Abstract
Background:
The correlation of metabolic syndrome and migraine headache was evaluated in some previous studies. However there is no study that compared the prevalence of metabolic syndrome in the patients with and without migraine. Control of coincidental factors such as metabolic syndrome reduces therapeutic resistance in migrainous patients. The aim of this study was to compare prevalence of metabolic syndrome in patients with and without migraine headache.
Materials and Methods:
200 migrainous patients diagnosed according to International Headache Society and 200 healthy controls without migraine enrolled in this study. Metabolic syndrome was diagnosed according to ATP III criteria in these two groups and compared with each other.
Results:
In this study, 17% (34) of migrainous patients and 15% (30) of healthy control without migraine had metabolic syndrome. (P = 0.585). Of the metabolic syndrome components, body mass index (P = 0.05) and waist circumference in migrainous (P = 0.03) were significantly more frequent.
Conclusion:
Our results demonstrate that metabolic syndrome and migraine headache had not significant correlation; however, higher body mass index and waist circumference as metabolic syndrome components had correlated with migraine headache.
Keywords: Metabolic syndrome, migraine, insulin resistance
INTRODUCTION
Migraine is an episodic headache with complicated and unknown pathophysiology.[1,2] Several studies showed that general and environmental factors are important pathophysiologic factor in migrainous.[3] The overall prevalence of migraine is 5-15%.[4,5,6] Migraine effects on the quality of life of the patients[7] and so prevention of migraine attacks is the purpose of lots of studies.[8] Some studies evaluate the correlation of metabolism with migraine headache by the goal of finding a way for preventing migraine attacks.[9]
Some studies were evaluated the correlation between environmental factors such as diabetes and obesity with migraine headache.[10,12] In a cohort study in 2012, no association was found between migraine and diabetes type 2.[11] Nevertheless, in another cross-sectional study, conflicting results were reported. Some of these studies demonstrate high prevalence of migraine in patients with diabetes.[12,13,14,15,16]
Diabetes and obesity are components of metabolic syndrome. Metabolic syndrome consists of diabetes, dyslipidemia, obesity, and hypertension.[8] Insulin resistance is an important part of the metabolic syndrome and it is a prognostic factor for developing cardiovascular disease and stroke in patients with metabolic syndrome.[17,18,19,20,21,22] The prevalence of metabolic syndrome in the west of Iran was reported 23.7% (24.4% of women and in 23.1% of men).[23] Guldiken et al reported that 19.5% of the patients with metabolic syndrome had migraine headache.[2] In another study, 31.9% of the migraine patients had metabolic syndrome.[24] The relationship between metabolic syndrome and migraine headache is still obscure.[2] Comparison of the prevalence of metabolic syndrome in patients with migraine headache and people without migraine was not done till now and also this comparison will help to find out if there is any direct correlation between migraine and metabolic syndrome or not.
Migraine has a complex mechanism and its relation with some coincidental factors such as stress and obesity were evaluated in some studies. Recognition of coincidental factors with migraine helps to control it better and reduce some therapeutic resistance in migrainous and also help to recognize the pathophysiology of migraine.
The aim of our study is to evaluate the prevalence of metabolic syndrome in patients with and without migraine headache.
MATERIALS AND METHODS
This was a case–control study. We consecutively recruited migrainous patients from the neurology outpatient service of the Isfahan Al Zahra hospital from 2011 until 2013 with the research project number of 290032. The diagnosis of migraine was based on International Headache Society Criteria.[25] In migrainous, characteristics of the headache such as location, duration, severity, trigger factors, and aura were ascertained, and the blood pressure level, anthropometric_measurements (weight, height, and waist circumference), body mass index (BMI), lipid profile, and fasting glucose level were measured. Severity of headache was evaluated according to the VAS scale between 0 and 10. We evaluated associated symptoms of patients with migraine headache such as nausea, vomiting, photophobia, and phonophobia and also migraine trigger factors were inquired from the questionnaire. The questionnaire consisted of some exogenous factors such as insomnia, starvation, menstruation, hypersomnia, depression, odor, light, cigarette, climate changes, cough and sneeze, and food (such as alcohol, tee, coffee, spice, vegetables, fatty food, sauce, onion, and citrus).
The control group was selected randomly from healthy subject by matched sex and age in a multiple district of Isfahan according to coverage of the health center. In this group, blood pressure level, anthropometric measurements (weight, height, waist circumference or WC), body mass index (BMI), lipid profile, and fasting glucose level were measured.
Diagnosis of metabolic syndrome in these 2 groups was based on adult treatment panel (ATP) III criteria,[26] according to which three of the following criteria were needed:
1. Central obesity: Waist circumference >102 cm in males and 88 cm in females.
2. Hypertriglyceridemia >150 mg/dl or on specific medication.
3. Low HDL cholesterol <40 mg/dl in males and <50 mg/dl in females.
4. Hypertension: Blood pressure >130 systolic or >85 mm Hg diastolic or specific medication.
5. Fasting plasma glucose >100 mg/dl or on specific medication or previously diagnosed type 2 diabetes.
The prevalence of metabolic syndrome in the patients with migraine headache and people without migraine headache was compared by using x2. The variables were considered significant if p value was <0.05. The statistical analysis was done using SPSS 16 version software.
RESULTS
A total of 200 migrainous patients and 200 healthy people without migraine were evaluated in this study. Demographic characteristics of the migrainous and control group were shown in Table 1.
Table 1.
Demographic characteristics of the migrainous patients and control group
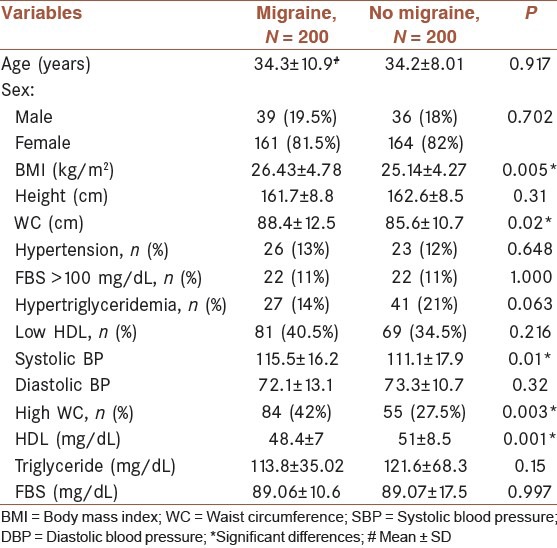
On the basis of the results shown in Table 1, high WC and BMI as the components of metabolic syndrome in the group of migrainous were more frequent than the control group (P = 0.003 and 0.005, respectively).
As shown in Table 1, systolic blood pressure and the mean HDL had also significant differences between the two groups. Migrainous had higher levels of systolic blood pressure and lower mean HDL.
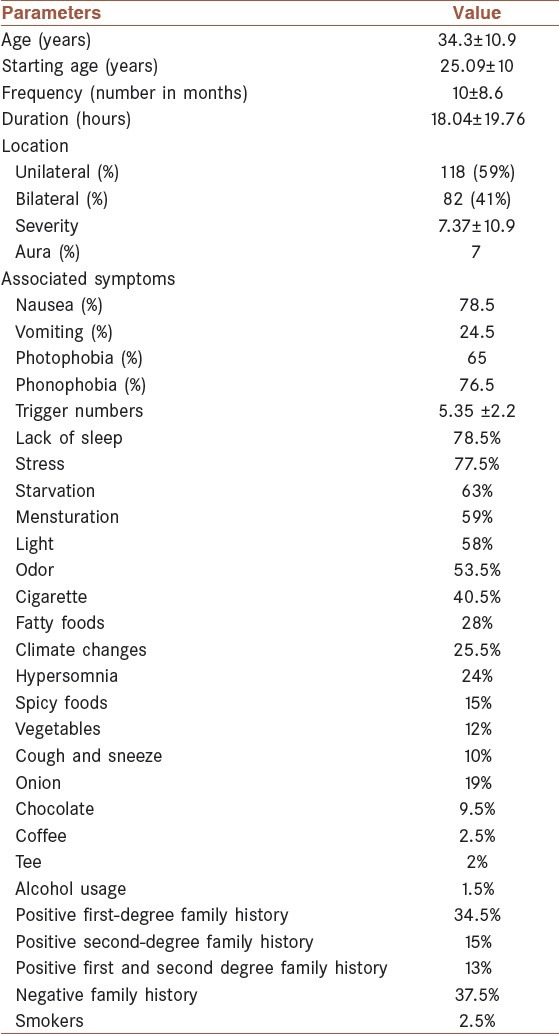
Characteristics of migraine headache in migrainous were shown in Table 2.
Table 2.
Characteristics of migraine headache
In the group of migrainous patients, 34 (17%) and in the control group 30 (15%) persons had metabolic syndrome.
There was no significant difference in metabolic syndrome prevalence between groups (P = 0.585). Anthropometric measurements and metabolic syndrome components were compared between the migrainous patients and control group with metabolic syndrome [Table 3].
Table 3.
Comparison of metabolic syndrome components between the case and control group with metabolic syndrome
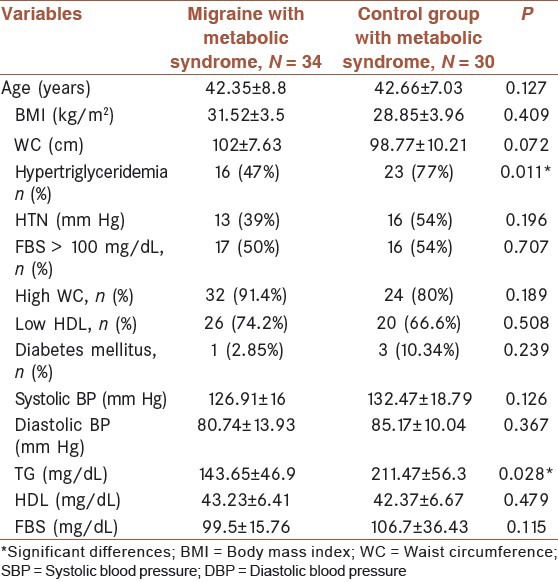
Hypertriglyceridemia was more frequent in the control group with metabolic syndrome than the migrainous patients with metabolic syndrome (P = 0.011).
DISCUSSION
In this study, metabolic syndrome frequency had not significant difference between migrainous and control groups. In our study, 17% of patients with migraine and 15% of patients without migraine had metabolic syndrome. Migraine patients were significantly more obese and had higher levels of WC than the control group, but no relation found between metabolic syndrome and migraine. Hypertriglyceridemia was more frequent in the control group with metabolic syndrome than the migrainous patients with metabolic syndrome.
Guldiken et al evaluated migraine prevalence in patients with metabolic syndrome and reported that 19.5% of patients with metabolic syndrome had migraine headache. According to Guldiken et al, the metabolic syndrome components were found more frequent in migraine.[2]
However, Saanjeev et al evaluated frequency of metabolic syndrome and insulin resistance in migraine and reported that migraine was associated with metabolic syndrome in 31.9% and insulin resistance in 11.1% patients.[24] Bigal et al showed that obesity was associated with headache frequency, but metabolic syndrome frequency was not studied.[27]
To the best of our knowledge, this is the first study considering the control group as a scale for comparing frequency of metabolic syndrome in migrainous patients. On the basis of the results of this study, it seems that metabolic syndrome cannot be considered as an etiologic factor for migraine headache. Some components of metabolic syndrome such as high BMI and high WC were significantly more frequent in migraine headache, but no correlation was found with metabolic syndrome and migraine. Migraine patients were more obese than the control group. Several general population group studies have shown a clear association between obesity and migraine in the reproductive age group.[28,29,30] Shengyuan et al reported that migraine prevalence was significantly raised in the morbidly obese group.[31]
Several of the inflammatory mediators that are increased in obese individuals are important in migraine pathophysiology, including interleukins and calcitonin gene-related peptide (CGRP). These mediators may increase the frequency, severity, and duration of migraine attacks.[27]
Correlation of hyperlipidemia and migraine was evaluated in a study and showed that hypertriglyceridemia and hypercholesterolemia were more frequent in migraineurs. Conversely, low HDL-C was less frequent among the patients compared with nonmigraineurs.[32] In this study, hypertriglyceridemia and low HDL according to the definition of ATPIII criteria were not significantly frequent in the group of migrainous, but the mean HDL had significant differences and the group of migrainous had lower levels of HDL. The comparison of migrainous with metabolic syndrome and the control group with metabolic syndrome showed that hypertriglyceridemia was more frequent in the control group with metabolic syndrome.
In conclusion, this study showed that metabolic syndrome and migraine headache had not significant correlation; however, higher body mass index and waist circumference as metabolic syndrome components had correlated with migraine headache. Future studies with larger sample size are needed to confirm this hypothesis.
ACKNOWLEDGMENTS
The authors wish to acknowledge the support of Isfahan University of Medical Sciences.
Footnotes
Source of Support: Isfahan university of Medical science
Conflict of Interest: Migraine Headache
REFERENCES
- 1.Sonbolestan SA, Heshmat K, Javanmard SH, Saadatnia M. Efficacy of Enalapril in Migraine Prophylaxis: A Randomized, Double-blind, Placebo-controlled Trial. Int J Prev Med. 2013;4:72–7. [PMC free article] [PubMed] [Google Scholar]
- 2.Guldiken B, Guldiken S, Taskiran B, Koc G, Turgut N, Kabayel L, et al. Migraine in metabolic syndrome. Neurologist. 2009;15:55–8. doi: 10.1097/NRL.0b013e31817781b6. [DOI] [PubMed] [Google Scholar]
- 3.Horev A, Wirguin I, Lantsberg L, Ifergane G. A high incidence of migraine with aura among morbidly obese women. Headache. 2005;5:936–8. doi: 10.1111/j.1526-4610.2005.05162.x. [DOI] [PubMed] [Google Scholar]
- 4.Robbins MS, Lipton RB. The epidemiology of primary headache disorder. Semin Neurol. 2010;30:107–19. doi: 10.1055/s-0030-1249220. [DOI] [PubMed] [Google Scholar]
- 5.Brennum J, Brinck T, Schriver L, Wanscher B, Soelberg Sørensen P, Tfelt-Hansen P, et al. Sumatriptan has no clinically relevant effect in the treatment of episodic tension type headache. Eur J Neurol. 1996;3:23–8. [Google Scholar]
- 6.Stang PE, Carson AP, Rose KM, Mo J, Ephross SA, Shahar E, et al. Headache, cerebrovascular symptoms, and stroke: The atherosclerosis risk in communities study. Neurology. 2005;64:1573–7. doi: 10.1212/01.WNL.0000158326.31368.04. [DOI] [PubMed] [Google Scholar]
- 7.Stefane T, Napoleão AA, Sousa FA, Hortense P. Influence of treatments for migraine on quality of life: Literature integrative review. Rev Bras Enferm. 2012;65:353–60. doi: 10.1590/s0034-71672012000200023. [DOI] [PubMed] [Google Scholar]
- 8.Takeshima T. Metabolic syndrome and prevention of migraine headache. Brain Nerve. 2009;61:1143–53. [PubMed] [Google Scholar]
- 9.Casucci G, Villani V, Cologno D, D’Onofrio F. Migraine and metabolism. Neurol Sci. 2012;1:S81–5. doi: 10.1007/s10072-012-1047-4. [DOI] [PubMed] [Google Scholar]
- 10.Khorvash F, Mottaghi T, Askari G, Maracy MR, Ghiasvand R, Maghsoudi Z, et al. The Association Between Serum Vitamin D Levels with General and Abdominal Obesity among Patients with Migraine. Int J Prev Med. 2013;4:s313–7. [PMC free article] [PubMed] [Google Scholar]
- 11.Cook NR, Benseñor IM, Lotufo PA, Lee IM, Skerrett PJ, Chown MJ, et al. Migraine and coronary heart disease in women and men. Headache. 2002;42:715–27. doi: 10.1046/j.1526-4610.2002.02173.x. [DOI] [PubMed] [Google Scholar]
- 12.Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA. 2006;296:283–91. doi: 10.1001/jama.296.3.283. [DOI] [PubMed] [Google Scholar]
- 13.Burch RC, Rist PM, Winter AC, Buring JE, Pradhan AD, Loder EW, et al. Migraine and risk of incident diabetes in women: A prospective study. Cephalalgia. 2012;32:991–7. doi: 10.1177/0333102412453954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davey G, Sedgwick P, Maier W, Visick G, Strachan DP, Anderson HR. Association between migraine and asthma: Matched case-control study. Br J Gen Pract. 2002;52:723–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Split W, Szydlowska M. Headaches in non-insulindependent diabetes mellitus. Funct Neurol. 1997;12:327–32. [PubMed] [Google Scholar]
- 16.Sillanpaa M, Aro H. Headache in teenagers: Comorbidity and prognosis. Funct Neurol. 2000;15(Suppl 3):116–21. [PubMed] [Google Scholar]
- 17.St-Pierre AC, Cantin B, Mauriège P, Bergeron J, Dagenais GR, Després JP, et al. Insulin resistance syndrome, body mass index and the risk of ischemic heart disease. CMAJ. 2005;172:1301–5. doi: 10.1503/cmaj.1040834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sattar N, Scherbakova O, Ford I, O’Reilly DS, Stanley A, Forrest E, et al. Elevated alanine aminotransferase predicts new-onset type 2 diabetes independently of classical risk factors, metabolic syndrome, and C-reactive protein in the west of Scotland coronary prevention study. Diabetes. 2004;53:2855–60. doi: 10.2337/diabetes.53.11.2855. [DOI] [PubMed] [Google Scholar]
- 19.Resnick HE, Jones K, Ruotolo G, Jain AK, Henderson J, Lu W, et al. Insulin resistance, the metabolic syndrome, and risk of incident cardiovascular disease in non-diabetic American Indians: The Strong Heart Study. Diabetes Care. 2003;26:861–7. doi: 10.2337/diacare.26.3.861. [DOI] [PubMed] [Google Scholar]
- 20.Takahashi K, Bokura H, Kobayashi S, Iijima K, Nagai A, Yamaguchi S. Metabolic syndrome increases the risk of ischemic stroke in women. Intern Med. 2007;46:643–8. doi: 10.2169/internalmedicine.46.6094. [DOI] [PubMed] [Google Scholar]
- 21.Kurl S, Laukkanen JA, Niskanen L, Laaksonen D, Sivenius J, Nyyssönen K, et al. Metabolic syndrome and the risk of stroke in middle-aged men. Stroke. 2006;37:806–11. doi: 10.1161/01.STR.0000204354.06965.44. [DOI] [PubMed] [Google Scholar]
- 22.Iso H, Sato S, Kitamura A, Imano H, Kiyama M, Yamagishi K, et al. Metabolic syndrome and the risk of ischemic heart disease and stroke among Japanese men and women. Stroke. 2007;38:1744–51. doi: 10.1161/STROKEAHA.106.469072. [DOI] [PubMed] [Google Scholar]
- 23.Sharifi F, Mousavinasab SN, Saeini M, Dinmohammadi M. Prevalence of metabolic syndrome in an adult urban population of the west of Iran. Exp Diabetes Res 2009. 2009 doi: 10.1155/2009/136501. 136501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhoi SK, Kalita J, Misra UK. Metabolic syndrome and insulin resistance in migraine. J Headache Pain. 2012;3:321–6. doi: 10.1007/s10194-012-0416-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The International Classification of Headache Disorders: 2nd edition. Headache classification sub-committee of the International Headache Society. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 26.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High blood cholesterol in Adults (Adults Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High blood cholesterol in Adults (Adults Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 27.Bigal ME, Lipton RB, Holland PR, Goadsby PJ. Obesity, migraine, and chronic migraine: Possible mechanisms of interaction. Neurology. 2007;68:1851–61. doi: 10.1212/01.wnl.0000262045.11646.b1. [DOI] [PubMed] [Google Scholar]
- 28.Peterlin BL, Rosso AL, Rapoport AM, Scher AI. Obesity and migraine: The effect of age, gender and adipose tissue distribution. Headache. 2010;50:52–62. doi: 10.1111/j.1526-4610.2009.01459.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Robberstad L, Dyb G, Hagen K, Stovner LJ, Holmen TL, Zwart JA. An unfavorable lifestyle and recurrent headaches among adolescents: The HUNT study. Neurology. 2010;75:712–7. doi: 10.1212/WNL.0b013e3181eee244. [DOI] [PubMed] [Google Scholar]
- 30.Vo M, Ainalem A, Qiu C, Peterlin BL, Aurora SK, Williams MA. Body mass index and adult weight gain among reproductive age women with migraine. Headache. 2011;51:559–69. doi: 10.1111/j.1526-4610.2010.01833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu S, Liu R, Yang X, Zhao G, Qiao X, Feng J, et al. Body mass index and migraine: A survey of the Chinese adult population. J Headache Pain. 2012;13:531–6. doi: 10.1007/s10194-012-0470-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saberi A, Hatamian HR, Kazemnejad E, Ghorbannejad N. Hyperlipidemia in migraine: Is it more frequent in migraineurs? Iran J Neurol. 2011;10:46–50. [PMC free article] [PubMed] [Google Scholar]


