Abstract
AIMS:
Pregnancies achieved by in vitro fertilization (IVF) are at increased risk of adverse outcome. The main objective of this study was to evaluate the predictive value of β-human chorionic gonadotrophin (β-HCG) and age of the patient for the successful outcome in IVF.
MATERIALS AND METHODS:
A retrospective study was done in 139 pregnancies after IVF at single IVF center from June 2007 to July 2012. The age of the patient and initial serum values of β-HCG on day 14 of embryo transfer were correlated with ongoing pregnancy (>12 weeks gestation).
RESULTS:
The β-HCG level on day 14 of more than 347 mIU/ml has a sensitivity of 72.2% and specificity of 73.6% in prediction of pregnancy beyond 12 weeks period of gestation. Positive likelihood ratio (LR) is 2.74 and negative LR is 0.37, (receiver operating characteristic area = 0.79).
DISCUSSION:
In IVF cycles, there is a lot of stress on the couples while the cycle is going on. There was a positive correlation between the higher values of early serum β-HCG levels and ongoing pregnancy. Hence, it can be used as an independent predictor of a successful outcome of IVF cycle.
CONCLUSION:
We concluded from our study that early serum β-HCG can be used as a predictor of a successful outcome in IVF.
KEY WORDS: Age, ongoing pregnancy, prediction, serum marker
INTRODUCTION
Early pregnancy loss such as biochemical pregnancy and spontaneous abortion are common during the first trimester.[1] Pregnancies achieved by in vitro fertilization (IVF) are at increased risk of adverse outcome as compared with natural pregnancies.[2] It is important to predict the complicated and poor pregnancy outcome for both treating clinician and the couple undergoing IVF. Thus, there is a need to have some serum markers, which can be used as early predictors so as to aid in counseling and management of the patient.
Serum human chorionic gonadotrophin (HCG) levels after 2 weeks of embryo transfer is a reliable marker to predict the pregnancy outcome in patients of IVF.[3] It is helpful in assessing the continuation of pregnancy even before the ultrasonography (USG). The ultrasound shows the gestational sac after 3rd week of embryo transfer (ET). The fetal cardiac activity which appears at 5th weeks of gestation on transvaginal ultrasound also can help to predict the outcome. However, the period between the first pregnancy test and a viable pregnancy on the ultrasound is extremely stressful for the couple awaiting the result of IVF. The studies have also shown that there is a direct correlation between the anxiety, stress and poor IVF outcome.[4] If we have some serum marker, which can predict IVF outcome early would be of great help to put both patient and treating physician at ease. The measurement of serum HCG levels on day 14 of ET has good sensitivity and specificity to predict pregnancy outcome in terms of viable and non-viable pregnancies.[5,6,7]
In the present study, the main objective was to investigate the role of day 14 serum HCG as a predictor of pregnancy outcome in patients undergoing IVF. The ongoing pregnancy was taken as those, which continued beyond 12 weeks of gestation. The early pregnancy loss included biochemical pregnancy, blighted ovum and ectopic pregnancy and missed abortion.
MATERIALS AND METHODS
A retrospective data analysis was performed for all IVF cycles completed at the study center from June 2007 to July 2012. As it was a retrospective analysis of the data, ethical approval was not required. The IVF cycles varied in the stimulation protocol used, based on physician preference, patient and clinical scenario. Only cycles utilizing fresh multi-cell embryos (day 3) or blastocysts (day 5) were considered. As part of the study center's routine protocol, serum quantitative β-HCG concentrations are taken on days 14 after embryo transfer. If the day-14 β-HCG test is positive, a second β-HCG concentration is taken 48 h later (day 16), in part to assist in predicting a viable intrauterine pregnancy or to aid in evaluating for a possible ectopic pregnancy. An ultrasound was then performed at 6-7 weeks' gestational age to verify cardiac activity and number of gestational sacs followed by a repeat scan at 12 weeks of gestation to see the ongoing pregnancy and to rule out missed abortion. Often additional β-HCG concentrations were drawn according to physician and patient desire for reassurance or to follow a falling concentration. An ongoing pregnancy for this study was defined as one which progressed at least 12 weeks gestation with the presence of fetal cardiac activity on ultrasound. Pregnancies defined as not ongoing were ectopic pregnancies and those that had falling β-HCG concentrations, which ultimately became negative, an empty gestational sac on ultrasound (anembryonic) or a fetal pole with no cardiac activity visualized (missed abortion). Multiple gestations were defined by having more than one embryo with cardiac activity.
Serum HCG level was measured with a chemiluminescent microparticle immunoassay for total β-HCG. The measuring range for HCG was 0.0-15,000 mIU/mL. Establishment of pregnancy was defined by an HCG level above 10 IU/L. Further classification of pregnancy outcomes was as follows: Chemical pregnancy was defined as pregnancy detected by HCG measurement without any gestational sac seen on ultrasound; ongoing pregnancy was defined as progression beyond 12 weeks' gestation.
Data from 171 women was analyzed with SPSS (Statistical Package for Social Sciences) version 12. The Mann-Whitney U-test was used for comparing continuous variables between groups. To assess the predictive accuracy of hormonal levels, receiver operating characteristic (ROC) curves and comparison of ROC curves were used. P < 0.05 was considered as statistically significant.
RESULTS
Pregnancy outcomes were followed in the IVF cycles using fresh embryos or blastocysts performed from June 2007 to July 2012. There were 171 pregnancies as a result of IVF during the above mentioned period, defined by a positive β-HCG on day-14 following embryo transfer. Because of incomplete data or non-uniform β-HCG analysis (i.e., samples not drawn on days 14 or 16 post ET), 32 cycles were excluded from the study. In all, 139 patients yielding pregnancies were included in the final analysis. The indications for IVF were tubal factor infertility (n = 75), unexplained infertility (n = 23), endometriosis (n = 17), male factor infertility (n = 35) and advanced maternal age (n = 33). The correlation of day 14 serum β-HCG levels and the age of patients with the ongoing pregnancy were evaluated in the present study. Out of 139 total pregnancies, there were 14 biochemical pregnancies (no gestational sac on ultrasound but only HCG >10 mIU/ml. There were five ectopic pregnancies and 13 missed abortions and seven spontaneous abortions. Patients were assigned two groups on the basis of continuation of pregnancy or first trimester loss for final analysis of the data.
Group I: Patients with ongoing pregnancy >12 weeks on USG (n = 100).
Group II: Patients without ongoing pregnancy (n = 39).
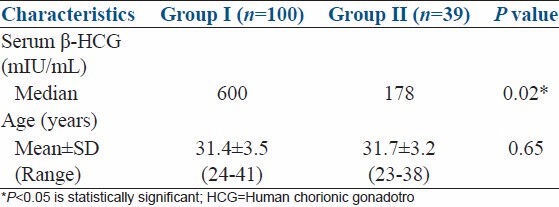
The value of β-HCG levels ranged from 9.7 mIU/ml to 4800 mIU/ml in the present study. The serum β-HCG levels were compared between the two groups using Mann-Whitney test as shown in Table 1. The median serum β-HCG levels in Group I (pregnancies beyond 12 weeks period of gestation) was 600 mIU/ml, whereas the median serum β-HCG levels in Group II (pregnancies less than 12 weeks period of gestation) was 178 mIU/ml. The difference between the two groups was statistically significant, P < 0.05. Hence, the initial β-HCG levels were statistically significantly higher in pregnancies that reached the ≥12 weeks period of gestation than those ≤12 week's period of gestation.
Table 1.
Comparison of serum β-HCG and age between two groups
When the cut-off value of β-HCG is taken as 347 mIU/ml then the sensitivity is 72.2% and specificity is 73.6% in prediction of pregnancy beyond 12 weeks period of gestation. Positive likelihood ratio (LR) is 2.74 for ongoing pregnancy and negative LR is 0.37, (ROC area = 0.79). The graph in Figure 1 shows the correlation of β-HCG and ongoing pregnancy.
Figure 1.
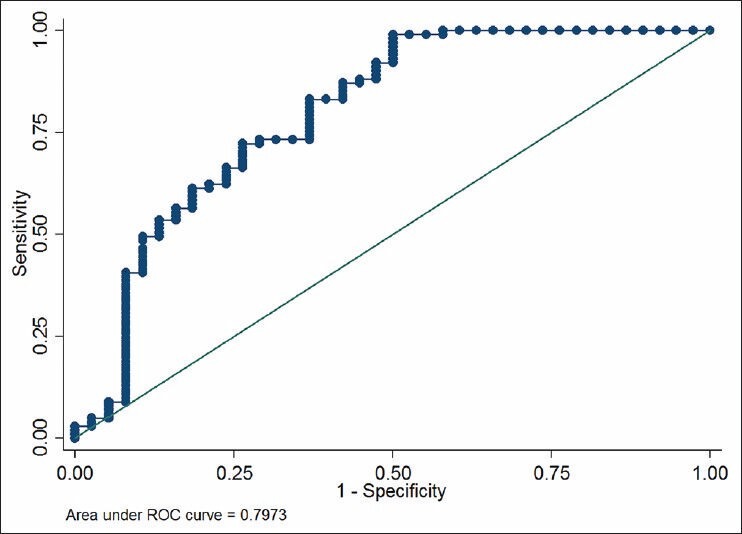
Graph showing receiver operating characteristic curve
The mean age in Group I was 31.4 ± 3.5 years (range: 24-41) and the mean age in Group II was 31.7 ± 3.2 years (range: 23-38), which is not significantly different [Table 1]. Hence, there was no correlation found between age and rate of ongoing pregnancy in the present study.
DISCUSSION
In IVF cycles, there is a lot of stress on the couples while the cycle is going on. The period after the first pregnancy test and before ultrasound shows a viable pregnancy is another burden to bear with. There has to be some serum marker or test, which can predict the pregnancy outcome to relieve the tension of the couple and also the treating clinician. Previously, people have done studies on initial serum HCG levels on day 16 of ET, serum progesterone levels and inhibin A levels to predict the outcome in IVF cycles.[8] There has been published data on serum HCG as a predictor of pregnancy outcome from the western countries.[5,6] We present our data from the developing country in the Asian population. This is a retrospective study analyzing data in 139 patients with IVF conception. In the present study, we investigated serum β-HCG levels and age to predict the pregnancy outcome in patients undergoing IVF at the earliest stage. We measured serum HCG levels at 14 days post ET in all patients. The study found that the higher values of initial serum β-HCG levels were associated with good pregnancy outcome and those pregnancies were likely to continue beyond 12 weeks. The sensitivity of serum HCG levels to predict ongoing pregnancy was 72.2% and sensitivity was 73.6% when the initial value was taken as 347 mIU/ml. In the present study, positive LR is 2.74 for ongoing pregnancy and negative LR is 0.37, (ROC area = 0.79). Previous studies have taken a cut-off value of 50 mIU/ml with a sensitivity and specificity of 75% and 81%, respectively.[9] The positive predictive value of HCG at this cut-off level was around 50% and its negative predictive value was 93% in those studies. HCG represents the functional activity of placental trophoblastic tissue and the low levels are associated with early pregnancy loss or poor outcome.
In the present study, we did not found any correlation between age and pregnancy outcome while one of the study in the literature shows poor pregnancy outcome with the advanced age of the patient. That study cited that age is inversely proportional to the chances of viable pregnancy in IVF patients.[10] The present study shows that initial serum β-HCG can be taken as the single best predictor of pregnancy outcome in patients undergoing IVF. The merit of this study is that it included patients at a single IVF center and the sample size is also large enough to represent the population.
CONCLUSION
We concluded from our study that early serum β-HCG can be used as single best predictor of successful pregnancy outcome in IVF.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Siddiqi TA, Caligaris JT, Miodovnik M, Holroyde JC, Mimouni F. Rate of spontaneous abortion after first trimester sonographic demonstration of fetal cardiac activity. Am J Perinatol. 1988;5:1–4. doi: 10.1055/s-2007-999640. [DOI] [PubMed] [Google Scholar]
- 2.Tummers P, De Sutter P, Dhont M. Risk of spontaneous abortion in singleton and twin pregnancies after IVF/ICSI. Hum Reprod. 2003;18:1720–3. doi: 10.1093/humrep/deg308. [DOI] [PubMed] [Google Scholar]
- 3.Homan G, Brown S, Moran J, Homan S, Kerin J. Human chorionic gonadotropin as a predictor of outcome in assisted reproductive technology pregnancies. Fertil Steril. 2000;73:270–4. doi: 10.1016/s0015-0282(99)00512-9. [DOI] [PubMed] [Google Scholar]
- 4.Klonoff-Cohen H, Chu E, Natarajan L, Sieber W. A prospective study of stress among women undergoing in vitro fertilization or gamete intrafallopian transfer. Fertil Steril. 2001;76:675–87. doi: 10.1016/s0015-0282(01)02008-8. [DOI] [PubMed] [Google Scholar]
- 5.Ochsenkühn R, Arzberger A, von Schönfeldt V, Engel J, Thaler CJ, Noss U. Predictive value of early serum beta-hCG levels after single blastocyst transfer. Acta Obstet Gynecol Scand. 2009;88:1382–8. doi: 10.3109/00016340903322743. [DOI] [PubMed] [Google Scholar]
- 6.Poikkeus P, Hiilesmaa V, Tiitinen A. Serum HCG 12 days after embryo transfer in predicting pregnancy outcome. Hum Reprod. 2002;17:1901–5. doi: 10.1093/humrep/17.7.1901. [DOI] [PubMed] [Google Scholar]
- 7.Papageorgiou TC, Leondires MP, Miller BT, Chang AS, Armstrong AB, Scott LA, et al. Human chorionic gonadotropin levels after blastocyst transfer are highly predictive of pregnancy outcome. Fertil Steril. 2001;76:981–7. doi: 10.1016/s0015-0282(01)02840-0. [DOI] [PubMed] [Google Scholar]
- 8.Kim JH, Shin MS, Yi G, Jee BC, Lee JR, Suh CS, et al. Serum biomarkers for predicting pregnancy outcome in women undergoing IVF: Human chorionic gonadotropin, progesterone, and inhibin A level at 11 days post-ET. Clin Exp Reprod Med. 2012;39:28–32. doi: 10.5653/cerm.2012.39.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Urbancsek J, Hauzman E, Fedorcsák P, Halmos A, Dévényi N, Papp Z. Serum human chorionic gonadotropin measurements may predict pregnancy outcome and multiple gestation after in vitro fertilization. Fertil Steril. 2002;78:540–2. doi: 10.1016/s0015-0282(02)03278-8. [DOI] [PubMed] [Google Scholar]
- 10.McCoy TW, Nakajima ST, Bohler HC., Jr Age and a single day-14 beta-HCG can predict ongoing pregnancy following IVF. Reprod Biomed Online. 2009;19:114–20. doi: 10.1016/s1472-6483(10)60054-5. [DOI] [PubMed] [Google Scholar]


