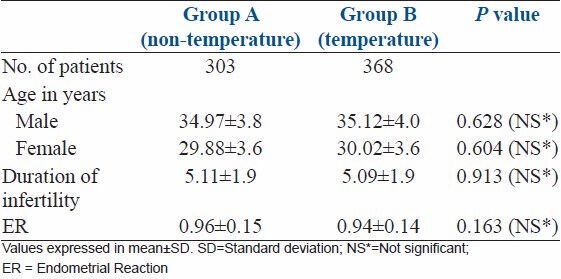
Table 2.
Comparison of sperm parameters in patients before and after sperm preparation
The clinical pregnancy rates and their outcome according to the semen parameters after preparation are summarized in Table 3. None of the variables showed any significant effect between these two groups.
Table 3.
Pregnancy outcome of the intrauterine inseminations between the study groups
DISCUSSION
The nature of this study was to compare the efficacy of non-temperature and temperature controlled centrifugation on semen preparation techniques for IUI and their possible effects on pregnancy outcome in unexplained infertility. The comparison of two types of centrifugation on more or less the same semen count and motility is the only way to detect possible intrinsic differences between the two processes. However, our data showed no significant difference between the sample prepared by using non-temperature and temperature controlled centrifuge.
Unexplained infertility was considered ideal since in the absence of female pathology, the impact of sperm parameters can be studied in a better model. In unexplained infertility, ovarian stimulation and IUI appears to be effective.[8] In a retrospective analysis carried out by,[9] the average IUI pregnancy rate per cycle for unexplained infertility was 18%. Our present study is also comparable with this.
Pregnancy rate after IUI has been evaluated according to indication, age, and duration of infertility in some studies.[4,10,11,12] In our study, there was no significant difference between the two groups with respect to age, duration of infertility and in terms of endometrial thickness.
CONCLUSION
Sperm preparation techniques have added value, safety and also enhanced success rates in IUI treatment cycles. Ovulation induction combined with IUI seems to be the first line of treatment in idiopathic infertility. No significant difference in the pregnancy rate was observed between the non-temperature and temperature controlled centrifuge in terms of sperm concentration, motility and morphology. These results confirm that the sperm preparation technique either at room temperature or at 37°C did not affect the semen parameters and their clinical pregnancy outcome. However, further studies would need to be conducted in order to establish the fact. To the best of our knowledge, this is the first study done specifically to compare the outcomes.
ACKNOWLEDGMENTS
The authors would like to thank Mrs. Sugunaa, Mrs. Srimathi and Mrs. Sajjitha Research Department, G G Hospital for helping in preparing this manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Khalil MR, Rasmussen PE, Erb K, Laursen SB, Rex S, Westergaard LG. Homologous intrauterine insemination. An evaluation of prognostic factors based on a review of 2473 cycles. Acta Obstet Gynecol Scand. 2001;80:74–81. doi: 10.1034/j.1600-0412.2001.800115.x. [DOI] [PubMed] [Google Scholar]
- 2.Wainer R, Albert M, Dorion A, Bailly M, Bergère M, Lombroso R, et al. Influence of the number of motile spermatozoa inseminated and of their morphology on the success of intrauterine insemination. Hum Reprod. 2004;19:2060–5. doi: 10.1093/humrep/deh390. [DOI] [PubMed] [Google Scholar]
- 3.Miller DC, Hollenbeck BK, Smith GD, Randolph JF, Christman GM, Smith YR, et al. Processed total motile sperm count correlates with pregnancy outcome after intrauterine insemination. Urology. 2002;60:497–501. doi: 10.1016/s0090-4295(02)01773-9. [DOI] [PubMed] [Google Scholar]
- 4.Kraemer M, Fillion C, Martin-Pont B, Auger J. Factors influencing human sperm kinematic measurements by the Celltrak computer-assisted sperm analysis system. Hum Reprod. 1998;13:611–9. doi: 10.1093/humrep/13.3.611. [DOI] [PubMed] [Google Scholar]
- 5.Marín-Briggiler CI, Tezón JG, Miranda PV, Vazquez-Levin MH. Effect of incubating human sperm at room temperature on capacitation-related events. Fertil Steril. 2002;77:252–9. doi: 10.1016/s0015-0282(01)02982-x. [DOI] [PubMed] [Google Scholar]
- 6.Arici A, Byrd W, Bradshaw K, Kutteh WH, Marshburn P, Carr BR. Evaluation of clomiphene citrate and human chorionic gonadotropin treatment: A prospective, randomized, crossover study during intrauterine insemination cycles. Fertil Steril. 1994;61:314–8. doi: 10.1016/s0015-0282(16)56524-8. [DOI] [PubMed] [Google Scholar]
- 7.Nuojua-Huttunen S, Tomas C, Bloigu R, Tuomivaara L, Martikainen H. Intrauterine insemination treatment in subfertility: An analysis of factors affecting outcome. Hum Reprod. 1999;14:698–703. doi: 10.1093/humrep/14.3.698. [DOI] [PubMed] [Google Scholar]
- 8.van der Westerlaken LA, Naaktgeboren N, Helmerhorst FM. Evaluation of pregnancy rates after intrauterine insemination according to indication, age, and sperm parameters. J Assist Reprod Genet. 1998;15:359–64. doi: 10.1023/A:1022576831691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao Y, Vlahos N, Wyncott D, Petrella C, Garcia J, Zacur H, et al. Impact of semen characteristics on the success of intrauterine insemination. J Assist Reprod Genet. 2004;21:143–8. doi: 10.1023/B:JARG.0000031246.76666.f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Badawy A, Elnashar A, Eltotongy M. Effect of sperm morphology and number on success of intrauterine insemination. Fertil Steril. 2009;91:777–81. doi: 10.1016/j.fertnstert.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Data, D.2010.“Infertility in rise”, India Today. 2010. Jul, [Accessed on 19.02.2011]. http://indiatoday.intoday.in/site/story/103037/cover-story/infertility-on-the-rise.html?page=1 .
- 12.Sharmistha Dey. 2010. Infertility rises at alarming pace in India, English.news.cn. 2010. Jul, http://http://news.xinhuanet.com/english2010/world/2010-07/16/c_111963155.htm .


